Heatwave Mortality in Summer 2020 in England: An Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Heatwave Definitions Used
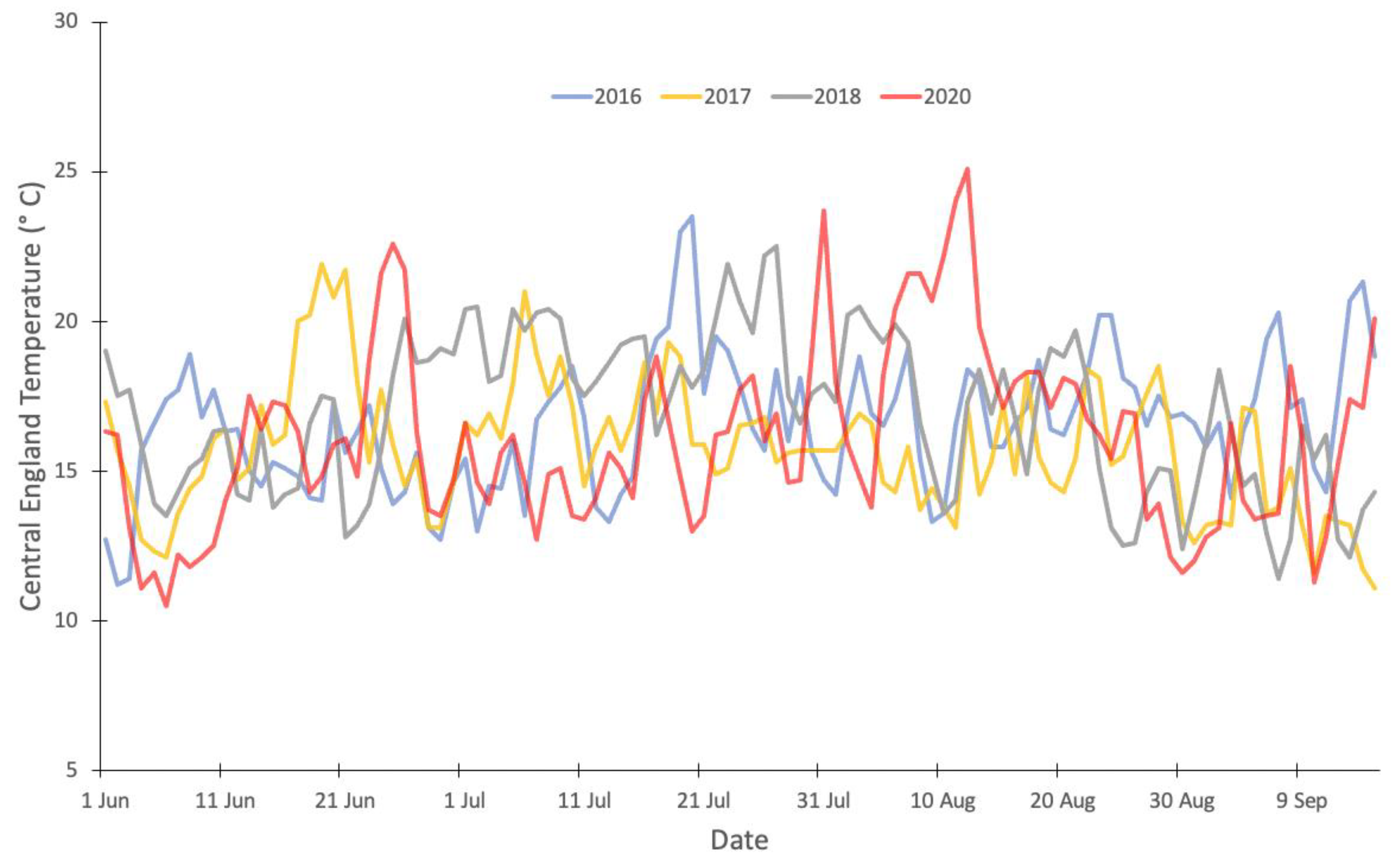
- Heatwave1 (H1) 23 to 27 June. East Midlands, West Midlands, East of England, London, Southeast and Southwest of England reached Level 3 HHA, and CET reached 20 °C;
- Heatwave2 (H2) 30 July to 1 August. No region reached a Level 3 HHA however CET reached 20 °C;
- Heatwave3 (H3) 5 to 15 August. East of England, London, and Southeast of England reached a Level 3 HHA, and CET reached 20 °C.
2.2. All-Cause Mortality Data
2.3. Episode Analysis
2.4. Heatwave Impacts by Age, Cause of Death, Place of Death and Region
3. Results
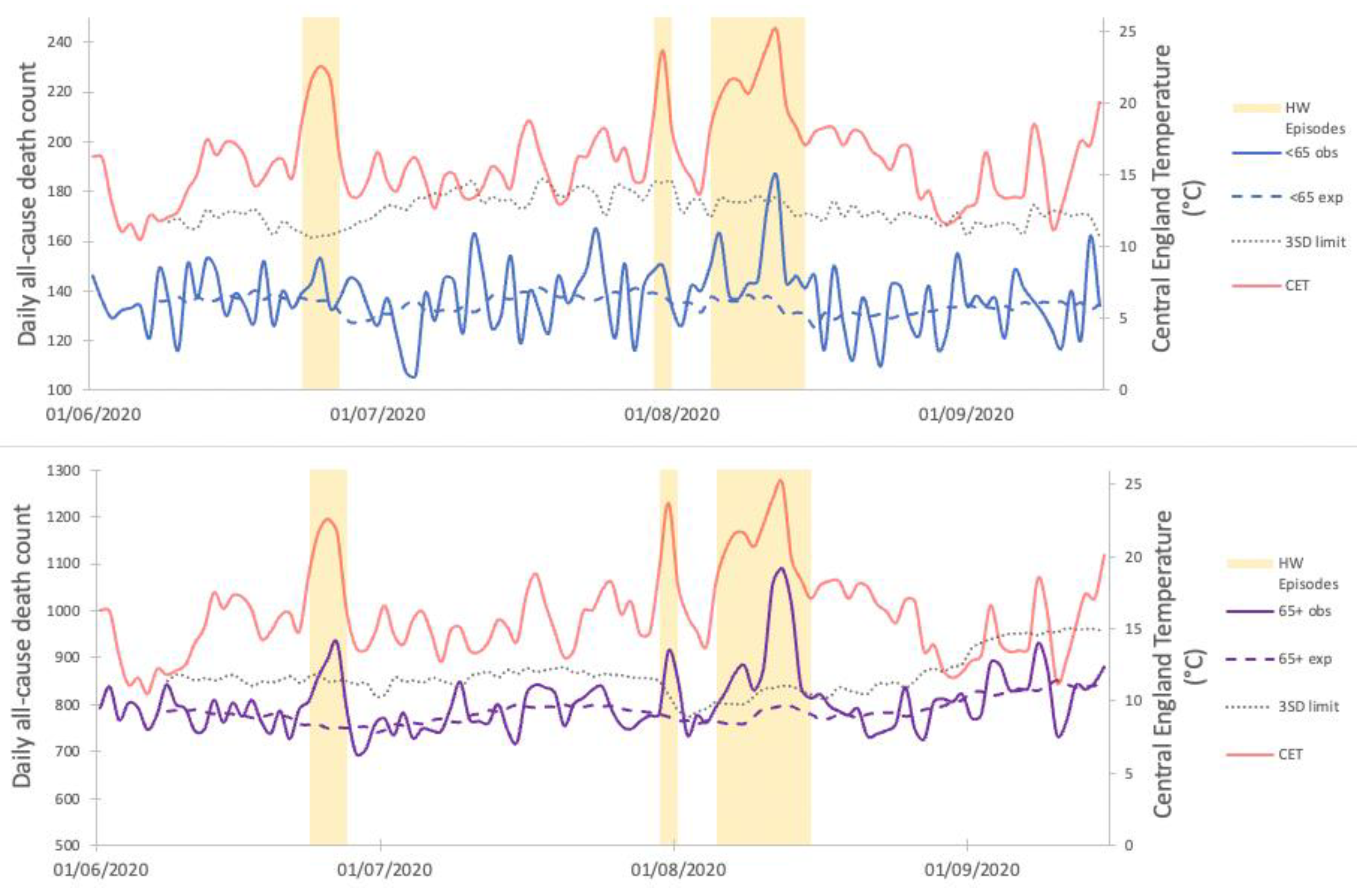
3.1. Descriptive Analysis
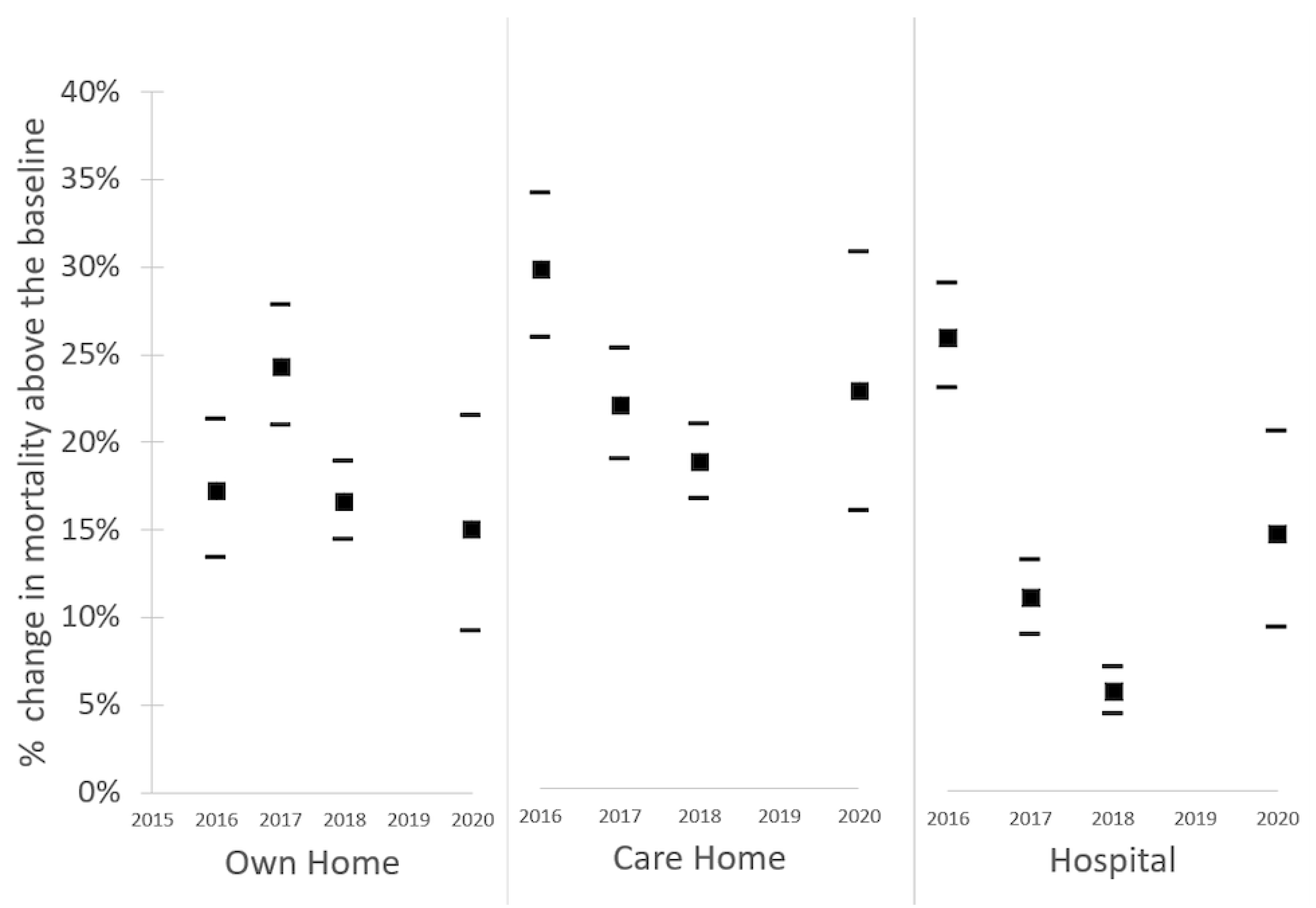
3.2. Place of Death
3.3. Cause of Death
4. Discussion
4.1. Summary of Findings
4.2. Potential Contributing Factors
4.3. Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Armstrong, B. Models for the Relationship Between Ambient Temperature and Daily Mortality. Epidemiology 2006, 17, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, B.G.; Chalabi, Z.; Fenn, B.; Hajat, S.; Kovats, S.; Milojevic, A.; Wilkinson, P. Association of mortality with high temperatures in a temperate climate: England and Wales. J. Epidemiol. Community Health 2011, 65, 340–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gasparrini, A.; Guo, Y.; Sera, F.; Vicedo-Cabrera, A.M.; Huber, V.; Tong, P.; Coelho, M.d.S.Z.S.; Saldiva, P.H.N.; Lavigne, E.; Correa, P.M.; et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet. Health 2017, 1, E360–E367. [Google Scholar] [CrossRef]
- Hajat, S.; Kovats, R.S.; Lachowycz, K. Heat-related and cold-related deaths in England and Wales: Who is at risk? Occup. Environ. Med. 2007, 64, 93. [Google Scholar] [CrossRef] [Green Version]
- Hajat, S.; Vardoulakis, S.; Heaviside, C.; Eggen, B. Climate change effects on human health: Projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. J. Epidemiol. Community Health 2014, 68, 641–648. [Google Scholar] [CrossRef] [Green Version]
- Kovats, R.S.; Hajat, S.; Wilkinson, P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occup. Environ. Med. 2004, 61, 893. [Google Scholar] [CrossRef] [Green Version]
- Climate Change 2014: Synthesis Report. In Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. AR5; Intergovernmental Panel on Climate Change: Geneva, Switzerland, 2014; p. 732.
- Allen, M.; Mustafa, B.; Shukla, P.; Chen, Y.; de Coninck, H.; Connors, S.; van Diemen, R.; Dube, O.P.; Ebi, K.L.; Engelbrecht, F.; et al. Global Warming of 1.5 °C—An IPCC Special Report on the Impacts of Global Warming of 1.5 °C above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty; Intergovernmental Panel on Climate Change: Geneva, Switzerland, 2018. [Google Scholar]
- Perkins-Kirkpatrick, S.E.; Lewis, S.C. Increasing trends in regional heatwaves. Nat. Commun. 2020, 11, 3357. [Google Scholar] [CrossRef]
- Slingo, J. Latest scientific evidence for observed and projected climate change. In The Third UK Climate Change Risk Assessment Technical Report; Prepared for the Climate Change Committee; Betts, R.A., Haward, A.B., Pearson, K.V., Eds.; Climate Change Committee: London, UK, 2021. [Google Scholar]
- Kovats, S.; Brisley, S. Health, communities and the built environment. In The Third UK Climate Change Risk Assessment Technical Report the Third UK Climate Change Risk Assessment Technical Report Committee on Climate Change; Climate Change Committee: London, UK, 2021. [Google Scholar]
- Arnell, N.W.; Kay, A.L.; Freeman, A.; Rudd, A.C.; Lowe, J.A. Changing climate risk in the UK: A multi-sectoral analysis using policy-relevant indicators. Clim. Risk Manag. 2021, 31, 100265. [Google Scholar] [CrossRef]
- Thompson, R.; Hornigold, R.; Page, L.; Waite, T. Associations between high ambient temperatures and heat waves with mental health outcomes: A systematic review. Public Health 2018, 161, 171–191. [Google Scholar] [CrossRef]
- Public Health England. Heatwave Plan for England; Public Health England: London, UK, 2015. Available online: https://www.gov.uk/government/publications/heatwave-plan-for-england (accessed on 1 March 2022).
- Public Health England. Heatwave Plan for England Making the Case: The Impact of Heat on Health—Now and in the Future; Public Health England: London, UK, 2016. [Google Scholar]
- Taylor, J.; Davies, M.; Mavrogianni, A.; Shrubsole, C.; Hamilton, I.; Das, P.; Jones, B.; Oikonomou, E.; Biddulph, P. Mapping indoor overheating and air pollution risk modification across Great Britain: A modelling study. Build. Environ. 2016, 99, 1–12. [Google Scholar] [CrossRef]
- Klepeis, N.E.; Nelson, W.C.; Ott, W.R.; Robinson, J.P.; Tsang, A.M.; Switzer, P.; Behar, J.V.; Hern, S.C.; Engelmann, W.H. The National Human Activity Pattern Survey (NHAPS): A resource for assessing exposure to environmental pollutants. J. Expo. Sci. Environ. Epidemiol. 2001, 11, 231–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schweizer, C.; Edwards, R.D.; Bayer-Oglesby, L.; Gauderman, W.J.; Ilacqua, V.; Jantunen, M.J.; Lai, H.K.; Nieuwenhuijsen, M.; Künzli, N. Indoor time–microenvironment–activity patterns in seven regions of Europe. J. Expo. Sci. Environ. Epidemiol. 2006, 17, 170–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- PHE Heatwave Mortality Monitoring. PHE Heatwave Mortality Monitoring: Summer 2018; Public Health England: London, UK, 2018. [Google Scholar]
- PHE Heatwave Mortality Monitoring. PHE Heatwave Mortality Monitoring: Summer 2016; Public Health England: London, UK, 2016. [Google Scholar]
- PHE Heatwave Mortality Monitoring. PHE Heatwave Mortality Monitoring: Summer 2017; Public Health England: London, UK, 2017. [Google Scholar]
- PHE Heatwave Mortality Monitoring: Summer 2019; Public Health England: London, UK, 2019.
- PHE Heatwave Mortality Monitoring. Heatwave Mortality Monitoring Report: 2020; Public Health England: London, UK, 2020. [Google Scholar]
- Kendon, M.; McCarthy, M.; Jevrejeva, S.; Matthews, A.; Sparks, T.; Garforth, J. State of the UK Climate 2020. Int. J. Climatol. 2021, 41, 1–76. [Google Scholar] [CrossRef]
- Met Office. Summer 2020; Met Office: Exeter, UK, 2020. [Google Scholar]
- Public Health England. Heat-Health Risks and COVID-19: Actions to Prevent Harm; Public Health England: London, UK, 2020. [Google Scholar]
- Hughes, H.E.; Hughes, T.C.; Morbey, R.; Challen, K.; Oliver, I.; Smith, G.E.; Elliot, A.J. Emergency department use during COVID-19 as described by syndromic surveillance. J. Emerg. Med. J. 2020, 37, 600–604. [Google Scholar] [CrossRef] [PubMed]
- Parker, D.E.; Legg, T.P.; Folland, C.K. A new daily Central England Temperature Series, 1772–1991. Int. J. Clim. 1992, 12, 317–342. [Google Scholar] [CrossRef]
- Public Health England. Classification of Place of Death. A Technical Bulletin from the National End of Life Care Intelligence Network; Public Health England: London, UK, 2019. [Google Scholar]
- Kovats, S.; Johnson, H.; Griffiths, C. Mortality in southern England during the 2003 heat wave by place of death. Health Stat. Q. 2006, 29, 6–8. [Google Scholar]
- Green, H.K.; Andrews, N.; Armstrong, B.; Bickler, G.; Pebody, R. Mortality during the 2013 heatwave in England—How did it compare to previous heatwaves? A retrospective observational study. Environ. Res. 2016, 147, 343–349. [Google Scholar] [CrossRef]
- WHO. Heat and Health in the WHO European Region: Updated Evidence for Effective Prevention; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Lo, Y.T.E.; Mitchell, D.M.; Thompson, R.; O’Connell, E.; Gasparrini, A. Estimating heat-related mortality in near real time for national heatwave plans. Environ. Res. Lett. 2022, 17, 024017. [Google Scholar] [CrossRef]
- Michelozzi, P.; De Sario, M.; Accetta, G.; de’Donato, F.; Kirchmayer, U.; D’Ovidio, M.; Perucci, C.A. Temperature and summer mortality: Geographical and temporal variations in four Italian cities. J. Epidemiol. Community Health 2006, 60, 417–423. [Google Scholar] [CrossRef] [Green Version]
- Murage, P.; Hajat, S.; Kovats, R.S. Effect of night-time temperatures on cause and age-specific mortality in London. Environ. Epidemiol. 2017, 1, e005. [Google Scholar] [CrossRef]
- García-Herrera, R.; Díaz, J.; Trigo, R.M.; Luterbacher, J.; Fischer, E.M. A Review of the European Summer Heat Wave of 2003. Crit. Rev. Environ. Sci. Technol. 2010, 40, 267–306. [Google Scholar] [CrossRef]
- Raleigh, V.S. UK’s record on pandemic deaths. BMJ 2020, 370, m3348. [Google Scholar] [CrossRef] [PubMed]
- Excess mortality in England, week ending 25 September 2020. In Weekly Excess Mortality in England Reports; Public Health England: London, UK, 2020.
- Mavrogianni, A.; Wilkinson, P.; Davies, M.; Biddulph, P.; Oikonomou, E. Building characteristics as determinants of propensity to high indoor summer temperatures in London dwellings. Build. Environ. 2012, 55, 117–130. [Google Scholar] [CrossRef] [Green Version]
- Hamilton, I.; Milner, J.; Chalabi, Z.; Das, P.; Jones, B.; Shrubsole, C.; Davies, M.; Wilkinson, P. Health effects of home energy efficiency interventions in England: A modelling study. BMJ Open 2015, 5, e007298. [Google Scholar] [CrossRef]
| Variable | Category | Number of Deaths | % Total |
|---|---|---|---|
| Age | 0–64 | 17,675 | 15% |
| 65+ | 102,102 | 85% | |
| Sex | Male | 59,482 | 50% |
| Female | 60,295 | 50% | |
| Region | Northeast England (NE) | 6592 | 6% |
| Northwest England (NW) | 16,865 | 14% | |
| Yorkshire and Humber (Y&H) | 12,367 | 10% | |
| East Midlands (EM) | 11,040 | 9% | |
| West Midlands (WM) | 13,624 | 11% | |
| East of England (EoE) | 13,695 | 11% | |
| London (LON) | 11,456 | 10% | |
| Southeast England (SE) | 20,027 | 17% | |
| Southwest England (SW) | 14,111 | 12% | |
| Place of death categories defined by NEoLCIN Underlying cause of death | Own home | 40,772 | 34% |
| Care home | 25,670 | 21% | |
| Hospital | 6924 | 6% | |
| Hospice | 46,097 | 38% | |
| Elsewhere * | 354 | <1% | |
| Underlying Cause of death (ICD10 codes) | Ischaemic heart disease (I20 to I25) | 948 | 2% |
| Stroke—cerebrovascular diseases (I60 to I69) | 6891 | 6% | |
| Other circulatory diseases (I00 to I19, I26 to I59 and I70 to I99) | 30,955 | 26% | |
| Cancer (C00 to C97) | 4086 | 3% | |
| Acute respiratory infections—including flu/pneumonia (J10 to J11, J12 to J18) | 3410 | 3% | |
| Chronic lower respiratory diseases—including asthma (J40 to J47) | 5190 | 4% | |
| Other respiratory diseases (J00 to J09, J19 to J39, J60 to J99) | 8415 | 7% | |
| Dementia and Alzheimer’s disease (F01,F03,G30) | 13,843 | 12% | |
| Diseases of the urinary system (N00 to N39) | 1843 | 2% | |
| Cirrhosis and other liver diseases (K70, K73 to K74) | 2016 | 2% | |
| Parkinson’s disease (G20) | 1660 | 1% | |
| Suicide (X60 to X84) | 991 | 1% | |
| Accidents (V01 to X59) | 1948 | 2% |
| Place of Death Category | Age Group | Heatwave Event | ||
|---|---|---|---|---|
| H1 | H2 | H3 | ||
| Deaths at home | <65 | 5 (−14 to 24) | 0 (−8 to 8) | 61 (3 to 119) |
| 65+ | 90 (50 to 130) | 20 (2 to 39) | 416 (289 to 542) | |
| Deaths in care homes | <65 | −2 (−6 to 3) | N/A | 28 (12 to 43) |
| 65+ | 87 (53 to 121) | 54 (39 to 70) | 463 (353 to 573) | |
| Deaths in hospitals | <65 | 15 (−4 to 33) | 6 (−3 to 15) | 63 (0 to 126) |
| 65+ | 146 (105 to 187) | 19 (−1 to 39) | 437 (298 to 576) | |
| Deaths in hospices | <65 | 4 (−4 to 12) | 4 (0 to 8) | 14 (−14 to 43) |
| 65+ | 0 (−17 to 17) | 4 (−3 to 11) | 64 (14 to 115) | |
| Deaths in all settings | <65 | 23 (3 to 23) | 9 (0 to 18) | 175 (110 to 240) |
| 65+ | 322 (274 to 371) | 100 (78 to 123) | 1384 (1225 to 1543) | |
| Cause of Death | Age Group | H1 | H2 | H3 |
|---|---|---|---|---|
| Ischemic HD (ICD10 code: I20 to I25) | <65 | −4 (−7 to −2) | −9 (−11 to −7) | 12 (9 to 15) |
| 65+ | 18 (14 to 22) | 9 (6 to 13) | 7 (0 to 13) | |
| Cerebrovascular diseases (ICD10 code: I60 to I69) | <65 | 11 (8 to 13) | 11 (8 to 13) | 9 (5 to 13) |
| 65+ | 25 (17 to 34) | 0 (−7 to 7) | 69 (56 to 83) | |
| All circulatory deaths (ICD10 code: I00 to I99) | <65 | 29 (22 to 35) | 6 (1 to 12) | 33 (22 to 44) |
| 65+ | 115 (97 to 133) | 45 (31 to 60) | 408 (380 to 435) | |
| Acute respiratory infections (including flu/pneumonia) ICD10 code: J10 to J11, J12 to J18) | <65 | 1 (−1 to 3) | −3 (−4 to −1) | −4 (−7 to −1) |
| 65+ | 19 (13 to 25) | 15 (10 to 20) | 16 (6 to 25) | |
| Chronic lower respiratory deaths (ICD10 code: J40 to J47) | <65 | −3 (−6 to 0) | −3 (−5 to −1) | 9 (5 to 13) |
| 65+ | 30 (23 to 38) | 14 (8 to 19) | 118 (107 to129) | |
| Other respiratory deaths (ICD10 code: J00 to J09, J19 to J39, J60 to J99) | <65 | −11 (−15 to −8) | 3 (−5 to 0) | 9 (4 to 14) |
| 65+ | 72 (63 to 82) | 11 (4 to 19) | 192 (187 to 206) | |
| Alzheimer’s and Dementia (ICD10 code: F01,F03,G30) | <65 | N/A | N/A | 0 (−1 to 2) |
| 65+ | 47 (34 to 60) | 23 (13 to 33) | 62 (42 to 83) | |
| Parkinson’s disease (ICD10 code: G20) | <65 | N/A | N/A | N/A |
| 65+ | 3 (−1 to 8) | 8 (4 to 11) | −1 (−8 to 7) | |
| All cancer deaths (ICD10 code: C00 to C97) | <65 | 8 (5 to 11) | 4 (1 to 6) | −10 (−15 to −5) |
| 65+ | 17 (11 to 24) | 8 (3 to 13) | −10 (−20 to 0) | |
| Diseases of the urinary system (ICD10 code: N00 to N39) | <65 | N/A | N/A | 5 (4 to 7) |
| 65+ | −13 (−18 to 8) | −5 (−8 to −1) | 9 (2 to 16) | |
| Cirrhosis and other liver diseases (ICD10 code: K70, K73 to K74) | <65 | −5 (−9 to −1) | −9 (−12 to −5) | −22 (−28 to−15) |
| 65+ | 3 (0 to 6) | 4 (2 to 6) | 14 (10 to 18) | |
| Suicide (ICD10 code: X60 to X84) | <65 | 5 (3 to 7) | −2 (−4 to 0) | −14 (−18 to 11) |
| 65+ | −2 (−4 to 1) | 6 (4 to 8) | 4 (0 to 8) | |
| Accidental death (ICD10 codes: V01 to X59) | <65 | −4 (−7 to −2) | −9 (−11 to −7) | 12 (9 to 15) |
| 65+ | 18 (14 to 22) | 9 (6 to 13) | 7 (0 to 13) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thompson, R.; Landeg, O.; Kar-Purkayastha, I.; Hajat, S.; Kovats, S.; O’Connell, E. Heatwave Mortality in Summer 2020 in England: An Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 6123. https://doi.org/10.3390/ijerph19106123
Thompson R, Landeg O, Kar-Purkayastha I, Hajat S, Kovats S, O’Connell E. Heatwave Mortality in Summer 2020 in England: An Observational Study. International Journal of Environmental Research and Public Health. 2022; 19(10):6123. https://doi.org/10.3390/ijerph19106123
Chicago/Turabian StyleThompson, Ross, Owen Landeg, Ishani Kar-Purkayastha, Shakoor Hajat, Sari Kovats, and Emer O’Connell. 2022. "Heatwave Mortality in Summer 2020 in England: An Observational Study" International Journal of Environmental Research and Public Health 19, no. 10: 6123. https://doi.org/10.3390/ijerph19106123
APA StyleThompson, R., Landeg, O., Kar-Purkayastha, I., Hajat, S., Kovats, S., & O’Connell, E. (2022). Heatwave Mortality in Summer 2020 in England: An Observational Study. International Journal of Environmental Research and Public Health, 19(10), 6123. https://doi.org/10.3390/ijerph19106123







