Prevalence of Anxiety in University Students during the COVID-19 Pandemic: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
- (a)
- (“students” OR “University students” OR “Post-secondary students” OR “graduate students”) AND
- (b)
- (“severe acute respiratory syndrome coronavirus 2” OR “COVID-19” OR “SARS-CoV-2” OR “COVID-19 pandemic) AND
- (c)
- (“Psychological Stress” OR “Anxiety” OR “stress”, “OR “Mental Health” OR “Mental Disorders” OR “Stress Disorders”).
2.2. Inclusion and Exclusion Criteria
2.3. Data Retrieval
2.4. Outcome Measure
2.5. Assessment of Quality for Included Studies
2.6. Data Analysis
2.7. Assessment of Heterogeneity
2.8. Publication Bias Assessment
2.9. Sensitivity Analysis
3. Results
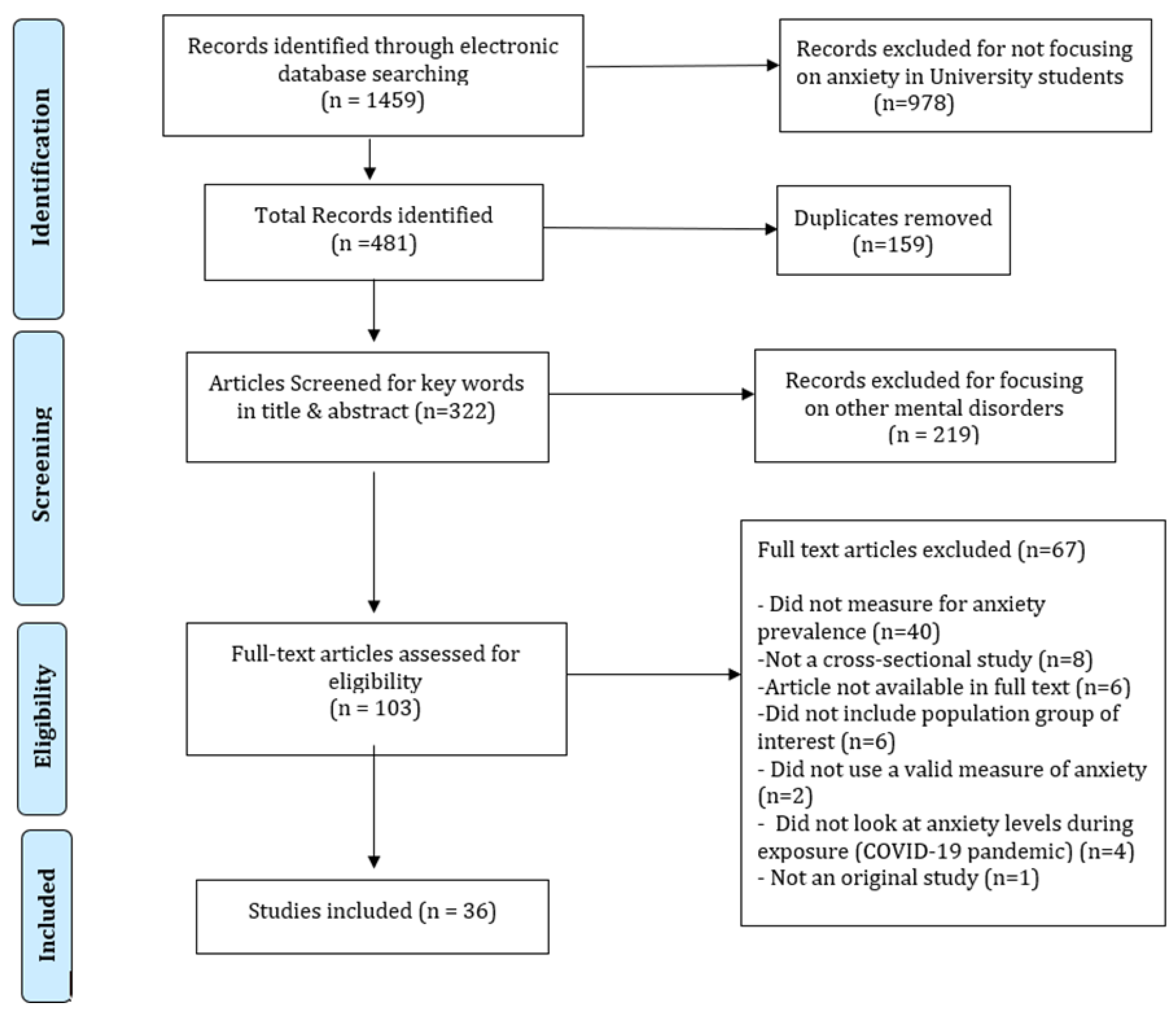
3.1. Selection and Evaluation of Studies
3.2. Characteristics of the Included Studies
3.3. Screening Tools for Anxiety
3.4. Quality Assessment
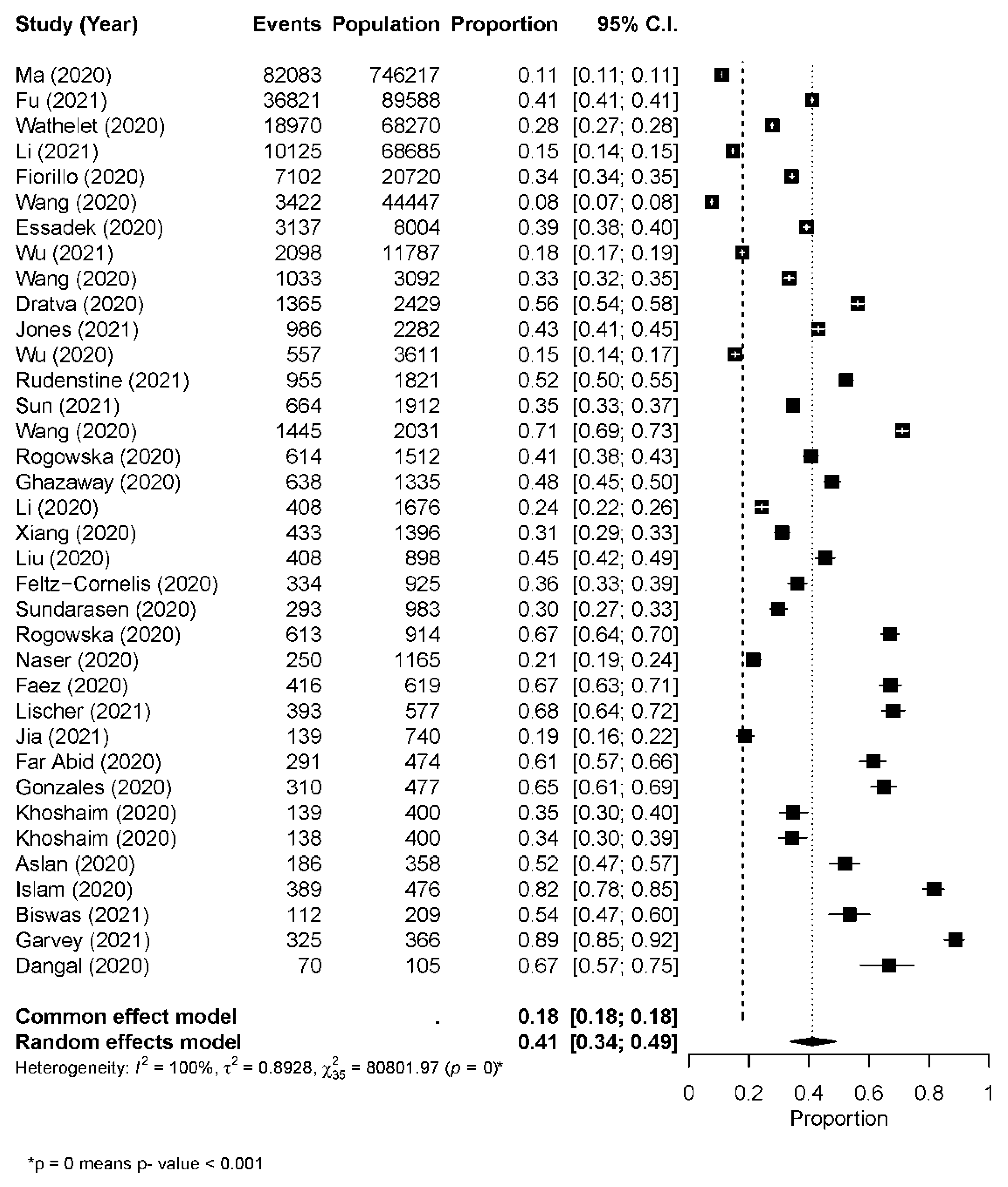
3.5. Prevalence of Anxiety
3.6. Subgroup Analysis
3.7. Sensitivity Analysis
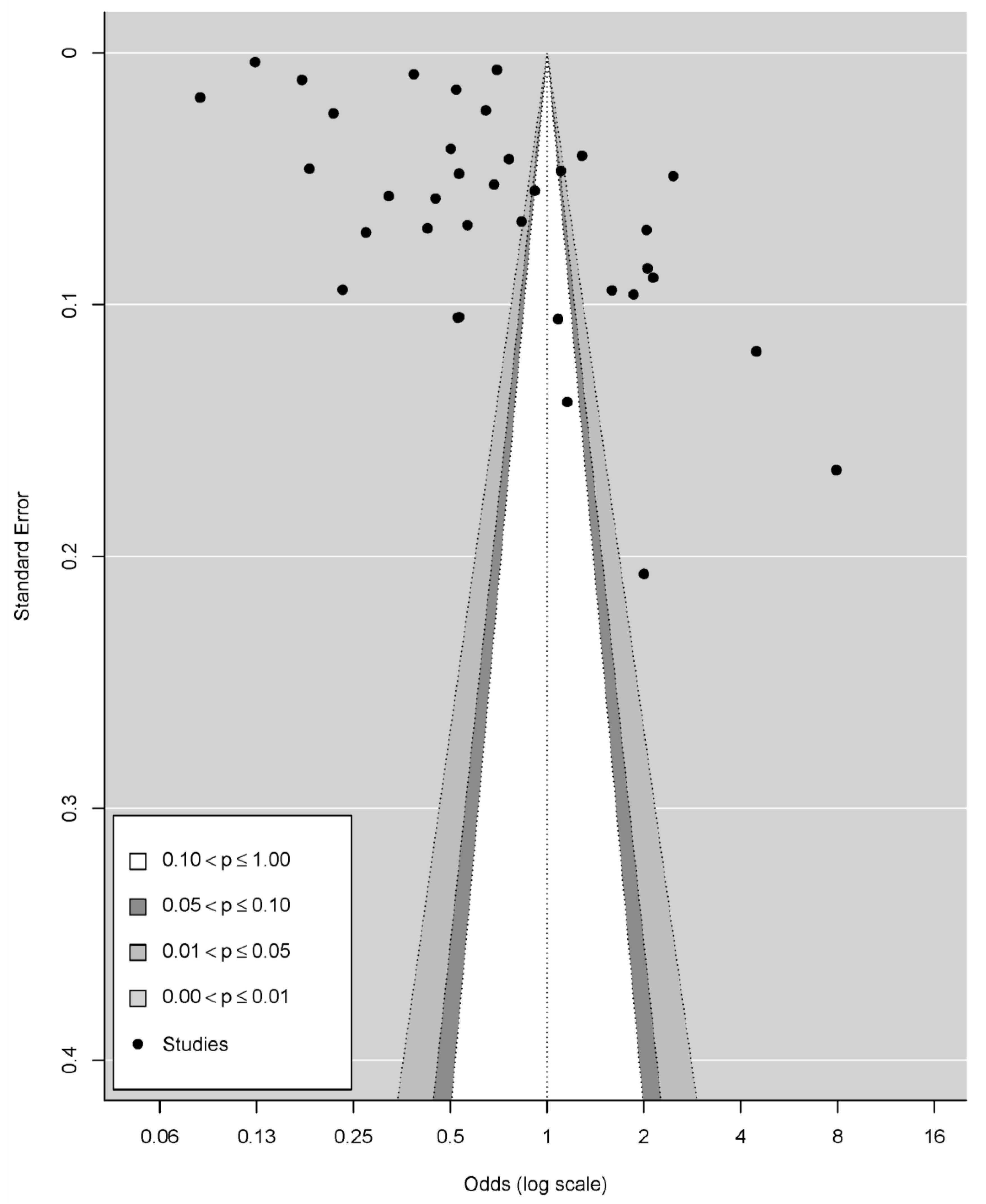
3.8. Publication Bias
4. Discussion
4.1. Overview and Interpretation of the Synthesized Findings
4.2. Prevalence of Anxiety by Geographical Regions
4.3. Subgroup Analyses (Sex)
4.4. Future Research Directions
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Zarocostas, J. What next for the coronavirus response? Lancet 2020, 395, 401. [Google Scholar] [CrossRef] [Green Version]
- Cucinotta, D. Parmensis MV-ABMA, 2020 Undefined. WHO Declares COVID-19 a Pandemic. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/7569573/ (accessed on 26 June 2021).
- Javed, B.; Sarwer, A.; Soto, E.B.; Mashwani, Z.U.R. The coronavirus (COVID-19) pandemic’s impact on mental health. Int. J. Health Plan. Manag. 2020, 35, 993–996. [Google Scholar] [CrossRef] [PubMed]
- Ahrendt, D.; Cabrita, J.; Clerici, E.; Hurley, J.; Leoncikas, T.; Mascherini, M.; Riso, S.; Sándor, E. Living, Working and COVID-19|Eurofound. 2020. Available online: https://www.eurofound.europa.eu/publications/report/2020/living-working-and-COVID-19 (accessed on 26 June 2021).
- Savitsky, B.; Findling, Y.; Ereli, A.; Hendel, T. Anxiety and coping strategies among nursing students during the COVID-19 pandemic. Nurse Educ. Pract. 2020, 46, 102809. [Google Scholar] [CrossRef]
- Gritsenko, V.; Skugarevsky, O.; Konstantinov, V.; Khamenka, N.; Marinova, T.; Reznik, A.; Isralowitz, R. COVID 19 Fear, Stress, Anxiety, and Substance Use Among Russian and Belarusian University Students. Int. J. Ment. Health Addict. 2020, 19, 2362–2368. [Google Scholar] [CrossRef]
- Mamun, M.A.; Chandrima, R.M.; Griffiths, M.D. Mother and Son Suicide Pact Due to COVID-19-Related Online Learning Issues in Bangladesh: An Unusual Case Report. Int. J. Ment. Health Addict. 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Aristovnik, A.; Keržič, D.; Ravšelj, D.; Tomaževič, N.; Umek, L. Impacts of the COVID-19 Pandemic on Life of Higher Education Students: A Global Perspective. Sustainability 2020, 12, 8438. [Google Scholar] [CrossRef]
- Tian, F.; Li, H.; Tian, S.; Yang, J.; Shao, J.; Tian, C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID. Psychiatry Res. 2020, 288, 112992. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Owusu-Fordjour, C.; Koomson, C.K.; Hanson, D. The impact of COVID-19 on learning—The perspective of the ghanaian student. Eur. J. Educ. Stud. 2020, 7, 88–101. Available online: www.oapub.org/edu (accessed on 26 June 2021).
- Solmi, M.; Radua, J.; Olivola, M.; Croce, E.; Soardo, L.; de Pablo, G.S.; Shin, J.I.; Kirkbride, J.B.; Jones, P.; Kim, J.H.; et al. Age at onset of mental disorders worldwide: Large-scale meta-analysis of 192 epidemiological studies. Mol. Psychiatry 2021, 17, 22. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Gonzalez, T.; De La Rubia, M.A.; Hincz, K.P.; Comas-Lopez, M.; Subirats, L.; Fort, S.; Sacha, G.M. Influence of COVID-19 confinement on students’ performance in higher education. PLoS ONE 2020, 15, e0239490. [Google Scholar] [CrossRef]
- Elmer, T.; Mepham, K.; Stadtfeld, C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 2020, 15, e0236337. [Google Scholar] [CrossRef]
- Pan, H. A Glimpse of University Students’ Family Life Amidst the COVID-19 Virus. J. Loss Trauma 2020, 25, 594–597. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Liu, J.; Zhong, X. Psychological State of College Students During COVID-19 Epidemic. SSRN Electron. J. 2020. Available online: https://papers.ssrn.com/abstract=3552814 (accessed on 27 June 2021).
- Baloran, E.T. Knowledge, Attitudes, Anxiety, and Coping Strategies of Students during COVID-19 Pandemic. J. Loss Trauma 2020, 25, 635. Available online: https://www.tandfonline.com/action/journalInformation?journalCode=upil20 (accessed on 27 June 2021). [CrossRef]
- Kapasia, N.; Paul, P.; Roy, A.; Saha, J.; Zaveri, A.; Mallick, R.; Barman, B.; Das, P.; Chouhan, P. Impact of lockdown on learning status of undergraduate and postgraduate students during COVID-19 pandemic in West Bengal, India. Child. Youth Serv. Rev. 2020, 116, 105194. [Google Scholar] [CrossRef]
- Sahu, P. Closure of Universities Due to Coronavirus Disease 2019 (COVID-19): Impact on Education and Mental Health of Students and Academic Staff. Cureus 2020, 12, e7541. [Google Scholar] [CrossRef] [Green Version]
- Zimmermann, M.; Bledsoe, C.; Papa, A. Initial impact of the COVID-19 pandemic on college student mental health: A longitudinal examination of risk and protective factors. Psychiatry Res. 2021, 305, 114254. [Google Scholar] [CrossRef] [PubMed]
- Santabárbara, J.; Bueno-Notivol, J.; Lipnicki, D.M.; Olaya, B.; Pérez-Moreno, M.; Gracia-García, P.; Idoiaga-Mondragon, N.; Ozamiz-Etxebarria, N. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: A rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 107, 110244. [Google Scholar] [CrossRef]
- Santabárbara, J.; Lasheras, I.; Lipnicki, D.M.; Bueno-Notivol, J.; Pérez-Moreno, M.; López-Antón, R.; De la Cámara, C.; Lobo, A.; Gracia-García, P. Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2020, 109, 110207. [Google Scholar] [CrossRef] [PubMed]
- Patsali, M.E.; Mousa, D.-P.V.; Papadopoulou, E.V.; Papadopoulou, K.K.; Kaparounaki, C.K.; Diakogiannis, I.; Fountoulakis, K.N. University students’ changes in mental health status and determinants of behavior during the COVID-19 lockdown in Greece. Psychiatry Res. 2020, 292, 113298. [Google Scholar] [CrossRef]
- Odriozola-González, P.; Planchuelo-Gómez, A.; Irurtia, M.J.; de Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020, 290, 113108. [Google Scholar] [CrossRef]
- Mofatteh, M. Risk factors associated with stress, anxiety, and depression among university undergraduate students. AIMS Public Health 2021, 8, 36–65. [Google Scholar] [CrossRef] [PubMed]
- Browning, M.H.E.M.; Larson, L.R.; Sharaievska, I.; Rigolon, A.; McAnirlin, O.; Mullenbach, L.; Cloutier, S.; Vu, T.M.; Thomsen, J.; Reigner, N.; et al. Psychological impacts from COVID-19 among university students: Risk factors across seven states in the United States. PLoS ONE 2021, 16, e0245327. [Google Scholar] [CrossRef]
- Abdel Wahed, W.Y.; Hassan, S.K. Prevalence and associated factors of stress, anxiety and depression among medical Fayoum University students. Alexandria J. Med. 2017, 53, 77–84. Available online: https://www.tandfonline.com/action/journalInformation?journalCode=tajm20 (accessed on 28 June 2021). [CrossRef] [Green Version]
- Sankhi, S.; Marasine, N.R. Impact of COVID-19 Pandemic on Mental Health of the General Population, Students, and Health Care Workers. Eur. J. Med. Sci. 2020, 2, 64–72. [Google Scholar] [CrossRef]
- Rotenstein, L.S.; Ramos, M.A.; Torre, M.; Bradley Segal, J.; Peluso, M.J.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students a systematic review and meta-analysis. JAMA 2016, 316, 2214–2236. Available online: https://jamanetwork.com/ (accessed on 28 June 2021). [CrossRef] [PubMed] [Green Version]
- Stallman, H.M. Psychological distress in university students: A comparison with general population data. Aust. Psychol. 2010, 45, 249–257. [Google Scholar] [CrossRef]
- Eisenberg, D.; Gollust, S.E.; Golberstein, E.; Hefner, J.L. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am. J. Orthopsychiatry 2007, 77, 534–542. [Google Scholar] [CrossRef] [Green Version]
- Hendriks, S.M.; Spijker, J.; Licht, C.M.M.; Hardeveld, F.; De Graaf, R.; Batelaan, N.M.; Penninx, B.W.J.H.; Beekman, A.T.F. Long-term disability in anxiety disorders. BMC Psychiatry 2016, 16, 248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghazawy, E.R.; Ewis, A.A.; Mahfouz, E.M.; Khalil, D.M.; Arafa, A.; Mohammed, Z.; Mohammed, E.-N.F.; Hassan, E.E.; Hamid, S.A.; Ewis, S.A.; et al. Psychological impacts of COVID-19 pandemic on the university students in Egypt. Health Promot. Int. 2021, 36, 1116–1125. [Google Scholar] [CrossRef] [PubMed]
- Copeland, W.E.; McGinnis, E.; Bai, Y.; Adams, Z.; Nardone, H.; Devadanam, V.; Rettew, J.; Hudziak, J.J. Impact of COVID-19 Pandemic on College Student Mental Health and Wellness. J. Am. Acad. Child Adolesc. Psychiatry 2021, 60, 134–141.e2. [Google Scholar] [CrossRef] [PubMed]
- Lasheras, I.; Gracia-García, P.; Lipnicki, D.M.; Bueno-Notivol, J.; López-Antón, R.; de la Cámara, C.; Lobo, A.; Santabárbara, J. Prevalence of anxiety in medical students during the Covid-19 pandemic: A rapid systematic review with meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 6603. Available online: https://www.mdpi.com/journal/ijerph (accessed on 30 June 2021). [CrossRef] [PubMed]
- Marvaldi, M.; Mallet, J.; Dubertret, C.; Moro, M.R.; Guessoum, S.B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 126, 252–264. [Google Scholar] [CrossRef] [PubMed]
- Al Maqbali, M.; Al Sinani, M.; Al-Lenjawi, B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. J. Psychosomatic Res. 2021, 141, 110343. [Google Scholar] [CrossRef]
- Chang, J.-J.; Ji, Y.; Li, Y.-H.; Pan, H.-F.; Su, P.-Y. Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: A meta-analysis. J. Affect. Disord. 2021, 292, 242–254. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Tufanaru, C.; Qureshi, R.; Mattis, P.; Mu, P. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s approach. JBI Evid. Implement. 2015, 13, 163–169. Available online: https://pubmed.ncbi.nlm.nih.gov/26262566/ (accessed on 29 June 2021). [CrossRef]
- Ades, A.E.; Lu, G.; Higgins, J.P.T. The interpretation of random-effects meta-analysis in decision models. Med. Decis. Mak. 2005, 25, 646–654. Available online: https://journals.sagepub.com/doi/10.1177/0272989×05282643 (accessed on 29 June 2021). [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557. [Google Scholar] [CrossRef] [Green Version]
- Aslan, I.; Ochnik, D.; Çınar, O. Exploring Perceived Stress among Students in Turkey during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 8961. [Google Scholar] [CrossRef] [PubMed]
- Essadek, A.; Rabeyron, T. Mental health of French students during the COVID-19 pandemic. J. Affect. Disord. 2020, 277, 392–393. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z.; Chen, Z.; Yu, Q.; Jiang, J.; Fan, F.; et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, e181. [Google Scholar] [CrossRef] [PubMed]
- Naser, A.Y.; Dahmash, E.Z.; Al-Rousan, R.; Alwafi, H.; Alrawashdeh, H.M.; Ghoul, I.; Abidine, A.; Bokhary, M.A.; Al-Hadithi, H.T.; Ali, D.; et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain Behav. 2020, 10, e01730. [Google Scholar] [CrossRef] [PubMed]
- Rogowska, A.M.; Kuśnierz, C.; Bokszczanin, A. Examining Anxiety, Life Satisfaction, General Health, Stress and Coping Styles During COVID-19 Pandemic in Polish Sample of University Students. Psychol. Res. Behav. Manag. 2020, 13, 797–811. [Google Scholar] [CrossRef]
- Rogowska, A.M.; Pavlova, I.; Kuśnierz, C.; Ochnik, D.; Bodnar, I.; Petrytsa, P. Does Physical Activity Matter for the Mental Health of University Students during the COVID-19 Pandemic? J. Clin. Med. 2020, 9, 3494. [Google Scholar] [CrossRef] [PubMed]
- Dangal, M.R.; Bajracharya, L.S. Students Anxiety Experiences during COVID-19 in Nepal. Kathmandu Univ. Med. J. 2020, 18, 53–57. [Google Scholar] [CrossRef]
- Rudenstine, S.; McNeal, K.; Schulder, T.; Ettman, C.K.; Hernandez, M.; Gvozdieva, K.; Galea, S. Depression and Anxiety During the COVID-19 Pandemic in an Urban, Low-Income Public University Sample. J. Trauma. Stress 2021, 34, 12–22. [Google Scholar] [CrossRef]
- Sun, S.; Goldberg, S.B.; Lin, D.; Qiao, S.; Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Glob. Health 2021, 17, 15, Correction in Glob. Health 2021, 17, 52. [Google Scholar] [CrossRef]
- Biswas, S.; Biswas, A. Anxiety level among students of different college and universities in India during lock down in connection to the COVID-19 pandemic. J. Public Health 2021. [Google Scholar] [CrossRef]
- Fu, W.; Yan, S.; Zong, Q.; Anderson-Luxford, D.; Song, X.; Lv, Z.; Lv, C. Mental health of college students during the COVID-19 epidemic in China. J. Affect. Disord. 2021, 280, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Garvey, A.M.; García, I.J.; Franco, S.H.O.; Fernández, C.M. The Psychological Impact of Strict and Prolonged Confinement on Business Students during the COVID-19 Pandemic at a Spanish University. Int. J. Environ. Res. Public Health 2021, 18, 1710. [Google Scholar] [CrossRef] [PubMed]
- Dratva, J.; Zysset, A.; Schlatter, N.; Von Wyl, A.; Huber, M.; Volken, T. Swiss University Students’ Risk Perception and General Anxiety during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 7433. [Google Scholar] [CrossRef]
- Akhtarul Islam, M.; Barna, S.D.; Raihan, H.; Nafiul Alam Khan, M.; Tanvir Hossain, M. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: A web-based cross-sectional survey. PLoS ONE 2020, 15, e0238162. [Google Scholar] [CrossRef]
- Faez, M.; Hadi, J.; Abdalqader, M.; Assem, H.; Ads, H.O.; Ghazi, H.F. Impact of Lockdown Due to COVID-19 on Mental Health among Students in Private University at Selangor. Eur. J. Mol. Clin. Med. 2020, 7, 508–517. [Google Scholar]
- Li, M.; Liu, L.; Yang, Y.; Wang, Y.; Yang, X.; Wu, H. Psychological Impact of Health Risk Communication and Social Media on College Students During the COVID-19 Pandemic: Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e20656. [Google Scholar] [CrossRef]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S.; Hahm, H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef]
- Gonzales, G.; de Mola, E.L.; Gavulic, K.A.; McKay, T.; Purcell, C. Mental Health Needs Among Lesbian, Gay, Bisexual, and Transgender College Students During the COVID-19 Pandemic. J. Adolesc. Health 2020, 67, 645–648. [Google Scholar] [CrossRef]
- Xiang, M.-Q.; Tan, X.-M.; Sun, J.; Yang, H.-Y.; Zhao, X.-P.; Liu, L.; Hou, X.-H.; Hu, M. Relationship of Physical Activity with Anxiety and Depression Symptoms in Chinese College Students During the COVID-19 Outbreak. Front. Psychol. 2020, 11, 582436. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Tao, S.; Zhang, Y.; Li, S.; Ma, L.; Yu, Y.; Sun, G.; Li, T.; Tao, F. Geographic Distribution of Mental Health Problems Among Chinese College Students During the COVID-19 Pandemic: Nationwide, Web-Based Survey Study. J. Med. Internet Res. 2021, 23, e23126. [Google Scholar] [CrossRef]
- Wang, X.; Hegde, S.; Son, C.; Keller, B.; Smith, A.; Sasangohar, F. Investigating Mental Health of US College Students during the COVID-19 Pandemic: Cross-Sectional Survey Study. J. Med. Internet Res. 2020, 22, e22817. [Google Scholar] [CrossRef]
- Sundarasen, S.; Chinna, K.; Kamaludin, K.; Nurunnabi, M.; Baloch, G.M.; Khoshaim, H.B.; Hossain, S.F.A.; Sukayt, A. Psychological Impact of COVID-19 and Lockdown among University Students in Malaysia: Implications and Policy Recommendations. Int. J. Environ. Res. Public Health 2020, 17, 6206. [Google Scholar] [CrossRef] [PubMed]
- Khoshaim, H.B.; Al-Sukayt, A.; Chinna, K.; Nurunnabi, M.; Sundarasen, S.; Kamaludin, K.; Baloch, G.M.; Hossain, S.F.A. How students in the Kingdom of Saudi Arabia are coping with COVID-19 pandemic. J. Public Health Res. 2020, 9, 1898. [Google Scholar] [CrossRef]
- Khoshaim, H.B.; Al-Sukayt, A.; Chinna, K.; Nurunnabi, M.; Sundarasen, S.; Kamaludin, K.; Baloch, G.M.; Hossain, S.F.A. Anxiety Level of University Students During COVID-19 in Saudi Arabia. Front. Psychiatry 2020, 11, 579750. [Google Scholar] [CrossRef]
- Jia, Y.; Qi, Y.; Bai, L.; Han, Y.; Xie, Z.; Ge, J. Knowledge–attitude–practice and psychological status of college students during the early stage of COVID-19 outbreak in China: A cross-sectional study. BMJ Open 2021, 11, e045034. [Google Scholar] [CrossRef]
- Far Abid Hossain, S.; Nurunnabi, M.; Sundarasen, S.; Chinna, K.; Kamaludin, K.; Baloch, G.M.; Khoshaim, H.B.; Sukayt, A. Socio-psychological impact on Bangladeshi students during COVID. J. Public Health Res. 2020, 9 (Suppl. 1), 1911. Available online: https://www.jphres.org/index.php/jphres/article/view/jphr.2021.1911 (accessed on 30 June 2021).
- Fiorillo, A.; Sampogna, G.; Giallonardo, V.; Del Vecchio, V.; Luciano, M.; Albert, U.; Carmassi, C.; Carrà, G.; Cirulli, F.; Dell’Osso, B.; et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. Eur. Psychiatry 2020, 63, e87. [Google Scholar] [CrossRef]
- Jones, H.E.; Manze, M.; Ngo, V.; Lamberson, P.; Freudenberg, N. The Impact of the COVID-19 Pandemic on College Students’ Health and Financial Stability in New York City: Findings from a Population-Based Sample of City University of New York (CUNY) Students. J. Hered. 2021, 98, 187–196. [Google Scholar] [CrossRef]
- Lischer, S.; Safi, N.; Dickson, C. Remote learning and students’ mental health during the COVID-19 pandemic: A mixed-method enquiry. Prospects 2021. [Google Scholar] [CrossRef]
- Wathelet, M.; Duhem, S.; Vaiva, G.; Baubet, T.; Habran, E.; Veerapa, E.; Debien, C.; Molenda, S.; Horn, M.; Grandgenèvre, P.; et al. Factors Associated With Mental Health Disorders Among University Students in France Confined During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2025591. [Google Scholar] [CrossRef]
- Li, Y.; Zhao, J.; Ma, Z.; McReynolds, L.S.; Lin, D.; Chen, Z.; Wang, T.; Wang, D.; Zhang, Y.; Zhang, J.; et al. Mental Health Among College Students During the COVID-19 Pandemic in China: A 2-Wave Longitudinal Survey. J. Affect. Disord. 2021, 281, 597–604. [Google Scholar] [CrossRef]
- Wittchen, H.-U.; Jacobi, F. Size and burden of mental disorders in Europe—a critical review and appraisal of 27 studies. Eur. Neuropsychopharmacol. 2005, 15, 357–376. [Google Scholar] [CrossRef] [Green Version]
- Bandelow, B.; Michaelis, S. Epidemiology of anxiety disorders in the 21st century. Dialog Clin. Neurosci. 2015, 17, 327–335. [Google Scholar]
- Reports_ACHA-NCHAIIc. Available online: https://www.acha.org/NCHA/ACHA-NCHA_Data/Publications_and_Reports/NCHA/Data/Reports_ACHA-NCHAIIc.aspx (accessed on 5 July 2021).
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Auerbach, R.P.; Alonso, J.; Axinn, W.G.; Cuijpers, P.; Ebert, D.D.; Green, J.G.; Hwang, I.; Kessler, R.C.; Liu, H.; Mortier, P.; et al. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychological Med. 2016, 46, 2955–2970. Available online: https://pubmed.ncbi.nlm.nih.gov/27484622/ (accessed on 5 July 2021). [CrossRef] [PubMed] [Green Version]
- Gratz, K.L.; Mann, A.J.; Tull, M.T. Suicidal ideation among university students during the COVID-19 pandemic: Identifying at-risk subgroups. Psychiatry Res. 2021, 302, 114034. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Chen, H.; Liu, L.; Liu, Y.; Zhang, N.; Sun, Z.; Lou, Q.; Ge, W.; Hu, B.; Li, M. Anxiety and Sleep Problems of College Students During the Outbreak of COVID. Front. Psychiatry 2020, 11, 588693. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Drakos, A.; Zuo, Q.K.; Huang, E. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 301, 113863. [Google Scholar] [CrossRef]
- Tasnim, R.; Islam, M.S.; Sujan, M.S.H.; Sikder, M.T.; Potenza, M.N. Suicidal ideation among Bangladeshi university students early during the COVID-19 pandemic: Prevalence estimates and correlates. Child Youth Serv. Rev. 2020, 119, 105703. [Google Scholar] [CrossRef]
- Garlow, S.J.; Rosenberg, J.; Moore, J.D.; Haas, A.P.; Koestner, B.; Hendin, H.; Nemeroff, C.B. Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depress. Anxiety 2008, 25, 482–488. [Google Scholar] [CrossRef]
- Hawton, K.; Comabella, C.C.i.; Haw, C.; Saunders, K. Risk factors for suicide in individuals with depression: A systematic review. J. Affect. Disord. 2013, 147, 17–28. Available online: https://pubmed.ncbi.nlm.nih.gov/23411024/ (accessed on 6 July 2021). [CrossRef]
- Hossain, M. Current status of global research on novel coronavirus disease (COVID-19): A bibliometric analysis and knowledge mapping. F1000Research 2020, 9, 374. [Google Scholar] [CrossRef]
- Li, S.W.; Wang, Y.; Yang, Y.Y.; Lei, X.M.; Yang, Y.F. Analysis of influencing factors of anxiety and emotional disorders in children and adolescents during home isolation during the epidemic of novel coronavirus pneumonia. Chin. J. Child Health 2020, 28, 1–9. [Google Scholar]
- Eskin, M.; Sun, J.-M.; Abuidhail, J.; Yoshimasu, K.; Kujan, O.; Janghorbani, M.; Flood, C.; Carta, M.G.; Tran, U.S.; Mechri, A.; et al. Suicidal Behavior and Psychological Distress in University Students: A 12-nation Study. Arch. Suicide Res. 2016, 20, 369–388. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liyanage, S.; Saqib, K.; Khan, A.F.; Thobani, T.R.; Tang, W.-C.; Chiarot, C.B.; AlShurman, B.A.; Butt, Z.A. Prevalence of Anxiety in University Students during the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 62. https://doi.org/10.3390/ijerph19010062
Liyanage S, Saqib K, Khan AF, Thobani TR, Tang W-C, Chiarot CB, AlShurman BA, Butt ZA. Prevalence of Anxiety in University Students during the COVID-19 Pandemic: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(1):62. https://doi.org/10.3390/ijerph19010062
Chicago/Turabian StyleLiyanage, Shefali, Kiran Saqib, Amber Fozia Khan, Tijhiana Rose Thobani, Wang-Choi Tang, Cameron B. Chiarot, Bara’ Abdallah AlShurman, and Zahid Ahmad Butt. 2022. "Prevalence of Anxiety in University Students during the COVID-19 Pandemic: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 1: 62. https://doi.org/10.3390/ijerph19010062
APA StyleLiyanage, S., Saqib, K., Khan, A. F., Thobani, T. R., Tang, W.-C., Chiarot, C. B., AlShurman, B. A., & Butt, Z. A. (2022). Prevalence of Anxiety in University Students during the COVID-19 Pandemic: A Systematic Review. International Journal of Environmental Research and Public Health, 19(1), 62. https://doi.org/10.3390/ijerph19010062







