Associations of Physical Activity, School Safety, and Non-Prescription Steroid Use in Adolescents: A Structural Equation Modeling Approach
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instrumentation
2.3. Measures
2.3.1. Non-Prescription Steroid Use
2.3.2. Physical Activity Items
2.3.3. Unsafe School Items
2.3.4. Demographic Covariates
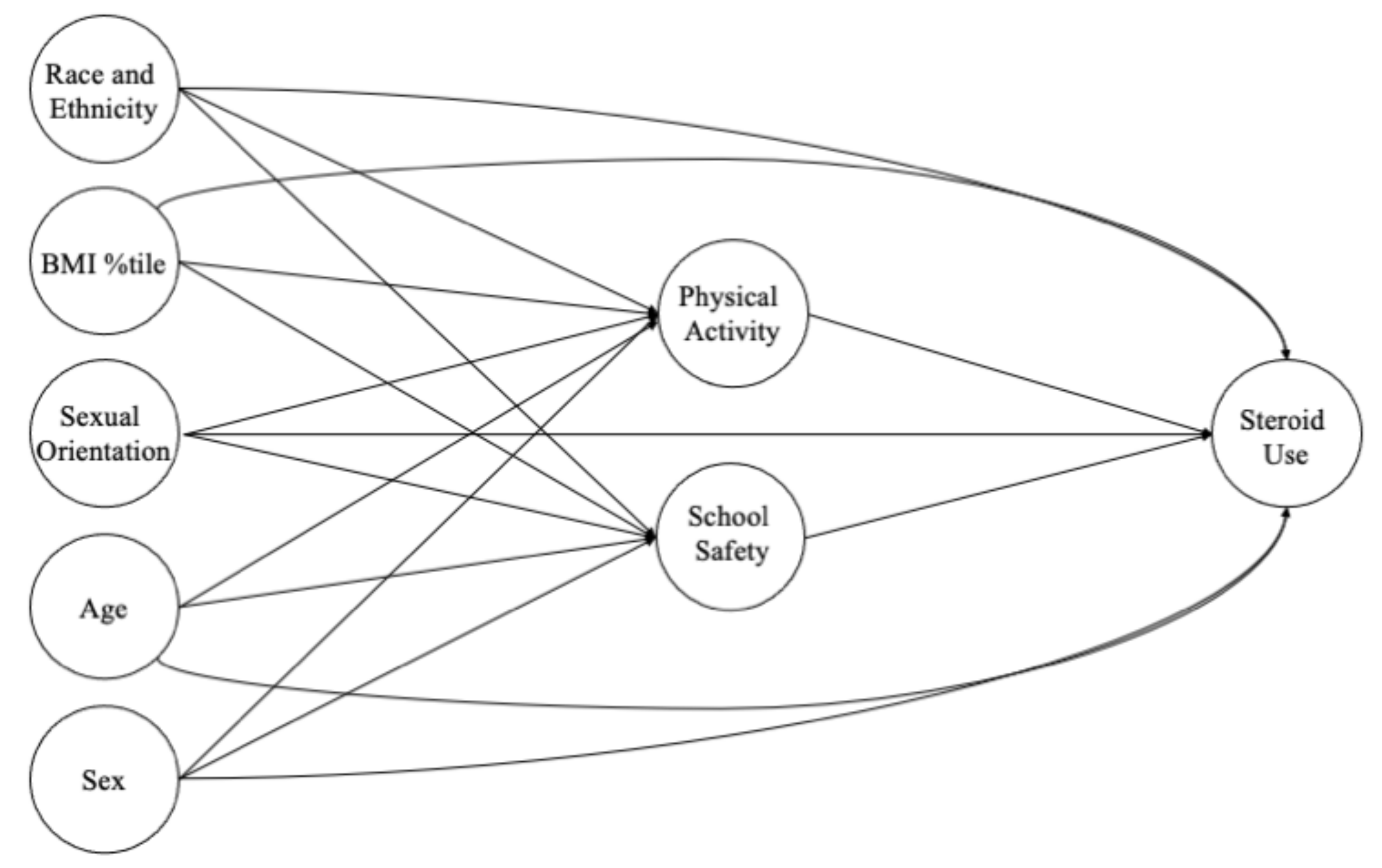
2.4. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Structural Equation Model Fit
3.3. Latent Variable Covariances
3.4. Associations with Non-Prescription Steroid Use
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Elkins, R.L.; King, K.; Nabors, L.; Vidourek, R. School and parent factors associated with steroid use among adolescents. J. Sch. Health 2017, 87, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Bahrke, M.S.; Yesalis, C.E.; Kopstein, A.N.; Stephens, J.A. Risk factors associated with anabolic-androgenic steroid use among adolescents. Sports Med. 2000, 29, 397–405. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Division of Behavioral and Social Sciences and Education; Board on Children, Youth, and Families; Committee on Applying Lessons of Optimal Adolescent Health to Improve Behavioral Outcomes for Youth. Promoting Positive Adolescent Health Behaviors and Outcomes: Thriving in the 21st Century; Kahn, N.F., Graham, R., Eds.; National Academies Press: Washington, DC, USA, 2019. [Google Scholar]
- Braams, B.R.; van Duijvenvoorde, A.C.; Peper, J.S.; Crone, E.A. Longitudinal changes in adolescent risk-taking: A comprehensive study of neural responses to rewards, pubertal development, and risk-taking behavior. J. Neurosci. 2015, 35, 7226–7238. [Google Scholar] [CrossRef] [PubMed]
- Crone, E.A.; van Duijvenvoorde, A.C.K. Multiple pathways of risk taking in adolescence. Dev. Rev. 2021, 62, 100996. [Google Scholar] [CrossRef]
- Harmer, P.A. Anabolic-androgenic steroid use among young male and female athletes: Is the game to blame? Br. J. Sports Med. 2010, 44, 26–31. [Google Scholar] [CrossRef]
- Hartgens, F.; Kuipers, H. Effects of androgenic-anabolic steroids in athletes. Sports Med. 2004, 34, 513–554. [Google Scholar] [CrossRef]
- Irving, L.M.; Wall, M.; Neumark-Sztainer, D.; Story, M. Steroid use among adolescents: Findings from Project EAT. J. Adolesc. Health 2002, 30, 243–252. [Google Scholar] [CrossRef]
- DuRant, R.H.; Escobedo, L.G.; Heath, G.W. Anabolic-steroid use, strength training, and multiple drug use among adolescents in the United States. Pediatrics 1995, 96, 23–28. [Google Scholar] [CrossRef]
- Yesalis, C.E.; Kennedy, N.J.; Kopstein, A.N.; Bahrke, M.S. Anabolic-androgenic steroid use in the United States. JAMA 1993, 270, 1217–1221. [Google Scholar] [CrossRef]
- Middleman, A.B.; Faulkner, A.H.; Woods, E.R.; Emans, S.J.; DuRant, R.H. High-risk behaviors among high school students in Massachusetts who use anabolic steroids. Pediatrics 1995, 96, 268–272. [Google Scholar] [CrossRef]
- Miller, K.E.; Barnes, G.M.; Sabo, D.F.; Melnick, M.J.; Farrell, M.P. Anabolic-Androgenic steroid use and other adolescent problem behaviors: Rethinking the male athlete assumption. Sociol. Perspsectives 2002, 45, 467–489. [Google Scholar] [CrossRef]
- Mulcahey, M.K.; Schiller, J.R.; Hulstyn, M.J. Anabolic steroid use in adolescents: Identification of those at risk and strategies for prevention. Phys. Sportsmed. 2010, 38, 105–113. [Google Scholar] [CrossRef]
- Kutsyuruba, B.; Klinger, D.A. Relationships among school climate, school safety, and student achievement and well-being: A review of literature. Rev. Educ. 2015, 3, 103–135. [Google Scholar] [CrossRef]
- Wong, M.D.; Coller, K.M.; Dudovitz, R.N.; Kennedy, D.P.; Buddin, R.; Shapiro, M.F.; Kataoka, S.H.; Brown, A.F.; Tseng, C.-H.; Bergman, P.; et al. Successful schools and risky behaviors among low-income adolescents. Pediatrics 2014, 134, e389–e396. [Google Scholar] [CrossRef] [Green Version]
- Dimitrova, E.; Kotzeva, T.; Alexandrova-Karamanova, A. Psychosocial school environment and health risk behaviours of adolescents in Bulgaria: Results from multilevel analysis. Int. J. Public Health 2020, 65, 1331–1344. [Google Scholar] [CrossRef]
- Bosworth, K.; Ford, L.; Hernandaz, D. School climate factors contributing to student and faculty perceptions of safety in select Arizona schools. J. Sch. Health 2011, 81, 194–201. [Google Scholar] [CrossRef]
- Astor, R.A.; Benbenishty, R.; Zeira, A.; Vinokur, A. School climate, observed risky behaviors, and victimization as predictors of high school students’ fear and judgments of school violence as a problem. Health Educ. Behav. 2002, 29, 716–736. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Methodology of the Youth Risk Behavior Surveillance System-2013. MMWR Recomm. Rep. 2013, 62, 1–20. [Google Scholar]
- Brener, N.D.; Colluns, J.L.; Kann, L.; Warren, C.W.; Williams, B.I. Reliability of the Youth Risk Behavior Survey questionnaire. Am. J. Epidemiol. 1995, 141, 575–580. [Google Scholar] [CrossRef]
- Blashill, A.J.; Calzo, J.P.; Griffiths, S.; Murray, S.B. Anabolic steroid misuse among US adolescent boys: Disparities by sexual orientation and race/ethnicity. Am. J. Public Health 2017, 107, 319–321. [Google Scholar] [CrossRef]
- Kann, L.; McManus, T.; Harris, W.A.; Shanklin, S.L.; Flint, K.H.; Hawkins, J.; Queen, B.; Lowry, R.; Olsen, E.O.; Chyen, D.; et al. Youth Risk Behavior Surveillance—United States, 2015. MMWR 2016, 65, 1–174. [Google Scholar] [CrossRef]
- Kann, L.; McManus, T.; Harris, W.A.; Shanklin, S.L.; Flint, K.H.; Queen, B.; Lowry, R.; Chyen, D.; Whittle, L.; Thornton, J.; et al. Youth Risk Behavior Surveillance—United States, 2017. MMWR 2018, 67, 1–114. [Google Scholar] [CrossRef]
- Underwood, J.M.; Brener, N.; Thornton, J.; Harris, W.A.; Bryan, L.N.; Shanklin, S.L.; Deputy, N.; Roberts, A.M.; Queen, B.; Chyen, D.; et al. Overview and Methods for the Youth Risk Behavior Surveillance System—United States, 2019. MMWR Suppl. 2020, 69, 1–10. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.; Shi, D. A comparison of full information maximum likelihood and multiple imputation in structural equation modeling with missing data. Psychol. Methods 2021, 26, 466–485. [Google Scholar] [CrossRef] [PubMed]
- MacCallum, R.C.; Browne, M.W.; Sugawara, H.M. Power analysis and determination of sample size for covariance structure modeling. Psychol. Methods 1996, 1, 130–149. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Xia, Y.; Yang, Y. RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: The story they tell depends on the estimation methods. Behav. Res. 2019, 51, 409–428. [Google Scholar] [CrossRef]
- Sandvik, M.R.; Bakken, A.; Loland, S. Anabolic-androgenic steroid use and correlates in Norwegian adolescents. Eur. J. Sport Sci. 2018, 18, 903–910. [Google Scholar] [CrossRef]
- DuRant, R.H.; Rickert, V.I.; Ashworth, C.S.; Newman, C.; Slavens, G. Use of multiple drugs among adolescents who use anabolic steroids. N. Engl. J. Med. 1993, 328, 922–926. [Google Scholar] [CrossRef]
- Cohen, J.; Collins, R.; Darkes, J.; Gwartney, D. A league of their own: Demographics, motivations and patterns of use of 1955 male adult non-medical anabolic steroid users in the United States. J. Int. Soc. Sports Nutr. 2007, 4, 12. [Google Scholar] [CrossRef] [Green Version]
- Kanayama, G.; Boynes, M.; Hudson, J.I.; Field, A.E.; Pope, H.G., Jr. Anabolic steroid abuse among teenage girls: An illusory problem? Drug Alcohol Depend. 2007, 88, 156–162. [Google Scholar] [CrossRef] [Green Version]
- Havnes, I.A.; Jørstad, M.L.; Innerdal, I.; Bjørnebekk, A. Anabolic-androgenic steroid use among women—A qualitative study on experiences of masculinizing, gonadal and sexual effects. Int. J. Drug Policy 2021, 95, 102876. [Google Scholar] [CrossRef]
- Daily, S.M.; Mann, M.J.; Lilly, C.L.; Bias, T.K.; Smith, M.L.; Kristjansson, A.L. School Climate as a Universal Intervention to Prevent Substance Use Initiation in Early Adolescence: A Longitudinal Study. Health Educ. Behav. 2020, 47, 402–411. [Google Scholar] [CrossRef]
- Sagoe, D.; Mentzoni, R.A.; Hanss, D.; Pallesen, S. Aggression Is Associated with Increased Anabolic-Androgenic Steroid Use Contemplation Among Adolescents. Subst. Use Misuse 2016, 51, 1462–1469. [Google Scholar] [CrossRef]
- Hauger, L.E.; Havnes, I.A.; Jørstad, M.L.; Bjørnebekk, A. Anabolic androgenic steroids, antisocial personality traits, aggression and violence. Drug Alcohol Depend. 2021, 221, 108604. [Google Scholar] [CrossRef]


| Variable | Level | n | Weighted % |
|---|---|---|---|
| Sex | Male | 21,502 | 50.4% |
| Female | 22,168 | 49.6% | |
| Race/Ethnicity | White | 19,778 | 53.1% |
| American Indian or Alaska Native | 445 | 0.6% | |
| Asian | 1893 | 4.1% | |
| Black or African American | 6503 | 13.1% | |
| Native Hawaiian or Pacific Islander | 285 | 0.6% | |
| Hispanic or Latino | 4917 | 9.7% | |
| Multiple Races–Hispanic/Latino | 6889 | 14.0% | |
| Multiple Races–Non-Hispanic/Latino | 2223 | 4.8% | |
| Weight Status | Healthy Weight | 27,286 | 69.4% |
| Overweight or Obese | 12,358 | 30.6% | |
| Sexual Minority | Non-Sexual Minority | 33,711 | 93.2% |
| Sexual Minority | 2680 | 6.8% |
| Latent Variable | Survey Item | Total Sample Mean (SD) | Females Mean (SD) | Males Mean (SD) |
|---|---|---|---|---|
| Physical Activity | Weekly Frequency of Meeting 60 minutes of Physical Activity (0–7 Scale) (n missing = 1363) | 3.8 (2.5) | 3.3 (2.4) | 4.3 *** (2.5) |
| Number of Sports Teams (0–3 Scale) (n missing = 9437) | 0.9 (1.0) | 0.8 (1.0) | 1.0 *** (1.0) | |
| Weekly Frequency of Muscle Strengthening Activity (0–7 Scale) (n missing = 13,559) | 2.8 (2.5) | 2.2 (2.3) | 3.4 *** (2.5) | |
| Unsafe School | Carry a Weapon on School Property (0–4 Scale) (n missing = 1190) | 0.1 (0.6) | 0.05 (0.43) | 0.15 *** (0.7) |
| Absenteeism Because School is Unsafe (0–4 Scale) (n missing = 2731) | 0.1 (0.6) | 0.1 (0.5) | 0.1 (0.5) | |
| Fight at School (0–7 Scale) (n missing = 1137) | 0.1 (0.7) | 0.1 (0.5) | 0.2 *** (0.5) |
| 1. Age | 2. Female | 3. Sexual Minority | 4. BMI %tile | 5. Race/Ethnic Minority | |
|---|---|---|---|---|---|
| 1. Age | 1 | ||||
| 2. Female | −0.03 *** | 1 | |||
| 3. Sexual Minority | −0.23 *** | 0.11 *** | 1 | ||
| 4. BMI %tile | −0.04 *** | 0.00 | 0.01 | 1 | |
| 5. Race/Ethnic Minority | 0.01 * | −0.01 | 0.00 | 0.09 *** | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brusseau, T.A.; Burns, R.D. Associations of Physical Activity, School Safety, and Non-Prescription Steroid Use in Adolescents: A Structural Equation Modeling Approach. Int. J. Environ. Res. Public Health 2022, 19, 87. https://doi.org/10.3390/ijerph19010087
Brusseau TA, Burns RD. Associations of Physical Activity, School Safety, and Non-Prescription Steroid Use in Adolescents: A Structural Equation Modeling Approach. International Journal of Environmental Research and Public Health. 2022; 19(1):87. https://doi.org/10.3390/ijerph19010087
Chicago/Turabian StyleBrusseau, Timothy A., and Ryan D. Burns. 2022. "Associations of Physical Activity, School Safety, and Non-Prescription Steroid Use in Adolescents: A Structural Equation Modeling Approach" International Journal of Environmental Research and Public Health 19, no. 1: 87. https://doi.org/10.3390/ijerph19010087
APA StyleBrusseau, T. A., & Burns, R. D. (2022). Associations of Physical Activity, School Safety, and Non-Prescription Steroid Use in Adolescents: A Structural Equation Modeling Approach. International Journal of Environmental Research and Public Health, 19(1), 87. https://doi.org/10.3390/ijerph19010087







