Abstract
Background: Sports injuries have physical and psychological effects that negatively affect sports performance. Although there are data available on sports injuries in wheelchair basketball, some aspects need to be clarified, such as the location, mechanisms and risk factors for injury, which are not well described due to variations and/or a lack of definition of injury. The aim of this study was to determine epidemiological information, primary injury characteristics and affected body regions in wheelchair basketball players; Methods: The PubMed, Science Direct, Scopus, Web of Science and Google Scholar databases were used; Results: eight articles were included in this review. The shoulder was the body region most affected (N = 60; 22.1%). When divided by body segments, the upper limbs were the most affected (N = 128; 47.2%), followed by the head and/or face (N = 53; 19.5%), trunk (included spine and ribs) (N = 48; 17.8%) and lower limbs (N = 42; 15.5%); Conclusions: wheelchair basketball players suffer a large number of injuries with different characteristics that are mainly linked to biomechanics and sport. These results can be used to guide coaches in structuring training to minimize recurring injuries, in addition to assisting in the organization of medical teams in competitions.
1. Introduction
Wheelchair basketball (WB) is a Paralympic sport played by two teams of five players each, comprising players with physical impairments who can be allocated to eight different classes (1.0–4.5). The game proceeds at a fast pace, in which, the teams seek to score points in the opponent’s basket. This modality is popular worldwide and has been present in all editions of the Paralympic Games [1]. Due to being a contact sport and due to the sport’s mechanics, in which, frequent shoulder movements are performed (throwing, passing, chair touching), it is expected that this practice contributes to sports injuries.
Sports injuries have both physical and psychological effects that negatively affect sports performance. Once injured, an athlete may need to abstain from the activity, which may vary from days to months [2]. The longer the withdrawal period, the more common it is to observe detraining, as well as a loss of strength and agility. In addition, psychological conditions are also related to injuries, such as anxiety, stress, depression, fear of reinjury and low self-esteem [3]. Therefore, it is important to understand the mechanisms, impact and prevention of sports injuries in Paralympic sports.
A study performed at the London 2012 Paralympic Games observed a variation in the epidemiology of injuries between sports and drew attention to the need for specific longitudinal studies for each of the different modalities [4]. In London 2012, WB recorded 34 injuries, 65% of which were acute injuries, and 23% of which were overuse injuries [5]. In the Rio 2016 Paralympic Games, 4504 interventions were recorded, in which, 399 players were treated by the physiotherapy service. For this competition, eight WB players sought physical therapy, totaling 11 treatments [6], with traumatic injuries being the primary incidents [7].
Although several studies on Olympic sports have identified injuries [8,9,10], Paralympic sports still lack this same evidence. Even though data are available regarding sports injuries in WB [5,7], some aspects need to be clarified. To date, bit data, and details such as location, mechanisms and injury risk factors, are not well-described due to variations and/or a lack of injury definition. Therefore, the aim of this study was to conduct a systematic review of the literature to determine the epidemiological information, primary injury characteristics and body regions affected in WB players.
2. Materials and Methods
This systematic review is presented in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [11] and was registered with the International Prospective Register of Systematic Review (PROSPERO; available at: https://www.crd.york.ac.uk/PROSPERO/) accessed on 28 May 2020 (registration number: CRD42020159566) [12]. The study question and other systemic review procedures were addressed with reference to the following PICO strategy: WB players (participants) of highly competitive levels; data collection regarding sports injuries in WB (intervention); descriptive data about injury epidemiology in WB (comparison); and main characteristics of sports injuries in WB (outcomes).
The systematic search comprised observational studies, prospective or retrospective studies and cohort studies. Studies were eligible for inclusion according to the following criteria: (i) involving WB players, (ii) papers written in English and (iii) presents numerical data of WB injuries. Studies were excluded from analysis based on the following criteria: (i) duplicate studies and (ii) studies on WB that did not address the prevalence or incidence of injuries.
English language searches of the electronic databases PubMed/Medline, ScienceDirect, Scopus, Web of Science and Google Scholar. Articles were retrieved from electronic databases using the following search strategy: “wheelchair basketball” AND “injury” OR “injuries” OR “sports injury”. In the search performed on Google Scholar, the advanced search option was used to retrieve articles with the exact phrase “wheelchair basketball” and with at least one of the following words: “injury”, “injuries” or “sports injury”. These words needed to occur in the title of the manuscript. Identified articles on the systematic search were initially checked for relevance by two independent researchers (first and third authors). Articles were selected after a sequential reading of the title and abstract, always in this order. Subsequently, the researchers reviewed the full texts of potentially eligible articles. A third researcher (second author) resolved any disagreements among reviewers regarding inclusion of the study. The references of the articles were consulted to identify possible additional studies. The articles were placed in a list in an Excel spreadsheet and the duplicates were removed.
Data extraction was performed by two independent researchers (first and third authors), supported by a third researcher (second author) when necessary. Data extracted from WB injuries included type of injuries, body region injury, injury level, year of publication, objectives, sample, gender and primary outcomes.
Study quality was assessed according to STROBE-SIIS (Sports Injury and Illness Surveillance) Statement, a checklist of items for the reporting of observational studies on injury and illness in sports, which is considered an appropriate tool to assess the methodological quality of epidemiological studies of sports injuries and illness. This tool consists of 23 items that aim to evaluate the methodological rigor of studies.
3. Results
3.1. Included Studies
Initially, screening identified 873 records in the databases. After removing duplicates, 268 studies remained that were selected for title and abstract analysis, of which, 235 were removed. Full reading was conducted for 33 articles, and the inclusion and exclusion criteria were applied. From those 33 articles, 25 did not meet the inclusion criteria and were excluded. Finally, eight studies were included in the final analysis (Figure 1), the oldest being published in 1999 and the most recent being published in 2020.
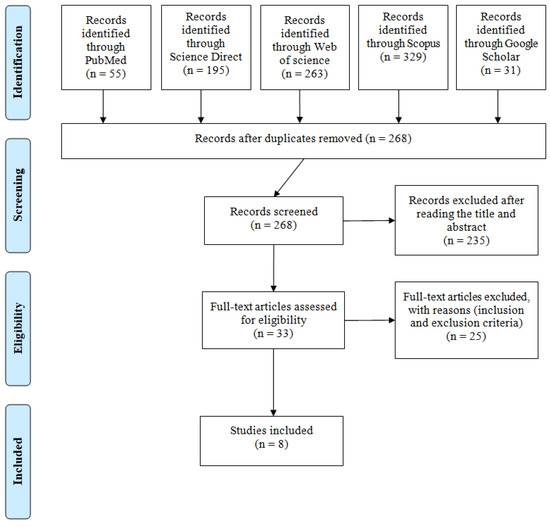
Figure 1.
PRISMA flow diagram.
3.2. Quality Assessment
In general, the articles differed little in the evaluation of methodological quality. Through analysis, we identified that the articles have good methodological quality (Appendix A).
3.3. Study Characteristics
Five papers were classified as cross-sectional observational studies, one as a descriptive self-report, one as a prospective study and one as a survey. The primary characteristics are briefly described in Table 1. Seven hundred and fifty-three WB players were included in the eight articles, 462 of whom were men and 291 of whom were women. Of the total number of players evaluated, 274 were injured players, with 271 injuries of different etiologies.

Table 1.
Description of articles.
The region of the body that presented the highest number of injuries was the shoulder (N = 60; 22.2%), followed by the head (N = 52; 19.2%), and other body regions are described in Table 2 and Figure 2. The body segment that presented the highest number of injuries was the upper limbs (N = 128; 47.2%) followed by the head and/or face (N = 53; 19.5%), trunk (spine and ribs included) (N = 48; 17.8%) and lower limbs (N = 42; 15.5%). Concussion (N = 52, 23.8%), muscle injury/contusion (N = 34; 15.5%), myalgia (N = 33; 15.1%) and pressure injuries (N = 32, 14.6%) were the primary diagnoses (Table 3).

Table 2.
Summary of injuries by body.
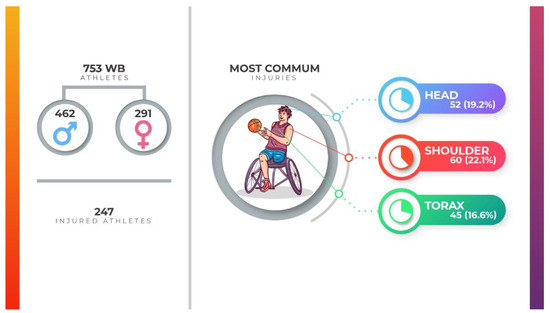
Figure 2.
Infographic of main wheelchair basketball injuries.

Table 3.
Diagnosis of injuries.
4. Discussion
The aim of this review was to determine the epidemiological information, primary injury characteristics and body regions affected in WB players. The systematic review included only quantitative studies involving 753 players of both sexes. The primary results are that 274 (36.4%) players suffered injuries, with the upper limbs being most affected (47.2%), followed by the region of the head and/or face (19.5%). Regarding established diagnoses of injuries, concussion (23.8%) followed by myalgia (15.1%) were the most reported.
The International Olympic Committee, through consensus to record and report epidemiological data on injuries and illnesses in sport in 2020, defines injury and illness as follows: injury is tissue damage or other derangement of normal physical function due to participation in sports, resulting from the rapid or repetitive transfer of kinetic energy. Illness is a complaint or disorder experienced by an athlete not related to injury [21]. In this review, most articles reported their sports injury definition, considering their research focus. Therefore, we obtained a wide variety of definitions, which makes comparison between papers’ results difficult. However, Nielsen et al. [22] argue that a single, universal definition of sports injury is not necessary but that the choice should be made to seek a balance between a variety of factors and how these factors generally compete, and the authors encourage researchers to match their choice of definition with the purpose, configuration and design of the study.
4.1. Study Populations
The studies selected for this review included 753 WB players, 462 of whom were men and 291 of whom were women. Observing this information, we identified that it is more common for articles to be composed of male samples and that the articles often do not consider gender differences when reporting injuries.
According to a study by Derman et al. (2018), female para-athletes are at higher risk of sports injuries (IR of 11.1 (95% CI 9.7 to 12.7), p < 0.05) compared to male athletes (IR of 9.3 (95% CI 8.3 to 10.4)). This may be related to a condition called “female athlete triad”, which consists of low energy availability with or without disordered eating, menstrual dysfunction and low bone density that is related to the recurrent appearance of sports injuries in women [23,24]. In addition, hormonal factors, such as differences in estrogen and relaxin activity, make women more likely to experience joint instability and ligament laxity [25,26], which can lead to injuries during sports practice.
4.2. Sports Injury Mechanism
Considering the mechanism, sports injuries can be classified into trauma (traumatic) or overload categories. Traumatic injuries are caused by a single, specific and identifiable event. They can occur with contact (e.g., shock of the body against structures or the opponent’s body) or without contact (e.g., sprain). Overload injuries are caused by repetitive microtrauma, without the identification of a specific event causing the injury. These lesions may have either a sudden or gradual onset [27]. Among the articles reviewed here, only one clearly described the mechanism of injury. A description of this point is important to understand factors that can lead to the occurrence of injuries, in addition to helping in the prevention process.
During sports practice, athletes are exposed to traumatic and overload injuries. In the case of basketball, the biomechanics of the sport itself can influence the appearance of injuries [28]. The use of the shoulder joint in repetitive movements (propulsion, throwing and passing) can cause the appearance of injuries due to overload. In the same way, sudden changes in direction during movement on the court and the shock with other players can cause the appearance of traumatic injuries. Knowing the biomechanics of the sport helps to minimize injuries and improve sports performance [29,30].
4.3. Upper Limb Injuries
With the heterogeneity in the reports, many terms were found in the papers describing injuries to the upper limbs. In summary, we categorize data of injuries in the fingers, hands, wrists, forearms/arms and shoulders into a single group: upper limb injuries.
The highest frequency of WB injuries was in the upper limb, highlighting the shoulder region. These injuries are linked to repeated movements that the sport itself requires, such as the handling of the wheelchair and the biomechanics of the throw in this position [28]. In addition, the shoulder is an anatomically unstable region, being more prone to injuries [31]. In WB, the power transmission to the pitch is with the trunk, unlike conventional basketball players, where the force starts in the lower limbs.
In the literature, shoulder injuries in wheelchair sports are primary represented by shoulder impact syndrome and rotator cuff injuries [32] that generate pain, a loss of muscle strength and a decreased range of motion, resulting in changes in biomechanics and positioning, providing muscle shortening and difficulty in performing sports and daily life tasks [28]. These injuries are related to repetitive movements and force movements performed above the head [33], activities that are present in WB practice. In addition to the shoulder region, we also highlighted injuries to the fingers, hands and wrists, which are primarily represented by fractures and sprains. In general, basketball is a contact sport and therefore promotes the appearance of these injuries, which represents a negative impact on the athlete primarily because it affects the dexterity and skill that an athlete needs to master the ball and perform movements [34].
4.4. Head Injuries
The primary head injury observed in these studies was concussion. Sport-related concussion is a traumatic brain injury induced by biomechanical forces and may be caused by either a direct blow to the head, face, neck or elsewhere on the body with an impulsive force transmitted to the head. Symptoms of neurological impairment usually appear quickly and resolve spontaneously; however, these signs and symptoms in some cases can appear over a few minutes to hours. The acute clinical signs and symptoms largely reflect a functional disturbance rather than a structural injury; therefore, no abnormalities were observed in standard structural neuroimaging exams [35,36].
The signs and symptoms of concussion include loss or not of consciousness, memory impairment, headache, nausea and vomiting, visual disturbances and eye movement, balance impairment and behavioral changes. However, signs and symptoms are not, by themselves, a diagnosis of concussion, and, for suspected diagnosis of concussion, the clinical signs and symptoms cannot be explained by drugs, alcohol, medication use, other injuries or other comorbidities [37,38]. At present, it is known that most athletes are able to recover from clinical symptoms, even in the first month after the injury, but the return to sports needs to occur gradually [36]. As previously mentioned, basketball is a contact sport, and, for this reason, the incidence rates of concussions in this sport are higher compared to low contact sports.
Intervention protocols and behaviors already exist in the literature, such as The Sports Concussion Assessment Tool 5 (SCAT5), which can be used on and off the court [37]. In addition, we emphasize that concussion prevention strategies, such as using specific equipment and changing sport-specific rules to avoid more serious contact, should be carefully considered.
4.5. Lower Limbs Injuries (Knee, Hip and Ischiatic Region)
Injuries with higher incidence found in the lower limbs included pressure sore injuries, contusions and abrasions on the skin. The appearance of pressure sore injuries is observed in players who depend on the wheelchair for their locomotion and who present sensitivity changes in areas that remain in contact with the chair, primarily ischiatic and sacrum regions; therefore, people with spinal cord injury are the most affected [16,17]. It is important to note that pressure injuries are not exclusive to athletes, but the practice of sports can be a factor that promotes their occurrence. Players with lower classifications usually have greater trunk instability and might be at risk for the occurrence of pressure injuries compared to players of higher classes who, in turn, have better postural control, since these players with lower scores do not experience posture changes, such as tilting the trunk and lowering the pressure points when sitting. These injuries present as a risk factor for poor blood circulation in the region with greater contact with the chair, pressure at specific points for long periods during the day and friction of the skin, and, within sports practice, sweat favors an environment conducive to the development of these injuries. The authors report that, if untreated, these injuries can lead to serious conditions, such as sepsis, and represent the risk of suspension from sports practice until the injury is completely healed [17].
Regarding bruises and abrasions on the skin, as has been previously indicated, WB is a contact sport where these situations can occur during the game. In certain movements, parts of the metal structure encounter the opponent’s body, which may cause these injuries.
4.6. Spinal Injuries (Cervical, Thoracic and Lumbar)
Spinal injuries do not seem to be directly related to sports practice, yet the incidence of pain in the spine region, primarily lumbar, in permanent wheelchair users is high, and this population seems to be more susceptible to the onset of this type of pain compared to the general population [38]. These pain symptoms, both acute and chronic, may be related to the ergonomic characteristics of the chair, since these users spend most of their time sitting in these chairs that might not have the necessary anatomical adjustments, resulting in pain [39]. In addition to ergonomic factors, it is also necessary to mention factors such as non-physical activity, muscle inactivity and neuropathies [38]. The prevention of this condition is important because pain negatively affects the quality of life of individuals, and the changes in positioning, the practice of physical activities and the realization of necessary ergonomic adjustments in the chair would be preventive factors for the onset of pain.
4.7. Collection Pattern
Most studies presented here do not clearly describe the characteristics of the sport injuries. Some studies that focused on different sport modalities did not individually report the number, region or diagnosis of injuries for each sport. Some of the injuries mentioned in the articles have not had their etiology or mechanism of injury studied, making it difficult to analyze whether the injury was acquired during training and games or off the court, whether the injury is prior to sports practice or not and with what mechanism. Not having this information prevents us from making coherent decisions to prevent sports injuries. Most articles defined the concepts of injuries in their publications (Table 1).
These differences demonstrate the importance of standardizing collections for studies on sports injuries. To date, there is no protocol for collecting data on injuries in wheelchair basketball, demonstrating the need to create a standard model. Clear exposure of these points is needed so that sports injury epidemiology, focusing on incidence and prevalence, have a positive impact on the literature and clinical practice [30].
In this sense, Magno and Silva [40] proposed the Sports Injury Protocol in Paralympic Sports, a sports injury data protocol in Paralympic sports that is multimodal, multi-handicap, multifactorial and accessible. This system consists of six stages: consent form, impairment data, modality data, training diary, competition diary and sports injury. Through the steps of this system, it is possible to obtain data on the characteristics of sports injuries and their internal and external factors. Determining these aspects is essential for structuring a good research methodology for sports injuries.
As previously mentioned, studies with a clear methodology enable the replication of studies and the application of results on injuries in different contexts, such as training, rehabilitation and logistics organization in sports championships.
4.8. Future Perspective
Within sports medicine, our findings contribute to the decision making of the sports team (doctors, physiotherapists, coaches, physical trainers) through the knowledge of the main injuries, where it is possible to structure training to prevent them. In this sense, the creation of an injury prevention protocol for the sport is interesting.
We have a model of success in football using the FIFA 11+ prevention protocol. Studies that evaluated the FIFA 11+ program found that the application of the protocol reduced the number of injured athletes and improved performance components, both neuromuscular and motor [41,42].
Currently, there is no protocol for the prevention of injuries in wheelchair basketball. Following the injuries highlighted in this review, a protocol aimed at this sport would have a pressure injury prevention program (this type of injury impacts training and can keep the athlete away from sports) and a sequence of exercises that simulate the sports practice aiming to improve movements and strengthen the upper limbs and core, with increasing difficulties, which could be used to warm up athletes. Strategies in this sense would decrease the risk of injury and, when there was an injury, decrease the time away from the athletes.
5. Conclusions
WB players experience several injuries with different etiologies. The largest number of injuries was observed in the upper limbs, especially in the shoulder region. An important factor in the injury process in this sport is the fact that the activity offers many contacts for its players. In this study, we determined that the most affected body regions were the shoulder, hand, head and spine. In addition, the primary diagnoses were concussions, muscle injury/contusion and myalgia. These findings can be used to direct coaches to structure training aimed at minimizing recurrent injuries in addition to helping to organize medical teams in competitions, given that sports injuries occur with greater frequency in WB.
Author Contributions
Conceptualization, K.S. and M.M.e.S.; methodology, K.S.; resources, K.S. and A.C.e.S.; writing—original draft preparation, K.S.; writing—review and editing, A.S., J.G., A.C.e.S. and M.M.e.S. All authors have read and agreed to the published version of the manuscript.
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brazil (CAPES)—Finance Code 001 and PROPESP/Federal University of Para (PAPQ).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
STROBE-SIIS (Sports Injury and Illness Surveillance) Statement 1.0—a checklist of items for the reporting of observational studies on injury and illness in sports.
| Item | Item No | Recommendation from the STROBE Statement | STROBE-SIIS Extension | Soo Hoo et al. (2018) | Shimizu et al. (2017) | Wessels et al. (2012) | Mutsuzaki et al. (2014) | Huzmeli et al. (2017) | Rocco and Saito (2006) | Curtis and Black (1999) | Hollander et al. (2020) |
| Title and abstract | 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract | Yes | Yes | Yes | No | Yes | No | Yes | Yes | |
| (b) Provide in the abstract an informative and balanced summary of what was carried out and what was found | SIIS-1.1. Include information on the sport, athlete population (sex, age, geographic region) and level of competition. SIIS-1.2. Include the duration of observation (e.g., one season, one year, multiple years). | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | ||
| Introduction | |||||||||||
| Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Objectives | 3 | State specific objectives, including any pre-specified hypotheses | SIIS-3.1. State whether study was registered. Identify the registration number and database used. SIIS-3.2. State the specific purpose of your study (e.g., to describe the injury burden associated with Olympic-level rowing) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Methods | |||||||||||
| Study design | 4 | Present key elements of study design early in the paper | SIIS-4.1. Clearly specify which health problems are being observed. SIIS-4.2. State explicitly which approach was used to record the health problem data, including all outcome measures or tools SIIS-4.3. State explicitly which coding system was used to classify the health problems (e.g., OSIICS, SMDCS, ICD, etc.) SIIS-4.4. Where relevant, clearly describe how athletes were categorized. Variables to consider could include the type of athlete and/or sport, the environment in which the sport occurs (e.g., type of course or playing area), the typical duration of the sport, the degree of physical contact permitted in the sport and the equipment permitted. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Setting | 5 | Describe the setting, locations and relevant dates, including periods of recruitment, exposure, follow-up and data collection | SIIS-5.1. Describe the location, level of play, dates of observation and data collection methods (i.e., who, what, where). SIIS-5.2. Specify the dates of the surveillance period and how the data were handled when the study covered more than one season/calendar year. SIIS-5.3. Define whether the health problem data were collected prospectively or retrospectively. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Participants | 6 | (a) Cohort study—give the eligibility criteria and the sources and methods of selection of participants. Describe methods of follow-up Case-control study—give the eligibility criteria and the sources and methods of case ascertainment and control selection. Give the rationale for the choice of cases and controls Cross-sectional study—give the eligibility criteria and the sources and methods of selection of participants | SIIS-6.1. Define the population of athletes and how they were selected and recruited. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (b) Cohort study—for matched studies, give matching criteria and number of exposed and unexposed Case-control study—for matched studies, give matching criteria and the number of controls per case | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |||
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders and effect modifiers. Give diagnostic criteria, if applicable | SIIS-7.1. Justify why you measured your primary and secondary outcomes of interest in the specific way chosen. SIIS-7.2. Describe the method for identifying your health predictor | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Data sources/measurement | 8 | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | SIIS-8.1. Specify who collected/reported the data for the study and their qualifications (e.g., qualified doctor, data analyst, etc.). SIIS-8.2. Specify who coded the data for the study and their qualifications (e.g., qualified doctor, data analyst, etc.). In many instances, this will not be the same as SIIS-8.1. SIIS-8.3. Specify the direct methods used to collect the data and the use of physical documents or any electronic tools. If extracting information from existing sources, specify the data source. SIIS-8.4. Specify the timing of and window for data collection (e.g., day health problem occurred or following day). Specify the frequency of data collection (e.g., daily, weekly, monthly). SIIS-8.5. Report the duration of surveillance (e.g., tournament, season, whole year, playing career). | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Bias | 9 | Describe any efforts to address potential sources of bias | SIIS-9.1. Clearly report any validation or reliability assessment of the data collection of tools. SIIS-9.2. Formally acknowledge any potential biases in associated with the data collection method (e.g., self- report, recall bias, reporting by nonmedically trained staff, etc.) | No | No | No | No | No | No | No | No |
| Study size | 10 | Explain how the study size was arrived at | No | Yes | Yes | Yes | Yes | No | Yes | Yes | |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | SIIS-11.1 Explain in detail how multiple injuries/illness episodes are handled both in individual athletes and across athletes/surveillance periods. SIIS-11.2. Specify how injury severity was calculated. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding | SIIS-12.1. Specify how exposure to risk has been adjusted for and specify the units (e.g., per participant, per athlete exposure, etc.). SIIS-12.2 Specify how relevant risk measures (incidence, prevalence, etc.) were calculated. SIIS-12.3. When relevant to the study aim, specify how injury occurred. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (b) Describe any methods used to examine subgroups and interactions | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |||
| (c) Explain how missing data were addressed | SIIS-12.4. For studies reporting multiple health problems, state clearly how these were handled (e.g., time to the first injury only, ignoring subsequent return to play and reinjuries, or modeling of all injuries). SIIS-12.5. Explain how/if athletes not included at outset (e.g., those already injured) were handled in the analyses. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | ||
| (d) Cohort study—if applicable, explain how loss to follow-up was addressed Case-control study—if applicable, explain how matching of cases and controls was addressed Cross-sectional study—if applicable, describe analytical methods taking account of sampling strategy | SIIS-12.6. In longitudinal studies, it is particularly important to explain how athlete follow-up has been managed. For example, what happened if a player was transferred to another team or has been censored (for those no longer part of the study due to removal during the observation period). Censoring can occur when athletes are removed due to transfer out of the team/study, injury/illness or due to study design. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | ||
| (e) Describe any sensitivity analyses | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |||
| Results | |||||||||||
| Participants | 13 | (a) Report numbers of individuals at each stage of study—e.g., numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up and analyzed | SIIS-13.1. Clearly state the number of athletes followed-up, the number (and %) of those with the health problem and the number of problems reported among them (a median number of problems per affected athlete could be useful). SIIS-13.2. For studies over multiple seasons/years, report the total numbers of health problems for each year and numbers common to each period. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (b) Give reasons for non-participation at each stage | SIIS-13.3. Report how athletes removed (e.g., due to transfer of teams or time-out due to injury or illness) impact upon data at key data collection/reporting points, ideally with a flow diagram | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | ||
| Descriptive data | 14 | (a) Give characteristics of study participants (e.g., demographic, clinical, social) and information on exposures and potential confounders | SIIS-14.1. Include detail on the level of competition being observed (e.g., by age levels, skill level, sex, etc.). | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (b) Indicate number of participants with missing data for each variable of interest | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |||
| (c) Cohort study—summarize follow-up time (e.g., average and total amount) | NA | NA | NA | NA | NA | NA | NA | NA | |||
| Outcome data | 15 | Cohort study—report numbers of outcome events or summary measures over time | SIIS-15.1. In many observational studies, individuals will sustain more than one health problem over the surveillance period. Take care to ensure descriptive data representing both the number of health problems and the number of athletes affected. It is important to represent effectively both the analysis and reporting of correct units for frequency data, i.e., the % of affected athletes or the % of injuries, body regions, etc. | NA | NA | NA | NA | NA | NA | NA | NA |
| Case-control study—report numbers in each exposure category, or summary measures of exposure | NA | NA | NA | NA | NA | NA | NA | NA | |||
| Cross-sectional study—report numbers of outcome events or summary measures | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |||
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (e.g., 95% confidence interval). Make clear which confounders were adjusted for and why they were included | SIIS-16.1. Report exposure-adjusted incidence or prevalence measures with appropriate confidence intervals when presenting risk measures. SIIS-16.2. Report details of interest, such as mode of onset | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (b) Report category boundaries when continuous variables were categorized | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | No | No | No | No | No | No | No | No | |||
| Other analyses | 17 | Report other analyses conducted—e.g., analyses of subgroups and interactions, and sensitivity analyses | SIIS-17.1 Report injury diagnosis information, including region and tissue type in tabular form. | No | No | No | No | No | No | No | No |
| Discussion | |||||||||||
| Key results | 18 | Summarize key results with reference to study objectives | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias | SIIS-19.1. Discuss limitations in the data collection and coding procedures adopted, including in relation to any risk measures calculated. | Yes | Yes | Yes | Yes | No | No | Yes | Yes |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies and other relevant evidence | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Generalizability | 21 | Discuss the generalizability (external validity) of the study results | SIIS-21.1. Discuss the generalizability of the athlete study population, and health problem subgroups of interest, to broader athlete groups. | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Other information | |||||||||||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Ethics | 23 | SIIS-23.1. Outline how individual athlete data privacy and confidentiality considerations were addressed, in line with the Declaration of Helsinki. | No | Yes | Yes | Yes | No | No | No | Yes | |
References
- IWBF History of Wheelchair Basketball. IWBF—International Wheelchair Basketball Federation. IWBF, Switzerland 2018. Available online: https://iwbf.org/the-game/history-wheelchair-basketball/ (accessed on 10 November 2020).
- Schneider, S.; Seither, B.; Tönges, S.; Schmitt, H. Sports injuries: Population based representative data on incidence, diagnosis, sequelae, and high risk groups. Br. J. Sports Med. 2006, 40, 334–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, C.-J.; Meierbachtol, A.; George, S.Z.; Chmielewski, T.L. Fear of Reinjury in Athletes. Sports Health 2017, 9, 162–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engebretsen, L.; Soligard, T.; Steffen, K.; Alonso, J.M.; Aubry, M.; Budgett, R.; Dvorak, J.; Jegathesan, M.; Meeuwisse, W.H.; Mountjoy, M.; et al. Sports injuries and illnesses during the London Summer Olympic Games 2012. Br. J. Sports Med. 2013, 47, 407–414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willick, S.E.; Webborn, N.; Emery, C.; Blauwet, C.A.; Pit-Grosheide, P.; Stomphorst, J.; Van de Vliet, P.; Marques, N.A.P.; Martinez-Ferrer, J.O.; Jordaan, E.; et al. The epidemiology of injuries at the London 2012 Paralympic Games. Br. J. Sports Med. 2013, 47, 426–432. [Google Scholar] [CrossRef]
- Macedo, C.S.G.; Tadiello, F.F.; Medeiros, L.T.; Antonelo, M.C.; Alves, M.A.F.; Mendonça, L.D. Physical Therapy Service delivered in the Polyclinic During the Rio 2016 Paralympic Games. Phys. Ther. Sport 2019, 36, 62–67. [Google Scholar] [CrossRef]
- Derman, W.; Schwellnus, M.P.; Jordaan, E.; Runciman, P.; Blauwet, C.; Webborn, N.; Lexell, J.; Van de Vliet, P.; Tuakli-Wosornu, Y.; Kissick, J.; et al. Sport, sex and age increase risk of illness at the Rio 2016 Summer Paralympic Games: A prospective cohort study of 51,198 athlete days. Br. J. Sports Med. 2018, 52, 17–23. [Google Scholar] [CrossRef] [Green Version]
- Soligard, T.; Steffen, K.; Palmer, D.; Alonso, J.M.; Bahr, R.; Lopes, A.D.; Dvorak, J.; Grant, M.-E.; Meeuwisse, W.; Mountjoy, M.; et al. Sports injury and illness incidence in the Rio de Janeiro 2016 Olympic Summer Games: A prospective study of 11274 athletes from 207 countries. Br. J. Sports Med. 2017, 51, 1265–1271. [Google Scholar] [CrossRef]
- Junge, A.; Langevoort, G.; Pipe, A.; Peytavin, A.; Wong, F.; Mountjoy, M.; Beltrami, G.; Terrell, R.; Holzgraefe, M.; Charles, R.; et al. Injuries in Team Sport Tournaments during the 2004 Olympic Games. Am. J. Sports Med. 2006, 34, 565–576. [Google Scholar] [CrossRef]
- Junge, A.; Engebretsen, L.; Mountjoy, M.L.; Alonso, J.M.; Renström, P.A.F.H.; Aubry, M.J.; Dvorak, J. Sports Injuries during the Summer Olympic Games 2008. Am. J. Sports Med. 2009, 37, 2165–2172. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Phys. Ther. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Booth, A.; Clarke, M.; Dooley, G.; Ghersi, D.; Moher, D.; Petticrew, M.; Stewart, L. The nuts and bolts of PROSPERO: An international prospective register of systematic reviews. Syst. Rev. 2012, 1, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curtis, K.A.; Black, K. Shoulder pain in female wheelchair basketball players. J. Orthop. Sports Phys. Ther. 1999, 29, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Rocco, F.M.; Saito, E.T. Epidemiology of sportive injuries in basketball wheelchair players. Acta Fisiatr 2006, 13, 17–20. [Google Scholar]
- Wessels, K.K.; Broglio, S.P.; Sosnoff, J.J. Concussions in Wheelchair Basketball. Arch. Phys. Med. Rehabil. 2012, 93, 275–278. [Google Scholar] [CrossRef]
- Mutsuzaki, H.; Tachibana, K.; Shimizu, Y.; Hotta, K.; Fukaya, T.; Karasawa, M.; Ikeda, E.; Wadano, Y. Factors associated with deep tissue injury in male wheelchair basketball players of a Japanese national team. Asia-Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2014, 1, 72–76. [Google Scholar] [CrossRef] [Green Version]
- Shimizu, Y.; Mutsuzaki, H.; Tachibana, K.; Tsunoda, K.; Hotta, K.; Fukaya, T.; Ikeda, E.; Yamazaki, M.; Wadano, Y. A survey of deep tissue injury in elite female wheelchair basketball players. J. Back Musculoskelet. Rehabil. 2017, 30, 427–434. [Google Scholar] [CrossRef]
- Huzmeli, E.D.; Katayifci, N.; Hallaceli, H. Injuries in Wheelchair Basketball Players. New Trends Issues Proc. Adv. Pure Appl. Sci. 2017, 29–35. [Google Scholar] [CrossRef] [Green Version]
- Soo Hoo, J.A.; Latzka, E.; Harrast, M.A. A Descriptive Study of Self-Reported Injury in Non-elite Adaptive Athletes. PM&R 2019, 11, 25–32. [Google Scholar] [CrossRef] [Green Version]
- Hollander, K.; Kluge, S.; Glöer, F.; Riepenhof, H.; Zech, A.; Junge, A. Epidemiology of injuries during the Wheelchair Basketball World Championships 2018: A prospective cohort study. Scand. J. Med. Sci. Sports 2020, 30, 199–207. [Google Scholar] [CrossRef] [Green Version]
- Bahr, R.; Clarsen, B.; Derman, W.; Dvorak, J.; Emery, C.A.; Finch, C.F.; Hägglund, M.; Junge, A.; Kemp, S.; Khan, K.M.; et al. International Olympic Committee consensus statement: Methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)). Br. J. Sports Med. 2020, 54, 372–389. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, R.Ø.; Shrier, I.; Casals, M.; Nettel-Aguirre, A.; Møller, M.; Bolling, C.; Bittencourt, N.F.N.; Clarsen, B.; Wedderkopp, N.; Soligard, T.; et al. Statement on Methods in Sport Injury Research from the First METHODS MATTER Meeting, Copenhagen, 2019. J. Orthop. Sports Phys. Ther. 2020, 50, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Daily, J.P.; Stumbo, J.R. Female Athlete Triad. Prim. Care 2018, 45, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Loveless, M.B. Female athlete triad. Curr. Opin. Obs. Gynecol. 2017, 29, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Saremi, H.; Yavarikia, A.; Jafari, N. Generalized Ligamentous Laxity: An Important Predisposing Factor for Shoulder Injuries in Athletes. Iran Red Crescent Med. J. 2016, 18, e38903. [Google Scholar] [CrossRef] [Green Version]
- Faryniarz, D.A.; Bhargava, M.; Lajam, C.; Attia, E.T.; Hannafin, J.A. Quantitation of estrogen receptors and relaxin binding in human anterior cruciate ligament fibroblasts. In Vitro Cell Dev. Biol. Anim. 2006, 42, 176–181. [Google Scholar] [CrossRef]
- Verhagen, E. Sports Injury Research; Van Mechelen, W., Ed.; Oxford University Press: Oxford, UK; New York, NY, USA, 2010. [Google Scholar]
- Wilroy, J.; Hibberd, E. Evaluation of a Shoulder Injury Prevention Program in Wheelchair Basketball. J. Sport Rehabil. 2018, 27, 554–559. [Google Scholar] [CrossRef]
- Morriën, F.; Taylor, M.J.D.; Hettinga, F.J. Biomechanics in Paralympics: Implications for Performance. Int. J. Sports Physiol. Perform. 2017, 12, 578–589. [Google Scholar] [CrossRef] [Green Version]
- Vanlandewijck, Y.; Theisen, D.; Daly, D. Wheelchair propulsion biomechanics: Implications for wheelchair sports. Sports Med. 2001, 31, 339–367. [Google Scholar] [CrossRef]
- Cuéllar, R.; Ruiz-Ibán, M.A.; Cuéllar, A. Anatomy and Biomechanics of the Unstable Shoulder. Open Orthop. J. 2017, 11, 919–933. [Google Scholar] [CrossRef]
- Edmonds, E.W.; Hopsital, R.C.; Diego, S. Common Conditions in the Overhead Athlete. Am. Fam. Physician 2014, 89, 5. [Google Scholar]
- Morrow, M.M.B.; Kaufman, K.R.; An, K.-N. Scapula Kinematics and Associated Impingement Risk in Manual Wheelchair Users During Propulsion and a Weight Relief Lift. Clin. Biomech. 2011, 26, 352–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morse, K.W.; Hearns, K.A.; Carlson, M.G. Return to Play after Forearm and Hand Injuries in the National Basketball Association. Orthop. J. Sports Med. 2017, 5, 2325967117690002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collins, M.W.; Kontos, A.P.; Okonkwo, D.O.; Almquist, J.; Bailes, J.; Barisa, M.; Bazarian, J.; Bloom, O.J.; Brody, D.L.; Cantu, R.; et al. Concussion is Treatable: Statements of Agreement from the Targeted Evaluation and Active Management (TEAM) Approaches to Treating Concussion Meeting held in Pittsburgh, October 15–16, 2015. Neurosurgery 2016, 79, 912–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCrory, P.; Meeuwisse, W.; Dvorak, J.; Aubry, M.; Bailes, J.; Broglio, S.; Cantu, R.C.; Cassidy, D.; Echemendia, R.J.; Castellani, R.J.; et al. Consensus statement on concussion in sport—The 5th international conference on concussion in sport held in Berlin, October 2016. Br. J. Sports Med. 2017, 51, 838–847. [Google Scholar] [PubMed] [Green Version]
- Weiler, R.; Blauwet, C.; Clarke, D.; Dalton, K.; Derman, W.; Fagher, K.; Gouttebarge, V.; Kissick, J.; Lee, K.; Lexell, J.; et al. Concussion in para sport: The first position statement of the Concussion in Para Sport (CIPS) Group. Br. J. Sports Med. 2021, 55, 1187–1195. [Google Scholar] [CrossRef]
- Kovacs, F.M.; Seco, J.; Royuela, A.; Barriga, A.; Zamora, J. Prevalence and factors associated with a higher risk of neck and back pain among permanent wheelchair users: A cross-sectional study. Spinal. Cord. 2018, 56, 392–405. [Google Scholar] [CrossRef] [Green Version]
- Li, C.-T.; Chen, Y.-N.; Chang, C.-H.; Tsai, K.-H. The Effects of Backward Adjustable Thoracic Support in Wheelchair on Spinal Curvature and Back Muscle Activation for Elderly People. PLoS ONE 2014, 9, e113644. [Google Scholar] [CrossRef]
- Silva, M.E.; Passos, M. Protocolo de Lesão Esportiva no Esporte Paralímpico (PLEEP): Proposta Para a Coleta de Dados. Sports Injuries Protocol for Paralympic Sport: Proposal for Data Acquisition. 2013. Available online: http://repositorio.unicamp.br/acervo/detalhe/917378?guid=1652035045095&returnUrl=%2fresultado%2flistar%3fguid%3d1652035045095%26quantidadePaginas%3d1%26codigoRegistro%3d917378%23917378&i=1 (accessed on 17 December 2020).
- Barengo, N.C.; Meneses-Echávez, J.F.; Ramírez-Vélez, R.; Cohen, D.D.; Tovar, G.; Bautista, J.E.C. The impact of the FIFA 11+ training program on injury prevention in football players: A systematic review. Int. J. Environ. Res. Public Health 2014, 11, 11986–12000. [Google Scholar] [CrossRef] [Green Version]
- Silvers-Granelli, H.J.; Bizzini, M.; Arundale, A.; Mandelbaum, B.R.; Snyder-Mackler, L. Does the FIFA 11+ Injury Prevention Program Reduce the Incidence of ACL Injury in Male Soccer Players? Clin. Orthop. Relat. Res. 2017, 475, 2447–2455. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).