Does Telerehabilitation Help in Reducing Disability among People with Musculoskeletal Conditions? A Preliminary Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Setting
2.3. Intervention
2.4. Outcome Measures
2.5. Analyses
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huang, Y.; Xu, X. Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 328 Diseases and Injuries for 195 Countries, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef] [Green Version]
- Blyth, F.M.; Briggs, A.M.; Schneider, C.H.; Hoy, D.G.; March, L.M. The Global Burden of Musculoskeletal Pain—Where to from Here? Am. J. Public Health 2019, 109, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Jafni, T.I.; Bahari, M.; Ismail, W.; Radman, A. Understanding the Implementation of Telerehabilitation at Pre-Implementation Stage: A Systematic Literature Review. Procedia Comput. Sci. 2017, 124, 452–460. [Google Scholar] [CrossRef]
- Cottrell, M.A.; Hill, A.J.; O’Leary, S.P.; Raymer, M.E.; Russell, T.G. Service Provider Perceptions of Telerehabilitation as an Additional Service Delivery Option within an Australian Neurosurgical and Orthopaedic Physiotherapy Screening Clinic: A Qualitative Study. Musculoskelet. Sci. Pract. 2017, 32, 7–16. [Google Scholar] [CrossRef]
- Russell, T.; Gillespie, N.; Hartley, N.; Theodoros, D.; Hill, A.; Gray, L. Exploring the Predictors of Home Telehealth Uptake by Elderly Australian Healthcare Consumers. J. Telemed. Telecare 2015, 21, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Wade, V.A.; Eliott, J.A.; Hiller, J.E. Clinician Acceptance Is the Key Factor for Sustainable Telehealth Services. Qual. Health Res. 2014, 24, 682–694. [Google Scholar] [CrossRef]
- COVID-19: Practice Based Resources. Available online: https://world.physio/covid-19-information-hub/covid-19-practice-based-resources (accessed on 29 November 2021).
- Mani, S.; Sharma, S.; Omar, B.; Paungmali, A.; Joseph, L. Validity and Reliability of Internet-Based Physiotherapy Assessment for Musculoskeletal Disorders: A Systematic Review. J. Telemed. Telecare 2017, 23, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Cottrell, M.A.; O’Leary, S.P.; Swete-Kelly, P.; Elwell, B.; Hess, S.; Litchfield, M.-A.; McLoughlin, I.; Tweedy, R.; Raymer, M.; Hill, A.J.; et al. Agreement between Telehealth and In-Person Assessment of Patients with Chronic Musculoskeletal Conditions Presenting to an Advanced-Practice Physiotherapy Screening Clinic. Musculoskelet. Sci. Pract. 2018, 38, 99–105. [Google Scholar] [CrossRef] [Green Version]
- Cottrell, M.A.; O’Leary, S.P.; Raymer, M.; Hill, A.J.; Comans, T.; Russell, T.G. Does Telerehabilitation Result in Inferior Clinical Outcomes Compared with In-Person Care for the Management of Chronic Musculoskeletal Spinal Conditions in the Tertiary Hospital Setting? A Non-Randomised Pilot Clinical Trial. J. Telemed. Telecare 2021, 27, 444–452. [Google Scholar] [CrossRef]
- Iles, R.; Taylor, N.F.; Davidson, M.; O’Halloran, P. Telephone Coaching Can Increase Activity Levels for People with Non-Chronic Low Back Pain: A Randomised Trial. J. Physiother. 2011, 57, 231–238. [Google Scholar] [CrossRef] [Green Version]
- Kosterink, S.M.; Huis in’t Veld, R.M.; Cagnie, B.; Hasenbring, M.; Vollenbroek-Hutten, M.M. The Clinical Effectiveness of a Myofeedback-Based Teletreatment Service in Patients with Non-Specific Neck and Shoulder Pain: A Randomized Controlled Trial. J. Telemed. Telecare 2010, 16, 316–321. [Google Scholar] [CrossRef] [Green Version]
- Cottrell, M.A.; Galea, O.A.; O’Leary, S.P.; Hill, A.J.; Russell, T.G. Real-Time Telerehabilitation for the Treatment of Musculoskeletal Conditions Is Effective and Comparable to Standard Practice: A Systematic Review and Meta-Analysis. Clin. Rehabil. 2016, 31, 625–638. [Google Scholar] [CrossRef]
- Cottrell, M.A.; Hill, A.J.; O’Leary, S.P.; Raymer, M.E.; Russell, T.G. Patients Are Willing to Use Telehealth for the Multidisciplinary Management of Chronic Musculoskeletal Conditions: A Cross-Sectional Survey. J. Telemed. Telecare 2017, 24, 445–452. [Google Scholar] [CrossRef]
- Bennell, K.L.; Marshall, C.J.; Dobson, F.; Kasza, J.; Lonsdale, C.; Hinman, R.S. Does a Web-Based Exercise Programming System Improve Home Exercise Adherence for People with Musculoskeletal Conditions? Am. J. Phys. Med. Rehabil. 2019, 98, 850–858. [Google Scholar] [CrossRef]
- Kingdom of Saudi Arabia National Health Information Center (NHIC) in Saudi Health Council (SHC) Telemedicine Regulations in the Kingdom of Saudi Arabia 2021. Available online: https://nhic.gov.sa/Initiatives/Documents/The%20Executive%20Rules%20of%20Telehealth.pdf (accessed on 29 November 2021).
- Lakens, D. Calculating and Reporting Effect Sizes to Facilitate Cumulative Science: A Practical Primer for T-Tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [Green Version]
- Nicholas, M.K. The Pain Self-Efficacy Questionnaire: Taking Pain into Account. Eur. J. Pain 2007, 11, 153–163. [Google Scholar] [CrossRef]
- Almutairi, B.A.; Al Odaibi, F.A.; Alnahdi, A.H.; Omar, M.; Algashami, A.; Alonazi, M. Cross-Cultural Adaptation and Validation of the Arabic Version of the Pain Self-Efficacy Questionnaire in Arab People with Chronic Low Back Pain. Physiother. Theory Pract. 2021, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Horn, K.K.; Jennings, S.; Richardson, G.; van Vliet, D.; Hefford, C.; Abbott, J.H. The Patient-Specific Functional Scale: Psychometrics, Clinimetrics, and Application as a Clinical Outcome Measure. J. Orthop. Sport Phys. Ther. 2012, 42, 30–42. [Google Scholar] [CrossRef] [Green Version]
- Alnahdi, A.H.; Murtada, B.A.; Zawawi, A.T.; Omar, M.T.; Alsobayel, H.I. Cross-Cultural Adaptation and Measurement Properties of the Arabic Version of the Patient-Specific Functional Scale in Patients with Lower Extremity Musculoskeletal Disorders. Disabil. Rehabil. 2021, 15, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.C.; Kang, S.; Benedetto, E.; Myers, H.; Blackburn, S.; Smith, S.; Dunn, K.M.; Hay, E.; Rees, J.; Beard, D.; et al. Development and Initial Cohort Validation of the Arthritis Research UK Musculoskeletal Health Questionnaire (MSK-HQ) for Use across Musculoskeletal Care Pathways. BMJ Open 2016, 6, e012331. [Google Scholar] [CrossRef] [PubMed]
- Algarni, F.S.; Alotaibi, A.N.; Altowaijri, A.M.; Al-Sobayel, H. Cross-Cultural Adaptation and Validation of the Arabic Version of Musculoskeletal Health Questionnaire (MSK-HQ-Ar). Int. J. Environ. Res. Public Health 2020, 17, 5168. [Google Scholar] [CrossRef]
- Al Saffer, Q.; Al-Ghaith, T.; Alshehri, A.; Al-Mohammed, R.; Al Homidi, S.; Hamza, M.M.; Herbst, C.H.; Alazemi, N. The Capacity of Primary Health Care Facilities in Saudi Arabia: Infrastructure, Services, Drug Availability, and Human Resources. BMC Health Serv. Res. 2021, 21, 365. [Google Scholar] [CrossRef] [PubMed]
- Ku, B.P.S.; Tse, A.W.S.; Pang, B.C.H.; Cheung, N.T.; Pang, J.Y.W.; Chan, J.K.Y.; Hui, H.L.; Chu, D.; Choi, K.H.W. Tele-Rehabilitation to Combat Rehabilitation Service Disruption during COVID-19 in Hong Kong: Observational Study. JMIR Rehabil. Assist. Technol. 2021, 8, e19946. [Google Scholar] [CrossRef] [PubMed]
- Murray, T.; Murray, G.; Murray, J. Remote Musculoskeletal Assessment Framework: A Guide for Primary Care. Cureus 2021, 13, e12778. [Google Scholar] [CrossRef]
- Gialanella, B.; Ettori, T.; Faustini, S.; Baratti, D.; Bernocchi, P.; Comini, L.; Scalvini, S. Home-Based Telemedicine in Patients with Chronic Neck Pain. Am. J. Phys. Med. Rehabil. 2017, 96, 327–332. [Google Scholar] [CrossRef]
- Jiang, S.; Xiang, J.; Gao, X.; Guo, K.; Liu, B. The Comparison of Telerehabilitation and Face-To-Face Rehabilitation after Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. J. Telemed. Telecare 2016, 24, 257–262. [Google Scholar] [CrossRef]
- Turolla, A.; Rossettini, G.; Viceconti, A.; Palese, A.; Geri, T. Musculoskeletal Physical Therapy during the COVID-19 Pandemic: Is Telerehabilitation the Answer? Phys. Ther. 2020, 100, 1260–1264. [Google Scholar] [CrossRef]
- Comans, T.; Raymer, M.; O’Leary, S.; Smith, D.; Scuffham, P. Cost-Effectiveness of a Physiotherapist-Led Service for Orthopaedic Outpatients. J. Health Serv. Res. Policy 2014, 19, 216–223. [Google Scholar] [CrossRef]
- Bornhöft, L.; Thorn, J.; Svensson, M.; Nordeman, L.; Eggertsen, R.; Larsson, M.E.H. More Cost-Effective Management of Patients with Musculoskeletal Disorders in Primary Care after Direct Triaging to Physiotherapists for Initial Assessment Compared to Initial General Practitioner Assessment. BMC Musculoskelet. Disord. 2019, 20, 186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elrod, J.K.; Fortenberry, J.L. The Hub-And-Spoke Organization Design: An Avenue for Serving Patients Well. BMC Health Serv. Res. 2017, 17, 457. [Google Scholar] [CrossRef]
- Chen, S.-C.; Lin, C.-H.; Su, S.-W.; Chang, Y.-T.; Lai, C.-H. Feasibility and Effect of Interactive Telerehabilitation on Balance in Individuals with Chronic Stroke: A Pilot Study. J. Neuroeng. Rehabil. 2021, 18, 71. [Google Scholar] [CrossRef] [PubMed]
- Hernando-Garijo, I.; Ceballos-Laita, L.; Mingo-Gómez, M.T.; Medrano-de-la-Fuente, R.; Estébanez-de-Miguel, E.; Martínez-Pérez, M.N.; Jiménez-del-Barrio, S. Immediate Effects of a Telerehabilitation Program Based on Aerobic Exercise in Women with Fibromyalgia. Int. J. Environ. Res. Public Health 2021, 18, 2075. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Piña, M.; Molina-Garcia, P.; Femia, P.; Ashe, M.C.; Martín-Martín, L.; Salazar-Graván, S.; Salas-Fariña, Z.; Prieto-Moreno, R.; Castellote-Caballero, Y.; Estevez-Lopez, F.; et al. Effects of Tele-Rehabilitation Compared with Home-Based In-Person Rehabilitation for Older Adult’s Function after Hip Fracture. Int. J. Environ. Res. Public Health 2021, 18, 5493. [Google Scholar] [CrossRef] [PubMed]
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth Transformation: COVID-19 and the Rise of Virtual Care. J. Am. Med. Inform. Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | n (%) | |
|---|---|---|
| Age, years, mean (SD) | 33 (8) | |
| Gender, male | 83 (87) | |
| Marital status | Single | 53 (56) |
| Married | 42 (44) | |
| Level of education | Illiterate | 1 (1) |
| High school | 3 (3) | |
| College | 91 (96) | |
| Employment status | Employed | 81 (85) |
| Unemployed | 12 (13) | |
| Retired | 2 (2) | |
| Region | Riyadh | 48 (51) |
| Qassim | 9 (10) | |
| Tabuk | 6 (6) | |
| Jazan | 6 (6) | |
| Eastern region | 4 (4) | |
| Jeddah | 4 (4) | |
| Other | 18 (19) | |
| Smoker | 28 (28) | |
| Body mass index, weight (kg)/height (m)2, mean (SD) | 25 (4) | |
| Past medical history | Hypertension | 7 (7) |
| Diabetes | 6 (6) | |
| Musculoskeletal disorder | Lower back pain | 35 (37) |
| Knee pain | 13 (14) | |
| Neck pain | 9 (10) | |
| Shoulder pain | 7 (7) | |
| Ankle pain | 5 (5) | |
| Hip pain | 2 (2) | |
| Elbow pain | 2 (2) | |
| Post-operative condition | 14 (15) | |
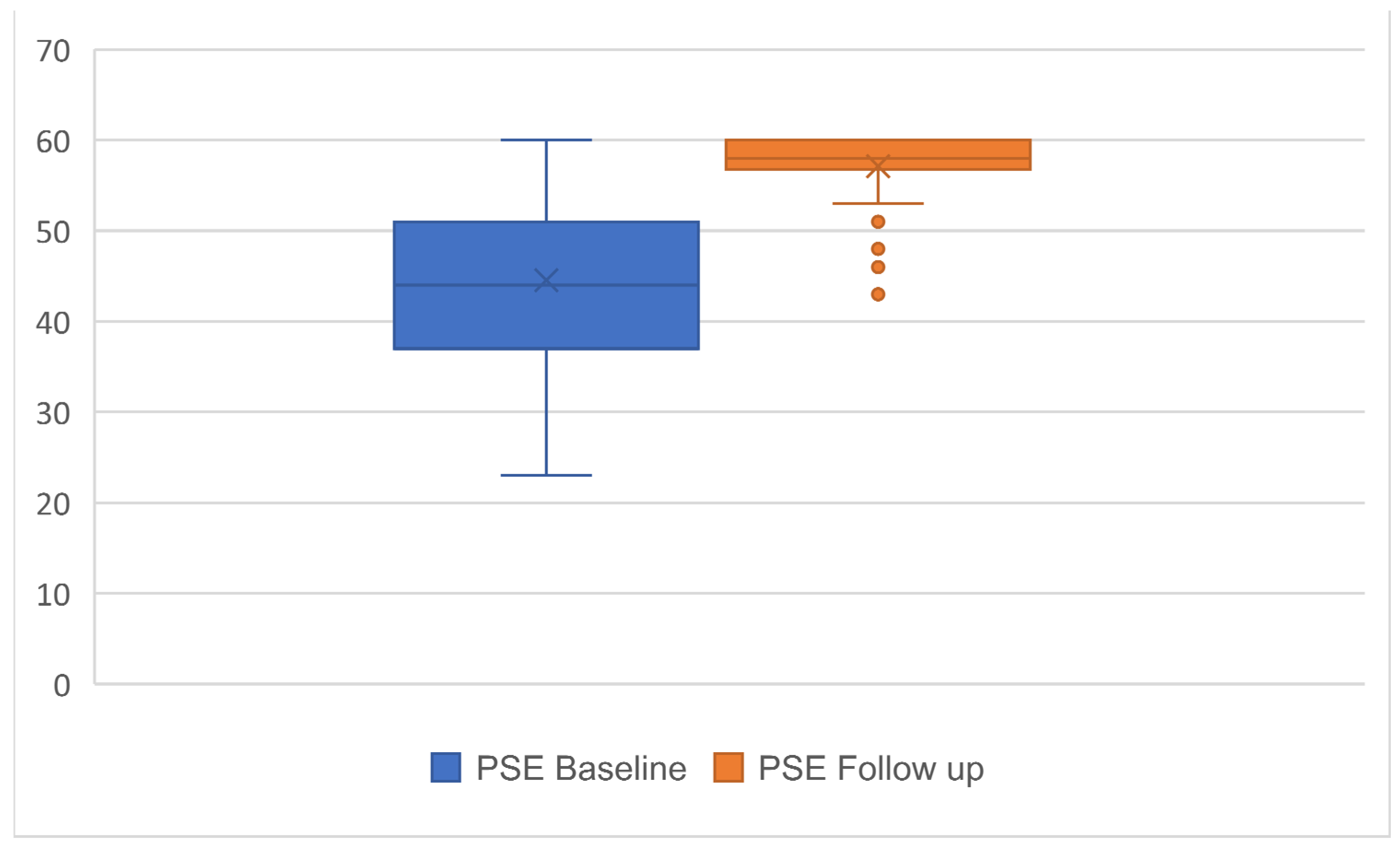
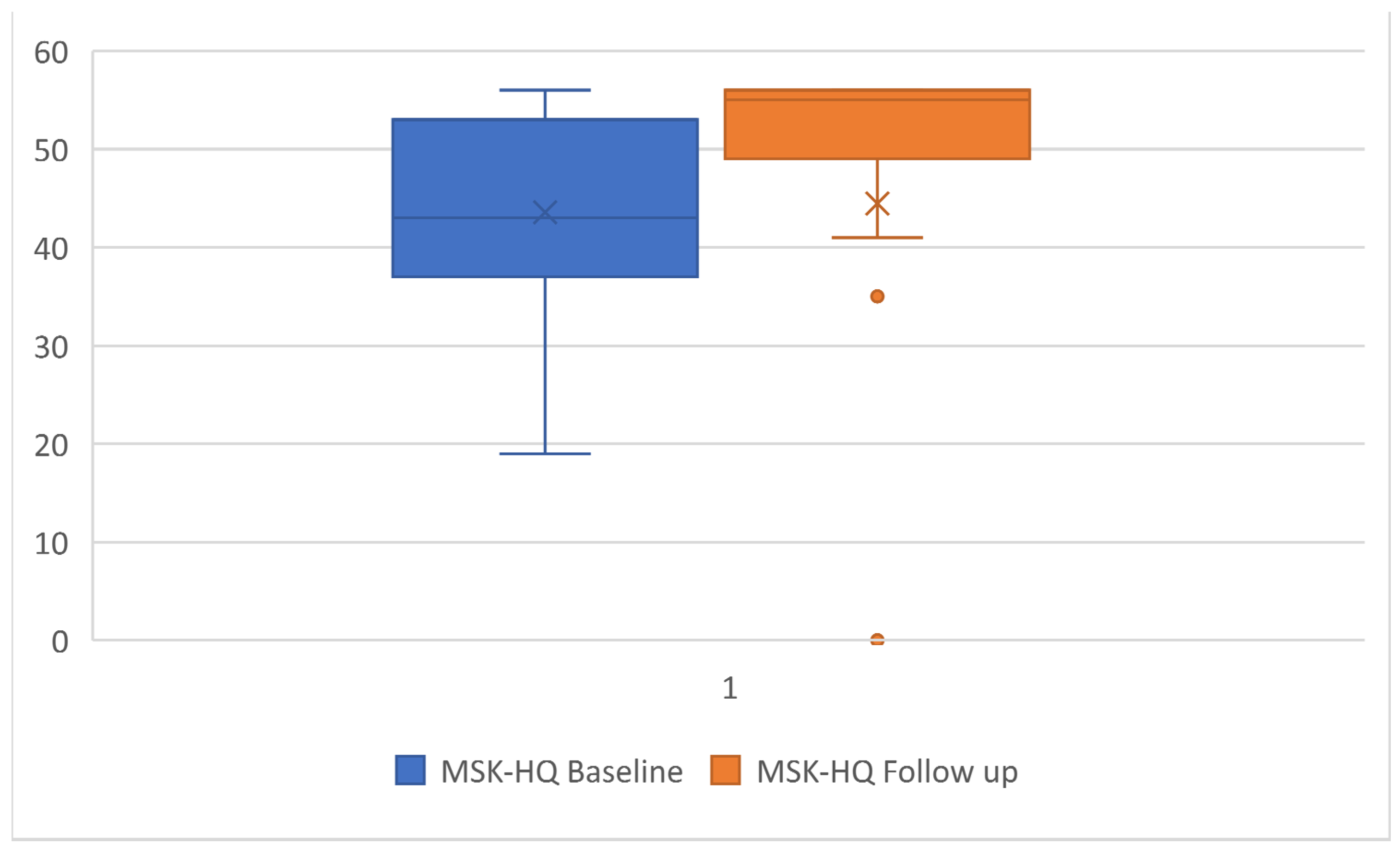
| Outcome Measures | Baseline Mean (SD) | Follow Up Mean (SD) | Effect Size (Cohen’s d) |
|---|---|---|---|
| Pain Self-Efficacy Questionnaire | 44.6 (9.6) | 57.1 (3.6) | −1.9 * |
| Patient-Specific Functional Scale | 8.1 (2.1) | 9.4 (0.5) | 0.6 * |
| Musculoskeletal Health Questionnaire | 43.6 (9.3) | 54.2 (3.6) | −1.4 * |
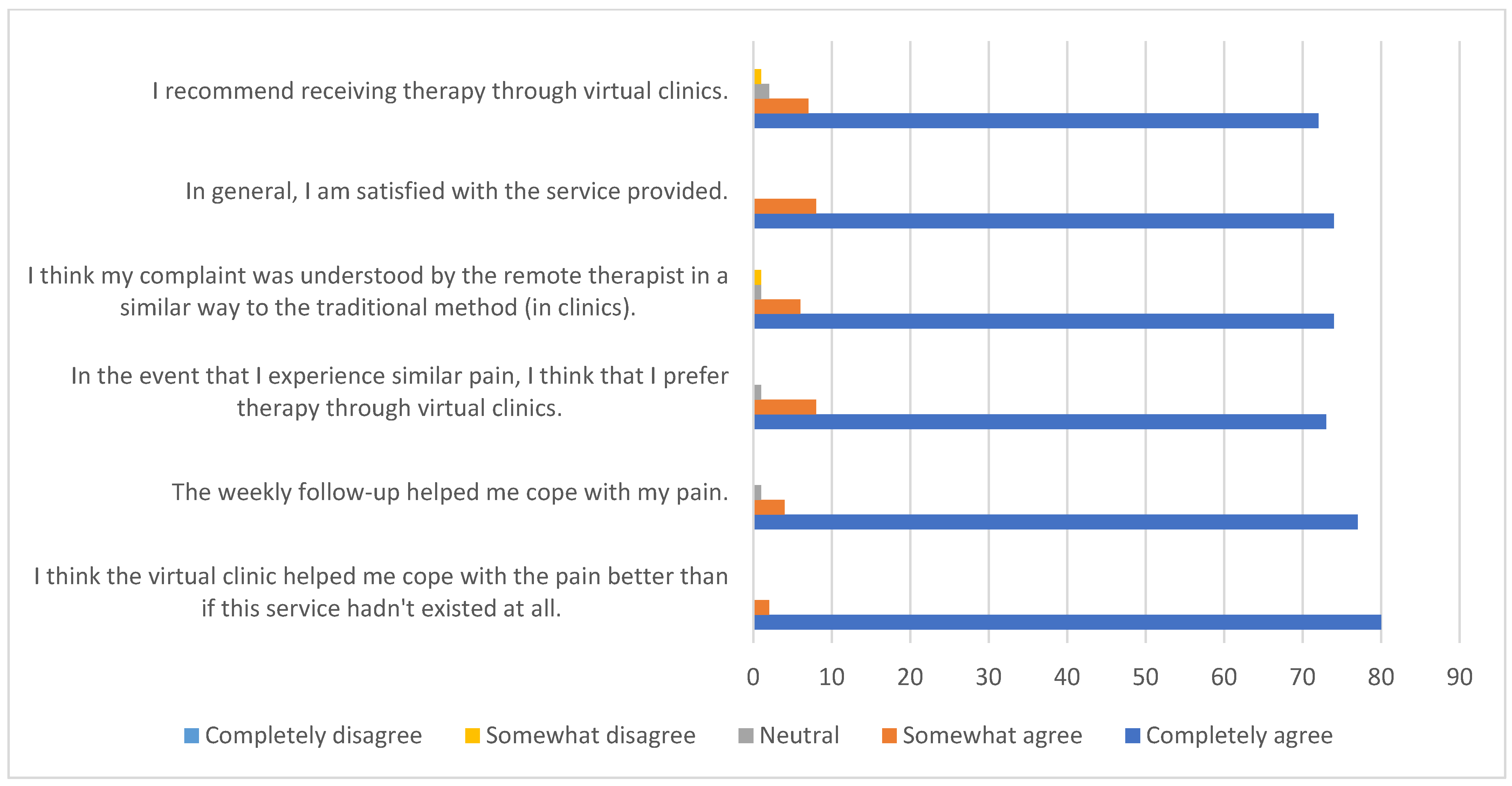
| Statements | Completely Agree n (%) | Somewhat Agree n (%) | Neutral n (%) | Somewhat Disagree n (%) | Completely Disagree n (%) |
|---|---|---|---|---|---|
| I think the virtual clinic helped me cope with the pain better than if this service hadn’t existed at all. | 76 (80) | 2 (2) | 0 (0) | 0 (0) | 0 (0) |
| The weekly follow-up helped me cope with my pain. | 73 (77) | 4 (4) | 1 (1) | 0 (0) | 0 (0) |
| In the event that I experience similar pain, I think that I prefer therapy through virtual clinics. | 69 (73) | 8 (8) | 1 (1) | 0 (0) | 0 (0) |
| I think my complaint was understood by the remote therapist in a similar way to the traditional method (in clinics). | 70 (74) | 6 (6) | 1 (1) | 1 (1) | 0 (0) |
| In general, I am satisfied with the service provided. | 70 (74) | 8 (8) | 0 (0) | 0 (0) | 0 (0) |
| I recommend receiving therapy through virtual clinics. | 68 (72) | 7 (7) | 2 (2) | 1 (1) | 0 (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsobayel, H.; Alodaibi, F.; Albarrati, A.; Alsalamah, N.; Alhawas, F.; Alhowimel, A. Does Telerehabilitation Help in Reducing Disability among People with Musculoskeletal Conditions? A Preliminary Study. Int. J. Environ. Res. Public Health 2022, 19, 72. https://doi.org/10.3390/ijerph19010072
Alsobayel H, Alodaibi F, Albarrati A, Alsalamah N, Alhawas F, Alhowimel A. Does Telerehabilitation Help in Reducing Disability among People with Musculoskeletal Conditions? A Preliminary Study. International Journal of Environmental Research and Public Health. 2022; 19(1):72. https://doi.org/10.3390/ijerph19010072
Chicago/Turabian StyleAlsobayel, Hana, Faris Alodaibi, Ali Albarrati, Norah Alsalamah, Fadwa Alhawas, and Ahmed Alhowimel. 2022. "Does Telerehabilitation Help in Reducing Disability among People with Musculoskeletal Conditions? A Preliminary Study" International Journal of Environmental Research and Public Health 19, no. 1: 72. https://doi.org/10.3390/ijerph19010072
APA StyleAlsobayel, H., Alodaibi, F., Albarrati, A., Alsalamah, N., Alhawas, F., & Alhowimel, A. (2022). Does Telerehabilitation Help in Reducing Disability among People with Musculoskeletal Conditions? A Preliminary Study. International Journal of Environmental Research and Public Health, 19(1), 72. https://doi.org/10.3390/ijerph19010072








