Stuck in the Present: A Human Lack of Ability to Visualise (Different) Needs in the Future May Hamper Timely Implementation of AAL and Supportive Technology
Abstract
:1. Introduction
Framing of the Research Design
2. Method
2.1. Research Design and Research Questions
2.2. Target Group
2.3. Privacy and Pretesting
2.4. Data Processing
2.5. Univariate and Multivariate Statistics
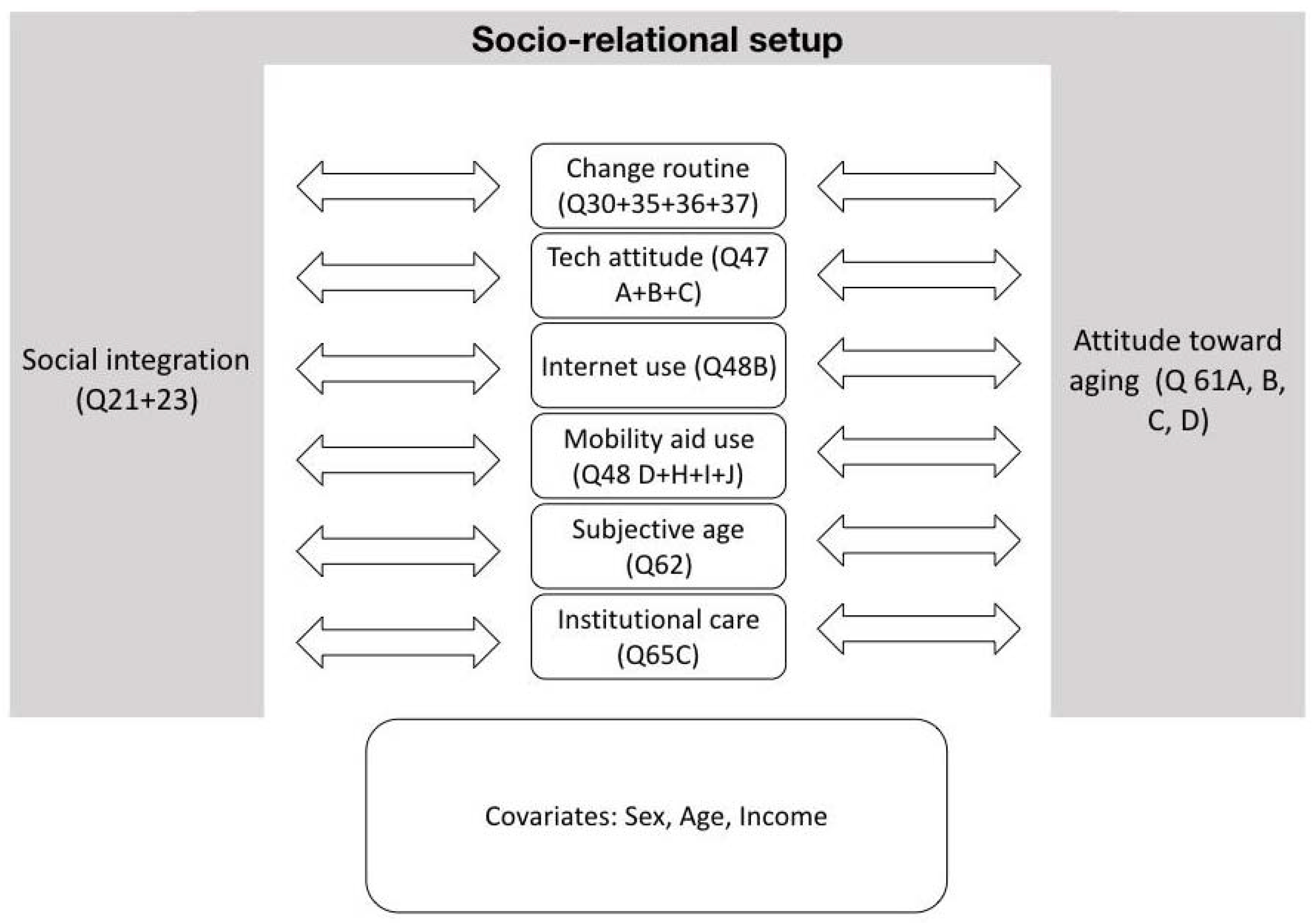
- “social integration” (Q21 + Q23);
- “Compared to others my age, I feel healthier/less healthy (Q61A);
- fitter/less fit (Q61B);
- more active/less active (Q61C); and
- more content/less content” (Q61D) separately on the variables;
- (a)
- “Change of Routines” (Q30 + 35 + 36 + 37);
- (b)
- “Technology Attitude” (Q47 A + B + C), “Mobility Aid use” (Q48D + H + I + J);
- (c)
- “Internet use” (Q48B);
- (d)
- “Subjective Age” (Q62);
- (e)
- Institutional Care Openness” (Q65C).
- “Compared to others my age, I feel healthier/less healthy (Q61A);
- fitter/less fit (Q61B);
- more active/less active (Q61C); and
- more content/less content” (Q61D) separately on the variables;
- (a)
- “Change of Routines” (Q30 + 35 + 36 + 37);
- (b)
- “Technology Attitude” (Q47 A + B + C), “Mobility Aid use” (Q48D + H + I + J);
- (c)
- “Internet use” (Q48B);
- (d)
- “Subjective Age” (Q62);
- (e)
- Institutional Care Openness” (Q65C).
3. Results
3.1. Descriptive Results
3.1.1. Ageing in Place and Care
3.1.2. Home Adaptations and Technology Use
3.1.3. Subjective Ageing
3.2. Univariate Results
3.2.1. Social Integration, Change Routines, Technology Attitude
3.2.2. Institutional Care Openness
3.3. Multivariate Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dobre, C.; Mavromoustakis, C.X.; Garcia, N.M.; Mastorakis, G.; Goleva, R.I. Introduction to the AAL and ELE Systems. In Ambient Assisted Living and Enhanced Living Environments; Elsevier: Amsterdam, The Netherlands, 2017; pp. 1–16. ISBN 978-0-12-805195-5. [Google Scholar]
- Peine, A.; Faulkner, A.; Jæger, B.; Moors, E. Science, Technology and the ‘Grand Challenge’ of Ageing—Understanding the Socio-Material Constitution of Later Life. Technol. Forecast. Soc. Chang. 2015, 93, 1–9. [Google Scholar] [CrossRef]
- AAL Europe Programme. 2020. Available online: http://www.aal-europe.eu (accessed on 24 February 2022).
- Van Dyk, S.; Lessenich, S.; Denninger, T.; Richter, A. The Many Meanings of “Active Ageing”. Confronting Public Discourse with Older People’s Stories. Rech. Sociol. Anthropol. 2013, 44, 97–115. [Google Scholar] [CrossRef]
- Wan, X.; Lighthall, N.R.; Paulson, D. Subjective Markers of Successful Aging and Change in Internet Use among Older Adults: The Distinctive Role of Subjective Health. Comput. Hum. Behav. 2022, 127, 107064. [Google Scholar] [CrossRef]
- Zhang, S.; Nugent, C.; Lundström, J.; Sheng, M. Ambient Assisted Living for Improvement of Health and Quality of Life—A Special Issue of the Journal of Informatics. Informatics 2018, 5, 4. [Google Scholar] [CrossRef] [Green Version]
- Bechtold, U.; Waibel, U.; Sotoudeh, M. DiaLogbuch AAL Dialoge zu Active and Assisted Living; Austrian Computer Society: Vienna, Austria, 2016; ISBN 978-3-902580-12-2. [Google Scholar]
- Fletcher-Watson, B.; Crompton, C.J.; Hutchison, M.; Lu, H. Strategies for Enhancing Success in Digital Tablet Use by Older Adults: A Pilot Study. Gerontechnology 2016, 15, 162–170. [Google Scholar] [CrossRef] [Green Version]
- Mollenkopf, H. Societal Aspects and Individual Preconditions of Technological Development. Gerontechnology 2016, 15, 216–226. [Google Scholar] [CrossRef]
- Tinker, A. Some Ethical Issues in Research on the Housing of Older People. Gerontechnology 2016, 15, 192–197. [Google Scholar] [CrossRef]
- Bechtold, U.; Sotoudeh, M. Assistive Technologies: Their Development from a Technology Assessment Perspective. Gerontechnology 2013, 11, 521–533. [Google Scholar] [CrossRef]
- Czaja, S.J.; Charness, N.; Fisk, A.D.; Hertzog, C.; Nair, S.N.; Rogers, W.A.; Sharit, J. Factors Predicting the Use of Technology: Findings from the Center for Research and Education on Aging and Technology Enhancement (Create). Psychol. Aging 2006, 21, 333–352. [Google Scholar] [CrossRef] [Green Version]
- Bechtold, U.; Capari, L. Paternalistic Rather Than Assistive? Concepts and Social Attributions of Older Adults Represented in Active Assisted Living Technology Project Descriptions. Gerontechnology 2020, 18, 193–205. [Google Scholar] [CrossRef]
- Neven, L.; Peine, A. From Triple Win to Triple Sin: How a Problematic Future Discourse Is Shaping the Way People Age with Technology. Societies 2017, 7, 26. [Google Scholar] [CrossRef]
- Cesta, A.; Cortellessa, G.; Fracasso, F.; Orlandini, A.; Turno, M. User Needs and Preferences on AAL Systems That Support Older Adults and Their Carers. J. Ambient Intell. Smart Environ. 2018, 10, 49–70. [Google Scholar] [CrossRef] [Green Version]
- Bechtold, U. Technologies in Care for Older People. Austria. In Technologies in Care for Older People; European Parliamentary Technology Assessment (EPTA Report); EPTA: Stockholm, Sweden, 2019; pp. 18–24. [Google Scholar]
- Austria Population Structure—Forecast 2017–2075. 2018. Available online: http://wko.at/statistik/bundesland/BevStruktur2050.pdf (accessed on 24 February 2022).
- Population Forecast for Austria up to 2050 by Age Group. 2012. Available online: http://wko.at/statistik/wgraf/2012_32_Bevölkerungsprognose_2050.pdf (accessed on 24 February 2022).
- Ruppe, G.; Stueckler, A.; Klambauer, E.; Wosko, P.; Pleschberger, S. Austrian Interdisciplinary Study on the Oldest Old. 2013. Available online: http://www.oepia.at/hochaltrigkeit/wp-content/uploads/2015/05/OEIHS_Endbericht_Endfassung1.pdf (accessed on 24 February 2022).
- Forecast Results Vienna 2018 to 2048. 2018. Available online: https://www.wien.gv.at/statistik/bevoelkerung/tabellen/bev-2048.html (accessed on 24 February 2022).
- Lestari, S.K.; de Luna, X.; Eriksson, M.; Malmberg, G.; Ng, N. A Longitudinal Study on Social Support, Social Participation, and Older Europeans’ Quality of Life. SSM—Popul. Health 2021, 13, 100747. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.-N.; Hu, P.; Yao, Y.; Zhao, Q.-H. Social Support as a Mediator between Depression and Quality of Life in Chinese Community-Dwelling Older Adults with Chronic Disease. Geriatr. Nurs. 2019, 40, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Vozikaki, M.; Linardakis, M.; Micheli, K.; Philalithis, A. Activity Participation and Well-Being among European Adults Aged 65 Years and Older. Soc. Indic. Res. 2017, 131, 769–795. [Google Scholar] [CrossRef]
- Ward, M.; McGarrigle, C.A.; Kenny, R.A. More Than Health: Quality of Life Trajectories among Older Adults—Findings from The Irish Longitudinal Study of Ageing (TILDA). Qual. Life Res. 2019, 28, 429–439. [Google Scholar] [CrossRef]
- Hawton, A.; Green, C.; Dickens, A.P.; Richards, S.H.; Taylor, R.S.; Edwards, R.; Greaves, C.J.; Campbell, J.L. The Impact of Social Isolation on the Health Status and Health-Related Quality of Life of Older People. Qual. Life Res. 2011, 20, 57–67. [Google Scholar] [CrossRef]
- Heo, J.; Chun, S.; Lee, S.; Lee, K.H.; Kim, J. Internet Use and Well-Being in Older Adults. Cyberpsychol. Behav. Soc. Netw. 2015, 18, 268–272. [Google Scholar] [CrossRef]
- Bechtold, U.; Stauder, N.; Fieder, M. Let’s Walk It: Mobility and the Perceived Quality of Life in Older Adults. Int. J. Environ. Res. Public Health 2021, 18, 11515. [Google Scholar] [CrossRef]
- Baumstarck, K.; Pelletier, J.; Butzkueven, H.; Fernández, O.; Flachenecker, P.; Idiman, E.; Stecchi, S.; Boucekine, M.; Auquier, P.; for the MusiQoL Study Group. Health-Related Quality of Life as an Independent Predictor of Long-Term Disability for Patients with Relapsing-Remitting Multiple Sclerosis. Eur. J. Neurol. 2013, 20, 907-e79. [Google Scholar] [CrossRef]
- Wang, C.; Pu, R.; Ghose, B.; Tang, S. Chronic Musculoskeletal Pain, Self-Reported Health and Quality of Life among Older Populations in South Africa and Uganda. Int. J. Environ. Res. Public Health 2018, 15, 2806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baruch, Y.; Holtom, B.C. Survey Response Rate Levels and Trends in Organizational Research. Hum. Relat. 2008, 61, 1139–1160. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988; ISBN 978-0-8058-0283-2. [Google Scholar]
- Tavares, A.I. Health and Life Satisfaction Factors of Portuguese Older Adults. Arch. Gerontol. Geriatr. 2022, 99, 104600. [Google Scholar] [CrossRef]
- Rubin, D.C.; Berntsen, D. People over Forty Feel 20% Younger Than Their Age: Subjective Age across the Lifespan. Psychon. Bull. Rev. 2006, 13, 776–780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qiao, H.; Du, X.; Li, S.; Sun, Y.; Feng, W.; Wu, Y. Does Older Subjective Age Predict Poorer Cognitive Function and Higher Risk of Dementia in Middle-Aged and Older Adults? Psychiatry Res. 2021, 298, 113807. [Google Scholar] [CrossRef]
- Stephan, Y.; Sutin, A.R.; Caudroit, J.; Terracciano, A. Subjective Age and Changes in Memory in Older Adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2016, 71, 675–683. [Google Scholar] [CrossRef]
- Hubley, A.M.; Russell, L.B. Prediction of Subjective Age, Desired Age, and Age Satisfaction in Older Adults: Do Some Health Dimensions Contribute More Than Others? Int. J. Behav. Dev. 2009, 33, 12–21. [Google Scholar] [CrossRef]
- Weiss, D.; Lang, F.R. “They” Are Old but “I” Feel Younger: Age-Group Dissociation as a Self-Protective Strategy in Old Age. Psychol. Aging 2012, 27, 153–163. [Google Scholar] [CrossRef] [Green Version]
- Van Orden, K.A. Considering the Impact of Research Assessments: A Commentary on “COVID-19 Related Loneliness and Psychiatric Symptoms Among Older Adults: The Buffering Role of Subjective Age”. Am. J. Geriatr. Psychiatry 2020, 28, 1205–1207. [Google Scholar] [CrossRef]
- Lübbe, H. Gegenwartsschrumpfung. In Autorität; Kray, R., Pfeiffer, K.L., Studer, T., Eds.; VS Verlag für Sozialwissenschaften: Wiesbaden, Germany, 1992; pp. 78–91. ISBN 978-3-531-12401-8. [Google Scholar]
- Ehret, S.; Gehring, P.; Grebe, H.; Höffe, O.; Jakobs, T.; Martens, E.; Otto, W.G.; Wiegand, C.; Martens, E.; Otto, W.-G.; et al. Altern in Unserer Zeit: Späte Lebensphasen Zwischen Vitalität Und Endlichkeit; Rentsch, T., Zimmermann, H.-P., Kruse, A., Eds.; Campus: Frankfurt, Germany, 2013; ISBN 978-3-593-39908-9. [Google Scholar]
- Fleuren, N.; Depla, M.F.I.A.; Pasman, H.R.W.; Janssen, D.J.A.; Onwuteaka-Philipsen, B.D.; Hertogh, C.M.P.M.; Huisman, M. Association between Subjective Remaining Life Expectancy and Advance Care Planning in Older Adults: A Cross-Sectional Study. J. Pain Symptom Manag. 2021, 62, 757–767. [Google Scholar] [CrossRef]
- Carstensen, L.L. Socioemotional Selectivity Theory: The Role of Perceived Endings in Human Motivation. Gerontologist 2021, 61, 1188–1196. [Google Scholar] [CrossRef] [PubMed]
- Banks, J.; Bassoli, E.; Mammi, I. Changing Attitudes to Risk at Older Ages: The Role of Health and Other Life Events. J. Econ. Psychol. 2020, 79, 102208. [Google Scholar] [CrossRef]
- Festinger, L. A Theory of Cognitive Dissonance; Stanford University Press: Stanford, CA, USA, 2001; ISBN 978-0-8047-0911-8. [Google Scholar]
- Kollmuss, A.; Agyeman, J. Mind the Gap: Why Do People Act Environmentally and What Are the Barriers to Pro-Environmental Behavior? Environ. Educ. Res. 2002, 8, 239–260. [Google Scholar] [CrossRef] [Green Version]
- Sailer, A.; Wilfing, H.; Straus, E. Greenwashing and Bluewashing in Black Friday-Related Sustainable Fashion Marketing on Instagram. Sustainability 2022, 14, 1494. [Google Scholar] [CrossRef]
- Nakagomi, A.; Shiba, K.; Kawachi, I.; Ide, K.; Nagamine, Y.; Kondo, N.; Hanazato, M.; Kondo, K. Internet Use and Subsequent Health and Well-Being in Older Adults: An Outcome-Wide Analysis. Comput. Hum. Behav. 2022, 130, 107156. [Google Scholar] [CrossRef]
- Poli, A.; Kelfve, S.; Klompstra, L.; Strömberg, A.; Jaarsma, T.; Motel-Klingebiel, A. Prediction of (Non)Participation of Older People in Digital Health Research: Exergame Intervention Study. J. Med. Internet Res. 2020, 22, e17884. [Google Scholar] [CrossRef]
- Chen, Y.; Persson, A. Internet Use among Young and Older Adults: Relation to Psychological Well-Being. Educ. Gerontol. 2002, 28, 731–744. [Google Scholar] [CrossRef]
- König, R.; Seifert, A.; Doh, M. Internet Use among Older Europeans: An Analysis Based on SHARE Data. Univ. Access Inf. Soc. 2018, 17, 621–633. [Google Scholar] [CrossRef]
- Eurostat. How Popular Is Internet Use among Older People? 2020. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20210517-1 (accessed on 24 February 2022).
- Halmdienst, N.; Schmidt, M. Digitale Kompetenz der Generation 50+ in Österreich. 2018. Available online: https://www.share-austria.at/fileadmin/user_upload/papers/SHARE_Report_10_2018_Digitale_Kompetenz_online.pdf (accessed on 24 February 2022).
- Szybalska, A.; Broczek, K.; Puzianowska-Kuznicka, M.; Slusarczyk, P.; Chudek, J.; Skalska, A.; Mossakowska, M. Self-Rated Health and Its Association with All-Cause Mortality of Older Adults in Poland: The PolSenior Project. Arch. Gerontol. Geriatr. 2018, 79, 13–20. [Google Scholar] [CrossRef]
- Wu, S.; Wang, R.; Zhao, Y.; Ma, X.; Wu, M.; Yan, X.; He, J. The Relationship between Self-Rated Health and Objective Health Status: A Population-Based Study. BMC Public Health 2013, 13, 320. [Google Scholar] [CrossRef] [Green Version]
- Benyamini, Y. Why Does Self-Rated Health Predict Mortality? An Update on Current Knowledge and a Research Agenda for Psychologists. Psychol. Health 2011, 26, 1407–1413. [Google Scholar] [CrossRef] [PubMed]
| Age | Mean (in yrs.) | SD (in yrs.) |
| 74 | 6654 | |
| Sex | Frequency | Percent |
| Male | 91 | 37.3% |
| Female | 151 | 61.6% |
| Income | ||
| Below 500 Euro | 7 | 2.9% |
| 500–1000 Euro | 24 | 10% |
| 1000–2000 Euro | 93 | 38.9% |
| 2000–3000 Euro | 58 | 24.3% |
| 3000–4000 Euro | 20 | 8.4% |
| 4000–5000 Euro | 8 | 3.3% |
| More than 5000 Euro | 8 | 3.3% |
| Health Compared to Others (61A) | Fitness Compared to Others (61B) | Activeness Compared to Others (61C) | Contentedness Compared to Others (61D) | |
|---|---|---|---|---|
| Health compared to others (61A) | 1 | |||
| Fitness compared to others (61B) | 0.580 ** | 1 | ||
| Activeness compared to others (61C) | 0.553 ** | 0.562 ** | 1 | |
| Contentedness compared to others (61D) | 0.444 ** | 0.402 ** | 0.446 ** | 1 |
| Change Routines (Q30 + Q35 + Q36 + Q37) | Technology Attitude (Q47) | Mobility Aid Use (Q48D + H + I + J) | Internet Use (Q48B) | Subjective Age (Q62) | Institutional Care Openness (Q65C) | |
|---|---|---|---|---|---|---|
| Social Integration (Q21 + Q23) | 4.149 | 0.479 | 2.736 | 0.905 | 1.458 | 7.703 |
| Health compared to others (Q61A) | 4.249 | 0.015 | 21.260 *** | 5.175 * | 11.866 *** | 6.501 |
| Fitness compared to others (Q61B) | 5.060 | 1.664 | 28.581 *** | 6.094 * | 11.811 *** | 18.279 *** |
| Activeness compared to others (Q61C) | 7.740 | 1.059 | 15.037 *** | 15.394 *** | 10.536 ** | 23.382 *** |
| Contentedness compared to others (Q61D) | 1.309 | 0.686 | 10.142 ** | 3.893 | 5.489 * | 4.419 |
| Change Routines (Q30 + Q35 + Q36 + Q37) | Technology Attitude (Q47) | Mobility Aid Use (Q48D + H + I + J) | Internet Use (Q48B) | Subjective Age (Q62) | Institutional Care Openness (Q65C) | |
|---|---|---|---|---|---|---|
| Health compared to others (Q61A) | −0.138 | 0.070 | 1.958 *** | −0.583 | −18.03 | −0.676 |
| Fitness compared to others (Q61B) | 0.123 | −0.326 | 2.068 *** | −0.896 * | −17.272 | 1.486 *** |
| Activeness compared to others (Q61C) | −0.101 | −0.339 | 1.586 *** | −0.9134 * | −2.681 * | 1.336 *** |
| Contentedness compared to others (Q61D) | −0.213 | −0.393 | 1.419 *** | −1.053 ** | −1.738 * | 0.534 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bechtold, U.; Stauder, N.; Fieder, M.; Wilfing, H. Stuck in the Present: A Human Lack of Ability to Visualise (Different) Needs in the Future May Hamper Timely Implementation of AAL and Supportive Technology. Int. J. Environ. Res. Public Health 2022, 19, 6804. https://doi.org/10.3390/ijerph19116804
Bechtold U, Stauder N, Fieder M, Wilfing H. Stuck in the Present: A Human Lack of Ability to Visualise (Different) Needs in the Future May Hamper Timely Implementation of AAL and Supportive Technology. International Journal of Environmental Research and Public Health. 2022; 19(11):6804. https://doi.org/10.3390/ijerph19116804
Chicago/Turabian StyleBechtold, Ulrike, Natalie Stauder, Martin Fieder, and Harald Wilfing. 2022. "Stuck in the Present: A Human Lack of Ability to Visualise (Different) Needs in the Future May Hamper Timely Implementation of AAL and Supportive Technology" International Journal of Environmental Research and Public Health 19, no. 11: 6804. https://doi.org/10.3390/ijerph19116804
APA StyleBechtold, U., Stauder, N., Fieder, M., & Wilfing, H. (2022). Stuck in the Present: A Human Lack of Ability to Visualise (Different) Needs in the Future May Hamper Timely Implementation of AAL and Supportive Technology. International Journal of Environmental Research and Public Health, 19(11), 6804. https://doi.org/10.3390/ijerph19116804






