Use of Information and Communication Technology by South Korean Occupational Therapists Working in Hospitals: A Cross-Sectional Study
Abstract
1. Introduction
2. Methods
2.1. Survey Design
2.2. Participants
2.3. Data Analysis
3. Results
3.1. Demographic Characteristics
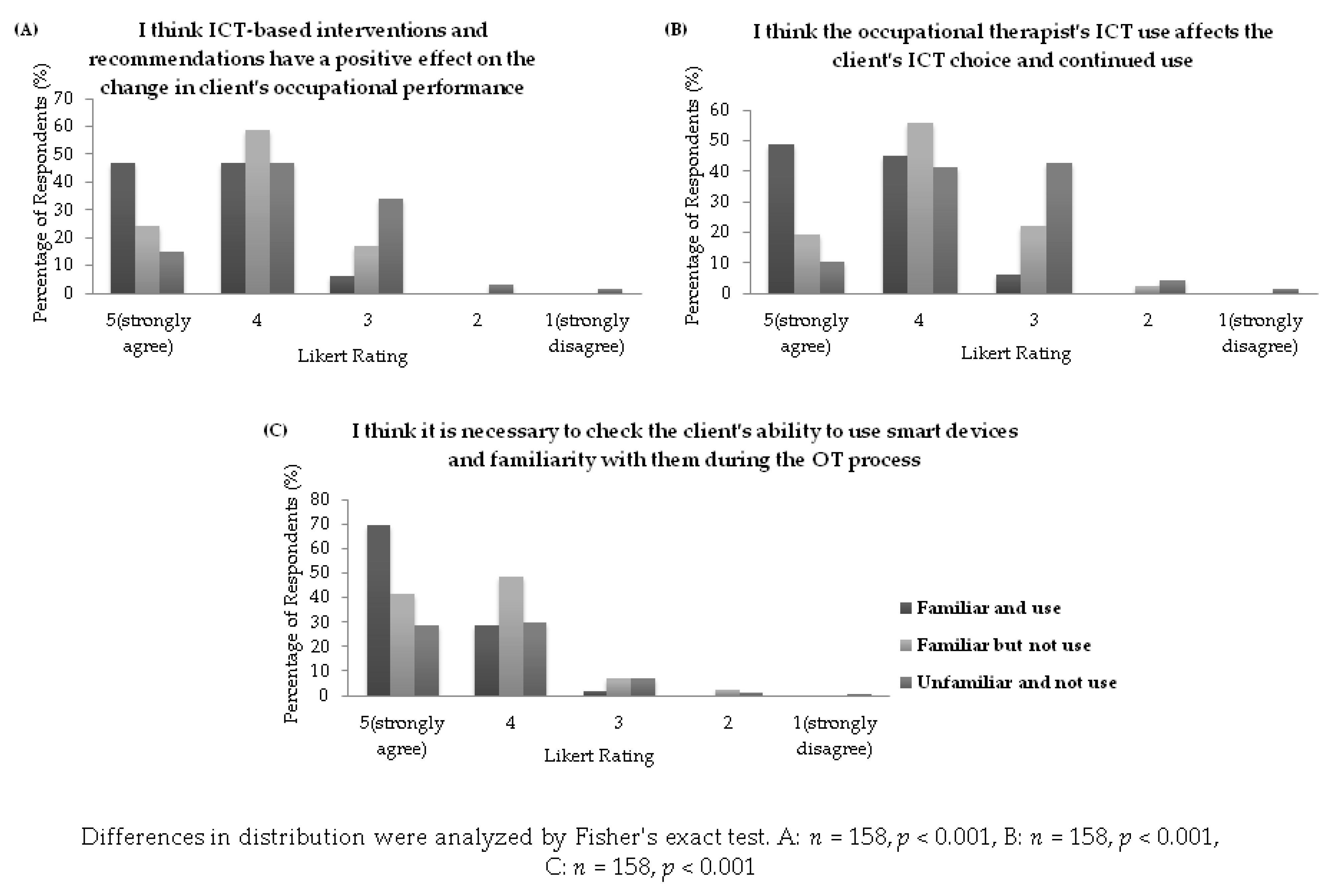
3.2. Opinions on the Therapeutic Use of ICT
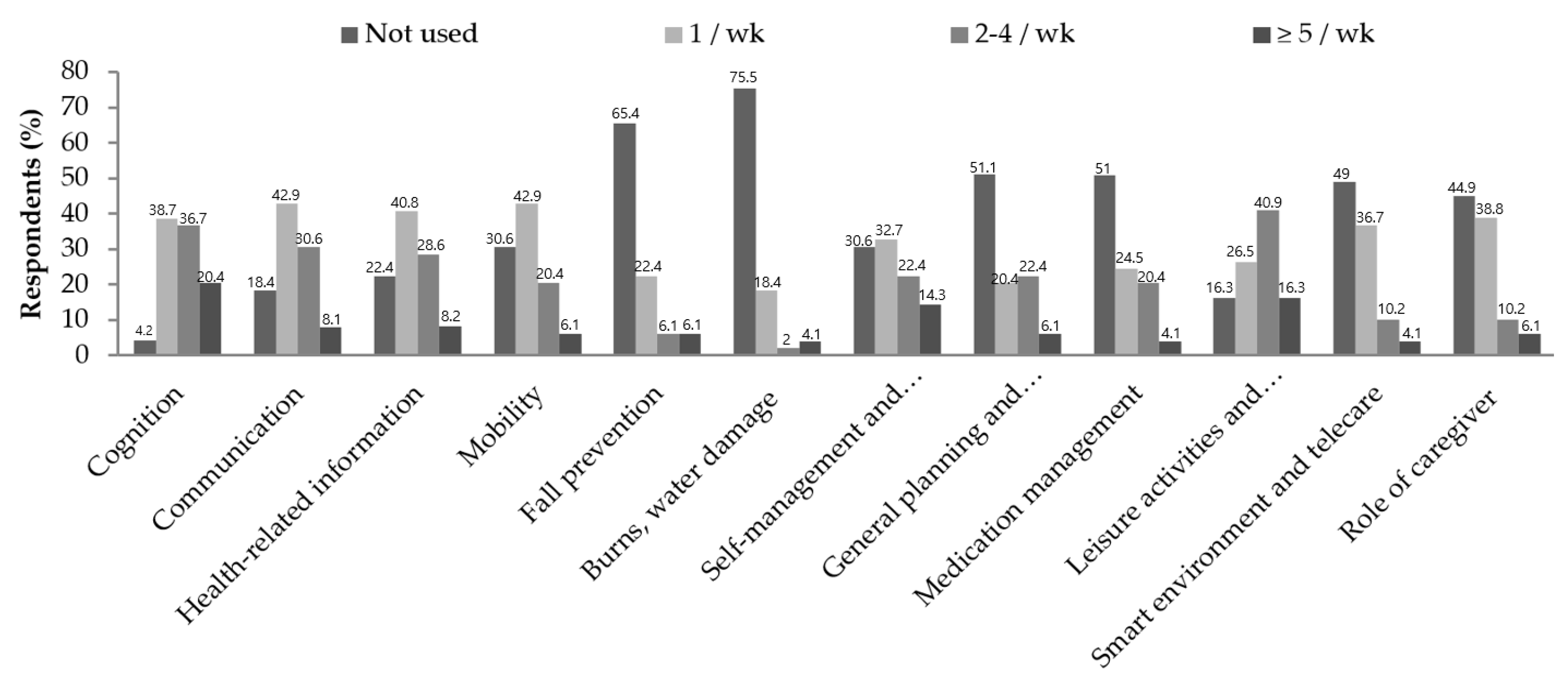
3.3. Application of ICT by Familiar Users in Clinical Practice
3.4. Factors Influencing ICT Use by OTs
4. Discussion
4.1. Opinions on the Therapeutic Uses of ICT
4.2. Familiarity with and Use of ICT
4.3. Factors Influencing ICT Use
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, K.B.; Han, K.H. A Study of the Digital Healthcare Industry in the Fourth Industrial Revolution. J. Converg. Inf. Technol. 2020, 10, 7–15. [Google Scholar]
- Industry Research Institute. New Growth Engine in the Era of the Fourth Industrial Revolution, the Smart Healthcare Industry. i-KIET Ind. Econ. 2017. Available online: https://eng.kiet.re.kr/kiet_eng/main.jsp?sub_num=209&ord=0&pageNo=3&state=view&recom=0&idx=10826 (accessed on 24 February 2022).
- Berwick, D.M.; Nolan, T.W.; Whittington, J. The triple aim: Care, health, and cost. Health Aff. 2008, 27, 759–769. [Google Scholar] [CrossRef]
- Mair, F.S.; May, C.; Finch, T.; Murray, E.; Anderson, G.; Sullivan, F.; O’donnell, C.; Wallace, P.; Epstein, O. Understanding the implementation and integration of e-health services. J. Telemed. Telecare 2007, 13, 36–37. [Google Scholar] [CrossRef]
- Health Care Special Committee. Healthcare Development Strategy based on the 4th Industrial Revolution. 2018. Available online: https://www.4th-ir.go.kr/article/detail/373?boardName=internalData&category=agenda (accessed on 24 February 2022).
- World Federation of Occupational Therapists. About Occupational Therapy. Available online: https://www.wfot.org/about/about-occupational-therapy (accessed on 23 February 2022).
- May, C.; Gask, L.; Atkinson, T.; Ellis, N.; Mair, F.; Esmail, A. Resisting and promoting new technologies in clinical practice: The case of telepsychiatry. Soc. Sci. Med. 2001, 52, 1889–1901. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening. Available online: https://apps.who.int/iris/bitstream/handle/10665/311977/WHO-RHR-19.8-eng.pdf?ua=1 (accessed on 2 March 2022).
- Chen, Y.R.; Schulz, P.J. The Effect of Information Communication Technology Interventions on Reducing Social Isolation in the Elderly: A Systematic Review. J. Med. Internet Res. 2016, 18, e18. [Google Scholar] [CrossRef]
- American Occupational Therapy Association. Occupational Therapy’s Role with Providing Assistive Technology Devices and Services. 2015. Available online: https://www.aota.org/-/media/Corporate/Files/AboutOT/Professionals/WhatIsOT/RDP/Facts/AT-fact-sheet.pdf (accessed on 8 January 2022).
- Canadian Association of Occupational Therapists. CAOT Position Statement Assistive Technology and Occupational Therapy. 2012. Available online: https://caot.in1touch.org/document/3655/assistivetechnology.pdf (accessed on 23 February 2022).
- Zonneveld, M.; Patomella, A.H.; Asaba, E.; Guidetti, S. The use of information and communication technology in healthcare to improve participation in everyday life: A scoping review. Disabil. Rehabil. 2020, 42, 3416–3423. [Google Scholar] [CrossRef]
- Collins, M. Occupational therapists’ experience with assistive technology in provision of service to clients with Alzheimer’s disease and related dementias. Phys. Occup. Ther. 2018, 36, 179–188. [Google Scholar] [CrossRef]
- Ninnis, K.; Van Den Berg, M.; Lannin, N.A.; George, S.; Laver, K. Information and communication technology use within occupational therapy home assessments: A scoping review. Br. J. Occup. Ther. 2019, 82, 141–152. [Google Scholar] [CrossRef]
- Hwang, N.K.; Shim, S.H. Use of Virtual Reality Technology to Support the Home Modification Process: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 11096. [Google Scholar] [CrossRef]
- Korean Occupational Therapists Association (KOTA). Statistics of Occupational Therapists Nationwide. Available online: https://www.kaot.org/pds/stat.jsp (accessed on 6 February 2022).
- Seifert, A.M.; Stotz, N.; Metz, A.E. Apps in therapy: Occupational therapists’ use and opinions. Disabil. Rehabil. Assist. Technol. 2017, 12, 772–779. [Google Scholar] [CrossRef]
- Canadian Association of Occupational Therapists. Technology for Occupation and Participation. 2016. Available online: https://caot.ca/site/pd/networks/technology?nav=sidebar (accessed on 2 February 2022).
- International Network on the Disability Creation Process. HDM-DCP Model. Available online: http://ripph.qc.ca/en/documents/quebec-classification/ (accessed on 7 February 2022).
- Aboujaoudé, A.; Bier, N.; Lussier, M.; Ménard, C.; Couture, M.; Demers, L.; Auger, C.; Pigot, H.; Caouette, M.; Lussier-Desrochers, D.; et al. Canadian Occupational Therapists’ Use of Technology With Older Adults: A Nationwide Survey. OTJR 2021, 41, 67–79. [Google Scholar] [CrossRef]
- National Information Society Agency. Information and Communication Assistive Technology Devices. Available online: https://www.at4u.or.kr/F01000000000/F01030000000.asp?UpCode=L3&strPDTSupplyDate=2021 (accessed on 7 February 2022).
- Ministry of Health and Welfare. Assistive Device Item Classification System. Available online: http://www.mohw.go.kr/react/jb/sjb0406vw.jsp?PAR_MENU_ID=03&MENU_ID=030406&page=1&CONT_SEQ=360004 (accessed on 7 February 2022).
- Ramsey, R. The Professional Expertise of Community-Practicing Occupational Therapists. Ph.D. Dissertation, University of San Francisco, San Francisco, CA, USA, 2007. [Google Scholar]
- Marwaa, M.N.; Ytterberg, C.; Guidetti, S. Significant others’ perspectives on person-centred information and communication technology in stroke rehabilitation—A grounded theory study. Disabil. Rehabil. 2020, 42, 2115–2122. [Google Scholar] [CrossRef]
- Grau-Pellicer, M.; Lalanza, J.F.; Jovell-Fernández, E.; Capdevila, L. Impact of mHealth technology on adherence to healthy PA after stroke: A randomized study. Top. Stroke Rehabil. 2020, 27, 354–368. [Google Scholar] [CrossRef]
- Solli, H.; Bjørk, I.T.; Hvalvik, S.; Hellesø, R. Like an extended family: Relationships that emerge when older caregivers use written messages to communicate in an ICT-based healthcare service. Inform. Health Soc. Care 2018, 43, 207–217. [Google Scholar] [CrossRef]
- American Occupational Therapy Association. Telehealth in occupational therapy. Am. J. Occup. Ther. 2018, 72, 7212410059. [Google Scholar]
- Lindqvist, E.; Borell, L. Computer-based assistive technology and changes in daily living after stroke. Disabil. Rehabil. Assist. Technol. 2012, 7, 364–371. [Google Scholar] [CrossRef]
- Gustavsson, M.; Ytterberg, C.; Nabsen Marwaa, M.; Tham, K.; Guidetti, S. Experiences of using information and communication technology within the first year after stroke—A grounded theory study. Disabil. Rehabil. 2018, 40, 561–568. [Google Scholar] [CrossRef]
- Wildevuur, S.E.; Simonse, L.W. Information and communication technology-enabled person-centered care for the “big five” chronic conditions: Scoping review. J. Med. Internet Res. 2015, 17, e77. [Google Scholar] [CrossRef]
- Allen Christensen, K.; Lund, K.M.; Thuesen, J. Evaluation of Person-Centredness in Rehabilitation for People Living with Dementia Is Needed: A Review of the Literature. J. Aging Res. 2019, 2019, 8510792. [Google Scholar] [CrossRef]
- Gustavsson, M.; Ytterberg, C.; Guidetti, S. Exploring future possibilities of using information and communication technology in multidisciplinary rehabilitation after stroke—A grounded theory study. Scand. J. Occup. Ther. 2020, 27, 223–230. [Google Scholar] [CrossRef]
- Bakas, T.; Clark, P.C.; Kelly-Hayes, M.; King, R.B.; Lutz, B.J.; Miller, E.L.; American Heart Association Council on Cardiovascular and Stroke Nursing and the Stroke Council. Evidence for stroke family caregiver and dyad interventions: A statement for healthcare professionals from the American Heart Association and American Stroke Association. Stroke 2014, 45, 2836–2852. [Google Scholar] [CrossRef]
- Wingham, J.; Adie, K.; Turner, D.; Schofield, C.; Pritchard, C. Participant and caregiver experience of the Nintendo Wii Sports™ after stroke: Qualitative study of the trial of Wii™ in stroke (TWIST). Clin. Rehabil. 2015, 29, 295–305. [Google Scholar] [CrossRef]
- Cappa, S.F.; Benke, T.; Clarke, S.; Rossi, B.; Stemmer, B.; van Heugten, C.M. Cognitive rehabilitation. In European Handbook of Neurological Management, 2nd ed.; N. Gilhus, N.E., Barnes, M.P., Brainin, M., Eds.; Wiley-Blackwell: New York, NY, USA, 2011; pp. 545–567. [Google Scholar]
- Lee, H.R.; Kim, J.Y.; Han, D.S. A Survey on the Cognitive Rehabilitation of Occupational Therapy in Korea. Korean J. Occup. Ther. 2012, 20, 73–84. [Google Scholar]
- Kim, S.Y.; Lee, E.H.; Jeong, S.J.; Shin, J.Y. Understanding the Silver Industry; Academician: Seoul, Korea, 2016. [Google Scholar]
- Park, S.Y.; Lee, Y.S.; Kang, C.W.; Park, H.O.; Bae, S.G.; Lee, J.W.; Choi, S.S. Current Trends Analysis of Welfare Technology in Korea for Older Adults and People with Disabilities. J. Korean Converg. Soc. 2017, 8, 295–304. [Google Scholar]
- Svensson, P.G. eHealth Applications in Health Care Management. eHealth Int. 2002, 1, 5. [Google Scholar] [CrossRef][Green Version]
- Chismar, W.G.; Wiley-Patton, S. Does the extended technology acceptance model apply to physicians. IEEE Comput. Soc. 2003, 7, 160a. Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.97.9056&rep=rep1&type=pdf (accessed on 22 February 2022).
- Kapadia, V.; Ariani, A.; Li, J.; Ray, P. Emerging ICT implementation issues in aged care. Int. J. Med. Inform. 2015, 84, 892–900. [Google Scholar] [CrossRef]
- Korea Association of Occupational Therapists. Digital Occupational Therapy, with a New Era. 2021. Available online: https://www.kaot.org/board/index.jsp?code=policy (accessed on 4 May 2022).
- Marwaa, M.N.; Kristensen, H.K.; Guidetti, S.; Ytterberg, C. Physiotherapists’ and occupational therapists’ perspectives on information and communication technology in stroke rehabilitation. PLoS ONE 2020, 15, e0236831. [Google Scholar] [CrossRef]
- Schaper, L.K.; Pervan, G.P. ICT and OTs: A model of information and communication technology acceptance and utilisation by occupational therapists. Int. J. Med. Inform. 2007, 76, S212–S221. [Google Scholar] [CrossRef]
- Waite, A. “App”titude: Smart gadget applications showing their worth in practice. OT Pract. 2012, 17, 9–12. [Google Scholar]
- Yamkovenko, S. Apps for Occupational Therapy: Find Apps for Your Practice Area. Available online: http://www.aota.org/apps (accessed on 20 February 2022).
| Variables | Total = 158 n (%) | Familiar Users = 49 | Familiar Non-Users = 41 | Unfamiliar Non-Users = 68 |
|---|---|---|---|---|
| Gender | ||||
| Female | 90 (57.0) | 19 (38.8) | 23 (56.1) | 48 (70.6) |
| Male | 68 (43.0) | 30 (61.2) | 18 (43.9) | 20 (29.4) |
| Age | ||||
| 20–29 | 64 (40.5) | 9 (18.4) | 18 (43.9) | 37 (54.4) |
| 30–39 | 74 (46.8) | 27 (55.1) | 21 (51.2) | 26 (38.2) |
| >40 | 20 (12.7) | 13 (26.5) | 2 (4.9) | 5 (7.4) |
| Mean ± SD | 31.8 ± 5.9 | 34.7 ± 6.2 | 31.1 ± 4.9 | 30.2 ± 5.5 |
| Practice experience | ||||
| 1–5 years | 55 (34.8) | 8 (16.3) | 15 (36.6) | 32 (47.0) |
| 6–10 years | 63 (39.9) | 21 (42.9) | 20 (48.8) | 22 (32.4) |
| 10–15 years | 25 (15.8) | 10 (20.4) | 5 (12.2) | 10 (14.7) |
| >10 years | 15 (9.5) | 10 (20.4) | 1 (2.4) | 4 (5.9) |
| Mean ± SD | 8.0 ± 4.8 | 10.3 ± 4.5 | 6.8 ± 3.8 | 7.0 ± 4.7 |
| Education | ||||
| Associate’s | 28 (17.7) | 6 (12.2) | 8 (19.5) | 14 (20.6) |
| Bachelor’s | 87 (55.1) | 24 (49.0) | 22 (53.6) | 41 (60.3) |
| Master’s & higher | 43 (27.2) | 19 (38.8) | 11 (26.9) | 13 (19.1) |
| Place of work | ||||
| University/General Hospital | 57(36.1) | 19 (38.8) | 12 (29.3) | 26 (38.2) |
| (Semi) Hospital | 57(36.1) | 17 (34.7) | 15 (36.6) | 25 (36.8) |
| Clinic | 1 (0.6) | 1 (2.0) | 0 (0.0) | 0 (0.0) |
| Nursing hospital | 7 (4.4) | 1 (2.0) | 2 (4.9) | 4 (5.9) |
| Public healthcare center (including dementia center) | 36 (22.8) | 11 (22.4) | 12 (29.2) | 13 (19.1) |
| Province of employment | ||||
| Seoul | 34 (21.5) | 13 (26.5) | 7 (17.1) | 14 (20.6) |
| Gyeonggi | 29 (18.4) | 14 (28.6) | 5 (12.2) | 10 (14.7) |
| Jeolla | 20 (12.7) | 5 (10.2) | 6 (14.6) | 9 (13.2) |
| Gyeongsang | 27 (17.1) | 4 (8.2) | 10 (24.4) | 13 (19.2) |
| Gangwon | 27 (17.1) | 3(6.1) | 8 (19.5) | 16 (23.5) |
| Chungcheong | 21 (13.3) | 10 (20.4) | 5 (12.2) | 6 (8.8) |
| Practice areas | ||||
| Assessment | 110 (69.6) | 33 (67.3) | 29 (70.7) | 48 (70.6) |
| Neurological | 113 (71.5) | 36 (73.5) | 27 (65.9) | 50 (73.5) |
| Musculoskeletal | 51 (32.3) | 21 (42.9) | 8 (19.5) | 22 (32.4) |
| Psychosocial | 20 (12.7) | 6 (12.2) | 5 (12.2) | 9 (13.2) |
| Prevocational/vocational | 10 (6.3) | 5 (10.2) | 3 (7.3) | 2 (2.9) |
| Cognitive/Perceptual | 88 (55.7) | 24 (50.0) | 20 (48.8) | 44 (64.7) |
| Hand therapy | 31 (19.6) | 12 (24.5) | 7 (17.1) | 12 (17.6) |
| Health promotion and wellness (community) | 31 (19.6) | 14 (28.6) | 7 (17.1) | 10 (14.7) |
| Developmental | 33 (20.9) | 12 (24.5) | 4 (9.8) | 17 (25.0) |
| Geriatric | 72 (45.6) | 20 (40.8) | 22 (53.7) | 30 (44.1) |
| Client | ||||
| CNS disorders | 133 (84.2) | 40 (81.6) | 36 (87.8) | 57 (83.8) |
| Musculoskeletal disorders | 63 (39.9) | 21 (42.9) | 12 (29.3) | 30 (44.1) |
| Cardiopulmonary disease | 18 (11.4) | 9 (18.4) | 3 (7.3) | 6 (8.8) |
| Hand injury | 37 (23.4) | 12 (24.5) | 7 (17.1) | 18 (26.5) |
| Arthritis and rheumatoid | 35 (22.2) | 10 (20.4) | 7 (17.1) | 18 (26.5) |
| Cancer | 19 (12.0) | 8 (16.3) | 2 (4.9) | 9 (13.2) |
| Geriatric diseases | 105 (66.5) | 24 (50.0) | 29 (70.7) | 52 (76.5) |
| Visual impairment | 23 (14.6) | 4 (8.2) | 3 (7.3) | 16 (23.5) |
| Hearing impairment | 14 (8.9) | 3 (6.1) | 3 (7.3) | 8 (11.8) |
| Mental illness | 20 (12.7) | 5 (10.2) | 6 (14.6) | 9 (13.2) |
| Intellectual disability | 42 (26.6) | 10 (20.4) | 7 (17.1) | 25 (36.8) |
| Cerebral palsy | 51 (32.3) | 13 (26.5) | 9 (22.0) | 29 (42.6) |
| Developmental disabilities | 39 (24.7) | 12 (24.5) | 4 (9.8) | 23 (33.8) |
| Genetic disorder | 27 (17.1) | 9 (18.4) | 3 (7.3) | 15 (22.1) |
| Learning disabilities | 20 (12.7) | 8 (16.3) | 3 (7.3) | 9 (13.2) |
| Language disorder | 22 (14.0) | 5 (10.2) | 6 (14.6) | 11 (16.2) |
| Autism | 29 (18.4) | 6 (12.2) | 6 (14.6) | 17 (25.0) |
| ICT-Based Interventions Or Recommendations | Users, n (%) |
|---|---|
| Personal factors | |
| Cognitive function | 47 (95.9) |
| Voice recordings or text memo function on tablets or smartphones | 47 (95.9) |
| Apps for cognitive function improvement training | 38 (77.6) |
| App-based games (e.g., Baduk, Korean Chess, Sudoku, RumiCube) | 38 (77.6) |
| Reminders app | 11 (22.4) |
| Calendar app | 11 (22.4) |
| Timer app | 10 (20.4) |
| Photos app | 9 (18.4) |
| Digital photo frame | 3 (6.1) |
| Virtual reality software | 1 (2.0) |
| Communication | 40 (81.6) |
| Internet video call app or video phone | 23 (46.9) |
| Voice recognition (voice command) function on smartphones | 20 (40.8) |
| Smart AAC for communication | 16 (32.7) |
| Image dictionary app on tablets or smartphones | 16 (32.7) |
| Use of social media (e.g., blog, SNS, Kakao Talk open chat) | 14 (28.6) |
| Text-to-Speech app or device | 13 (26.5) |
| Smart AAC for language training | 11 (22.4) |
| Adaptive smartphone (e.g., smartphone customized for the elderly) | 9 (18.4) |
| Special mouse or special keyboard, key guard | 7 (14.3) |
| Optical character reader | 3 (6.1) |
| Braille translation app | 2 (4.1) |
| Bone conduction hearing aids | 1 (2.0) |
| Health-related information | 38 (77.6) |
| Exercise program websites or video channels | 35 (71.4) |
| Websites or video channels to obtain information about diseases and conditions | 25 (51.0) |
| Apps to track physical activity (e.g., steps, repetitive movements) | 22 (44.9) |
| Apps to record or track physiological changes (e.g., heart rate, blood pressure) | 10 (20.4) |
| Apps to manage lifestyle patterns (e.g., drinking, smoking, exercise) | 10 (20.4) |
| Apps to record or track psychological states (e.g., mood, anxiety, panic) | 8 (16.3) |
| Web forums dealing with health-related topics | 6 (12.2) |
| Self-reliance and participation | |
| Mobility | 34 (69.4) |
| Apps for directions and public transportation (e.g., Naver Map, Kakao Map) | 26 (53.1) |
| GPS location-tracking apps or watches | 13 (26.5) |
| GPS white cane | 4 (8.2) |
| Products for motion restriction (e.g., beds with motion sensor, motion detection alarms) | 3 (6.1) |
| Fall prevention | 17 (34.7) |
| Fall detection watches or bands | 15 (30.6) |
| Personal emergency alarm systems | 11 (22.4) |
| Night sensor light that detects motion | 10 (20.4) |
| Prevention of burns or water damage | 12 (24.5) |
| Water temperature indicator | 9 (18.4) |
| Automatic hot water control system (e.g., automatic hot water control valve) | 7 (14.3) |
| Leakage, flood detection alarm | 3 (6.1) |
| Self-management and household activities | 34 (69.4) |
| Online grocery purchases | 33 (67.3) |
| Recipe websites or apps | 18 (36.7) |
| Robot vacuum cleaner | 16 (32.7) |
| Apps for household ledgers or budget planning | 15 (30.6) |
| Digital Cooking Timer | 12 (24.5) |
| Iron with automatic power off function | 8 (16.3) |
| Apps for meal planning or organization | 7 (14.3) |
| Sleep cycle monitoring apps | 5 (10.2) |
| General planning and management of daily activities | 24 (49.0) |
| Goal setting and management apps | 23 (46.9) |
| Apps that record accomplished activities (e.g., Logbook) | 15 (30.6) |
| Medication management | 24 (49.0) |
| Medication reminder apps | 19 (38.8) |
| Automatic pill dispenser | 12 (24.5) |
| Drug search, prescription information management apps | 7 (14.3) |
| Leisure activities and information access | 41 (83.7) |
| Information access using computers, tablets, smartphones, mobile games, Nintendo Wii | 38 (77.6) |
| Remote controls for the elderly (e.g., large button, universal) | 11 (22.4) |
| Environment | |
| Smart environments and telecare | 25 (51.0) |
| Smart home appliances and environmental control systems (automatic heating and lighting control systems) | 20 (40.8) |
| Home CCTV | 16 (32.7) |
| Remote control of home appliances and environment settings (e.g., room temperature, lighting, front door) via tablets and smartphones | 14 (28.6) |
| Emergency pager (carried by the patient and connected to the phone in case of an emergency) | 9 (18.4) |
| Telecare system | 3 (6.1) |
| Caregiver role support | 27 (55.1) |
| Websites providing information for client care | 23 (46.9) |
| Devices that measure and monitor parameters such as blood pressure, oxygen saturation, and heart rate | 13 (26.5) |
| Video conferences with caregiver | 10 (20.4) |
| Users (n = 49) | Non-Users (n = 41) | |
|---|---|---|
| Facilitators, n (%) | ||
| Ease of use (operation, manipulation) | 36 (73.5) | - |
| Usefulness when applied to client | 32 (65.3) | - |
| Reasonable purchase price and maintenance costs | 31 (63.3) | - |
| Easily obtainable product | 25 (51.0) | - |
| Financial and administrative support in the workplace | 15 (30.6) | - |
| Therapist’s proficiency in using ICT | 14 (28.6) | - |
| Reliability of the product or technology | 9 (18.4) | - |
| Barriers, n (%) | ||
| Lack of knowledge and training of therapist | 30 (61.2) | 14 (34.1) |
| Expensive product or technology | 27 (55.1) | 27 (65.9) |
| Lack of financial and administrative support in the workplace | 24 (50.0) | 17 (41.5) |
| Lack of experience of client in ICT | 22 (44.9) | 26 (63.4) |
| Lack of information about ICT within the department | 17 (34.7) | 16 (39.0) |
| Client’s negative attitude toward ICT application | 14 (28.6) | 11 (26.8) |
| Increase in therapist’s workload for ICT use | 9 (18.4) | 10 (24.4) |
| Negative experience of therapist in ICT application | 6 (12.2) | 2 (4.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, N.-K.; Shim, S.-H.; Cheon, H.-W. Use of Information and Communication Technology by South Korean Occupational Therapists Working in Hospitals: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 6022. https://doi.org/10.3390/ijerph19106022
Hwang N-K, Shim S-H, Cheon H-W. Use of Information and Communication Technology by South Korean Occupational Therapists Working in Hospitals: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(10):6022. https://doi.org/10.3390/ijerph19106022
Chicago/Turabian StyleHwang, Na-Kyoung, Sun-Hwa Shim, and Hye-Won Cheon. 2022. "Use of Information and Communication Technology by South Korean Occupational Therapists Working in Hospitals: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 10: 6022. https://doi.org/10.3390/ijerph19106022
APA StyleHwang, N.-K., Shim, S.-H., & Cheon, H.-W. (2022). Use of Information and Communication Technology by South Korean Occupational Therapists Working in Hospitals: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(10), 6022. https://doi.org/10.3390/ijerph19106022







