Predictors of Frequent Emergency Department Use and Hospitalization among Patients with Substance-Related Disorders Recruited in Addiction Treatment Centers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Context–the Quebec Healthcare System
2.2. Study Sample, Design, and Sources
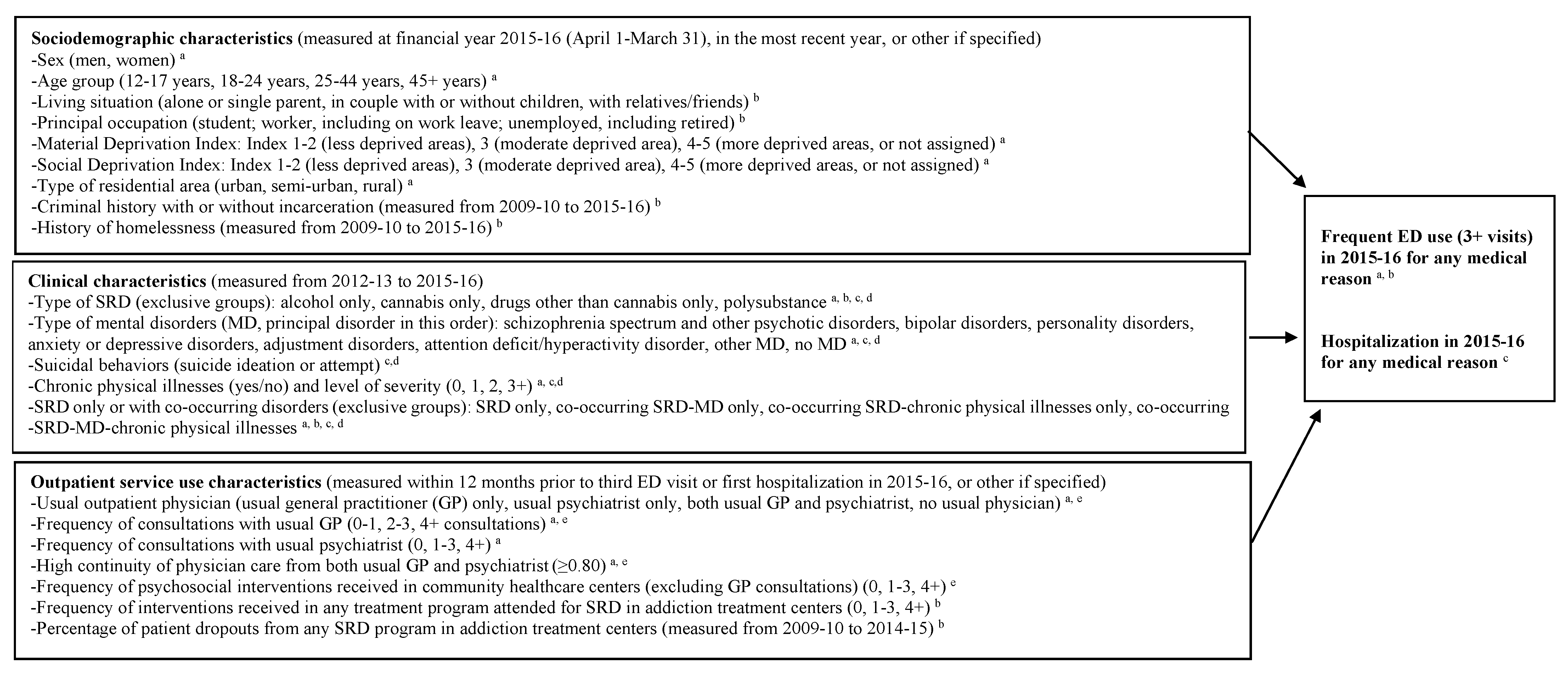
2.3. Variables
2.4. Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- APA. Diagnostic and Statistic Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Doupe, M.B.; Palatnick, W.; Day, S.; Chateau, D.; Soodeen, R.-A.; Burchill, C.; Derksen, S. Frequent Users of Emergency Departments: Developing Standard Definitions and Defining Prominent Risk Factors. Ann. Emerg. Med. 2012, 60, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Minassian, A.; Vilke, G.M.; Wilson, M.P. Frequent emergency department visits are more prevalent in psychiatric, alcohol abuse, and dual diagnosis conditions than in chronic viral illnesses such as hepatitis and human immunodeficiency virus. J. Emerg. Med. 2013, 45, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Cederbaum, J.A.; Guerrero, E.G.; Mitchell, K.R.; Kim, T. Utilization of emergency and hospital services among individuals in substance abuse treatment. Subst. Abus. Treat. Prev. Policy 2014, 9, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, S.; Schultz, E.; Raven, M.; Wang, N.E.; Stocks, C.L.; Delgado, M.K.; McDonald, K.M. Development and Validation of the Agency for Healthcare Research and Quality Measures of Potentially Preventable Emergency Department (ED) Visits: The ED Prevention Quality Indicators for General Health Conditions. Health Serv. Res. 2017, 52, 1667–1684. [Google Scholar] [CrossRef]
- Nesper, A.C.; Morris, B.A.; Scher, L.M.; Holmes, J.F. Effect of Decreasing County Mental Health Services on the Emergency Department. Ann. Emerg. Med. 2016, 67, 525–530. [Google Scholar] [CrossRef]
- Suen, L.W.; Makam, A.N.; Snyder, H.R.; Repplinger, D.; Kushel, M.B.; Martin, M.; Nguyen, O.K. National Prevalence of Alcohol and Other Substance Use Disorders Among Emergency Department Visits and Hospitalizations: NHAMCS 2014–2018. J. Gen. Intern. Med. 2021. online ahead of print. [Google Scholar] [CrossRef]
- Vu, F.; Daeppen, J.B.; Hugli, O.; Iglesias, K.; Stucki, S.; Paroz, S.; Canepa Allen, M.; Bodenmann, P. Screening of mental health and substance users in frequent users of a general Swiss emergency department. BMC Emerg. Med. 2015, 15, 27. [Google Scholar] [CrossRef] [Green Version]
- Penzenstadler, L.; Gentil, L.; Huynh, C.; Grenier, G.; Fleury, M.J. Variables associated with low, moderate and high emergency department use among patients with substance-related disorders. Drug Alcohol Depend. 2020, 207, 107817. [Google Scholar] [CrossRef]
- Kingston, R.E.F.; Marel, C.; Mills, K.L. A systematic review of the prevalence of comorbid mental health disorders in people presenting for substance use treatment in Australia. Drug Alcohol Rev. 2017, 36, 527–539. [Google Scholar] [CrossRef]
- Di Giovanni, P.; Di Martino, G.; Zecca, I.A.L.; Porfilio, I.; Romano, F.; Staniscia, T. Trend in Hospital Admissions of Drug Addicts and Associated Factors from 2006 to 2015: An Observational Study on the Hospitals’ Discharge Registries from a Region of Central Italy. Ann. Ig. 2020, 32, 376–384. [Google Scholar]
- Huynh, C.; Ferland, F.; Blanchette-Martin, N.; Menard, J.M.; Fleury, M.J. Factors Influencing the Frequency of Emergency Department Utilization by Individuals with Substance Use Disorders. Psychiatr. Q 2016, 87, 713–728. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.T.; Swartz, M.S.; Wu, Z.; Mannelli, P.; Yang, C.; Blazer, D.G. Alcohol and drug use disorders among adults in emergency department settings in the United States. Ann. Emerg. Med. 2012, 60, 172–180.e5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Association des centres de réadaptation en dépendance du Québec. Rapport Annuel 2013–2014. Baliser L’action. Protéger L’offre de Service en Dépendance; Association des Centres de Réadaptation en Dépendance: Montréal, QC, Canada, 2014. [Google Scholar]
- Régie de l’assurance maladie du Québec. Rapport Annuel de Gestion, 2016–2017; Régie de l’assurance maladie du Québec: Québec, QC, Canada, 2017. [Google Scholar]
- Gaulin, M.; Simard, M.; Candas, B.; Lesage, A.; Sirois, C. Combined impacts of multimorbidity and mental disorders on frequent emergency department visits: A retrospective cohort study in Quebec, Canada. CMAJ 2019, 191, E724–E732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krieg, C.; Hudon, C.; Chouinard, M.C.; Dufour, I. Individual predictors of frequent emergency department use: A scoping review. BMC Health Serv. Res. 2016, 16, 594. [Google Scholar] [CrossRef] [Green Version]
- Pampalon, R.; Hamel, D.; Gamache, P.; Raymond, G. A deprivation index for health planning in Canada. Chronic. Dis. Can. 2009, 29, 178–191. [Google Scholar] [CrossRef]
- Simard, M.; Dubé, M.; Myles, G.; Sirois, C. La Prévalence de la Multimorbidité au Québec: Portrait Pour L’année 2016–2017; Institut national de Santé Publique du Québec: Québec, QC, Canada, 2019. [Google Scholar]
- Dreiher, J.; Comaneshter, D.S.; Rosenbluth, Y.; Battat, E.; Bitterman, H.; Cohen, A.D. The association between continuity of care in the community and health outcomes: A population-based study. Isr. J. Health Policy Res. 2012, 1, 21. [Google Scholar] [CrossRef] [Green Version]
- Wang, P.S.; Demler, O.; Kessler, R.C. Adequacy of Treatment for Serious Mental Illness in the United States. Am. J. Public Health 2002, 92, 92–98. [Google Scholar] [CrossRef]
- Menear, M.; Duhoux, A.; Roberge, P.; Fournier, L. Primary care practice characteristics associated with the quality of care received by patients with depression and comorbid chronic conditions. Gen. Hosp. Psychiatry 2014, 36, 302–309. [Google Scholar] [CrossRef]
- Young, A.S.; Klap, R.; Shoai, R.; Wells, K.B. Persistent depression and anxiety in the United States: Prevalence and quality of care. Psychiatr. Serv. 2008, 59, 1391–1398. [Google Scholar] [CrossRef]
- Breslau, N.; Reeb, K.G. Continuity of care in a university-based practice. J. Med. Educ. 1975, 50, 965–969. [Google Scholar] [CrossRef]
- Swanson, J.O.; Vogt, V.; Sundmacher, L.; Hagen, T.P.; Moger, T.A. Continuity of care and its effect on readmissions for COPD patients: A comparative study of Norway and Germany. Health Policy 2018, 122, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, J.W.; Harel, O.; Carpenter, J.R. Asymptotically Unbiased Estimation of Exposure Odds Ratios in Complete Records Logistic Regression. Am. J. Epidemiol. 2015, 182, 730–736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akaike, H. Information Theory and an Extension of the Maximum Likelihood Principle. In Proceedings of the 2nd International Symposium on Information Theory; Petrov, B.N., Csaki, F., Eds.; Akademiai Kiado: Budapest, Magyarország, 1973; pp. 267–281. [Google Scholar]
- Menard, S. Applied Logistic Regression Analysis, 2nd ed.; Sage Pulication, Inc.: Thousand Oaks, CA, USA, 2001. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 17; StataCorp LLC: College Station, TX, USA, 2021. [Google Scholar]
- Moe, J.; Camargo, C.A.; Davis, R.B.; Jelinski, S.; Rowe, B.H. Frequent emergency department use and mortality in patients with substance and opioid use in Alberta: A population-based retrospective cohort study. CJEM 2019, 21, 482–491. [Google Scholar] [CrossRef] [PubMed]
- SAMSHA. Key Substance use and Mental Health Indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56); Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Brockville, MD, USA, 2021. Available online: https://www.samhsa.gov/data/report/2020-nsduh-annual-national-report (accessed on 23 January 2022).
- Penzenstadler, L.; Gentil, L.; Grenier, G.; Khazaal, Y.; Fleury, M.J. Risk factors of hospitalization for any medical condition among patients with prior emergency department visits for mental health conditions. BMC Psychiatry 2020, 20, 431. [Google Scholar] [CrossRef]
- Brennan, J.J.; Chan, T.C.; Hsia, R.Y.; Wilson, M.P.; Castillo, E.M. Emergency department utilization among frequent users with psychiatric visits. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2014, 21, 1015–1022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, J.D.; Calkins, M.E.; Scott, J.C.; Bach, E.C.; Gur, R.E. Cannabis Use, Polysubstance Use, and Psychosis Spectrum Symptoms in a Community-Based Sample of U.S. Youth. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2017, 60, 653–659. [Google Scholar] [CrossRef]
- Connor, J.P.; Gullo, M.J.; White, A.; Kelly, A.B. Polysubstance use: Diagnostic challenges, patterns of use and health. Curr. Opin. Psychiatry 2014, 27, 269–275. [Google Scholar] [CrossRef] [Green Version]
- Armoon, B.; Grenier, G.; Cao, Z.; Huynh, C.; Fleury, M.J. Frequencies of emergency department use and hospitalization comparing patients with different types of substance or polysubstance-related disorders. Subst. Abus. Treat. Prev. Policy 2021, 16, 89. [Google Scholar] [CrossRef]
- Piscopo, K.; Lipari, R.N.; Cooney, J.; Glasheen, C. Suicidal Thoughts and Behavior among Adults: Results from the 2015 National Survey on Drug Use and Health; NSDUH Data Review; National Survey on Drug Use and Health: Rockville, MD, USA, 2016; p. 71. [Google Scholar]
- Poorolajal, J.; Haghtalab, T.; Farhadi, M.; Darvishi, N. Substance use disorder and risk of suicidal ideation, suicide attempt and suicide death: A meta-analysis. J. Public Health 2016, 38, e282–e291. [Google Scholar] [CrossRef]
- Canner, J.K.; Giuliano, K.; Selvarajah, S.; Hammond, E.R.; Schneider, E.B. Emergency department visits for attempted suicide and self harm in the USA: 2006-2013. Epidemiol. Psychiatr. Sci. 2018, 27, 94–102. [Google Scholar] [CrossRef] [Green Version]
- Martins, S.S.; Sampson, L.; Cerda, M.; Galea, S. Worldwide Prevalence and Trends in Unintentional Drug Overdose: A Systematic Review of the Literature. Am. J. Public Health 2015, 105, e29–e49. [Google Scholar] [CrossRef] [PubMed]
- Fareed, A.; Stout, S.; Casarella, J.; Vayalapalli, S.; Cox, J.; Drexler, K. Illicit opioid intoxication: Diagnosis and treatment. Subst. Abus. 2011, 5, 17–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fulde, G.W.; Forster, S.L. The impact of amphetamine-type stimulants on emergency services. Curr. Opin. Psychiatry 2015, 28, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Maghsoudi, N.; Tanguay, J.; Scarfone, K.; Rammohan, I.; Ziegler, C.; Werb, D.; Scheim, A.I. Drug checking services for people who use drugs: A systematic review. Addiction 2022, 117, 532–544. [Google Scholar] [CrossRef]
- Ivsins, A.; Boyd, J.; Beletsky, L.; McNeil, R. Tackling the overdose crisis: The role of safe supply. Int. J. Drug Policy 2020, 80, 102769. [Google Scholar] [CrossRef]
- Kenney, S.R.; Anderson, B.J.; Bailey, G.L.; Herman, D.S.; Conti, M.T.; Stein, M.D. Examining Overdose and Homelessness as Predictors of Willingness to Use Supervised Injection Facilities by Services Provided Among Persons Who Inject Drugs. Am. J. Addict. Am. Acad. Psychiatr. Alcohol. Addict. 2021, 30, 21–25. [Google Scholar] [CrossRef]
- Connor, J.P.; Haber, P.S.; Hall, W.D. Alcohol use disorders. Lancet 2016, 387, 988–998. [Google Scholar] [CrossRef] [Green Version]
- Roerecke, M.; Rehm, J. Cause-specific mortality risk in alcohol use disorder treatment patients: A systematic review and meta-analysis. Int. J. Epidemiol. 2014, 43, 906–919. [Google Scholar] [CrossRef]
- Brorson, H.H.; Ajo Arnevik, E.; Rand-Hendriksen, K.; Duckert, F. Drop-out from addiction treatment: A systematic review of risk factors. Clin. Psychol. Rev. 2013, 33, 1010–1024. [Google Scholar] [CrossRef]
- Amaro, H.; Black, D.S. Moment-by-Moment in Women’s Recovery: Randomized controlled trial protocol to test the efficacy of a mindfulness-based intervention on treatment retention and relapse prevention among women in residential treatment for substance use disorder. Contemp. Clin. Trials 2017, 62, 146–152. [Google Scholar] [CrossRef] [Green Version]
- Earnshaw, V.A.; Sepucha, K.R.; Laurenceau, J.P.; Subramanian, S.V.; Brousseau, N.M.; Chaudoir, S.R.; Hill, E.C.; Morrison, L.M.; Kelly, J.F. Disclosure processes as predictors of relationship outcomes among people in recovery from opioid use disorder: A longitudinal analysis. Drug Alcohol Depend. 2021, 228, 109093. [Google Scholar] [CrossRef] [PubMed]
- Bourion-Bedes, S.; Simirea, A.; Di Patrizio, P.; Muller, O.; Clerc-Urmes, I.; Sy, A.; Schwan, R.; Viennet, S.; Baumann, C. Is early outpatient satisfaction with substance use disorder care a predictor of early dropout? Results of the SUBUSQOL cohort. J. Subst. Abus. Treat. 2020, 119, 108151. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.; Sullivan, N.; Monte, A.A.; Vargas, N.M.; Cooper, Z.D.; Ma, Y.; Meltzer, A.C. Motivational interviewing to treat substance use disorders in the emergency department: A scoping review. Am. J. Emerg. Med. 2022, 51, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Park, S.E.; Mosley, J.E.; Grogan, C.M.; Pollack, H.A.; Humphreys, K.; D’Aunno, T.; Friedmann, P.D. Patient-centered care’s relationship with substance use disorder treatment utilization. J. Subst. Abus. Treat. 2020, 118, 108125. [Google Scholar] [CrossRef]
- Hermann, R.C.; Leff, H.S.; Palmer, R.H.; Yang, D.; Teller, T.; Provost, S.; Jakubiak, C.; Chan, J. Quality measures for mental health care: Results from a national inventory. Med. Care Res. Rev. 2000, 57 (Suppl. S2), 136–154. [Google Scholar] [CrossRef]
- McCabe, R.; Bullenkamp, J.; Hansson, L.; Lauber, C.; Martinez-Leal, R.; Rossler, W.; Salize, H.J.; Svensson, B.; Torres-Gonzalez, F.; van den Brink, R.; et al. The therapeutic relationship and adherence to antipsychotic medication in schizophrenia. PLoS ONE 2012, 7, e36080. [Google Scholar] [CrossRef]
- Urbanoski, K.; Inglis, D.; Veldhuizen, S. Service Use and Unmet Needs for Substance Use and Mental Disorders in Canada. Can. J. Psychiatry 2017, 62, 551–559. [Google Scholar] [CrossRef] [Green Version]
- Hyshka, E.; Anderson, J.T.; Wild, T.C. Perceived unmet need and barriers to care amongst street-involved people who use illicit drugs. Drug Alcohol Rev. 2017, 36, 295–304. [Google Scholar] [CrossRef]
- Fleury, M.J.; Grenier, G.; Gentil, L. Profiles of Quebec specialist respondent-psychiatrists (SRP) based on their perceptions related to the capacity of the SRP function to improve treatment of mental health disorders in primary care and youth centers. Ment. Health Fam. Med. 2021, 19, 1054–1062. [Google Scholar]
- Fazel, S.; Geddes, J.R.; Kushel, M. The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet 2014, 384, 1529–1540. [Google Scholar] [CrossRef] [Green Version]
- Gentil, L.; Grenier, G.; Bamvita, J.M.; Fleury, M.J. Satisfaction with health and community services among homeless and formerly homeless individuals in Quebec, Canada. Health Soc. Care Community 2020, 28, 22–33. [Google Scholar] [CrossRef]
- Ngamini-Ngui, A.; Fleury, M.J.; Moisan, J.; Gregoire, J.P.; Lesage, A.; Vanasse, A. High users of emergency departments in Quebec among patients with both schizophrenia and a substance use disorder. Psychiatr. Serv. 2014, 65, 1389–1391. [Google Scholar] [CrossRef] [PubMed]
- Liebling, E.J.; Green, T.C.; Hadland, S.E.; Marshall, B.D.L. Injection drug use and overdose among young adults who use prescription opioids non-medically. Addict. Behav. 2018, 76, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Gicquel, L.; Ordonneau, P.; Blot, E.; Toillon, C.; Ingrand, P.; Romo, L. Description of Various Factors Contributing to Traffic Accidents in Youth and Measures Proposed to Alleviate Recurrence. Front. Psychiatry 2017, 8, 94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plaistow, J.; Masson, K.; Koch, D.; Wilson, J.; Stark, R.M.; Jones, P.B.; Lennox, B.R. Young people’s views of UK mental health services. Early Interv. Psychiatry 2014, 8, 12–23. [Google Scholar] [CrossRef]
- Onyeka, I.N.; Beynon, C.M.; Ronkainen, K.; Tiihonen, J.; Fohr, J.; Kuikanmaki, O.; Paasolainen, M.; Kauhanen, J. Hospitalization in a cohort seeking treatment for illicit drug use in Finland. J. Subst. Abus. Treat. 2015, 53, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Simunovic Filipcic, I.; Ivezic, E.; Jaksic, N.; Mayer, N.; Grah, M.; Rojnic Kuzman, M.; Bajic, Z.; Svab, V.; Herceg, M.; Filipcic, I. Gender differences in early onset of chronic physical multimorbidities in schizophrenia spectrum disorder: Do women suffer more? Early Interv. Psychiatry 2020, 14, 418–427. [Google Scholar] [CrossRef]
| N | % | |
|---|---|---|
| Sociodemographic characteristics (2015–2016, in the most recent year, or other if specified) | ||
| Men | 11,676 | 65.53 |
| Women | 6143 | 34.47 |
| Age group (years) | ||
| 12–17 | 800 | 4.49 |
| 18–24 | 2960 | 16.61 |
| 25–44 | 8016 | 44.99 |
| 45+ | 6043 | 33.91 |
| Living situation (n = 16,134) | ||
| Alone (or single parent) | 7376 | 45.72 |
| Couple with or without children | 3121 | 19.34 |
| Living with relatives/friends | 5637 | 34.94 |
| Principal occupation a | ||
| Student | 2422 | 13.59 |
| Worker, including on work leave | 5756 | 32.30 |
| Unemployed, including retired | 9641 | 54.11 |
| Material Deprivation Index b | ||
| 1 and 2 | 4748 | 26.65 |
| 3 | 3114 | 17.48 |
| 4, 5 and not assigned | 9957 | 55.88 |
| Social Deprivation Index b | ||
| 1 and 2 | 4029 | 22.61 |
| 3 | 2755 | 15.46 |
| 4, 5, and not assigned | 11,035 | 61.93 |
| Type of residential area (n = 17,802) | ||
| Urban (>100,000) | 9241 | 51.91 |
| Semi-urban (10,000 to 100,000) | 5193 | 29.17 |
| Rural (<10,000) | 3368 | 18.92 |
| Criminal history with or without incarceration (2009–2010 to 2015–2016) | 3467 | 19.46 |
| History of homelessness (2009–2010 to 2015–2016) | 2417 | 13.56 |
| Clinical characteristics (2012–2013 to 2015) | ||
| Type of substance-related disorders (SRD, exclusive groups) | ||
| Alcohol only | 3451 | 19.37 |
| Cannabis only | 1575 | 8.84 |
| Drugs other than cannabis only | 1379 | 7.74 |
| Polysubstance | 11,414 | 64.06 |
| Cannabis and other drugs c | 1957 | 10.98 |
| Cannabis and alcohol c | 1325 | 7.44 |
| Drugs other than cannabis and alcohol c | 3967 | 22.26 |
| Cannabis, other drugs and alcohol c | 4165 | 23.37 |
| Type of mental disorders (MD, principal disorder) d | ||
| Schizophrenia spectrum and other psychotic disorders | 2584 | 14.50 |
| Bipolar disorders | 1617 | 9.07 |
| Personality disorders | 2084 | 11.70 |
| Anxiety or depressive disorders | 5465 | 30.67 |
| Adjustment disorders | 439 | 2.46 |
| Attention deficit/hyperactivity disorder | 423 | 2.37 |
| Other MD | 409 | 2.30 |
| No MD | 4798 | 26.93 |
| Suicidal behaviors (suicide ideation or attempt) | 2779 | 15.60 |
| Chronic physical illnesses e | 7278 | 40.84 |
| Elixhauser comorbidity index | ||
| 0 | 14,504 | 81.40 |
| 1 | 1056 | 5.93 |
| 2 | 1191 | 6.68 |
| 3+ | 1068 | 5.99 |
| SRD only or with co-occurring disorders (exclusive groups) | ||
| SRD only | 3500 | 19.64 |
| Co-occurring SRD-MD only | 7041 | 39.51 |
| Co-occurring SRD-chronic physical illnesses only | 1298 | 7.28 |
| Co-occurring SRD-MD-chronic physical illnesses | 5980 | 33.56 |
| Outpatient service use characteristics (within 12 months prior to third emergency department (ED) visit or first hospitalization in 2015–2016, or other if specified) f | ||
| Usual outpatient physician g | ||
| Usual general practitioner (GP) only | 6338 | 35.57 |
| Usual psychiatrist only | 1226 | 6.88 |
| Both usual GP and psychiatrist | 1754 | 9.84 |
| No usual physician | 8501 | 47.71 |
| Frequency of consultations with usual GP g | ||
| 0–1 | 9727 | 54.59 |
| 2–3 | 4139 | 23.23 |
| 4+ | 3953 | 22.18 |
| Frequency of consultations with usual psychiatrist g | ||
| 0 | 14,839 | 83.28 |
| 1–3 | 1347 | 7.56 |
| 4+ | 1633 | 9.16 |
| High continuity of physician care from both usual GP and psychiatrist (≥0.80) h | 7823 | 43.90 |
| Frequency of psychosocial interventions received in community healthcare centers (excluding GP consultations) i | ||
| 0 | 10,999 | 61.73 |
| 1–3 | 3523 | 19.77 |
| 4+ | 3297 | 18.50 |
| Frequency of interventions received in any treatment programattended for SRD in addiction treatment centers j | ||
| 0 | 12,811 | 71.90 |
| 1–3 | 1523 | 8.55 |
| 4+ | 3485 | 19.56 |
| Percentage of patient dropouts from any SRD program in addiction treatment centers (2009–2010 to 2014–2015) k | ||
| Low (0 to 33%) | 6867 | 38.54 |
| Median (34 to 66%) | 3800 | 21.33 |
| High (67 to 100%) | 7152 | 40.14 |
| Outcomes (2015–2016) | ||
| Frequent ED use (3+ visits) for any medical reason l | 3221 | 18.08 |
| Hospitalization for any medical reason | 3018 | 16.94 |
| Frequent ED Use (3+) | Hospitalization | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | p-Value | 95% CI | OR | p-Value | 95% CI | |||
| Sociodemographic characteristics (2015–2016 or in the most recent year) | ||||||||
| Women (ref.: men) | 1.14 | 0.005 | 1.04 | 1.26 | ||||
| Age group (ref.: 45+ years) | ||||||||
| 12–17 | 1.47 | 0.001 | 1.17 | 1.86 | ||||
| 18–24 | 1.37 | <0.001 | 1.18 | 1.58 | ||||
| 25–44 | 1.10 | 0.065 | 0.99 | 1.22 | ||||
| Material Deprivation Index (ref.: 1 and 2) a | ||||||||
| 3 | 1.05 | 0.468 | 0.92 | 1.21 | ||||
| 4, 5, and not assigned | 1.29 | <0.001 | 1.16 | 1.43 | ||||
| Type of residential area (ref.: urban (>100,000)) | ||||||||
| Semi-urban (10,000 to 100,000) | 0.80 | <0.001 | 0.72 | 0.89 | 1.13 | 0.023 | 1.02 | 1.25 |
| Rural (<10,000) | 1.17 | 0.008 | 1.04 | 1.31 | 1.23 | 0.001 | 1.09 | 1.38 |
| History of homelessness (2009–2010 to 2015–2016) | 1.50 | <0.001 | 1.34 | 1.68 | 1.22 | 0.001 | 1.08 | 1.38 |
| Clinical characteristics (2012–2013 to 2015–2016) | ||||||||
| Type of SRD (exclusive groups, ref.: cannabis-related disorders only) | ||||||||
| Alcohol only | 1.20 | 0.138 | 0.94 | 1.52 | 1.33 | 0.016 | 1.05 | 1.68 |
| Drugs other than cannabis only | 1.61 | <0.001 | 1.24 | 2.08 | 1.03 | 0.823 | 0.78 | 1.36 |
| Polysubstance | 1.83 | <0.001 | 1.48 | 2.26 | 1.59 | <0.001 | 1.28 | 1.97 |
| Suicidal behaviors (suicide ideation or attempt) | 3.57 | <0.001 | 3.24 | 3.95 | 2.53 | <0.001 | 2.28 | 2.81 |
| Chronic physical illnesses (Elixhauser comorbidity index (ref.: 0)) b | ||||||||
| 1 | 1.77 | <0.001 | 1.50 | 2.10 | 2.21 | <.001 | 1.87 | 2.61 |
| 2 | 1.98 | <0.001 | 1.69 | 2.32 | 2.88 | <0.001 | 2.47 | 3.36 |
| 3+ | 5.23 | <0.001 | 4.45 | 6.15 | 11.64 | <0.001 | 9.88 | 13.72 |
| SRD only or with co-occurring disorders (exclusive groups, ref.: SRD only) | ||||||||
| Co-occurring SRD-mental disorders (MD) only | 1.93 | <0.001 | 1.63 | 2.28 | 1.93 | <0.001 | 1.59 | 2.34 |
| Co-occurring SRD-chronic physical illnesses only | 1.46 | 0.002 | 1.14 | 1.86 | 1.82 | <0.001 | 1.42 | 2.34 |
| Co-occurring SRD-MD-chronic physical illnesses | 2.77 | <0.001 | 2.31 | 3.33 | 2.89 | <0.001 | 2.36 | 3.54 |
| Outpatient service use characteristics (within 12 months prior to third ED visit or first hospitalization in 2015–2016, or other if specified) c | ||||||||
| Usual outpatient physician (ref.: no usual physician) d | ||||||||
| Usual general practitioner (GP) only | 1.39 | <0.001 | 1.19 | 1.61 | 1.39 | <0.001 | 1.18 | 1.63 |
| Usual psychiatrist only | 1.74 | <0.001 | 1.43 | 2.12 | 2.64 | <0.001 | 2.16 | 3.22 |
| Both usual GP and psychiatrist | 1.56 | <0.001 | 1.31 | 1.87 | 1.76 | <0.001 | 1.46 | 2.11 |
| High continuity of physician care score from both usual GP and psychiatrist (≥0.80) e | 0.73 | <0.001 | 0.64 | 0.84 | 0.80 | 0.002 | 0.69 | 0.92 |
| Frequency of psychosocial interventions received in community healthcare centers (excluding GP consultations) (ref.: 0) f | ||||||||
| 1–3 | 1.62 | <0.001 | 1.46 | 1.80 | 1.31 | <0.001 | 1.17 | 1.47 |
| 4+ | 1.77 | <0.001 | 1.59 | 1.97 | 1.52 | <0.001 | 1.36 | 1.70 |
| Percentage of patient dropouts from any SRD program in addiction treatment centers (2009–2010 to 2014–2015) (ref.: low (0 to 33%)) g | ||||||||
| Median (34 to 66%) | 1.30 | <0.001 | 1.16 | 1.45 | 1.11 | 0.091 | 0.98 | 1.24 |
| High (67 to 100%) | 1.25 | <0.001 | 1.13 | 1.38 | 1.04 | 0.428 | 0.94 | 1.16 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fleury, M.-J.; Cao, Z.; Grenier, G.; Huỳnh, C. Predictors of Frequent Emergency Department Use and Hospitalization among Patients with Substance-Related Disorders Recruited in Addiction Treatment Centers. Int. J. Environ. Res. Public Health 2022, 19, 6607. https://doi.org/10.3390/ijerph19116607
Fleury M-J, Cao Z, Grenier G, Huỳnh C. Predictors of Frequent Emergency Department Use and Hospitalization among Patients with Substance-Related Disorders Recruited in Addiction Treatment Centers. International Journal of Environmental Research and Public Health. 2022; 19(11):6607. https://doi.org/10.3390/ijerph19116607
Chicago/Turabian StyleFleury, Marie-Josée, Zhirong Cao, Guy Grenier, and Christophe Huỳnh. 2022. "Predictors of Frequent Emergency Department Use and Hospitalization among Patients with Substance-Related Disorders Recruited in Addiction Treatment Centers" International Journal of Environmental Research and Public Health 19, no. 11: 6607. https://doi.org/10.3390/ijerph19116607
APA StyleFleury, M.-J., Cao, Z., Grenier, G., & Huỳnh, C. (2022). Predictors of Frequent Emergency Department Use and Hospitalization among Patients with Substance-Related Disorders Recruited in Addiction Treatment Centers. International Journal of Environmental Research and Public Health, 19(11), 6607. https://doi.org/10.3390/ijerph19116607






