Towards Understanding Behaviour and Emotions of Children with CLN3 Disease (Batten Disease): Patterns, Problems and Support for Child and Family
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Data Analysis
- Which emotional and behavioural symptoms occur?
- +
- How do these symptoms develop?
- +
- Which circumstances or events that lead to (solutions of) these symptoms are seen?
- +
- Are there possible protective factors in the system around the child?
- What kind of support do the child and the family receive?
- With what kind of problems do the parents have to deal?
- What categories of emotional and behavioural symptoms are found?
- +
- Are there typical combinations of emotional and behavioural symptoms?
- +
- Is there a typical development of emotional and behavioural symptoms?
- +
- Are there typical circumstances or events that lead to (beginning and ending of) symptoms?
- +
- Are there commonly identified protective factors in the system around the child?
- What categories of support that the child with CLN3 disease receives can be found?
- What categories of support that the parents of a child with CLN3 disease receive can be found?
- How can the problems that these parents deal with be categorised?
3. Results
- deteriorating vision -> anxietyFor client 7 the anxiety starts at the age of 6, when also his vision deteriorates rapidly.
- declining mobility -> anxietyThe increase of anxiety of client 1 starts at the same time as a fast decline in mobility. In situations where she is standing or walking without support, she shows fear of falling.
- decline in cognitive skills (+rivalry) -> angerAs a result of the decline in cognitive skills of client 11, and the (normal) cognitive development of her younger sister, the two sisters are at the same cognitive level at some point, which leads to great rivalry and therefore great anger of client 11. When, half a year later, the younger sister has overtaken her older sister on cognitive skills, the anger and tantrums of client 11 fade away.
- decline of language skills -> angerIf client 4 cannot make clear what he wants to say and other people do not understand him, he becomes angry and agitated and raises his voice to repeat what he is saying, over and over again.
- physical decline -> sadnessClient 6 goes through periods of sadness because of the things he cannot do anymore and cries at night about this.
- cognitive decline -> sadnessClient 11 cannot remember the names of certain things, resulting in other people not understanding what she means. This makes her sad.Observed connections between CLN3 disease symptoms and behaviour:
- decline in motor skills and energy -> passivenessDue to the decline in motor skills, client 8 can do less and less things independently. She becomes increasingly passive.
- decline in energy -> less rebelliousAround the age of 20, client 4 acts less rebellious as a consequence of a decline in energy.
- Expressing in words what the environment looks like and what is happening
- Offering structure: clear daily routines, rules and boundaries
- Offer extra explanation and attention
- Clarify communication and support social contact
- Help to memorize things and to keep memories alive
- Stimulation and encouragement
- Acknowledging emotions and helping to control them
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Code | Subcode | Remarks |
|---|---|---|
| behaviour | physical aggression to others | |
| physical aggression to things | ||
| verbal aggression | ||
| self-injury | ||
| dominant | ||
| independent | including confident | |
| motivated | ||
| taking initiative | ||
| drawing attention | ||
| alert | ||
| giving reaction | for example: giving reaction when recognizing something | |
| cooperative | ||
| flexible | ||
| dependent | ||
| passive | including: withdrawn, apathetic | |
| insecure | for example: asking many questions | |
| evasive | ||
| unmotivated | ||
| rebellious | including anger and tantrums | |
| inpatient | ||
| restless | ||
| crying | including being upset | |
| auditory orientation | ||
| slow pace | including delayed reactions | |
| decreased impulse control | including impulsiveness in behaviour and reaction | |
| compulsive | tics (also verbally, like keeping asking questions), including stereotypical/repetitive behaviour | |
| obsessive | including rigidity and difficulty of letting go of subject | |
| focus on the familiar | including clinging to the past and to certainties | |
| focus on simple things | including preferring contact with younger children | |
| excessive talking | ||
| touching/groping | ||
| seeing behaviour | behaviour related to low vision, for example holding objects close to the face | |
| other | ||
| emotional factors | fear | |
| sadness | ||
| anger | including irritation | |
| happiness | ||
| other | ||
| physical factors | motor skills | including balance. This also includes (lack of) muscle tension. |
| visual disability | ||
| epilepsy | including psychogenic (non epileptic) seizures | |
| talking | ||
| eating | ||
| mobility | ||
| energy | ||
| toilet | everything having to do with toilet visits, incontinence, bowel movements, etc. | |
| sleeping | ||
| physical discomfort | for example pain and bedsores | |
| other | ||
| cognitive factors | memory | |
| attention | including concentration and awareness | |
| language | understanding of language and communication | |
| executive functioning | cognitive skills, e.g., planning, structuring, multitasking, problem solving, slowing down or initiating actions | |
| awareness of time | ||
| other | ||
| psychological factors | gloom | including depression |
| hallucination | including delusions | |
| stress | including tension | |
| high sensitivity | increased sensitivity to stimulating environments or situations | |
| confused | unable to tell a clear story | |
| other | ||
| personality factors | needs, preferences and interests | for example hobby’s |
| competence | characteristics such as perseverance, courage, resilience, but stubborn, rebellious, etc. | |
| other | ||
| development | early development | |
| learning development | ||
| puberty | ||
| other | ||
| surroundings | event | events that could impact the behaviour of the child |
| social | having to do with the social contacts of the child, including the relationship with the parents | |
| activities | daily activities, like eating, playing and activities at the care facility | |
| situation | the situation or circumstances (e.g., the state of affairs at home or at school) | |
| other | ||
| parents (support, request for help, problems) | Three different codes (parents—support, parents—request for help, parents—problems) that can be used with the same subcodes | |
| emotions | concerning the emotions of the parents, including coping and energy (fatigue, exhaustion) | |
| psychological factors | concerning psychological problems of the parents, either independent of the illness of their child or as a direct result of it (e.g., depression) | |
| psycho-education | concerning the information that is given/requested about the disease | |
| practical | concerning practical help, for example outsourcing care, safety and adjustments in the home | |
| interaction with the child | concerning for example, the communication, appropriate activities, the independence of the child, dealing with the visual impairment and providing structure (e.g., clear daily routines) | |
| interaction with care providers | the problem/cooperation/appreciation that plays a role in dealing with care providers, including differing views | |
| dealing with the situation | concerning dealing with other children in the family, relatives, how to communicate information about the disease, etc. | |
| other | ||
| child support | practical | assistance with showering, climbing stairs, getting dressed, etc., but also assistance from a physiotherapist, speech therapist, etc. |
| medication | for example for epilepsy or sleeping problems but also for behavioural problems | |
| secundary help | help or advice that is offered to someone else (eg the school or a teacher) so that the child can be guided better afterwards. | |
| structure | clear daily routines, rules, safe environment and clearly defined borders | |
| wording the environment | to express in words what the environment looks like and what is happening | |
| acknowledge/control emotions | help to steer the emotions in the right direction | |
| extra explanation/attention | for example repeating and clarifying the instruction (e.g., at school) and giving extra time, didactic but also individual attention. | |
| clarify communication | including supporting social contacts | |
| memory | help with memorizing things and helping to keep memories alive | |
| stimulation | encouragement to do something | |
| other | ||
| research result | important research results such as NCL diagnosis, stages of disease and registration of progress and deterioration |
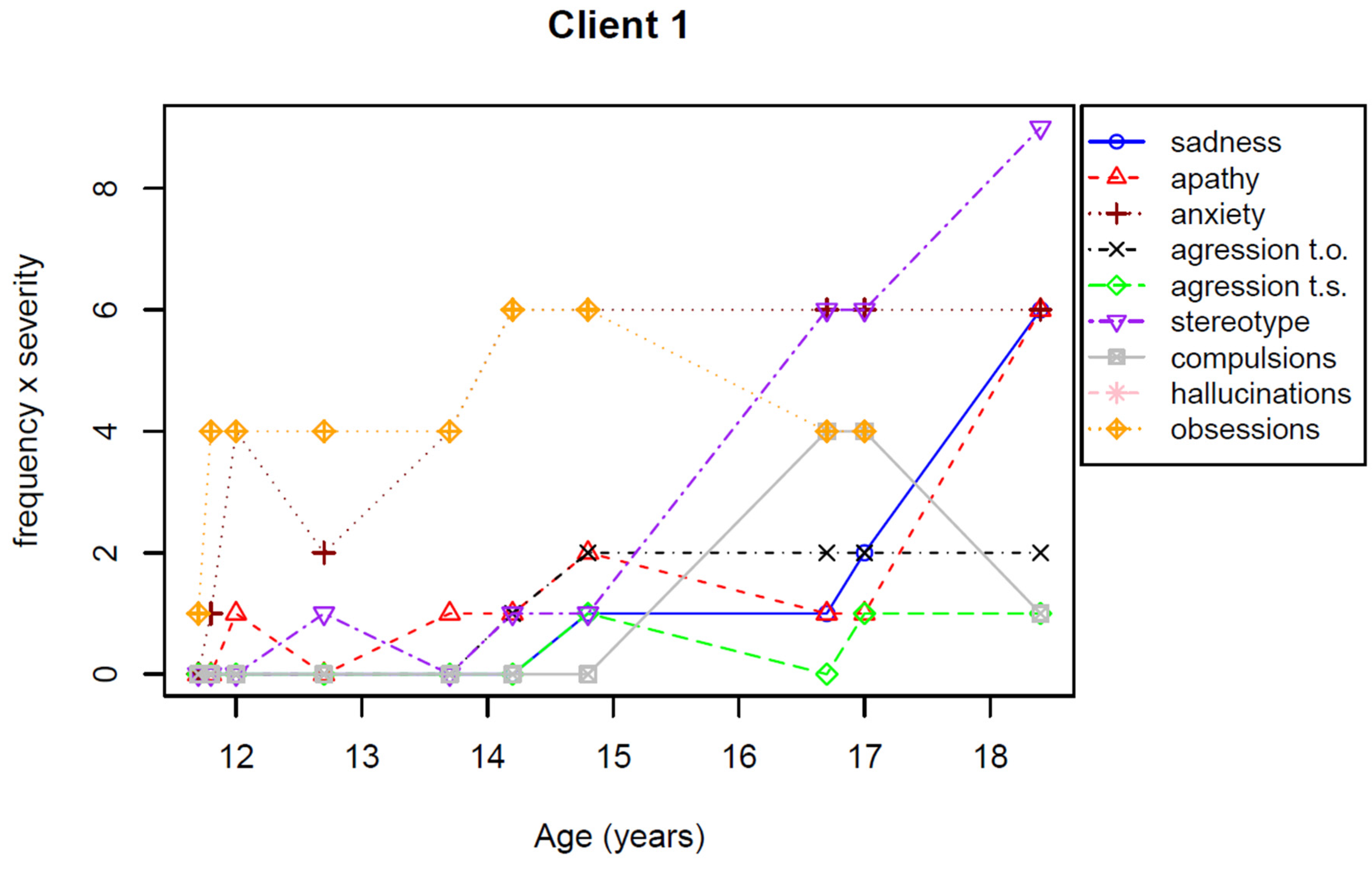
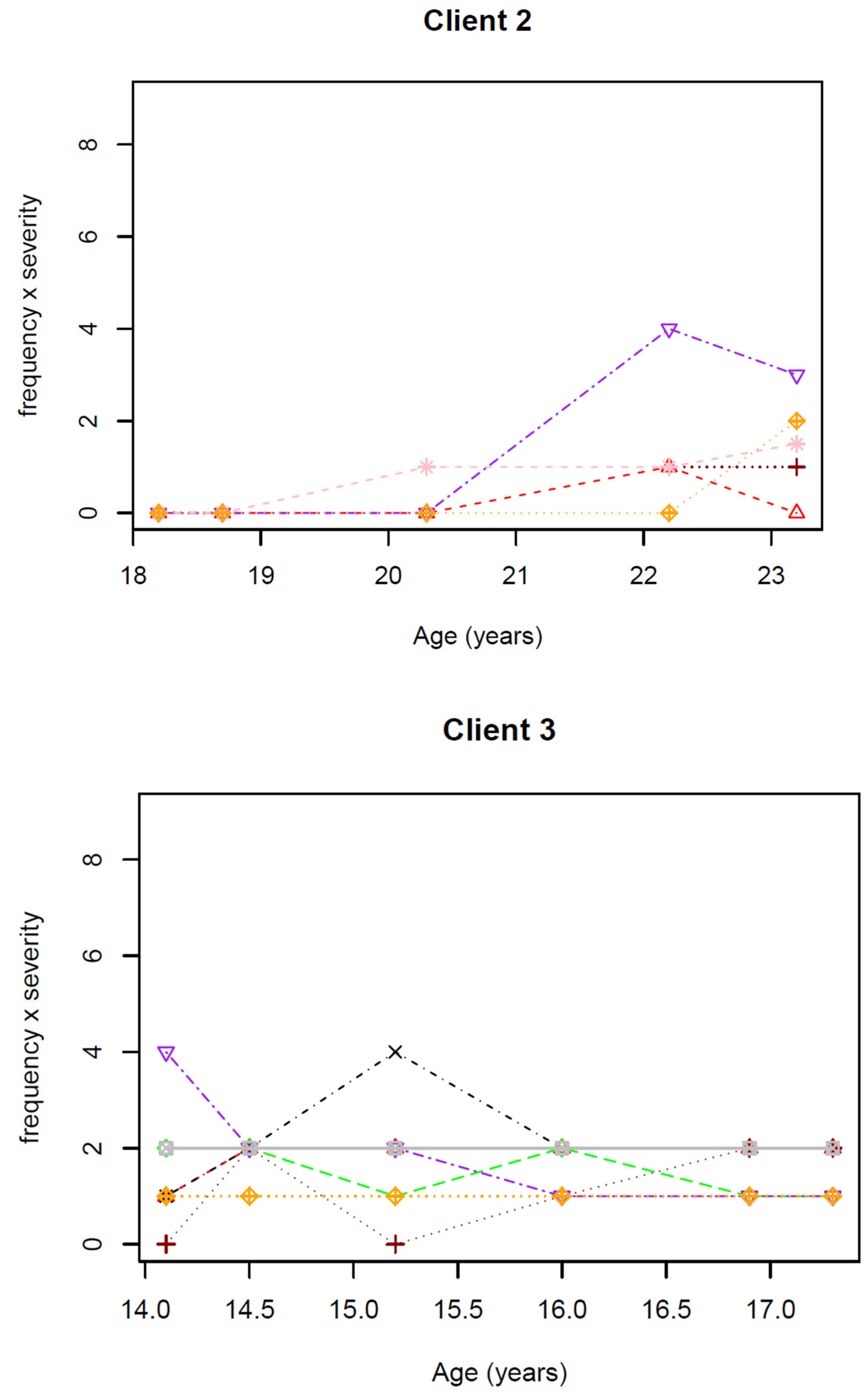
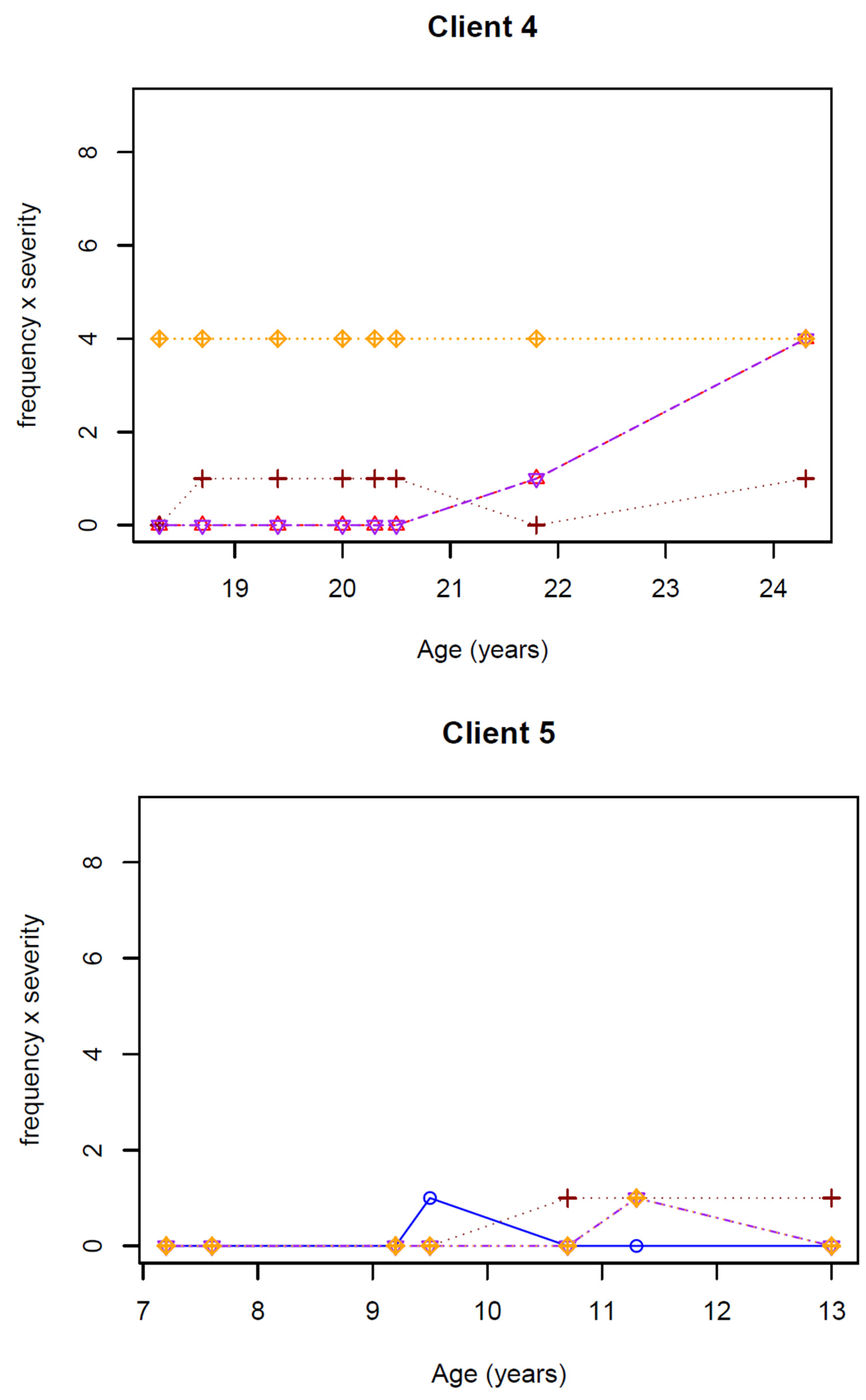
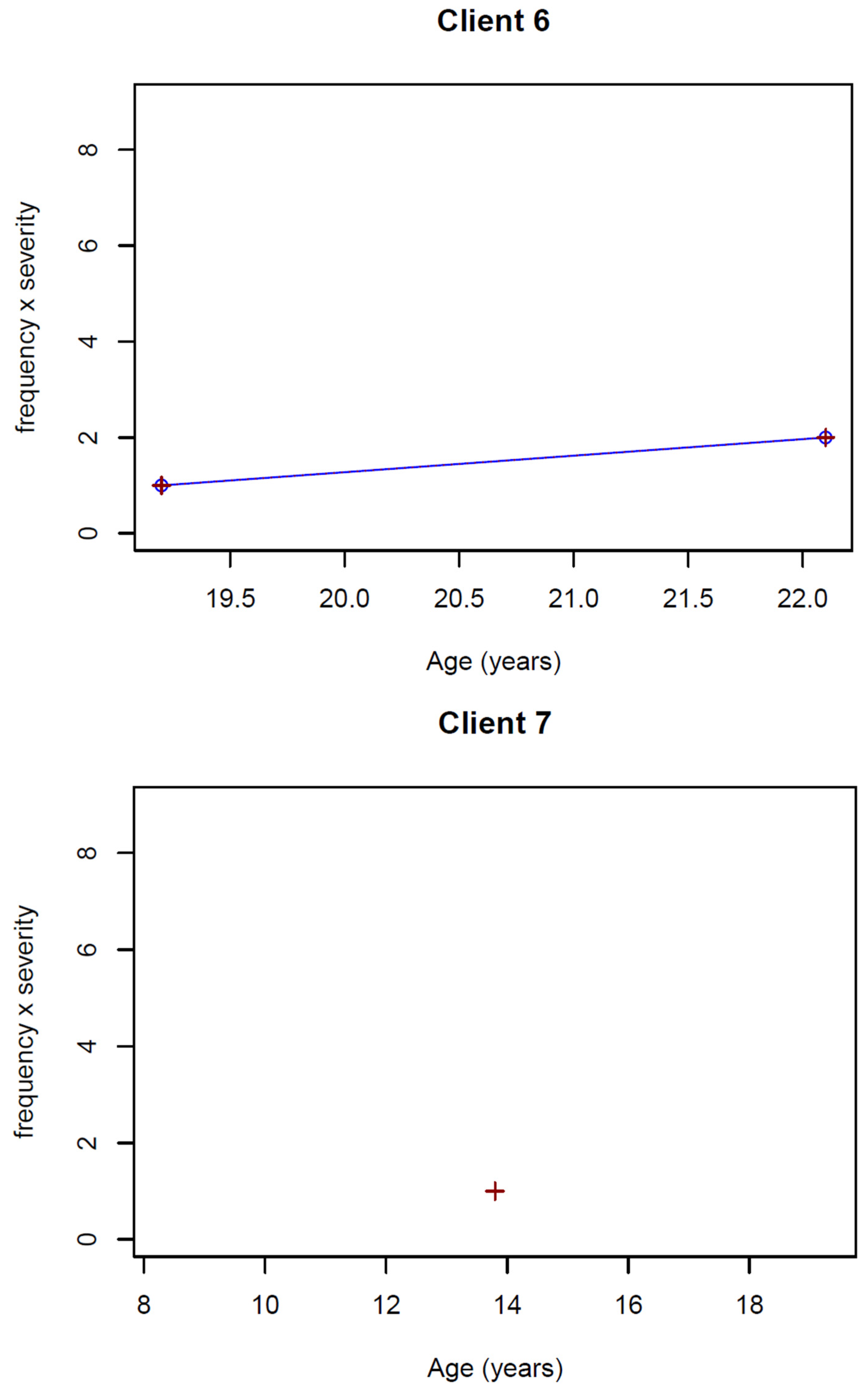
| Client | Sex | Age | Sadness | Apathy | Anxiety | Aggression t.o. | Aggression t.s. | Stereotype Behaviour | Compusions | Hallucinations | Obsessions | Medi-Cation y/n | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| f | s | f | s | f | s | f | s | f | s | f | s | f | s | f | s | f | s | ||||
| 1 | f | 11.7 11.8 12.0 12.7 13.7 14.2 14.8 16.7 17.0 18.4 | 0 0 0 0 0 0 1 1 1 2 | 0 0 0 0 0 0 1 1 2 3 | 0 0 1 0 1 1 1 1 1 2 | 0 0 1 0 1 1 2 1 1 3 | 0 1 2 1 2 2 2 2 2 2 | 0 1 2 2 2 3 3 3 3 3 | 0 0 0 0 0 1 1 1 1 1 | 0 0 0 0 0 1 2 2 2 2 | 0 0 0 0 0 0 1 1 1 1 | 0 0 0 0 0 0 1 0 1 1 | 0 0 0 1 0 1 1 2 2 3 | 0 0 0 1 0 1 1 3 3 3 | 0 0 0 0 0 0 0 2 2 1 | 0 0 0 0 0 0 0 2 2 1 | 0 0 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 0 0 | 1 2 2 2 2 2 2 2 2 | 1 2 2 2 2 3 3 2 2 | y y y y y y y y y y |
| 2 | m | 18.2 18.7 20.3 22.2 23.2 | 0 0 0 0 0 | 0 0 0 0 0 | 0 0 1 1 0 | 0 0 0 1 0 | 0 0 1 1 1 | 0 0 1 1 | 0 0 0 0 0 | 0 0 0 0 0 | 0 0 0 0 0 | 0 0 0 0 | 0 0 2 2 1.5 | 0 0 0 2 2 | 0 0 0 0 0 | 0 0 0 0 0 | 0 0 1 1 1 | 0 0 1 1 1.5 | 0 0 0 0 1 | 0 0 0 0 2 | n n n n |
| 3 | m | 14.1 14.5 15.2 16.0 16.9 17.3 | 0 0 0 0 0 0 | 0 0 0 0 0 0 | 1 1 1 1 1 1 | 1 2 2 2 2 2 | 0 1 0 1 1 1 | 0 2 0 1 2 2 | 1 1 2 1 1 1 | 1 2 2 2 2 2 | 1 1 1 1 1 1 | 2 2 1 2 1 1 | 2 1 1 1 1 1 | 2 2 2 1 1 1 | 1 1 1 1 1 1 | 2 2 2 2 2 2 | 0 0 0 0 0 0 | 0 0 0 0 0 0 | 1 1 1 1 1 1 | 1 1 1 1 1 1 | y y y y y y |
| 4 | m | 18.3 18.7 19.4 20.0 20.3 20.5 21.8 24.3 | 0 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 0 | 0 0 0 0 0 0 1 2 | 0 0 0 0 0 0 1 2 | 0 1 1 1 1 1 0 1 | 0 1 1 1 1 1 0 1 | 0 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 0 | 0 0 0 0 0 0 1 2 | 0 0 0 0 0 0 1 2 | 0 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 0 | 2 2 2 2 2 2 2 2 | 2 2 2 2 2 2 2 2 | y y y y y y y n |
| 5 | m | 7.2 7.6 9.2 9.5 10.7 11.3 13.0 | 0 0 0 1 0 0 0 | 0 0 0 1 0 0 0 | 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 | 0 0 0 0 1 1 1 | 0 0 0 0 1 1 1 | 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 | 0 0 0 0 0 1 0 | 0 0 0 0 0 1 0 | 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 | 0 0 0 0 0 0 0 | 0 0 0 0 0 1 0 | 0 0 0 0 0 1 0 | n n n n n n n |
| 6 | m | 19.2 22.1 | 1 1 | 1 2 | 0 0 | 0 0 | 1 1 | 1 2 | 0 0 | 0 0 | 0 0 | 0 0 | 0 0 | 0 0 | 0 0 | 0 0 | 0 0 | 0 0 | 0 0 | 0 0 | y y |
| 7 | m | 13.8 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | y |
| Sad Mood | Apathy | Anxiety | Aggression towards Others | Aggression towards Self | Stereotype/Repetitive Behaviour | Compulsions | Auditory Illusions | Obsessions | |
|---|---|---|---|---|---|---|---|---|---|
| number of clients who experience this (total = 7) | 3 (43%) | 4 (57%) | 7 (100%) | 2 (29%) | 2 (29%) | 5 (71%) | 2 (29%) | 1 (14%) | 5 (71%) |
References
- Geraets, R.D.; Hastings, M.L.; Kielian, T.; Pearce, D.A.; Weimer, J.M. Moving towards effective therapeutic strategies for Neuronal Ceroid Lipofuscinosis. Orphanet J. Rare Dis. 2016, 11, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mink, J.W.; Augustine, E.F.; Adams, H.R.; Marshall, F.J.; Kwon, J.M. Classification and natural history of the neuronal ceroid lipofuscinoses. J. Child Neurol. 2013, 28, 1101–1105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MedLinePlus. CLN3 Disease. Available online: https://medlineplus.gov/genetics/condition/cln3-disease/#frequency (accessed on 26 April 2022).
- Bartiméus. NCL. Available online: https://www.bartimeus.nl/expertise/het-ontwikkelen-van-onze-expertise/ncl (accessed on 26 April 2022).
- Østergaard, J.R. Juvenile neuronal ceroid lipofuscinosis (Batten disease): Current insights. Degener. Neurol. Neuromuscul. Dis. 2016, 6, 73–83. [Google Scholar] [CrossRef] [Green Version]
- Johnson, T.B.; Cain, J.T.; White, K.A.; Ramirez-Montealegre, D.; Pearce, D.A.; Weimer, J.M. Therapeutic landscape for Batten disease: Current treatments and future prospects. Nat. Rev. Neurol. 2019, 15, 161–178. [Google Scholar] [CrossRef] [PubMed]
- Mole, S.E.; Anderson, G.; Band, H.A.; Berkovic, S.F.; Cooper, J.D.; Kleine Holthaus, S.; McKay, T.R.; Medina, D.L.; Rahim, A.A.; Schulz, A.; et al. Clinical challenges and future therapeutic approaches for neuronal ceroid lipofuscinosis. Lancet Neurol. 2018, 18, 107–116. [Google Scholar] [CrossRef]
- Mirza, M.; Vainshtein, A.; DiRonza, A.; Chandrachud, U.; Haslett, L.J.; Palmieri, M.; Storch, S.S.; Groh, J.; Dobzinski, N.; Napolitano, G.; et al. The CLN3 gene and protein: What we know. Mol. Genet. Genom. Med. 2019, 7, e859. [Google Scholar] [CrossRef] [PubMed]
- Anderson, G.W.; Goebel, H.H.; Simonati, A. Human pathology in NCL. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2013, 1832, 1807–1826. [Google Scholar] [CrossRef] [Green Version]
- Adams, H.; de Blieck, E.A.; Mink, J.W.; Marshall, F.J.; Kwon, J.; Dure, L.; Rothberg, P.G.; Ramirez-Montealegre, D.; Pearce, D.A. Standardized assessment of behavior and adaptive living skills in juvenile neuronal ceroid lipofuscinosis. Dev. Med. Child Neurol. 2006, 48, 259–264. [Google Scholar] [CrossRef]
- Kuper, W.F.E.; van Alfen, C.; Rigterink, R.H.; Fuchs, S.A.; van Genderen, M.M.; van Hasselt, P.M. Timing of cognitive decline in CLN3 disease. J. Inherit. Metab. Dis. 2018, 41, 257–261. [Google Scholar] [CrossRef] [Green Version]
- Kuper, W.F.E.; van Alfen, C.; van Eck, L.; Huijgen, B.C.H.; Nieuwenhuis, E.E.S.; van Brussel, M.; van Hasselt, P.M. Motor function impairment is an early sign of CLN3 disease. Neurology 2019, 93, e293–e297. [Google Scholar] [CrossRef]
- Adams, H.R.; Beck, C.A.; Levy, E.; Jordan, R.; Kwon, J.M.; Marshall, F.J.; Mink, J.W. Genotype does not predict severity of behavioural phenotype in juvenile neuronal ceroid lipofuscinosis (Batten disease). Dev. Med. Child Neurol. 2010, 52, 637–643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, H.; Kwon, J.; Marshall, F.J.; de Blieck, E.A.; Pearce, D.A.; Mink, J.W. Neuropsychological symptoms of Juvenile-onset Batten disease: Experiences from two studies. J. Child Neurol. 2007, 22, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Bäckman, M.L.; Santavuori, P.R.; Åberg, L.E.; Aronen, E.T. Psychiatric symptoms of children and adolescents with juvenile neuronal ceroid lipofuscinosis. J. Intellect. Disabil. Res. 2005, 49, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Adams, H.R.; Mink, J.W.; University of Rochester Batten Center Study Group. Neurobehavioral features and natural history of juvenile neuronal ceroid lipofuscinosis (Batten disease). J. Child Neurol. 2013, 28, 1128–1136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Von Tetzchner, S.; Elmerskog, B.; Tossebro, A.; Rokne, S. Juvenile Neuronal Ceroid Lipofuscinosis, Childhood Dementia and Education; Snofugl Forlag: Melhus, Norway, 2019. [Google Scholar]
- Marshall, F.J.; de Blieck, E.A.; Mink, J.W.; Dure, L.; Adams, H.; Messing, S.; Rothberg, P.G.; Levy, E.; McDonough, T.; DeYoung, J.; et al. A clinical rating scale for Batten disease: Reliable and relevant for clinical trials. Neurology 2005, 65, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Santavuori, P.; Linnankivi, T.; Jaeken, J.; Vanhanen, S.-L.; Telakivi, T.; Heiskala, H. Psychological symptoms and sleep disturbances in neuronal ceroid-lipofuscinoses. J. Inherit. Metab. Dis. 1993, 16, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Baakman, B.; Niezen, R.; van Wageningen, J. Op Winst Blijven Spelen, over Kinderen en Jongeren Met JNCL; Bartimeus: Zeist, The Netherlands, 2008. [Google Scholar]
- Schulz, A.; Jain, M.; Butt, T.; Ballinger, R.; Eliasson, L.; Macey, J.; West, A. The challenges of living with and caring for a child or children affected by neuronal ceroid lipofuscinosis type 2 disease: In-depth family surveys in the United Kingdom and Germany. J. Inborn Errors Metab. Screen. 2020, 8, e20190013. [Google Scholar] [CrossRef]
- Cozart, E.J.; Augustine, E.F.; Mink, J.W.; Thatcher, A.R.; Adams, H.R. Batten disease and parents: Marital quality, support and communication. J. Intern. Child Neurol. 2017, 17, 114. [Google Scholar] [CrossRef]
- Olsman, E.; Veneberg, B.; van Alfen, C.; Touwen, D. The value of metaphorical reasoning in bioethics: An empirical-ethical study. Nurs. Ethics 2019, 26, 50–60. [Google Scholar] [CrossRef] [Green Version]
- Labbee, E.E. Emotional states and perceive family functioning of caregivers of chronically ill children. Psychol. Rep. 1996, 79, 1233–1234. [Google Scholar] [CrossRef]
- Labbee, E.E.; Lopez, I.; Murphy, L.; O’Brien, C. Optimism and psychosocial functioning in caring for children with battens and other neurological diseases. Psychol. Rep. 2002, 90, 1129–1135. [Google Scholar]
- Brehaut, J.C.; Kohen, D.E.; Garner, R.E.; Miller, A.R.; Lach, L.M.; Klassen, A.F.; Rosenbaum, P.L. Health among caregivers of children with health problems: Findings from a Canadian population-based study. Am. J. Public Health 2009, 99, 1254–1262. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M. Do the parent-child relationship and parenting behaviors differ between families with a child with and without a chronic illness? A meta-analysis. J. Pediatric Psychol. 2013, 38, 708–721. [Google Scholar] [CrossRef] [Green Version]
- Malcolm, C.; Forbat, L.; Anderson, G.; Gibson, F.; Hain, R. Challenging symptom profiles of life-limiting conditions in children: A survey of care professionals and families. Palliat. Med. 2011, 25, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Somanadhan, S.; Larkin, P.J. Parents’ experiences of living with, and caring for children, adolescents and young adults with mucopolysaccharidosis (MPS). Orphanet J. Rare Dis. 2016, 11, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zurynski, Y.; Deverell, M.; Dalkeith, T.; Johnson, S.; Christodoulou, J.; Leonard, H.; Elliott, E.J. Australian children living with rare diseases: Experiences of diagnosis and perceived consequences of diagnostic delays. Orphanet J. Rare Dis. 2017, 12, 68. [Google Scholar] [CrossRef]
- Krantz, M.; Malm, E.; Darin, N.; Sofou, K.; Savvidou, A.; Reilly, C.; Boström, P. Parental experiences of having a child with CLN3 disease (juvenile Batten disease) and how these experiences relate to family resilience. Child Care Health Dev. 2022. [Google Scholar] [CrossRef]
- Kazdin, A.E. Parent management training: Evidence, outcomes, and issues. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 1349–1356. [Google Scholar] [CrossRef]
- Elmerskog, B.; Tøssebro, A.G.; Atkinson, R.; Rokne, S.; Cole, B.; Ockelford, A.; Adams, H.R. Overview of advances in educational and social supports for young persons with NCL disorders. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 2020, 1866, 165480. [Google Scholar] [CrossRef]
- Kousi, M.; Lehesjoki, A.E.; Mole, S.E. Update of the mutation spectrum and clinical correlations of over 360 mutations in eight genes that underlie the neuronal ceroid lipofuscinoses. Hum. Mutat. 2012, 33, 42–63. [Google Scholar] [CrossRef]
- Wibbeler, E.; Nickel, M.; Schwering, C.; Schulz, A.; Mink, J.W. The Unified Batten Disease Rating Scale (UBDRS): Validation and reliability in an independent CLN3 disease sample. Eur. J. Paediatr. Neurol. 2022, 38, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Fossey, E.; Harvey, C.; McDermott, F.; Davidson, L. Understanding and evaluating qualitative research. Aust. N. Z. J. Psychiatry 2002, 36, 717–732. [Google Scholar] [CrossRef] [PubMed]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef] [Green Version]
- Goldsmith, L.J. Using Framework Analysis in Applied Qualitative Research. Qual. Rep. 2021, 26, 2061–2076. [Google Scholar] [CrossRef]
- Syed, M.; Nelson, S.C. Guidelines for establishing reliability when coding narrative data. Emerg. Adulthood 2015, 3, 375–387. [Google Scholar] [CrossRef] [Green Version]
- O’Connor, C.; Joffe, H. Intercoder reliability in qualitative research: Debates and practical guidelines. Int. J. Qual. Methods 2020, 19, 1–13. [Google Scholar] [CrossRef]
- Masten, M.C.; Williams, J.D.; Vermilion, J.; Adams, H.R.; Vierhile, A.; Collins, A.; Marshall, F.J.; Augustine, E.F.; Mink, J.W. The CLN3 Disease Staging System: A new tool for clinical research in Batten disease. Neurology 2020, 94, e2436–e2440. [Google Scholar] [CrossRef]
- Moors, A.; Fischer, M. Demystifying the role of emotion in behaviour: Toward a goal-directed account. Cogn. Emot. 2019, 33, 94–100. [Google Scholar] [CrossRef]
- Hassall, S.; Smith, D.M.; Rust, S.; Wittkowski, A. A systematic review and integrative sequential explanatory narrative synthesis: The psychosocial impact of parenting a child with a lysosomal storage disorder. J. Inherit. Metab. Dis. 2022, 45, 406–416. [Google Scholar] [CrossRef]
| Client Number | Gender | CLN3 Phenotype | Patient File (Age Range) | Interview Parents | UBDRS (Number of Periodic Measurements) |
|---|---|---|---|---|---|
| 1 | f | classic | yes (6–20) | yes | yes (10) |
| 2 | m | classic | yes (13–23) | no | yes (5) |
| 3 | m | classic | No | yes | yes (6) |
| 4 | m | classic | yes (8–22) | yes | yes (8) |
| 5 | m | protracted | yes (6–14) | yes | yes (7) |
| 6 (brother of 3) | m | classic | No | yes | yes (2) |
| 7 | m | classic | yes (6–13) | no | yes (1) |
| 8 | f | protracted | yes (6–22) | yes | no |
| 9 | m | classic | yes (7–10) | no | no |
| 10 | f | classic | yes (6–18) | no | no |
| 11 | f | classic | no | yes | no |
| Symptoms | Clients + Examples |
|---|---|
| Anxiety | Several examples of anxiety were found, some in relation to motor skills (1—afraid to fall) or vision (1—unexpected sounds), and others more general (5—fear for unknown things, 7—afraid at night or fear in the playground). |
| Sadness | Sadness about failing communication skills (11) and sadness about physical deterioration (6) was noticed. Delayed sadness, where the emotion comes only the next morning was repeatedly found for one client (1). Old songs that one client used to sing along with, make her sad at later age (1). |
| Rebellious | At home, some clients explore their boundaries (9) or get angry quickly (10). Not being understood was found to give rise to angry behaviour (4), as well as having to do things that one does not want to (8). |
| Aggression | Yelling and screaming was found to occur when getting angry or frustrated (1, 3); sometimes aggression towards others (1—pushing others), but also to the self was reported (1—hits herself when having an episode). Aggression towards things was also seen (3—trying to destroy things). In one case, rivalry between sisters (the younger sister levelling the cognitive skills of a client at some point) led to aggression (11). |
| Demanding | Demanding and claiming behaviour was seen towards parents and siblings (5, 8, 10) as well as dominant and demanding behaviour in general (4). |
| Focussing on the familiar | Several clients have a preference for familiar things, activities and rituals (1, 4, 5, 7, 8), including familiar topics in conversations (4). |
| Obsession | Several obsessions were reported, like obsessions with hair (1), soccer (2), ‘Sinterklaas’ (3), clothes with pictures of horses on it (11), stones and steam engines (4). |
| Stereotypical and compulsive behaviour | Several clients have lost inhibition with respect to talking (1, 2, 4, 5, 6, 8). They can go on and on about things and focus on the specific topics of their interest. Inappropriate behaviour in puberty was also noticed (4—touching ‘accidentally’ women’s breasts), as well as stubbornly continuing with something that is not possible anymore (11—typing letters to a friend). |
| Passive | Taking less initiative, preferring to listen while others talk and making less contact is seen with clients in a later stage of the disease (1, 2, 8), while phases of passiveness have also been noticed earlier on (need a lot of stimulation to get to an activity—10). |
| Increased sensitivity | At a certain point during the disease, some clients become more sensitive for noises or (mild) chaotic situations, like birthday parties (4, 8, 11). They get overstimulated and may even get a panic attack (8). |
| Hallucinations | For some clients, delusions and auditory hallucinations start during a later stage of the disease (2, 8), while one client was said to always have been in a fantasy world part of the time (3). |
| Type of Support | Examples |
|---|---|
| Emotional support | from partner, family, friends, health professionals, patient association and religion |
| Support for interaction with their child | advice from health professionals and other NCL-parents on providing structure, stimulation, explaining things, special toys, etc. |
| Psycho education—learning about CLN3 disease | explanation on (future) NCL-symptoms and how to deal with those, from health professionals and patient association |
| Practical support | e.g., adjustments in the house, nurses at home, financial advice, care facilities |
| Type of Problems | Examples |
|---|---|
| Emotions | Feelings of anger, sadness, despair, fairness and depression |
| Interaction with their child | How to react to strong emotions and problematic behaviour of the child? Difficult to stay patient. What to say when child asks about future? |
| Future prospect | (No) desire to know about future prospect; prepare for future. |
| Practical issues | Problems to arrange wheelchair, stairlift, parking permit, etc.; financial cuts at care facilities. |
| Energy | The care takes a lot of (physical and mental) energy and sacrifices |
| Choices with respect to CLN3 disease | e.g., choices between sheltered care facilities or care for the child at home, tube feeding, euthanasia, etc. |
| Interaction with health professionals | Disagreement with health professionals, second opinions, frustration about communication and waiting (lists) |
| Interaction with other people | Less attention for other children, relationship under pressure, losing friends because of limited time, harsh judgements from (ignorant) people |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Honingh, A.K.; Kruithof, Y.L.; Kuper, W.F.E.; van Hasselt, P.M.; Sterkenburg, P.S. Towards Understanding Behaviour and Emotions of Children with CLN3 Disease (Batten Disease): Patterns, Problems and Support for Child and Family. Int. J. Environ. Res. Public Health 2022, 19, 5895. https://doi.org/10.3390/ijerph19105895
Honingh AK, Kruithof YL, Kuper WFE, van Hasselt PM, Sterkenburg PS. Towards Understanding Behaviour and Emotions of Children with CLN3 Disease (Batten Disease): Patterns, Problems and Support for Child and Family. International Journal of Environmental Research and Public Health. 2022; 19(10):5895. https://doi.org/10.3390/ijerph19105895
Chicago/Turabian StyleHoningh, Aline K., Yvonne L. Kruithof, Willemijn F. E. Kuper, Peter M. van Hasselt, and Paula S. Sterkenburg. 2022. "Towards Understanding Behaviour and Emotions of Children with CLN3 Disease (Batten Disease): Patterns, Problems and Support for Child and Family" International Journal of Environmental Research and Public Health 19, no. 10: 5895. https://doi.org/10.3390/ijerph19105895
APA StyleHoningh, A. K., Kruithof, Y. L., Kuper, W. F. E., van Hasselt, P. M., & Sterkenburg, P. S. (2022). Towards Understanding Behaviour and Emotions of Children with CLN3 Disease (Batten Disease): Patterns, Problems and Support for Child and Family. International Journal of Environmental Research and Public Health, 19(10), 5895. https://doi.org/10.3390/ijerph19105895






