Work-Related Stress among a Cohort of Italian Long-Term Care Workers during the COVID-19 Pandemic: An Observational Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design, Setting, and Participants
2.2. Questionnaires
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| COVID-19 | Coronavirus Disease 2019 |
| LTC | Long-Term Care |
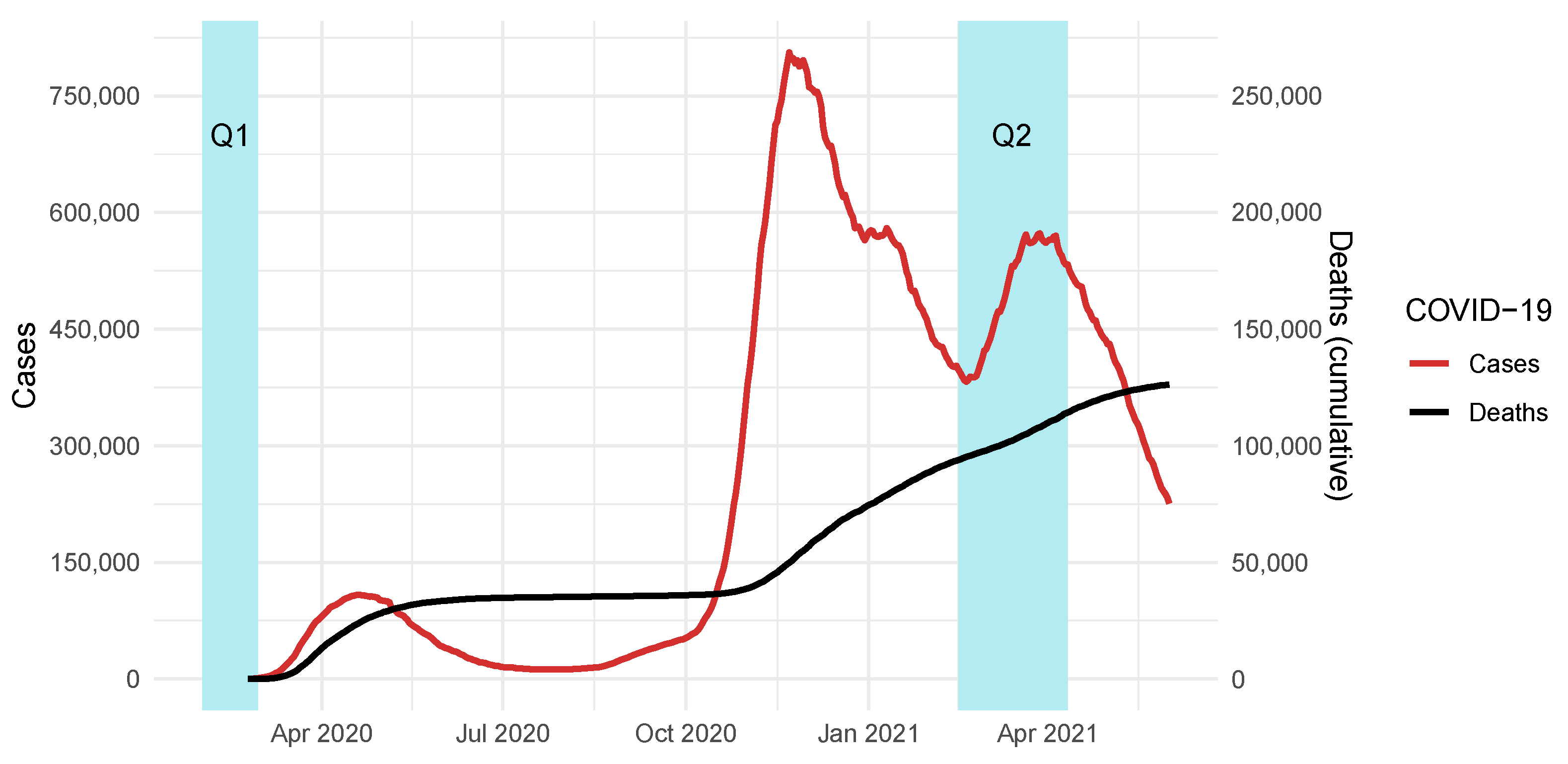
| Q1 | Questionnaire 1 |
| Q2 | Questionnaire 2 |
| PCA | Principal Component Analysis |
| KPDS | Kessler Psychological Distress Scale |
| MBI | Maslach Burnout Inventory |
| RSA | Resilience Scale for Adults |
References
- Cohen, S.; Janicki-Deverts, D.; Miller, G.E. Psychological Stress and Disease. JAMA 2007, 298, 1685. [Google Scholar] [CrossRef]
- Meng, L.B.; Zhang, Y.M.; Luo, Y.; Gong, T.; Liu, D.P. Chronic Stress A Potential Suspect Zero of Atherosclerosis: A Systematic Review. Front. Cardiovasc. Med. 2021, 8, 738654. [Google Scholar] [CrossRef]
- Liu, M.Y.; Li, N.; Li, W.A.; Khan, H. Association between psychosocial stress and hypertension: A systematic review and meta-analysis. Neurol. Res. 2017, 39, 573–580. [Google Scholar] [CrossRef]
- Lukan, J.; Bolliger, L.; Pauwels, N.S.; Luštrek, M.; Bacquer, D.D.; Clays, E. Work environment risk factors causing day-to-day stress in occupational settings: A systematic review. BMC Public Health 2022, 22, 240. [Google Scholar] [CrossRef]
- Westermann, C.; Kozak, A.; Harling, M.; Nienhaus, A. Burnout intervention studies for inpatient elderly care nursing staff: Systematic literature review. Int. J. Nurs. Stud. 2014, 51, 63–71. [Google Scholar] [CrossRef]
- G, C.P.; Krikorian, A.; Gómez-Romero, M.J.; Limonero, J.T. Resilience in Caregivers: A Systematic Review. Am. J. Hosp. Palliat. Med. 2019, 37, 648–658. [Google Scholar] [CrossRef]
- Hassard, J.; Teoh, K.R.H.; Visockaite, G.; Dewe, P.; Cox, T. The cost of work-related stress to society: A systematic review. J. Occup. Health Psychol. 2018, 23, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Dobnik, M.; Maletič, M.; Skela-Savič, B. Work-Related stress factors in nurses at Slovenian hospitals—A cross-sectional study. Slov. J. Public Health 2018, 57, 192–200. [Google Scholar] [CrossRef] [Green Version]
- Brunner, B.; Igic, I.; Keller, A.C.; Wieser, S. Who gains the most from improving working conditions? Health-related absenteeism and presenteeism due to stress at work. Eur. J. Health Econ. 2019, 20, 1165–1180. [Google Scholar] [CrossRef] [Green Version]
- Costello, H.; Walsh, S.; Cooper, C.; Livingston, G. A systematic review and meta-analysis of the prevalence and associations of stress and burnout among staff in long-term care facilities for people with dementia. Int. Psychogeriatrics 2019, 31, 1203–1216. [Google Scholar] [CrossRef]
- Hsu, H.C.; Kung, Y.W.; Huang, H.C.; Lin, Y.Y.; Chen, W.S. Work stress among nursing home care attendants in Taiwan: A questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 736–746. [Google Scholar] [CrossRef]
- Harrad, R.; Sulla, F. Factors associated with and impact of burnout in nursing and residential home care workers for the elderly. Acta Bio Medica Atenei Parm. 2018, 89, 60–69. [Google Scholar] [CrossRef]
- Fisher, E.; Cárdenas, L.; Kieffer, E.; Larson, E. Reflections from the “Forgotten Front Line”: A qualitative study of factors affecting wellbeing among long-term care workers in New York City during the COVID-19 pandemic. Geriatr. Nurs. 2021, 42, 1408–1414. [Google Scholar] [CrossRef]
- Bianchetti, A.; Rozzini, R.; Bianchetti, L.; Coccia, F.; Guerini, F.; Trabucchi, M. Dementia Clinical Care in Relation to COVID-19. Curr. Treat. Options Neurol. 2022, 24, 1–15. [Google Scholar] [CrossRef]
- Chuang, E.; Gazaway, S.; Harrell, E.R.; Elk, R. Protecting our Elders and Developing Equitable Policies During Public Health Emergencies: Ethical Recommendations. Curr. Geriatr. Rep. 2021, 10, 133–140. [Google Scholar] [CrossRef]
- Trumello, C.; Bramanti, S.M.; Ballarotto, G.; Candelori, C.; Cerniglia, L.; Cimino, S.; Crudele, M.; Lombardi, L.; Pignataro, S.; Viceconti, M.L.; et al. Psychological Adjustment of Healthcare Workers in Italy during the COVID-19 Pandemic: Differences in Stress, Anxiety, Depression, Burnout, Secondary Trauma, and Compassion Satisfaction between Frontline and Non-Frontline Professionals. Int. J. Environ. Res. Public Health 2020, 17, 8358. [Google Scholar] [CrossRef]
- Martín, J.; Padierna, A.; Villanueva, A.; Quintana, J.M. Evaluation of the mental health of care home staff in the Covid-19 era. What price did care home workers pay for standing by their patients? Int. J. Geriatr. Psychiatry 2021, 36, 1810–1819. [Google Scholar] [CrossRef]
- Riello, M.; Purgato, M.; Bove, C.; MacTaggart, D.; Rusconi, E. Prevalence of post-traumatic symptomatology and anxiety among residential nursing and care home workers following the first COVID-19 outbreak in Northern Italy. R. Soc. Open Sci. 2020, 7, 200880. [Google Scholar] [CrossRef]
- Rinaldi, C.; Bortoluzzi, S.; Airoldi, C.; Leigheb, F.; Nicolini, D.; Russotto, S.; Vanhaecht, K.; Panella, M. The Early Detection of Osteoporosis in a Cohort of Healthcare Workers: Is There Room for a Screening Program? Int. J. Environ. Res. Public Health 2021, 18, 1368. [Google Scholar] [CrossRef]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.T.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Windle, G.; Bennett, K.M.; Noyes, J. A methodological review of resilience measurement scales. Health Qual. Life Outcomes 2011, 9, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lace, J.W.; Greif, T.R.; McGrath, A.; Grant, A.F.; Merz, Z.C.; Teague, C.L.; Handal, P.J. Investigating the factor structure of the K10 and identifying cutoff scores denoting nonspecific psychological distress and need for treatment. Ment. Health Prev. 2019, 13, 100–106. [Google Scholar] [CrossRef]
- Lee, H.F. Determining Cutting Points of the Maslach Burnout Inventory for Nurses to Measure Their Level of Burnout Online. Hist. Res. 2017, 5, 1. [Google Scholar] [CrossRef] [Green Version]
- Sirigatti, S.; Stefanile, C.; Menoni, E. Per un adattamento italiano del Maslach Burnout Inventory (MBI). Boll. Psicol. Appl. 1988, 187, 33–39. [Google Scholar]
- Callegari, C.; Bertù, L.; Lucano, M.; Ielmini, M.; Braggio, E.; Vender, S. Reliability and validity of the Italian version of the 14-item Resilience Scale. Psychol. Res. Behav. Manag. 2016, 9, 277–284. [Google Scholar] [CrossRef] [Green Version]
- Benham, T.L.; Hart, A.; Bortolin, M.; Court, M.; Groves, J.; Kraus, A.; Newbury, B.; Voskanyan, A.; Yogman, M.; AlHajjaj, F.; et al. Preparing for the Second Surge: Preventing Posttraumatic Stress Disorder and Building Resilience for Health Care Workers in the Face of COVID-19. Disaster Med. Public Health Prep. 2020, 1–4. [Google Scholar] [CrossRef]
- Gee, P.M.; Weston, M.J.; Harshman, T.; Kelly, L.A. Beyond Burnout and Resilience: The Disillusionment Phase of COVID-19. AACN Adv. Crit. Care 2022, e1–e9. [Google Scholar] [CrossRef]
- Ju, G.; Lee, J.; Ahn, M.H.; Lee, J.; Kim, E.J.; Suh, S.; Chung, S. Effects of Depression and Resilience of Public Workers on Work-related Stress and Anxiety in Response to the COVID-19 Pandemic. J. Korean Med. Sci. 2021, 36, e262. [Google Scholar] [CrossRef]
- Franza, F.; Basta, R.; Pellegrino, F.; Solomita, B.; Fasano, V. The Role of Fatigue of Compassion, Burnout and Hopelessness in Healthcare: Experience in the Time of COVID-19 Outbreak. Psychiatr. Danub. 2020, 32, 10–14. [Google Scholar]
- Ruiz-Fernández, M.D.; Ramos-Pichardo, J.D.; Ibáñez-Masero, O.; Cabrera-Troya, J.; Carmona-Rega, M.I.; Ortega-Galán, A.M. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J. Clin. Nurs. 2020, 29, 4321–4330. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Kang, L.; Ma, S.; Chen, M.; Yang, J.; Wang, Y.; Li, R.; Yao, L.; Bai, H.; Cai, Z.; Xiang Yang, B.; et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 2020, 87, 11–17. [Google Scholar] [CrossRef]
- Gruber, E.M.; Zeiser, S.; Schröder, D.; Büscher, A. Workforce issues in home- and community-based long-term care in Germany. Health Soc. Care Community 2021, 29, 746–755. [Google Scholar] [CrossRef]
- Jirkovská, B.; Janečková, H. Workplace stress and employees’ well-being: Evidence from long-term care in the Czech Republic. Cent. Eur. J. Public Health 2019, 27, 87–92. [Google Scholar] [CrossRef] [Green Version]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The Psychological Impact of the SARS Epidemic on Hospital Employees in China: Exposure, Risk Perception, and Altruistic Acceptance of Risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef]
- Benfante, A.; Tesio, V.; Di Tella, M.; Romeo, A.; Castelli, L. From the First to the Second Wave of COVID-19: Anxiety, De-Pressive, and Post-Traumatic Stress Symptoms in the Italian Population. Int. J. Environ. Res. Public Health 2022, 19, 1239. [Google Scholar] [CrossRef]
- Shi, L.; Singh, D.A. Essentials of the U.S. Health Care System, 4th ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2017. [Google Scholar]
- Jessoula, M.; Pavolini, E.; Raitano, M.; Marcello, N. ESPN Thematic Report on Challenges in Long-Term Care; Technical Report; European Commission: Brussels, Belgium, 2018. [Google Scholar]
- Lapane, K.; Hughes, C. Considering the Employee Point of View: Perceptions of Job Satisfaction and Stress Among Nursing Staff in Nursing Homes. J. Am. Med. Dir. Assoc. 2007, 8, 8–13. [Google Scholar] [CrossRef]
- Barr, C.D.; Spitzmüller, C.; Stuebing, K.K. Too stressed out to participate? Examining the relation between stressors and survey response behavior. J. Occup. Health Psychol. 2008, 13, 232–243. [Google Scholar] [CrossRef]
- Shih, T.H.; Fan, X. Comparing Response Rates from Web and Mail Surveys: A Meta-Analysis. Field Methods 2008, 20, 249–271. [Google Scholar] [CrossRef]
- Tennant, C. Work-related stress and depressive disorders. J. Psychosom. Res. 2001, 51, 697–704. [Google Scholar] [CrossRef]
- Andel, R.; Crowe, M.; Hahn, E.A.; Mortimer, J.A.; Pedersen, N.L.; Fratiglioni, L.; Johansson, B.; Gatz, M. Work-Related Stress May Increase the Risk of Vascular Dementia. J. Am. Geriatr. Soc. 2012, 60, 60–67. [Google Scholar] [CrossRef] [Green Version]
- Fishta, A.; Backé, E.M. Psychosocial stress at work and cardiovascular diseases: An overview of systematic reviews. Int. Arch. Occup. Environ. Health 2015, 88, 997–1014. [Google Scholar] [CrossRef] [Green Version]
- Chandola, T.; Brunner, E.; Marmot, M. Chronic stress at work and the metabolic syndrome: Prospective study. BMJ 2006, 332, 521–525. [Google Scholar] [CrossRef] [Green Version]
- Restrepo, J.; Lemos, M. Addressing psychosocial work-related stress interventions: A systematic review. Work 2021, 70, 53–62. [Google Scholar] [CrossRef]


| Q1 (N = 197) | Q2 (N = 308) | p-Value | |
|---|---|---|---|
| Gender (female, N, rate) | 159 (81%) | 241 (78%) | 0.57 |
| Age (years, mean, CI95%) | 44.33 (42.89–45.78) | 45.38 (44.24–46.53) | 0.17 |
| Job seniority (years, mean, CI95%) | 7.66 (6.89–8.43) | 7.05 (6.46–7.64) | 0.19 |
| Healthcare worker (N, rate) | 96 (49%) | 143 (46%) | 0.76 |
| Chronic stress (score, mean, CI95%) | 15.82 (15.01–16.64) | Not measured | - |
| Work-related stress (score, mean, CI95%) | 27.84 (25.88–29.81) | 29.08 (27.41–30.75) | 0.65 |
| Resilience (score, mean, CI95%) | 58.86 (57.86–59.87) | Not measured | - |
| Chronic Stress − (N = 86) | Chronic Stress + (N = 111) | p-Value | |
|---|---|---|---|
| Age (years, mean) | 45.40 | 43.32 | 0.21 |
| Gender (female, n, mean) | 67 (86%) | 92 (83%) | 0.47 |
| Job seniority (years, mean) | 7.62 | 7.7 | 0.83 |
| Healthcare worker (N, rate) | 69 (80%) | 71 (64%) | 0.020 |
| Resilience (score, mean) | 60.66 | 57.42 | <0.001 |
| Resilience (high vs. low, N, rate) | 63 (73%) | 53 (48%) | <0.001 |
| Work-related stress (score, mean) | 20.83 | 30.48 | <0.001 |
| Work-related stress (high vs. medium/low, N, rate) | 0 (0%) | 20 (18%) | <0.001 |
| Estimate | Std. Error | T Value | p-Value | |
|---|---|---|---|---|
| Intercept | 17.66 | 15.34 | 1.15 | 0.25 |
| Healthcare worker | −1.13 | 2.43 | −0.47 | 0.64 |
| Gender (male) | −2.36 | 2.69 | −0.88 | 0.38 |
| Chronic stress score | 1.20 | 0.25 | 4.81 | <0.001 |
| Resilience score | −0.01 | 0.22 | −0.050 | 0.96 |
| Age (years) | −0.14 | 0.12 | −1.14 | 0.26 |
| Seniority (years) | 0.05 | 0.21 | 0.24 | 0.81 |
| Question Number (Domain) | Content |
|---|---|
| 6 (D1) | I feel I do not give a constructive contribution to the organization. |
| 9 (D1) | I feel I am not doing well my job. |
| 15 (D1) | I have no faith in my professional skills. |
| 5 (D2) | I feel burned out from of my job. |
| 7 (D2) | I feel a big gap between my ambition and my job. |
| 8 (D2) | I feel less enthusiast of my job than ever before. |
| 12 (D2) | I feel frustrated by my job. |
| 13 (D2) | I feel fatigued when I get up in the morning and have to face another day on the job. |
| 1 (D3) | I feel mentally exhausted by my job. |
| 3 (D3) | An entire working days is a heavy burden for me. |
| 11 (D3) | I feel drained at the end of a working day. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Conti, A.; Russotto, S.; Opizzi, A.; Ratti, M.; Nicolini, D.; Vanhaecht, K.; Panella, M. Work-Related Stress among a Cohort of Italian Long-Term Care Workers during the COVID-19 Pandemic: An Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 5874. https://doi.org/10.3390/ijerph19105874
Conti A, Russotto S, Opizzi A, Ratti M, Nicolini D, Vanhaecht K, Panella M. Work-Related Stress among a Cohort of Italian Long-Term Care Workers during the COVID-19 Pandemic: An Observational Study. International Journal of Environmental Research and Public Health. 2022; 19(10):5874. https://doi.org/10.3390/ijerph19105874
Chicago/Turabian StyleConti, Andrea, Sophia Russotto, Annalisa Opizzi, Matteo Ratti, Daniele Nicolini, Kris Vanhaecht, and Massimiliano Panella. 2022. "Work-Related Stress among a Cohort of Italian Long-Term Care Workers during the COVID-19 Pandemic: An Observational Study" International Journal of Environmental Research and Public Health 19, no. 10: 5874. https://doi.org/10.3390/ijerph19105874
APA StyleConti, A., Russotto, S., Opizzi, A., Ratti, M., Nicolini, D., Vanhaecht, K., & Panella, M. (2022). Work-Related Stress among a Cohort of Italian Long-Term Care Workers during the COVID-19 Pandemic: An Observational Study. International Journal of Environmental Research and Public Health, 19(10), 5874. https://doi.org/10.3390/ijerph19105874









