Shared Decision Making with Acutely Hospitalized, Older Poly-Medicated Patients: A Mixed-Methods Study in an Emergency Department
Abstract
:1. Introduction
2. Materials and Methods
2.1. Objectives
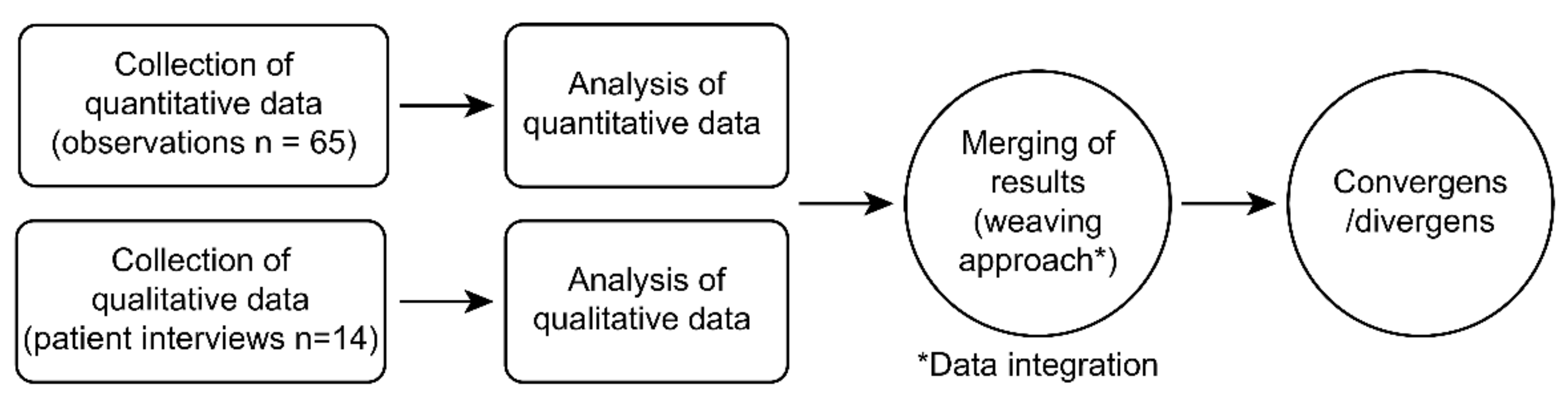
2.2. Study Design
2.3. Setting
2.4. Ethical Considerations
2.5. Quantitative Data
2.6. Quantitative Data Collections
2.6.1. Participants
2.6.2. Observing Patient Involvement Measurement (OPTION 5)
2.7. Quantitative Analysis and Statistics
2.8. Qualitative Data
2.9. Qualitative Data Collection
2.9.1. Participants
2.9.2. Semi-Structured Interviews
2.10. Qualitative Analysis
Thematic Analysis
2.11. Integration of Data
3. Results
3.1. Participants
3.2. Quantitative Results Presenting Option 5 and Items’ Scores
3.3. Integrating Quantitative and Qualitative Data
3.4. Overall Themes including Both Quantitative and Qualitative Data
- A low degree of SDM in conversations about medicine.
- A variation in the pro-active and non-active patient approach to conversations about medicine.
- No information on side effects.
- A preference for medication reduction.
3.4.1. Theme 1: A Low Degree of SDM in Conversations about Medicine in the ED
“No, I don’t think so, but it appeared we should hurry, I’m not sure, I’m not sure. [……….] No, I didn’t think we were talking about medicine, at all, but it is possible I was a little dazed when I first came in” (Pt ID #16).
Interviewer: “When you were in the Emergency Department, did anyone discuss your medication with you?” Patient: “No, they have everything in writing, so there is nothing to discuss. They simply glance at their screens to know what you get and don’t get” (Pt ID #2).
3.4.2. Theme 2: A Variation in the Pro-Active and Non-Active Patients’ Approach to Conversations about Medicine
“Yes, indeed, I believe I was engaged because they listened and heard what I had to say. I communicated my dissatisfaction and worry with the situation and my attitude toward it (the medicine). To me, it’s natural” (Pt ID #21).
“I’ve only just picked up on what was said to me. That is something I have to admit. I presume that the physicians who have dealt with me in the situations, that they are most familiar with what is the best. So, with what is required, I replied: “Yes, thank you.” But because I have no sense of medicine, I hear what the experts say to me, right?” (Pt ID #19).
“Well, it (involvement) would be wonderful for someone who does not have much control over it and is, if I may say so, gullible” (Pt ID #17).
“No, I don’t want to get involved, but the day when I am unable to care for myself, I would like to be involved in my medication” (Pt ID #5).
“I just got home, and my medicine says right here (on the medicine list) Losartan, which is the blood pressure medication I take once a day. The patient examines the medicine list attentively and states: It does not say whether it is for the blood pressure to rise or fall? I’m not sure of that” (Pt ID #11).
“Well, I care a lot, and I’ll try to follow what I get of medicine, and I can be skeptical if I get another medicine because if I was feeling fine with one, why suddenly switch to another? And yes, it does matter that I get involved in it. If not, I’ll look it up on the Internet myself if I don’t get clear information from the doctor. So, you can do that, and I will do it, or I get help from my grandson because I think they were terrible at informing people about it” (Pt ID #12).
3.4.3. Theme 3: No Information on Side Effects
“You see, I have such a fluctuating blood sugar and blood pressure, and the blood pressure is often too low, and in the last weeks I fell, so I have been extremely anxious about receiving too much medicine. It lowers my blood pressure” (Pt ID #21).
“No, that has not been discussed. They haven’t discussed it at all. But I guess they know what’s wrong with me and have looked into it” (Pt ID #5).
3.4.4. Theme 4: A Preference for Medication Reduction
“So, I think it would be nice if they inquired about your medication’s status. But then you have the thought in the back of your head that, uhh, they are so busy, they don’t have time [……].It would be wonderful if they asked if everything is OK with the medication you are receiving. Is there anything else you think should be changed? That would have been fantastic in my opinion” (Pt ID #17).
“You know what, I do not have much time left, so I don’t want to get involved. But I hope that what I get is something that will benefit me in some way. I assume that the physicians have examined everything and that I receive only what I require and nothing else” (Pt ID #2).
Interviewer: “But would you like to take less medicine?”
Patient: “Yes, in a way, because there are usually some side effects, and I experienced dizziness and they reduced the diuretics, because I became so dizzy” (Pt ID #2).
4. Discussion
Methodological Strength and Limitations
5. Conclusions
Implication for Healthcare Professionals
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Steffensen, K.D.; Hjelholt Baker, V.; Vinter, M.M. Implementing Shared Decision Making in Denmark: First Steps and Future Focus Areas. Z. Evid. Qual. Gesundhwes. 2017, 123–124, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Coulter, A. National Strategies for Implementing Shared Decision Making; Bertelsmann Foundation: Gütersloh, Germany, 2018. [Google Scholar]
- National Collaborating Centre for Primary Care (UK). Medicines Adherence: Involving Patients in Decisions about Prescribed Medicines and Supporting Adherence; National Institute for Health and Clinical Excellence: Guidance; Royal College of General Practitioners: London, UK, 2009. [Google Scholar]
- Barry, M.J.; Edgman-Levitan, S. Shared Decision Making—The Pinnacle of Patient-Centered Care. N. Engl. J. Med. 2012, 366, 780–781. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charles, C.; Gafni, A.; Whelan, T. Shared Decision-Making in the Medical Encounter: What Does It Mean? (Or It Takes at Least Two to Tango). Soc. Sci. Med. 1997, 44, 681–692. [Google Scholar] [CrossRef]
- Elwyn, G.; Durand, M.A.; Song, J.; Aarts, J.; Barr, P.J.; Berger, Z.; Cochran, N.; Frosch, D.; Galasiński, D.; Gulbrandsen, P.; et al. A Three-Talk Model for Shared Decision Making: Multistage Consultation Process. BMJ 2017, 359, j4891. [Google Scholar] [CrossRef] [Green Version]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What Is Polypharmacy? A Systematic Review of Definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Houlind, M.B.; Andersen, A.L.; Treldal, C.; Jørgensen, L.M.; Kannegaard, P.N.; Castillo, L.S.; Christensen, L.D.; Tavenier, J.; Rasmussen, L.J.H.; Ankarfeldt, M.Z.; et al. A Collaborative Medication Review Including Deprescribing for Older Patients in an Emergency Department: A Longitudinal Feasibility Study. J. Clin. Med. 2020, 9, 348. [Google Scholar] [CrossRef] [Green Version]
- Kantor, E.D.; Rehm, C.D.; Haas, J.S.; Chan, A.T.; Giovannucci, E.L. Trends in Prescription Drug Use Among Adults in the United States from 1999–2012. JAMA J. Am. Med. Assoc. 2015, 314, 1818–1830. [Google Scholar] [CrossRef]
- Morin, L.; Johnell, K.; Laroche, M.-L.; Fastbom, J.; Wastesson, J.W. The Epidemiology of Polypharmacy in Older Adults: Register-Based Prospective Cohort Study. CLEP 2018, 10, 289–298. [Google Scholar] [CrossRef] [Green Version]
- Vermunt, N.P.C.A.; Harmsen, M.; Westert, G.P.; Olde Rikkert, M.G.M.; Faber, M.J. Collaborative Goal Setting with Elderly Patients with Chronic Disease or Multimorbidity: A Systematic Review. BMC Geriatr. 2017, 17, 167. [Google Scholar] [CrossRef]
- Bunn, F.; Goodman, C.; Russell, B.; Wilson, P.; Manthorpe, J.; Rait, G.; Hodkinson, I.; Durand, M.-A. Supporting Shared Decision Making for Older People with Multiple Health and Social Care Needs: A Realist Synthesis. BMC Geriatr. 2018, 18, 165. [Google Scholar] [CrossRef]
- Durand, M.-A.; Carpenter, L.; Dolan, H.; Bravo, P.; Mann, M.; Bunn, F.; Elwyn, G. Do Interventions Designed to Support Shared Decision- Making Reduce Health Inequalities? A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e94670. [Google Scholar] [CrossRef] [Green Version]
- Coulter, A. Patient Engagement--What Works? J. Ambul. Care Manag. 2012, 35, 80–89. [Google Scholar] [CrossRef]
- Jansen, J.; Naganathan, V.; Carter, S.M.; McLachlan, A.J.; Nickel, B.; Irwig, L.; Bonner, C.; Doust, J.; Colvin, J.; Heaney, A.; et al. Too Much Medicine in Older People? Deprescribing through Shared Decision Making. BMJ 2016, 353, i2893. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffmann, T.; Jansen, J.; Glasziou, P. The Importance and Challenges of Shared Decision Making in Older People with Multimorbidity. PLoS Med. 2018, 15, e1002530. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Multimorbidity; Technical Series on Safer Primary Care; World Health Organization: Geneva, Switzerland, 2016; ISBN 978-92-4-151165-0. [Google Scholar]
- Flink, C.E.; Kehlet, K.H.; Gut, R.; Fuglsang, M. Inddragelse på Lige Fod—Oplevelser Med og Ønsker Til Inddragelse Blandt Socialt Sårbare Kræftpatienter; Kompetencecenter for Patientoplevelser: Frederiksberg, Denmark, 2017. (In Danish) [Google Scholar]
- Kaatmann, E. Inddragelse/Involvering i Behandlingen Af Diabetes—En Undersøgelse Om Mennesker Med Diabetes’ Ønsker Og Erfaringer Med Involvering/Inddragelse i Behandlingen Af Deres Diabetes; Bladtema om Inddragelse/Involvering; Diabetesforeningen: København, Denmark, 2017. (In Danish) [Google Scholar]
- Levinson, W.; Kao, A.; Kuby, A.; Thisted, R.A. Not All Patients Want to Participate in Decision Making. J. Gen. Intern. Med. 2005, 20, 531–535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weir, K.; Nickel, B.; Naganathan, V.; Bonner, C.; McCaffery, K.; Carter, S.M.; McLachlan, A.; Jansen, J. Decision-Making Preferences and Deprescribing: Perspectives of Older Adults and Companions About Their Medicines. J. Gerontol. Ser. B 2018, 73, e98–e107. [Google Scholar] [CrossRef] [PubMed]
- Miller, T.A. Health Literacy and Adherence to Medical Treatment in Chronic and Acute Illness: A Meta-Analysis. Patient Educ. Couns. 2016, 99, 1079–1086. [Google Scholar] [CrossRef] [Green Version]
- Flynn, D.; Knoedler, M.A.; Hess, E.P.; Murad, M.H.; Erwin, P.J.; Montori, V.M.; Thomson, R.G. Engaging Patients in Health Care Decisions in the Emergency Department Through Shared Decision-Making: A Systematic Review: Shared Decision-Making In the Ed. Acad. Emerg. Med. 2012, 19, 959–967. [Google Scholar] [CrossRef]
- Grudzen, C.R.; Anderson, J.R.; Carpenter, C.R.; Hess, E.P. The 2016 Academic Emergency Medicine Consensus Conference, Shared Decision Making in the Emergency Department: Development of a Policy-Relevant Patient-Centered Research Agenda May 10, 2016, New Orleans, LA. Acad. Emerg. Med. 2016, 23, 1313–1319. [Google Scholar] [CrossRef] [Green Version]
- Castaneda-Guarderas, A.; Glassberg, J.; Grudzen, C.R.; Ngai, K.M.; Samuels-Kalow, M.E.; Shelton, E.; Wall, S.P.; Richardson, L.D. Shared Decision Making With Vulnerable Populations in the Emergency Department. Acad. Emerg. Med. 2016, 23, 1410–1416. [Google Scholar] [CrossRef]
- Lindstroem, M.B.; Andersen, O.; Kallemose, T.; Rasmussen, L.J.H.; Rosthoej, S.; Jervelund, S.S. The Effect of the Employment of Consultants in the Emergency Department on Quality of Care and Equity—A Quasi-Experimental Retrospective Cohort Study; In Review; Research Square: Durham, NC, USA, 2019. [Google Scholar]
- Schoenfeld, E.M.; Goff, S.L.; Downs, G.; Wenger, R.J.; Lindenauer, P.K.; Mazor, K.M. A Qualitative Analysis of Patients’ Perceptions of Shared Decision Making in the Emergency Department: “Let Me Know I Have a Choice. Acad. Emerg. Med. 2018, 25, 716–727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eriksson-Liebon, M.; Roos, S.; Hellström, I. Patients’ Expectations and Experiences of Being Involved in Their Own Care in the Emergency Department: A Qualitative Interview Study. J. Clin. Nurs. 2021, 30, 1942–1952. [Google Scholar] [CrossRef] [PubMed]
- Fabricius, P.K.; Andersen, O.; Steffensen, K.D.; Kirk, J.W. The Challenge of Involving Old Patients with Polypharmacy in Their Medication during Hospitalization in a Medical Emergency Department: An Ethnographic Study. PLoS ONE 2021, 16, e0261525. [Google Scholar] [CrossRef] [PubMed]
- Scholl, I.; LaRussa, A.; Hahlweg, P.; Kobrin, S.; Elwyn, G. Organizational- and System-Level Characteristics That Influence Implementation of Shared Decision-Making and Strategies to Address Them—A Scoping Review. Implement. Sci. 2018, 13, 40. [Google Scholar] [CrossRef] [Green Version]
- Creswell, J.W. A Concise Introduction to Mixed Methods Research; SAGE Mixed Methods Research Series. SAGE: Thousand Oaks, CA, USA, 2015; ISBN 978-1-4833-5904-5. [Google Scholar]
- Fetters, M.D.; Molina-Azorin, J.F. A Checklist of Mixed Methods Elements in a Submission for Advancing the Methodology of Mixed Methods Research. J. Mix. Methods Res. 2019, 13, 414–423. [Google Scholar] [CrossRef]
- Barr, P.J.; O’Malley, A.J.; Tsulukidze, M.; Gionfriddo, M.R.; Montori, V.; Elwyn, G. The Psychometric Properties of Observer OPTION5, an Observer Measure of Shared Decision Making. Patient Educ. Couns. 2015, 98, 970–976. [Google Scholar] [CrossRef]
- Observer OPTION 5. 2014. Available online: http://www.glynelwyn.com/observer-option-5-2014.html (accessed on 19 January 2022).
- Couët, N.; Desroches, S.; Robitaille, H.; Vaillancourt, H.; Leblanc, A.; Turcotte, S.; Elwyn, G.; Légaré, F. Assessments of the Extent to Which Health-Care Providers Involve Patients in Decision Making: A Systematic Review of Studies Using the OPTION Instrument. Health Expect. 2015, 18, 542–561. [Google Scholar] [CrossRef]
- Translating Observer OPTION 5. Available online: http://www.glynelwyn.com/translating-observer-option-5.html (accessed on 2 January 2022).
- Kirkwood, B.R.; Sterne, J.A.C. Essential Medical Statistics, 2nd ed.; Blackwell Pub: Malden, MA, USA, 2003. [Google Scholar]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for Reporting Qualitative Research: A Synthesis of Recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef]
- Kvale, S.; Brinkmann, S. Interview: Introduktion Til et Håndværk, 2nd ed.; Hans Reitzel: Copenhague, Denmark, 2009; ISBN 978-87-412-5198-1. [Google Scholar]
- Elwyn, G.; Barr, P.J.; Grande, S.W.; Thompson, R.; Walsh, T.; Ozanne, E.M. Developing CollaboRATE: A Fast and Frugal Patient-Reported Measure of Shared Decision Making in Clinical Encounters. Patient Educ. Couns. 2013, 93, 102–107. [Google Scholar] [CrossRef] [Green Version]
- Willis, G.B.; Artino, A.R. What Do Our Respondents Think We’re Asking? Using Cognitive Interviewing to Improve Medical Education Surveys. J. Grad. Med. Educ. 2013, 5, 353–356. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.; Clarke, V. Reflecting on Reflexive Thematic Analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving Integration in Mixed Methods Designs—Principles and Practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef] [Green Version]
- Olling, K.; Stie, M.; Winther, B.; Steffensen, K.D. The Impact of a Patient Decision Aid on Shared Decision-making Behaviour in Oncology Care and Pulmonary Medicine—A Field Study Based on Real-life Observations. J. Eval. Clin. Pract. 2019, 25, 1121–1130. [Google Scholar] [CrossRef] [PubMed]
- Joseph-Williams, N.; Abhyankar, P.; Boland, L.; Bravo, P.; Brenner, A.T.; Brodney, S.; Coulter, A.; Giguere, A.; Hoffman, A.; Körner, M.; et al. What Works in Implementing Patient Decision Aids in Routine Clinical Settings? A Rapid Realist Review and Update from the International Patient Decision Aid Standards Collaboration. Med. Decis. Mak. 2020, 41, 0272989X20978208. [Google Scholar] [CrossRef]
- Stacey, D.; Légaré, F.; Lewis, K.; Barry, M.J.; Bennett, C.L.; Eden, K.B.; Holmes-Rovner, M.; Llewellyn-Thomas, H.; Lyddiatt, A.; Thomson, R.; et al. Decision Aids for People Facing Health Treatment or Screening Decisions. Cochrane Database Syst. Rev. 2017, 4. [Google Scholar] [CrossRef] [Green Version]
- Scalia, P.; Durand, M.-A.; Berkowitz, J.L.; Ramesh, N.P.; Faber, M.J.; Kremer, J.A.M.; Elwyn, G. The Impact and Utility of Encounter Patient Decision Aids: Systematic Review, Meta-Analysis and Narrative Synthesis. Patient Educ. Couns. 2019, 102, 817–841. [Google Scholar] [CrossRef]
- Savelberg, W.; Smidt, M.; Boersma, L.J.; van der Weijden, T. Elicitation of Preferences in the Second Half of the Shared Decision Making Process Needs Attention; a Qualitative Study. BMC Health Serv. Res. 2020, 20, 635. [Google Scholar] [CrossRef]
- Le Bosquet, K.; Barnett, N.; Minshull, J. Deprescribing: Practical Ways to Support Person-Centred, Evidence-Based Deprescribing. Pharmacy 2019, 7, 129. [Google Scholar] [CrossRef] [Green Version]
- Katz, M.G.; Jacobson, T.A.; Veledar, E.; Kripalani, S. Patient Literacy and Question-Asking Behavior During the Medical Encounter: A Mixed-Methods Analysis. J. Gen. Intern. Med. 2007, 22, 782–786. [Google Scholar] [CrossRef] [Green Version]
- Joseph-Williams, N.; Elwyn, G.; Edwards, A. Knowledge Is Not Power for Patients: A Systematic Review and Thematic Synthesis of Patient-Reported Barriers and Facilitators to Shared Decision Making. Patient Educ. Couns. 2014, 94, 291–309. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, C.U.; Kyriakidis, S.; Christensen, L.D.; Jacobsen, R.; Laursen, J.; Christensen, M.B.; Frølich, A. Medication-Related Experiences of Patients with Polypharmacy: A Systematic Review of Qualitative Studies. BMJ Open 2020, 10, e036158. [Google Scholar] [CrossRef] [PubMed]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Vest-Hansen, B.; Riis, A.H.; Christiansen, C.F. Registration of Acute Medical Hospital Admissions in the Danish National Patient Registry: A Validation Study. Clin. Epidemiol. 2013, 5, 129–133. [Google Scholar] [CrossRef] [Green Version]
| ID | Interview Telephone (T) or Home (H) | Sex (M/F) | Age (years) | Number of Medicines | Home Care or Kindship for Medicine Administration |
|---|---|---|---|---|---|
| 1 | H | M | 86 | 5 | No |
| 2 | T | F | 89 | 12 | Yes |
| 5 | T | F | 79 | 12 | No |
| 6 | T | F | 90 | 7 | Yes |
| 7 | T | M | 81 | 5 | Yes |
| 9 | T | F | 94 | 7 | No |
| 11 | T | M | 87 | 6 | No |
| 12 | T | F | 75 | 11 | Yes |
| 13 | T | F | 94 | 6 | Yes |
| 15 | T | M | 78 | 15 | Yes |
| 17 | T | F | 82 | 13 | No |
| 18 | T | M | 89 | 6 | No |
| 19 | T | F | 78 | 19 | No |
| 21 | T | M | 83 | 8 | Yes |
| Theme 1: Explore whether the patient recalls any medication-related conversations in the ED |
| 1. Opening Question: Do you recall speaking with anybody (physician, nurse, or pharmacist) about your medication during your ED stay? |
| 2. How did you feel about the medication conversations in the ED? |
| 3. How did you experience being part of the decision-making process for your medication? |
| Theme 2: Examine the patient’s experience of being engaged in medication choices in the ED |
| 4. What are your thoughts on being (or not being) involved, in the way that you did? |
| 5. When it comes to your medicine, what is the most crucial thing for you to be engaged in? |
| 6. How would you rather make decisions about your medicine? |
| Theme 3: Examine to see if the patient experienced SDM in conversations with the healthcare professionals about medicine (the Collaborate questionnaire inspired the following three questions) |
| 7. How did you feel about the healthcare professionals’ efforts to explain your medicine to you? |
| 8. How did you feel about the healthcare professionals’ efforts to understand what was most important to you in your medication? |
| 9. How was the impression of the effort made to incorporate what matters most to you in your future medication? |
| Characteristics | Observations Healthcare Professionals, n = 31 (Quantitative) | Interview Patients, n = 14 (Qualitative) |
|---|---|---|
| Women, n (%) | 18 (58.1) | 8 (57.1) |
| Men, n (%) | 13 (41.9) | 6 (42.9) |
| Experiences, mean (years) | 14.7 | - |
| Age mean (years) | 41.2 (range 26–65) | 84.6 (range 75–94) |
| Number of medications, mean | - | 9.4 |
| Item # | Behavior | Score | |||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | Mean | ||
| 1. Presenting options | For the health issue being discussed, the clinician draws attention to or confirms that alternate treatment or management options exist or that the need for a decision exists. If the patient rather than the clinician draws attention to the availability of options, the clinician responds by agreeing that the options need deliberation. | 41 | 16.5 | 4.5 | 3 | 0 | 0.53 |
| 2. Establishing a partnership with the patient | The clinician reassures the patient or reaffirms that the clinician will support the patient to become informed or deliberate about the options. If the patient states that they have sought or obtained information prior to the encounter, the clinician supports such a deliberation process. | 61 | 0 | 1 | 3 | 0 | 0.17 |
| 3. Describing pros and cons of options | The clinician gives information or checks understanding about the options that are considered reasonable (this can include taking no action), to support the patient in comparing alternatives. If the patient requests clarification, the clinician supports the process. | 51 | 8 | 3 | 2 | 1 | 0.37 |
| 4. Eliciting patient preferences | The clinician makes an effort to elicit the patient’s preferences in response to the options that have been described. If the patient declares their preference(s), the clinician is supportive. | 51 | 5 | 5 | 2 | 1 | 0.38 |
| 5. Integrating patient preferences into the decision | The clinician makes an effort to integrate the patient’s elicited preferences as decisions are made. If the patient indicates how best to integrate their preferences as decisions are made, the clinician makes an effort to do so. | 58.5 | 1.5 | 4 | 1 | 0 | 0.19 |
| Total OPTION 5 score: Summed for all 5 items | 1.64 | ||||||
| Total OPTION 5 score: Rescaled to 0–100 | 8.2 | ||||||
| Qualitative Findings’ Initial Themes | Meta-Inferences | Quantitative Findings’ OPTION 5 Score and Item Points | Confirmation, Discordance, or Expansion from Findings |
|---|---|---|---|
| Sparse communication about medicine in the ED | Theme 1: A low degree of SDM in conversations about medicine in the ED Most patients had not experienced much communication about their medicine and were not even aware that they could have different medicine options. | Total mean score: 8.2 (out of 100) | Confirmation Each analysis confirms that there is sparse SDM and communication about medicine in the ED. |
| Power disparities prevent dialogues about medicine | Theme 2: A variation in the pro-active and non-active patients’ approach to conversations about medicine Some pro-active patients were very much involved in decisions about their medicine in contrast to the non-active patients who were divided into two sub-groups. Some patients preferred to leave decisions to the healthcare professionals. The other sub-group was afraid of revealing that they were not in control of their medicine. | Item 2: Establishing a partnership with the patient (Mean points: 0.17) + Item 3: Describing pros and cons of options (Mean points: 0.37) | Expansion We found a variation between the pro-active and non-active patients’ approach, which influenced how much information and involvement the patient received and how satisfied they were with the information and involvement. |
| Talk about side effects | Theme 3: No information of side effects Most patients had preferences for more discussions about side effects, but this was rarely discussed or asked for. The low score on Item 4: Eliciting patient preferences also reflects that the healthcare professionals rarely investigate patients’ preferences, which also are reflected in theme 4. | Item 4: Eliciting patient preferences (Mean points: 0.38) | Discordance There are discordant findings in the two analyses because the Item 4 score is low (Mean 0.38), reflecting that the healthcare professionals rarely investigate patient preferences. However, older poly-medicated patients have preferences for more discussions and information of side effects and the option of reducing medicine, as do the non-active patients, even though they do not ask for it themselves. |
| Preferences for deprescribing | Theme 4: A preference for medication reduction Most patients preferred to take less medicine, but this option was rarely discussed (which also was reflected in the low Item 4 score) unless the pro-active patients asked for it themselves. For non-active patients, they lacked the desire to engage actively in decision making because of vulnerability and limited life horizon, so they had to put trust in their medicine and felt that there was no other choice. |
| Mean | SD | Median | Lower IQR | Upper IQR | |
|---|---|---|---|---|---|
| Total score | 8.2 | 16.2 | 0.0 | 0.0 | 5.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fabricius, P.K.; Aharaz, A.; Stefánsdóttir, N.T.; Houlind, M.B.; Steffensen, K.D.; Andersen, O.; Kirk, J.W. Shared Decision Making with Acutely Hospitalized, Older Poly-Medicated Patients: A Mixed-Methods Study in an Emergency Department. Int. J. Environ. Res. Public Health 2022, 19, 6429. https://doi.org/10.3390/ijerph19116429
Fabricius PK, Aharaz A, Stefánsdóttir NT, Houlind MB, Steffensen KD, Andersen O, Kirk JW. Shared Decision Making with Acutely Hospitalized, Older Poly-Medicated Patients: A Mixed-Methods Study in an Emergency Department. International Journal of Environmental Research and Public Health. 2022; 19(11):6429. https://doi.org/10.3390/ijerph19116429
Chicago/Turabian StyleFabricius, Pia Keinicke, Anissa Aharaz, Nina Thórný Stefánsdóttir, Morten Baltzer Houlind, Karina Dahl Steffensen, Ove Andersen, and Jeanette Wassar Kirk. 2022. "Shared Decision Making with Acutely Hospitalized, Older Poly-Medicated Patients: A Mixed-Methods Study in an Emergency Department" International Journal of Environmental Research and Public Health 19, no. 11: 6429. https://doi.org/10.3390/ijerph19116429
APA StyleFabricius, P. K., Aharaz, A., Stefánsdóttir, N. T., Houlind, M. B., Steffensen, K. D., Andersen, O., & Kirk, J. W. (2022). Shared Decision Making with Acutely Hospitalized, Older Poly-Medicated Patients: A Mixed-Methods Study in an Emergency Department. International Journal of Environmental Research and Public Health, 19(11), 6429. https://doi.org/10.3390/ijerph19116429






