The Relationship between Phase Angle, Nutrition Status, and Complications in Patients with Pancreatic Head Cancer
Abstract
1. Introduction
2. Methods
2.1. Subjects
2.2. Nutritional Assessment
2.3. Anthropometric and Bioelectrical Impedance Analysis Measurements
2.4. Clinical Outcomes
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
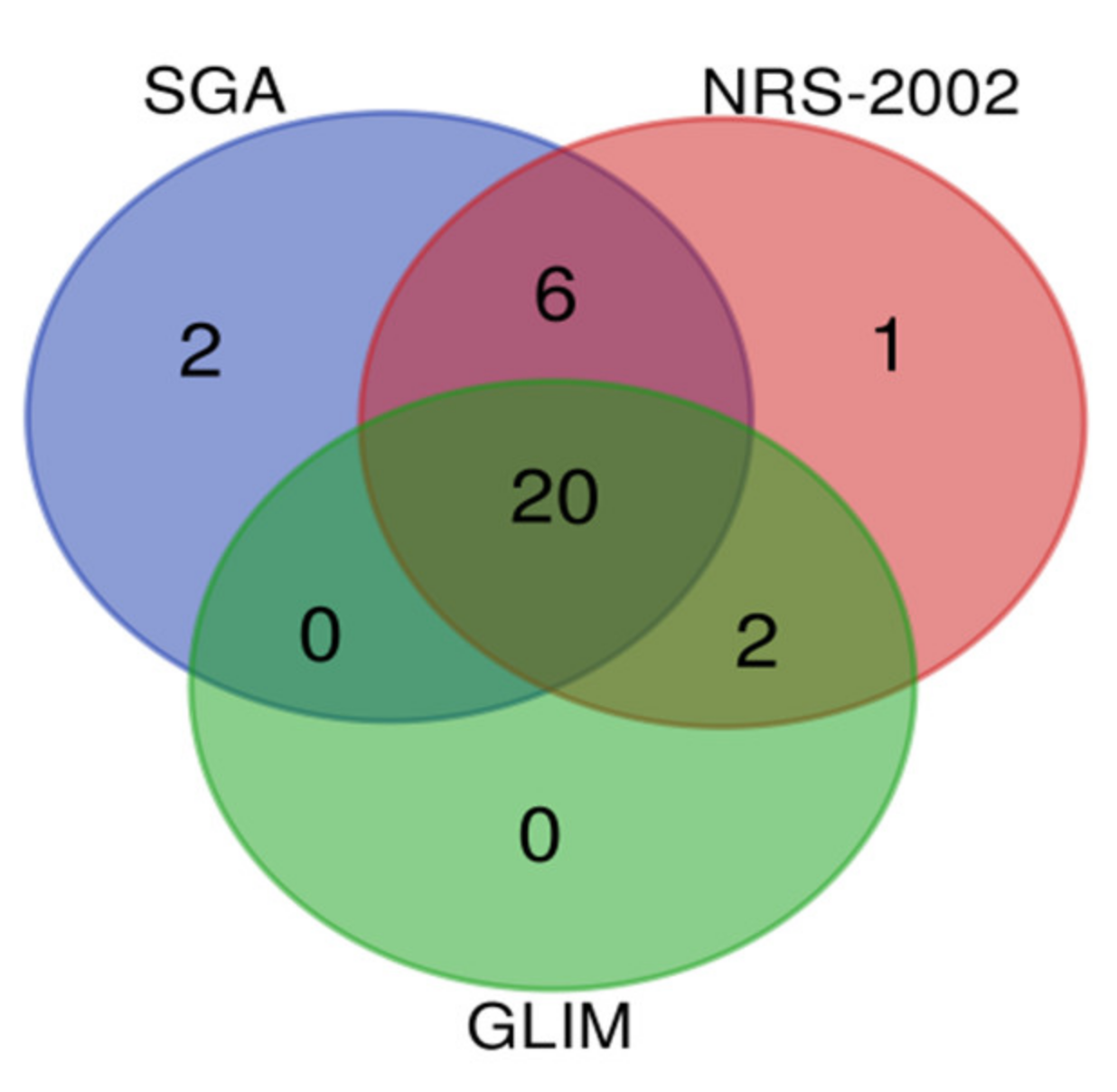
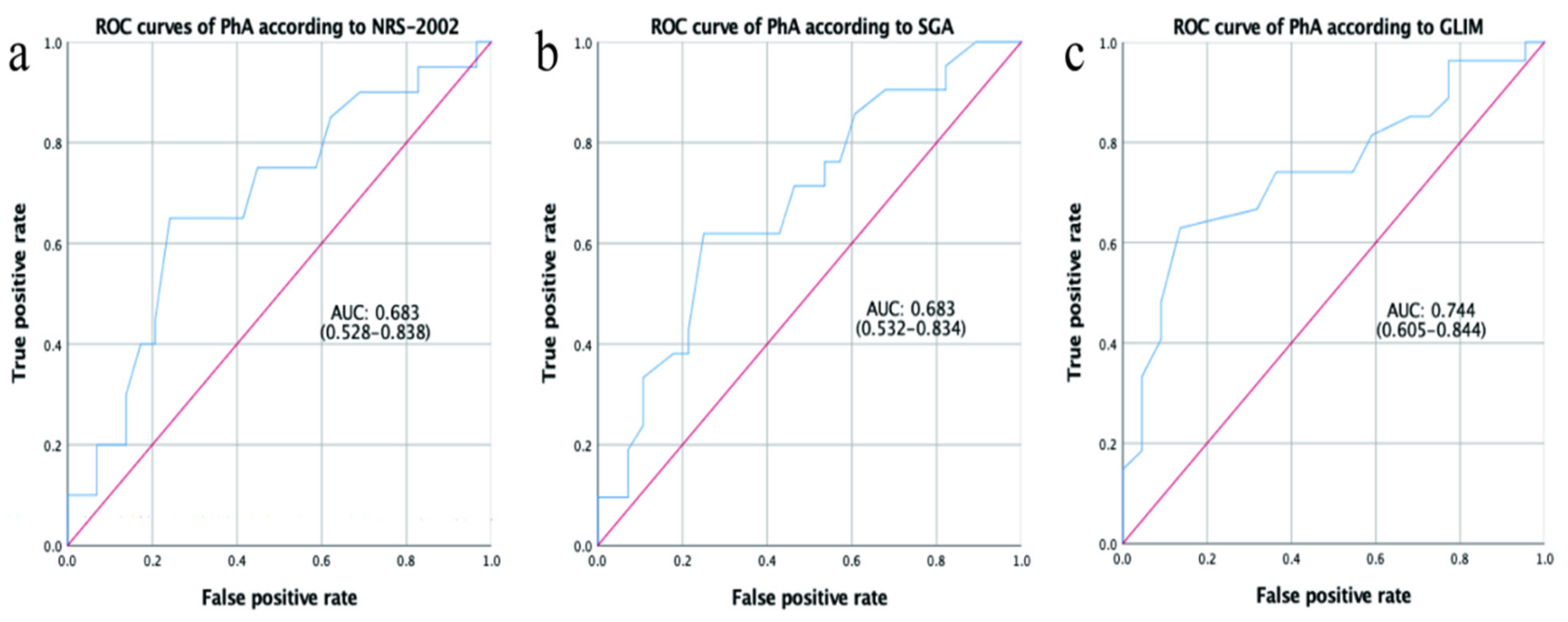
3.2. Association between PhA and Nutritional Status
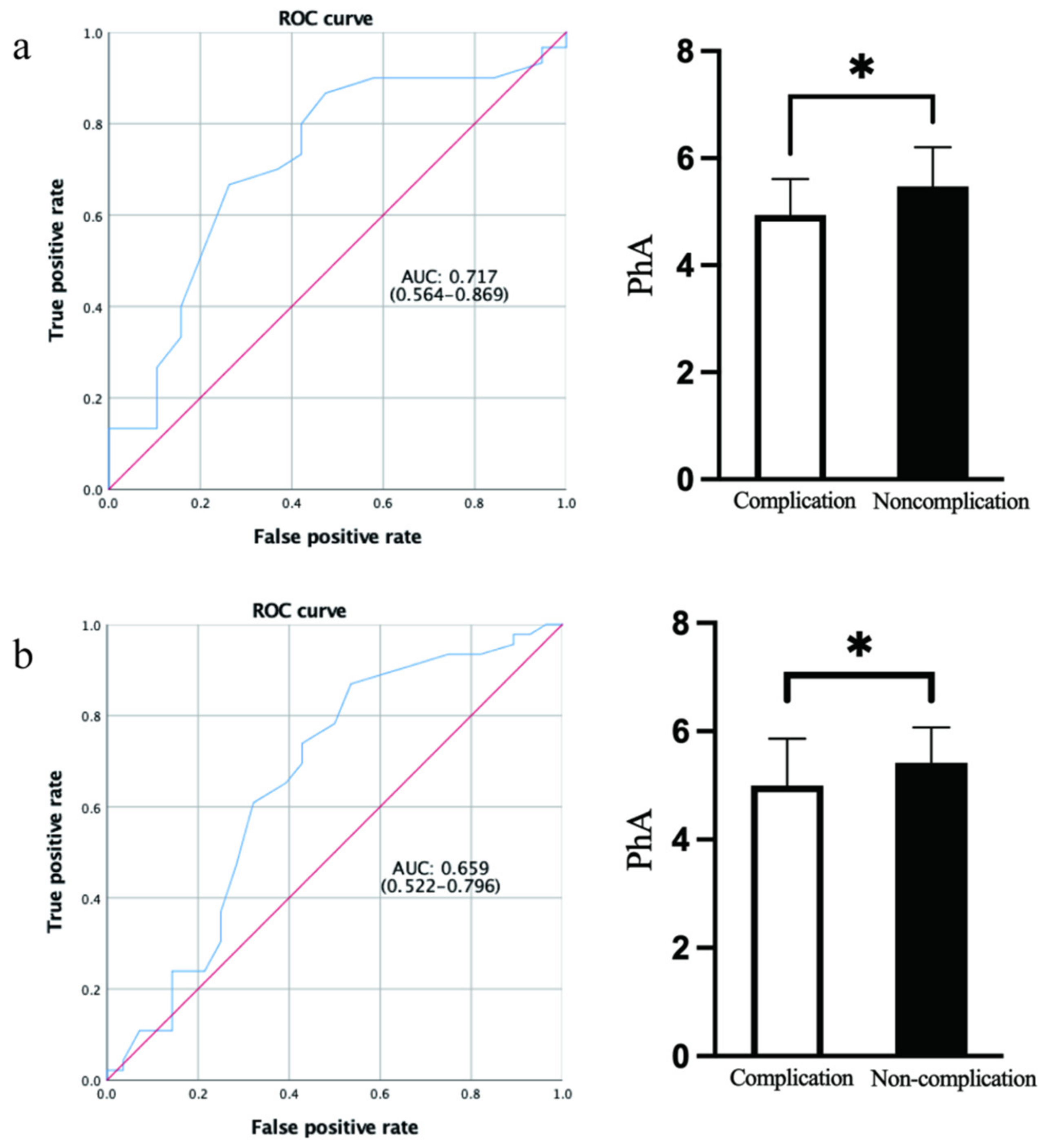
3.3. Association between PhA, Nutritional Status, and Complications
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mizrahi, J.D.; Surana, R.; Valle, J.W.; Shroff, R.T. Pancreatic cancer. Lancet 2020, 395, 2008–2020. [Google Scholar] [CrossRef]
- Gilliland, T.M.; Villafane-Ferriol, N.; Shah, K.P.; Shah, R.M.; Tran Cao, H.S.; Massarweh, N.N.; Silberfein, E.J.; Choi, E.A.; Hsu, C.; McElhany, A.L.; et al. Nutritional and Metabolic Derangements in Pancreatic Cancer and Pancreatic Resection. Nutrients 2017, 9, 243. [Google Scholar] [CrossRef] [PubMed]
- La Torre, M.; Ziparo, V.; Nigri, G.; Cavallini, M.; Balducci, G.; Ramacciato, G. Malnutrition and pancreatic surgery: Prevalence and outcomes. J. Surg. Oncol. 2013, 107, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Kondrup, J.; Allison, S.P.; Elia, M.; Vellas, B.; Plauth, M. ESPEN guidelines for nutrition screening 2002. Clin. Nutr. 2003, 22, 415–421. [Google Scholar] [CrossRef]
- Baccaro, F.; Moreno, J.B.; Borlenghi, C.; Aquino, L.; Armesto, G.; Plaza, G.; Zapata, S. Subjective Global Assessment in the Clinical Setting. J. Parenter. Enter. Nutr. 2007, 31, 406–409. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; de Baptista, G.A.; Barazzoni, R.; Blaauw, R.; Coats, A.J.S.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2018, 43, 32–40. [Google Scholar]
- Hamada, Y. Objective Data Assessment (ODA) Methods as Nutritional Assessment Tools. J. Med. Investig. 2015, 62, 119–122. [Google Scholar] [CrossRef][Green Version]
- Mazzoccoli, G. Body composition: Where and when. Eur. J. Radiol. 2016, 85, 1456–1460. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; de Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gomez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.-C.; Pirlich, M.; et al. Bioelectrical impedance analysis—Part I: Review of principles and methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef]
- Pirlich, M.; Schutz, T.; Spachos, T.; Ertl, S.; Weiss, M.L.; Lochs, H.; Plauth, M. Bioelectrical impedance analysis is a useful bedside technique to assess malnutrition in cirrhotic patients with and without ascites. Hepatology 2000, 32, 1208–1215. [Google Scholar] [CrossRef]
- Norman, K.; Stobaus, N.; Pirlich, M.; Bosy-Westphal, A. Bioelectrical phase angle and impedance vector analysis—Clinical relevance and applicability of impedance parameters. Clin. Nutr. 2012, 31, 854–861. [Google Scholar] [CrossRef] [PubMed]
- Mulasi, U.; Kuchnia, A.J.; Cole, A.J.; Earthman, C.P. Bioimpedance at the bedside: Current applications, limitations, and opportunities. Nutr. Clin. Pract. 2015, 30, 180–193. [Google Scholar] [CrossRef]
- Ruiz-Margain, A.; Macias-Rodriguez, R.U.; Duarte-Rojo, A.; Rios-Torres, S.L.; Espinosa-Cuevas, A.; Torre, A. Malnutrition assessed through phase angle and its relation to prognosis in patients with compensated liver cirrhosis: A prospective cohort study. Dig. Liver Dis. 2015, 47, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Yasui-Yamada, S.; Oiwa, Y.; Saito, Y.; Aotani, N.; Matsubara, A.; Matsuura, S.; Tanimura, M.; Tani-Suzuki, Y.; Kashihara, H.; Nishi, M.; et al. Impact of phase angle on postoperative prognosis in patients with gastrointestinal and hepatobiliary-pancreatic cancer. Nutrition 2020, 79–80, 110891. [Google Scholar] [CrossRef] [PubMed]
- Anonymous. The Bulletin of the American College of Surgeons: Keeping fellows informed for nearly 100 years. Bull. Am. Coll. Surg. 2012, 97, 17–43. [Google Scholar]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Poulia, K.A.; Sarantis, P.; Antoniadou, D.; Koustas, E.; Papadimitropoulou, A.; Papavassiliou, A.G.; Karamouzis, M.V. Pancreatic Cancer and Cachexia—Metabolic Mechanisms and Novel Insights. Nutrients 2020, 12, 1543. [Google Scholar] [CrossRef]
- Santos, I.; Mendes, L.; Mansinho, H.; Santos, C.A. Nutritional status and functional status of the pancreatic cancer patients and the impact of adjacent symptoms. Clin. Nutr. 2021, 40, 5486–5493. [Google Scholar] [CrossRef]
- Ward, L.C. Bioelectrical impedance analysis for body composition assessment: Reflections on accuracy, clinical utility, and standardisation. Eur. J. Clin. Nutr. 2019, 73, 194–199. [Google Scholar] [CrossRef]
- Sergi, G.; de Rui, M.; Stubbs, B.; Veronese, N.; Manzato, E. Measurement of lean body mass using bioelectrical impedance analysis: A consideration of the pros and cons. Aging Clin. Exp. Res. 2017, 29, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Varan, H.D.; Bolayir, B.; Kara, O.; Arik, G.; Kizilarslanoglu, M.C.; Kilic, M.K.; Sumer, F.; Kuyumcu, M.E.; Yesil, Y.; Yavuz, B.B.D.; et al. Phase angle assessment by bioelectrical impedance analysis and its predictive value for malnutrition risk in hospitalized geriatric patients. Aging Clin. Exp. Res. 2016, 28, 1121–1126. [Google Scholar] [CrossRef] [PubMed]
- Player, E.L.; Morris, P.; Thomas, T.; Chan, W.Y.; Vyas, R.; Dutton, J.; Tang, J.; Alexandre, L.; Forbes, A. Bioelectrical impedance analysis (BIA)-derived phase angle (PA) is a practical aid to nutritional assessment in hospital in-patients. Clin. Nutr. 2019, 38, 1700–1706. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, I.C.R.; Aredes, M.A.; Chaves, G.V. Applicability of the direct parameters of bioelectrical impedance in assessing nutritional status and surgical complications of women with gynecological cancer. Eur. J. Clin. Nutr. 2017, 71, 1278–1284. [Google Scholar] [CrossRef] [PubMed]
- Souza, N.C.; Avesani, C.M.; Prado, C.M.; Martucci, R.B.; Rodrigues, V.D.; de Pinho, N.B.; Heymsfield, S.B.; Gonzalez, M.C. Phase angle as a marker for muscle abnormalities and function in patients with colorectal cancer. Clin. Nutr. 2021, 40, 4799–4806. [Google Scholar] [CrossRef] [PubMed]
- Do Amaral Paes, T.C.; de Oliveira, K.C.C.; de Carvalho Padilha, P.; Peres, W.A.F. Phase angle assessment in critically ill cancer patients: Relationship with the nutritional status, prognostic factors and death. J. Crit. Care 2018, 44, 430–435. [Google Scholar] [CrossRef]
- Gupta, D.; Lis, C.G.; Dahlk, S.L.; King, J.; Vashi, P.G.; Grutsch, J.F.; Lammersfeld, C.A. The relationship between bioelectrical impedance phase angle and subjective global assessment in advanced colorectal cancer. Nutr. J. 2008, 7, 19. [Google Scholar] [CrossRef]
- Korousic Seljak, B.; Mlakar Mastnak, D.; Mrevlje, Z.; Veninsek, G.; Rotovnik Kozjek, N. A multi-center survey on hospital malnutrition and cachexia in Slovenia. Eur. J. Clin. Nutr. 2020, 74, 419–426. [Google Scholar] [CrossRef]
- Theilla, M.; Rattanachaiwong, S.; Kagan, I.; Rigler, M.; Bendavid, I.; Singer, P. Validation of GLIM malnutrition criteria for diagnosis of malnutrition in ICU patients: An observational study. Clin. Nutr. 2021, 40, 3578–3584. [Google Scholar] [CrossRef]
- Bosy-Westphal, A.; Danielzik, S.; Dorhofer, R.P.; Later, W.; Wiese, S.; Muller, M.J. Phase angle from bioelectrical impedance analysis: Population reference values by age, sex, and body mass index. JPEN J. Parenter. Enter. Nutr. 2006, 30, 309–316. [Google Scholar] [CrossRef]
- Kyle, U.G.; Genton, L.; Pichard, C. Low phase angle determined by bioelectrical impedance analysis is associated with malnutrition and nutritional risk at hospital admission. Clin. Nutr. 2013, 32, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Lukaski, H.C.; Kyle, U.G.; Kondrup, J. Assessment of adult malnutrition and prognosis with bioelectrical impedance analysis: Phase angle and impedance ratio. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Kang, J.S.; Han, Y.; Kim, H.; Kwon, W.; Kim, J.R.; Kim, S.-W.; Jang, J.-Y. Influence of preoperative nutritional status on clinical outcomes after pancreatoduodenectomy. HPB 2018, 20, 1051–1061. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Xiong, G.; Wang, X.; Peng, F.; Zhu, F.; Wang, M.; Qin, R. The Impact of Preoperative and Postoperative Malnutrition on Outcomes for Ampullary Carcinoma after Pancreaticoduodenectomy. Front. Oncol. 2021, 11, 748341. [Google Scholar] [CrossRef] [PubMed]
- Jablonska, B.; Pawlicki, K.; Mrowiec, S. Associations between Nutritional and Immune Status and Clinicopathologic Factors in Patients with Pancreatic Cancer: A Comprehensive Analysis. Cancers 2021, 13, 5041. [Google Scholar] [CrossRef]
- Probst, P.; Haller, S.; Bruckner, T.; Ulrich, A.; Strobel, O.; Hackert, T.; Diener, M.K.; Büchler, M.W.; Knebel, P. Prospective trial to evaluate the prognostic value of different nutritional assessment scores in pancreatic surgery (NURIMAS Pancreas). Br. J. Surg. 2017, 104, 1053–1062. [Google Scholar] [CrossRef]
- Lundberg, M.; Dickinson, A.; Nikander, P.; Orell, H.; Makitie, A. Low-phase angle in body composition measurements correlates with prolonged hospital stay in head and neck cancer patients. Acta Otolaryngol. 2019, 139, 383–387. [Google Scholar] [CrossRef]
- Uccella, S.; Mele, M.C.; Quagliozzi, L.; Rinninella, E.; Nero, C.; Cappuccio, S.; Cintonib, M.; Gasbarrinic, A.; Scambiaad, G.; Fagotti, A. Assessment of preoperative nutritional status using BIA-derived phase angle (PhA) in patients with advanced ovarian cancer: Correlation with the extent of cytoreduction and complications. Gynecol. Oncol. 2018, 149, 263–269. [Google Scholar] [CrossRef]
- Tzelnick, S.; Singer, P.; Shopen, Y.; Moshkovitz, L.; Fireman, S.; Shpitzer, T.; Mizrachi, A.; Bachar, G. Bioelectrical Impedance Analysis in Patients Undergoing Major Head and Neck Surgery: A Prospective Observational Pilot Study. J. Clin. Med. 2021, 10, 539. [Google Scholar] [CrossRef]
- Braga, M.; Capretti, G.; Pecorelli, N.; Balzano, G.; Doglioni, C.; Ariotti, R.; di Carlo, V. A prognostic score to predict major complications after pancreaticoduodenectomy. Ann. Surg. 2011, 254, 702–707, Discussion 7–8. [Google Scholar] [CrossRef]
- Sui, K.; Okabayshi, T.; Iwata, J.; Morita, S.; Sumiyoshi, T.; Iiyama, T.; Shimada, Y. Correlation between the skeletal muscle index and surgical outcomes of pancreaticoduodenectomy. Surg. Today 2018, 48, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Silva, M.C.; Barros, A.J.; Wang, J.; Heymsfield, S.B.; Pierson, R.N., Jr. Bioelectrical impedance analysis: Population reference values for phase angle by age and sex. Am. J. Clin. Nutr. 2005, 82, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Dutt, A.; Hemraj, S.; Bhat, S.; Manipadybhima, B. Phase Angle Measurement in Healthy Human Subjects through Bio-Impedance Analysis. Iran. J. Basic Med. Sci. 2012, 15, 1180–1184. [Google Scholar] [PubMed]
- Farias, C.L.; Campos, D.J.; Bonfin, C.M.; Vilela, R.M. Phase angle from BIA as a prognostic and nutritional status tool for children and adolescents undergoing hematopoietic stem cell transplantation. Clin. Nutr. 2013, 32, 420–425. [Google Scholar] [CrossRef]
- Pena, N.F.; Mauricio, S.F.; Rodrigues, A.M.S.; Carmo, A.S.; Coury, N.C.; Correia, M.; Generoso, S.V. Association Between Standardized Phase Angle, Nutrition Status, and Clinical Outcomes in Surgical Cancer Patients. Nutr. Clin. Pract. 2018, 34, 381–386. [Google Scholar] [CrossRef]

| Variable | Female | Male | p-Value |
|---|---|---|---|
| n = 18 | n = 31 | ||
| Age (years) | 57.61 ± 10.21 | 58.35 ± 11.98 | 0.826 |
| BMI (kg/m2) | 21.81 ± 2.77 | 22.35 ± 3.17 | 0.549 |
| PhA (°) | 4.97 ± 0.70 | 5.44 ± 0.73 | 0.035 |
| Total Body Water (kg) | 27.73 ± 4.68 | 35.75 ± 4.52 | <0.001 |
| Skeletal Muscle (kg) | 20.41 ± 3.78 | 27.02 ± 3.83 | <0.001 |
| Fat Free Mass (kg) | 37.78 ± 6.35 | 48.62 ± 6.14 | <0.001 |
| Fat Mass (kg) | 17.61 ± 6.04 | 16.25 ± 6.75 | 0.485 |
| Biceps circumference (cm) | 27.77 ± 2.72 | 29.46 ± 3.31 | 0.072 |
| ALB (g/L) | 40.78 ± 3.95 | 41.29 ± 5.00 | 0.711 |
| Days of Hospitalization (days) | 25.78 ± 15.99 | 25.71 ± 11.80 | 0.068 |
| Hospitalization Costs (CNY) | 99,665.67 ± 39,848.01 | 93,999.74 ± 21,012.52 | 0.157 |
| Variable | Spearman Correlation Coefficient | p-Value |
|---|---|---|
| Age (years) | −0.398 | 0.005 |
| BMI (kg/m2) | 0.325 | 0.023 |
| Biceps circumference (cm) | 0.422 | 0.003 |
| ALB (g/L) | 0.331 | 0.020 |
| Days of Hospitalization (days) | −0.146 | 0.317 |
| Hospitalization Costs (CNY) | −0.226 | 0.119 |
| Items | Malnourished | Well Nourished | p-Values |
|---|---|---|---|
| SGA | 5.07 ± 0.71 | 5.53 ± 0.73 | 0.032 |
| NRS-2002 | 5.09 ± 0.70 | 5.53 ± 0.75 | 0.043 |
| GLIM | 4.94 ± 0.61 | 5.53 ± 0.76 | 0.005 |
| Variable | Spearman Correlation Coefficient | p-Value |
|---|---|---|
| SGA | 0.314 | 0.028 |
| NRS-2002 | 0.312 | 0.029 |
| GLIM | 0.421 | 0.003 |
| Variable | Complications | No Complications | p-Values |
|---|---|---|---|
| n = 19 | n = 30 | ||
| Age (years) | 57.63 ± 11.79 | 58.37 ± 11.10 | 0.826 |
| PhA (°) | 4.94 ± 0.67 | 5.47 ± 0.73 | 0.013 |
| BMI (kg/m2) | 22.06 ± 2.99 | 22.21 ± 3.08 | 0.868 |
| Total body water (kg) | 32.85 ± 4.81 | 32.77 ± 6.69 | 0.965 |
| Skeletal muscle (kg) | 24.47 ± 3.97 | 24.66 ± 5.56 | 0.900 |
| Fat-Free Mass (kg) | 44.66 ± 6.51 | 44.62 ± 9.08 | 0.985 |
| Fat Mass (kg) | 17.02 ± 8.22 | 16.58 ± 5.21 | 0.820 |
| Biceps circumference (cm) | 28.79 ± 3.12 | 28.87 ± 3.28 | 0.930 |
| ALB (g/L) | 39.89 ± 5.05 | 41.87 ± 4.21 | 0.146 |
| Days of Hospitalization (days) | 35.84 ± 16.00 | 19.33 ± 5.06 | <0.001 |
| Hospitalization Expenses (CNY) | 119,924.05 ± 32,990.61 | 80,974.57 ± 12,017.24 | <0.001 |
| Items | Malnutrition | Complications in Malnutrition Group | χ2-Value | p-Value |
|---|---|---|---|---|
| NRS-2002 | 29 | 12 | 0.203 | 0.652 |
| SGA | 28 | 13 | 1.612 | 0.204 |
| GLIM | 22 | 10 | 0.750 | 0.386 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, S.; Yu, Z.; Shi, X.; Zhao, H.; Dai, M.; Chen, W. The Relationship between Phase Angle, Nutrition Status, and Complications in Patients with Pancreatic Head Cancer. Int. J. Environ. Res. Public Health 2022, 19, 6426. https://doi.org/10.3390/ijerph19116426
Zhou S, Yu Z, Shi X, Zhao H, Dai M, Chen W. The Relationship between Phase Angle, Nutrition Status, and Complications in Patients with Pancreatic Head Cancer. International Journal of Environmental Research and Public Health. 2022; 19(11):6426. https://doi.org/10.3390/ijerph19116426
Chicago/Turabian StyleZhou, Shengnan, Zhangping Yu, Xiaodong Shi, Huaiyu Zhao, Menghua Dai, and Wei Chen. 2022. "The Relationship between Phase Angle, Nutrition Status, and Complications in Patients with Pancreatic Head Cancer" International Journal of Environmental Research and Public Health 19, no. 11: 6426. https://doi.org/10.3390/ijerph19116426
APA StyleZhou, S., Yu, Z., Shi, X., Zhao, H., Dai, M., & Chen, W. (2022). The Relationship between Phase Angle, Nutrition Status, and Complications in Patients with Pancreatic Head Cancer. International Journal of Environmental Research and Public Health, 19(11), 6426. https://doi.org/10.3390/ijerph19116426





