Mapping Problematic Drinking Trends over Time in Urban, Semi-Urban, and Rural Populations
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Outcome Variables
Please record how often in the last 12 months you have had each of the following number of standard drinks in a day?
2.3. Other Variables
- (a)
- Likely to be well (10–15)
- (b)
- Likely to have a mild mental disorder (16–21)
- (c)
- Likely to have a moderate mental disorder (22–29)
- (d)
- Likely to have a severe mental disorder (30–50)
2.4. Statistical Analysis
3. Results
3.1. Population Characteristics
3.2. Overall Problematic Drinking Trends over Time by Location
3.2.1. Heavy Episodic Drinking
3.2.2. Long-Term Risky Drinking
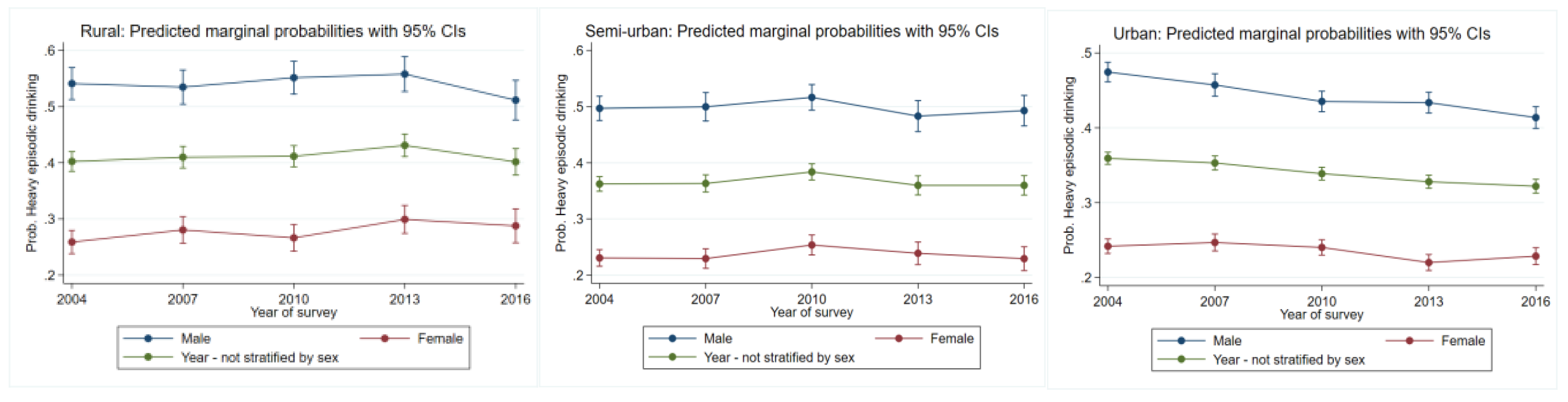
3.3. Problematic Drinking Trends over Time by Sex
3.3.1. Heavy Episodic Drinking
3.3.2. Long-Term Risky Drinking
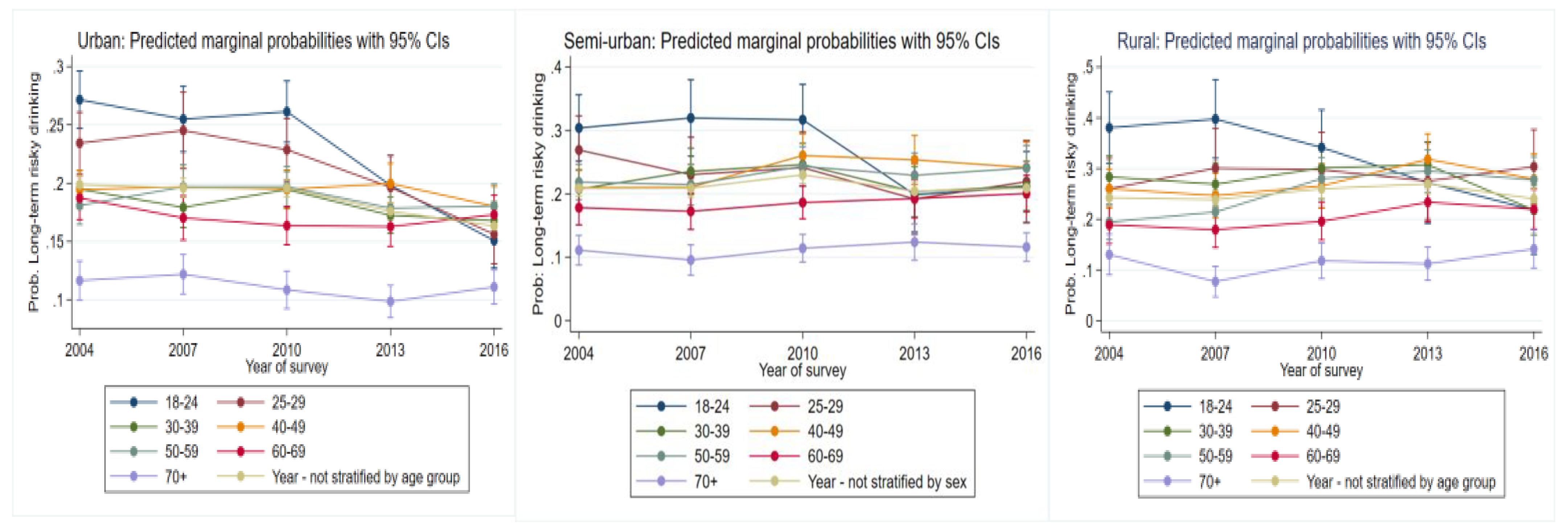
3.4. Problematic Drinking Trends over Time by Age Group
3.4.1. Heavy Episodic Drinking
3.4.2. Long-Term Risky Drinking
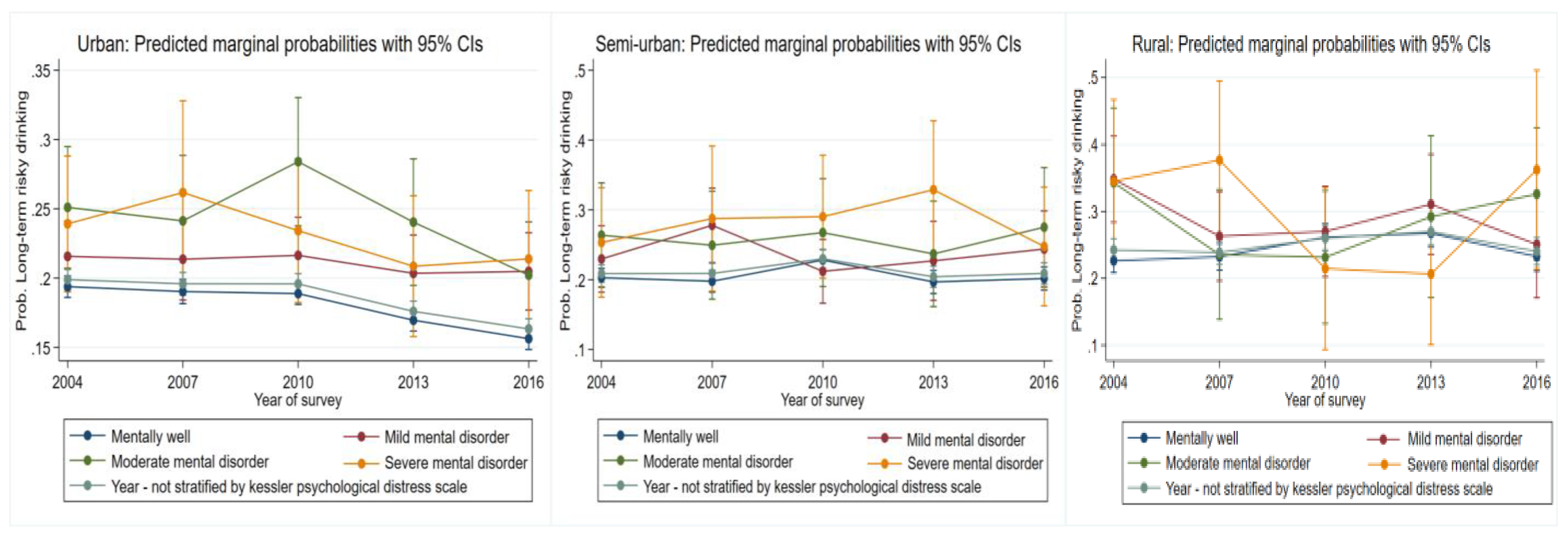
3.5. Problematic Drinking Trends over Time-Based on Psychological Well-Being
3.5.1. Heavy Episodic Drinking
3.5.2. Long-Term Risky Drinking
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilson, M.T. Drinking, anthropology of. IESBS 2015, 6, 658–662. [Google Scholar]
- Kirkby, D. “Beer, glorious beer:” Gender politics and Australian popular culture. J. Pop. Cult 2003, 37, 244–256. [Google Scholar] [CrossRef]
- Inder, J.K.; Handley, E.T.; Fitzgerald, M.; Lewin, J.T.; Coleman, C.; Perkins, D.; Kelly, J.B. Individual and district-level predictors of alcohol use: Cross sectional findings from a rural mental health survey in Australia. BMC Public Health 2012, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ogeil, P.R.; Lloyd, B.; Lam, T.; Lenton, S.; Burns, L.; Aiken, A.; Gilmore, W.; Chikritzhs, T.; Mattick, R.; Allsop, S.; et al. Pre-drinking behaviour of young health drinkers. Subst. Use Misuse 2016, 51, 1297–1306. [Google Scholar] [CrossRef] [PubMed]
- Intarut, N.; Pukdeesamai, P. Socioeconomic inequality in concurrent tobacco and alcohol consumption. Asian Pac. J. Cancer Prev. 2017, 18, 1913–1917. [Google Scholar] [CrossRef]
- Grittner, U.; Kuntsche, S.; Gmel, G.; Bloomfield, K. Alcohol consumption and social inequality at the individual and country levels—results from an international study. Eur. J. Public Health 2013, 23, 332–339. [Google Scholar] [CrossRef]
- Lui, P.P.; Tsong, Y.; Pham, S.; Ramadan, B.; Quezada, L.; Del Rio, M.; Zamboanga, L.B. Explaining the alcohol immigrant paradox: Perspectives from Mexican American adults. J. Lat. Psychol. 2020, 9, 109–124. [Google Scholar] [CrossRef]
- Levitt, E.; Ainuz, B.; Pourmoussa, A.; Acuna, J.; De La Rosa, M.; Zevallos, J.; Wang, W.; Rodriguez, P.; Castro, G.; Sanchez, M. Pre and post-immigration correlates of alcohol misuse among young adult recent latino immigrants: An ecodevelopmental approach. Int. J. Environ. Res. 2019, 16, 439. [Google Scholar]
- Myran, T.D.; Chen, T.J.; Bearnot, B.; Ip, M.; Giesbrecht, N.; Rees, W.V. Alcohol availability across neighborhoods in Ontario following alcohol sales deregulation, 2013–2017. Am. J. Public Health 2019, 109, 899–905. [Google Scholar] [CrossRef]
- Rehm, J. The risk associated with alcohol use and alcoholism. Alcohol Res. Health 2011, 34, 125–143. [Google Scholar]
- Chan, C.K.G.; Leung, K.J.; Quinn, C.; Connor, P.J.; Hides, L.; Gullo, M.J.; Alati, R.; Weier, M.; Kelly, B.A.; Hall, W.D. Trend in alcohol use in Australia over 13 years: Has there been a trend reversal. BMC Public Health 2016, 16, 1070. [Google Scholar] [CrossRef]
- Grech, A.; Ranga, A.; Allman-Farinelli, M. Increases in alcohol intakes are concurrent with higher energy intakes: Trends in alcohol consumption in Australian national surveys from 1983, 1995 and 2012. Nutrients 2017, 9, 944. [Google Scholar] [CrossRef]
- Stickley, A.; Razvodovsky, Y. Alcohol poisoning in Belarus: A comparison of urban-rural trends, 1990–2005. Alcohol Alcohol. 2009, 44, 326–331. [Google Scholar] [CrossRef]
- Vichitkunakorn, P.; Assanangkornchai, S. Trends in inequalities of alcohol-related harms among Thai households: 2007–2017. Drug Alcohol Depend. 2019, 204, 107577. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare (AIHW). Alcohol and Other Drug Use in Regional and Remote Australia: Consumption, Harms and Access to Treatment, 2016–2017; AIHW: Canberra, Australia, 2019. [Google Scholar]
- Duell, N.; Steinberg, L.; Icenogle, G.; Chien, J.; Chaudhary, N.; Giunta, D.L.; Dodge, A.K.; Fanti, A.K.; Lansford, E.J.; Oburu, P.; et al. Age Patterns in Risk Taking Across the World. J. Youth Adolesc. 2018, 47, 1052–1072. [Google Scholar] [CrossRef]
- Chaiyasong, S.; Huckle, T.; Mackintosh, A.; Meier, P.; Parry, H.D.C.; Callinan, S.; Cuong, V.P.; Kazantseva, E.; Gray-Phillip, G.; Parker, K.; et al. Drinking patterns vary by gender, age and country-level income: Cross-country analysis of the International Alcohol Control Study. Drug Alcohol Rev. 2018, 37, 53–62. [Google Scholar]
- Hasin, S.D.; Shmulewitz, D.; Keyes, K. Alcohol use and binge drinking among U.S. men, pregnant and non-pregnant women ages 18–44: 2002–2017. Drug Alcohol Depend. 2019, 205, 107590. [Google Scholar] [PubMed]
- Klimkiewicz, A.; Klimkiewicz, J.; Jakubczyk, A.; Kieres-Salomonski, I.; Wojnar, M. Comorbidity of alcohol dependence with other psychiatric disorders. Part I. Epidemiology of dual diagnosis. Psychiatr. Pol. 2015, 49, 265–275. [Google Scholar]
- Carra, G.; Bartoli, F.; Brambilla, G.; Crocamo, C.; Clerici, M. Comorbid Addiction and Major Mental Illness in Europe: A Narrative Review. Subst. Abus. 2015, 36, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Cucciare, A.M.; Ounpraseuth, T.S.; Curran, M.G.; Booth, M.B. Predictors of mental health and substance use disorder treatment use over 3 years among rural adults using stimulants. Subst. Abus. 2019, 40, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Bozic, S.; Vicendese, D.; Livingston, M.; Erbas, B. The role of psychological distress on long-term risky and heavy episodic drinking patterns in major cities and rural and remote areas. Aust. J. Rural Health 2021. [CrossRef]
- National Health and Medical Research Council (NHMRC). Australian Guidelines to Reduce Risks from Drinking Alcohol; NHMRC: Canberra, Australia, 2009. [Google Scholar]
- Andrews, G.; Slade, T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust. N. Z. J. Public Health 2001, 24, 494–497. [Google Scholar] [CrossRef]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.T.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitory population prevalence’s and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC: College Station, TX, USA, 2019. [Google Scholar]
- Pena, S.; Makela, P.; Valdivi, G.; Helakorpi, S.; Markkula, N.; Margozzini, P.; Koskinen, S. Socioeconomic inequalities in alcohol consumption in Chile and Finland. Drug Alcohol Depend. 2017, 173, 24–30. [Google Scholar] [CrossRef]
- Stelander, T.L.; Hoye, A.; Bramness, G.J.; Selbaek, G.; Lunde, L.; Wynn, R.; Gonli, K.O. The changing alcohol drinking patterns among older adults show that women are closing the gender gap in more frequent drinking: The Tromso study, 1994–2016. Subst. Abus. Treat. Prev. Policy 2016, 16, 45. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.; Ralph, B.; Elliot, K.; Robards, B.; Savic, M.; Lindsay, J.; O’Brien, K.; Lubman, D. Exploring Men’s Risky Drinking Cultures; Victorian Health Promotion Foundation: Melbourne, Australia, 2019. [Google Scholar]
- Hunt, G.; Antin, T. Gender and intoxication: From masculinity to intersectionality. Drugs 2019, 26, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Wilson, I.; Munro, G.; Hagger, A.; Dilkes-Frayne, E. A Survey of Alcohol Sponsorship of Good Sports Clubs; Victorian Health Promotion Foundation: Melbourne, Australia, 2012. [Google Scholar]
- Miller, P.; Droste, N.; Baker, T.; Gervis, C. Last drinks: A study of rural emergency department data collection to identify and target community alcohol-related violence. Emerg. Med. Australas 2015, 27, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Callinan, S.; Livingston, M. Drinking Trends by Age and Over Time among Baby Boomers and Older Drinkers; Foundations for Alcohol Research and Education: Canberra, Australia, 2018. [Google Scholar]
- Ecklund, M.A.; Nederhoff, M.D.; Hunt, L.S.; Horvath, J.K.; Nelson, F.T.; Plum, E.J.; Toomey, L.T. Focus group discussions with bat and restaurant management and staff regarding responsible alcohol beverage service. J. Drug Educ. 2017, 47, 87–107. [Google Scholar] [CrossRef]
- Carrington, K.; McIntosh, A.; Hogg, R.; Scott, J. Safeguarding Rural Australia: Addressing Masculinity and Violence in Rural Settings: Risky Behaviour in a Rural Australian Context: Analysis of Secondary Data Analysis; Centre for Law and Justice—Queensland University of Technology: Brisbane, Australia, 2011. [Google Scholar]
- D’Proff, J.M.; Mills, D.; Gray, R. Expecting the unexpected? Improving rural health in the era of bushfires, novel coronavirus and climate change. Aust. J. Rural Health 2020, 28, 107–109. [Google Scholar]
- Ponizovsky, M.A.; Rosca, P.; Haklai, Z.; Goldberger, N. Trends in dual diagnosis of severe mental illness and substance use disorders, 1996–2010, Israel. Drug Alcohol Depend. 2015, 148, 203–208. [Google Scholar] [CrossRef]
- Slavko, B.; Glavatskiy, K.; Prokopenko, M. City structure shapes directional resettlement flows in Australia. Sci. Rep. 2020, 10, 8235. [Google Scholar] [CrossRef]
- Morley, C.K.; Logge, W.; Pearson, S.; Baillie, A.; Haber, S.P. Socio economic and geographic disparities in access to pharmacotherapy for alcohol dependence. J. Subst. Abus. Treat. 2017, 74, 23–25. [Google Scholar] [CrossRef] [PubMed]
- Roche, A.; Pidd, K.; Kostadinov, V. Alcohol and drug related absenteeism: A costly problem. Aust. N. Z. J. Public Health 2015, 40, 236–239. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Youde, J. Globalization and Health; Rowman & Littlefield Publishers: Lanham, MD, USA, 2019. [Google Scholar]
- Macera, C.A.; Jackson, K.L.; Davis, D.R.; Kronfeld, J.J.; Blair, S.N. Patterns of non-response to a mail survey. J. Clin. Epidemiol. 1990, 43, 1427–1430. [Google Scholar] [CrossRef]
- Barbosa, C.; Cowell, J.; Dowd, N.W. Alcohol Consumption in Response to the COVID-19 Pandemic in the United States. J. Addict. Med. 2020, 15, 341–344. [Google Scholar] [CrossRef]



| Urban N = 80,458 | Heavy Episodic Drinking | Year | ||||
|---|---|---|---|---|---|---|
| 2007 | 2010 | 2013 | 2016 | |||
| Main Effects OR (CI) for Covariates Below | Covariate X Year Interaction OR (CI) | |||||
| Sex (Ref-Male) | Female | 0.30(0.28–0.33) | 1.13(0.99–1.30) | 1.22(1.08–1.39) | 1.11(0.97–1.26) | 1.31(1.15–1.49) |
| Age group (Ref-18–24) | 25–29 | 0.73(0.61–0.88) | 1.17(0.87–1.55) | 0.97(0.75–1.28) | 1.07(0.81–1.40) | 1.15(0.86–1.52) |
| 30–39 | 0.43(0.37–0.50) | 1.02(0.80–1.29) | 1.10(0.88–1.38) | 1.13(0.90–1.42) | 1.58(1.26–2.00) | |
| 40–49 | 0.30(0.26–0.35) | 1.10(0.86–1.40) | 1.22(0.97–1.54) | 1.42(1.12–1.80) | 2.00(1.58–2.53) | |
| 50–59 | 0.19(0.16–0.22) | 1.22(0.95–1.56) | 1.36(1.07–1.72) | 1.59(1.24–2.03) | 2.19(1.71–2.81) | |
| 60–69 | 0.12(0.10–0.14) | 1.09(0.83–1.43) | 1.30(1.00–1.68) | 1.53(1.78–1.99) | 2.31(1.78–3.00) | |
| 70+ | 0.06(0.04–0.06) | 1.25(0.90–1.72) | 1.07(0.78–1.47) | 1.25(0.91–1.71) | 1.98(1.45–2.71) | |
| Kessler (Ref–Well) | Mild | 1.19(1.02–1.39) | 0.97(0.78–1.22) | 1.01(0.80–1.26) | 1.10(0.80–1.26) | 1.11(0.89–1.39) |
| Moderate | 1.41(1.12–1.78) | 0.78(0.54–1.13) | 0.92(0.66–1.29) | 0.98(0.70–1.38) | 1.15(0.84–1.59) | |
| Severe | 1.02(0.77–1.34) | 1.15(0.74–1.80) | 1.06(0.71–1.58) | 1.18(0.78–1.80) | 1.40(0.95–2.08) | |
| Semi-Urban N = 25,053 | ||||||
| Sex (Ref-Male) | Female | 0.23(0.20–0.27) | 1.01(0.89–1.28) | 1.10 (0.88–1.37) | 1.21 (0.95–1.54) | 1.11(0.87–1.42) |
| Age group (Ref-18–24) | 25–29 | 0.47(0.32–0.68) | 1.37(0.78–2.41) | 1.16 (0.67–2.00) | 1.74(0.97–3.14) | 1.89(1.05–3.41) |
| 30–39 | 0.34(0.25–0.46) | 1.43(0.90–2.27) | 1.28 (0.82–2.02) | 1.68(1.02–2.77) | 1.74(1.04–2.90) | |
| 40–49 | 0.21(0.16–0.29) | 1.47(0.92–2.36) | 1.53(0.97–2.42) | 2.44(1.49–4.00) | 1.71(1.02–2.86) | |
| 50–59 | 0.13(0.09–0.18) | 1.36(0.85–2.19) | 1.45(0.92–2.29) | 2.13(1.29–3.52) | 2.28(1.37–3.79) | |
| 60–69 | 0.06(0.05–0.09) | 1.57(0.95–2.57) | 1.48(0.92–2.38) | 2.14(1.26–3.62) | 2.44(1.45–4.13) | |
| 70+ | 0.03(0.02–0.04) | 1.39(0.78–2.47) | 1.20(0.69–2.08) | 1.78(0.97–3.28) | 1.99(1.11–3.58) | |
| Kessler (Ref–Well) | Mild | 1.12(0.93–1.58) | 1.33(0.89–1.98) | 0.91(0.62–1.35) | 1.29(0.84–1.98) | 0.89(0.57–1.38) |
| Moderate | 1.31(0.91–1.90) | 1.08(0.61–1.90) | 0.92(0.53–1.57) | 0.73(0.39–1.38) | 1.23(0.70–2.15) | |
| Severe | 1.31(0.86–2.00) | 1.04(0.55–1.97) | 1.12(0.55–2.27) | 1.68(0.91–3.09) | 1.05(0.56–1.97) | |
| Rural N = 19,058 | ||||||
| Sex (Ref-Male) | Female | 0.23(0.18–0.28) | 1.15(0.85–1.56) | 1.05(0.78–1.41) | 1.26(0.94–1.69) | 1.54(1.13–2.09) |
| Age group (Ref-18–24) | 25–29 | 0.65(0.41–1.04) | 0.83(0.41–1.67) | 1.00(0.51–2.00) | 0.89(0.43–1.82) | 1.72(0.79–3.74) |
| 30–39 | 0.40(0.26–0.60) | 0.88(0.48–1.62) | 1.20(0.66–2.19) | 1.10(0.59–2.08) | 1.95(0.96–3.97) | |
| 40–49 | 0.24(0.16–0.37) | 1.05(0.57–1.97) | 1.38(0.75–2.52) | 1.75(0.92–3.32) | 2.89(1.42–5.88) | |
| 50–59 | 0.11(0.07–0.17) | 1.05(0.56–1.98) | 1.97(1.07–3.64) | 2.03(1.06–3.88) | 3.85(1.88–7.87) | |
| 60–69 | 0.08(0.05–0.12) | 0.73(0.38–1.42) | 1.14(0.60–2.19) | 1.60(0.82–3.14) | 2.96(1.42–6.16) | |
| 70+ | 0.03(0.02–0.06) | 0.58(0.26–1.32) | 1.26(0.58–2.72) | 1.03(0.47–2.27) | 2.54(1.11–5.86) | |
| Kessler (Ref–Well) | Mild | 1.70(1.21–2.39) | 0.66(0.39–1.12) | 0.60(0.35–1.02) | 0.72(0.43–1.20) | 0.59(0.32–1.09) |
| Moderate | 1.26(0.72–2.20) | 0.89(0.38–2.11) | 1.04(0.48–2.26) | 0.51(0.23–1.16) | 1.32(0.65–2.70) | |
| Severe | 0.82(0.46–1.48) | 1.96(0.88–4.34) | 3.43(1.55–7.61) | 1.24(0.50–3.08) | 1.51(0.65–3.54) | |
| Urban N = 80,458 | Long-Term Risky Drinking | Year | ||||
|---|---|---|---|---|---|---|
| 2007 | 2010 | 2013 | 2016 | |||
| Main Effects OR (CI) for Covariates | Covariate X Year Interaction OR (CI) | |||||
| Sex (Ref-Male) | Female | 0.27(0.25–0.30) | 1.24(1.06–1.44) | 1.23(1.06–1.41) | 1.16(1.00–1.34) | 1.28(1.10–1.49) |
| Age group (Ref-18–24) | 25–29 | 0.81(0.66–0.99) | 1.17(0.85–1.61) | 1.03(0.76–1.38) | 1.22(0.89–1.69) | 1.29(0.91–1.82) |
| 30–39 | 0.63(0.53–0.75) | 0.99(0.76–1.29) | 1.06(0.83–1.36) | 1.33(1.02–1.74) | 1.81(1.36–2.41) | |
| 40–49 | 0.63(0.53–0.75) | 1.12(0.86–1.46) | 1.07(0.83–1.37) | 1.61(1.23–2.10) | 1.98(1.49–2.64) | |
| 50–59 | 0.57(0.48–0.68) | 1.23(0.94–1.61) | 1.91(0.92–1.54) | 1.53(1.16–2.02) | 2.19(1.63–2.93) | |
| 60–69 | 0.60(0.50–0.72) | 0.98(0.74–1.30) | 0.90(0.69–1.17) | 1.30(0.98–1.73) | 1.98(1.48–2.66) | |
| 70+ | 0.33(0.27–0.41) | 1.17(0.86–1.60) | 0.90(0.72–1.35) | 1.29(0.94–1.77) | 2.09(1.51–2.90) | |
| Kessler (Ref–Well) | Mild | 1.16(0.97–1.37) | 1.01(0.77–1.31) | 1.04(0.81–1.33) | 1.10(0.85–1.42) | 1.22(0.94–1.58) |
| Moderate | 1.43(1.10–1.86) | 0.96(0.66–1.41) | 1.23(0.86–1.77) | 1.11(0.76–1.62) | 0.97(0.67–1.40) | |
| Severe | 1.34(0.99–1.80) | 1.16(0.72–1.86) | 1.00(0.65–1.54) | 0.98(0.63–1.53) | 1.12(0.72–1.72) | |
| Semi Urban N = 25,053 | ||||||
| Sex (Ref-Male) | Female | 0.20(1.17–0.24) | 1.15(0.88–1.50) | 1.28(1.00–1.64) | 1.14(0.86–1.50) | 1.26(0.97–1.65) |
| Age group (Ref-18–24) | 25–29 | 0.83(0.55–1.25) | 0.74(0.93–1.38) | 0.80(0.44–1.47) | 1.16(0.58–2.31) | 1.28(0.65–2.52) |
| 30–39 | 0.57(0.40–0.80) | 1.10(0.66–1.85) | 1.20(0.74–1.96) | 1.82(1.01–3.28) | 1.79(1.02–3.11) | |
| 40–49 | 0.57(0.41–0.81) | 0.93(0.56–1.56) | 1.29(0.80–2.08) | 2.45(1.39–4.33) | 2.10(1.21–3.63) | |
| 50–59 | 0.61(0.44–0.85) | 0.91(0.55–1.49) | 1.10(0.69–1.77) | 2.00(1.14–3.52) | 1.98(1.12–3.37) | |
| 60–69 | 0.46(0.33–0.65) | 0.89(0.53–1.49) | 1.01(0.62–1.64) | 2.08(1.18–3.67) | 2.03(1.18–3.45) | |
| 70+ | 0.26(0.18–0.37) | 0.78(0.44–1.38) | 0.99(0.59–1.69) | 2.15(1.16–3.97) | 1.84(1.04–3.26) | |
| Kessler (Ref–Well) | Mild | 1.19(0.97–1.64) | 1.38(0.88–2.17) | 0.76(0.48–1.18) | 1.02(0.63–1.67) | 1.10(0.69–1.74) |
| Moderate | 1.47(0.94–2.30) | 0.95(0.49–1.83) | 0.59(0.46–1.62) | 0.88(0.46–1.70) | 1.06(0.55–2.06) | |
| Severe | 1.38(0.85–2.23) | 1.26(0.59–2.69) | 1.04(0.52–2.06) | 1.56(0.77–3.18) | 0.97(0.48–1.95) | |
| Rural N = 19,058 | ||||||
| Sex (Ref-Male) | Female | 0.22(0.18–0.28) | 1.15(0.84–1.57) | 1.06(0.78–1.45) | 1.23(0.90–1.66) | 1.32(0.95–1.82) |
| Age group (Ref-18–24) | 25–29 | 0.53(0.33–0.86) | 1.17(0.56–2.42) | 1.49(0.73–3.08) | 1.91(0.89–4.10) | 3.02(1.34–6.85) |
| 30–39 | 0.61(0.41–0.91) | 0.86(0.48–1.56) | 1.34(0.74–2.42) | 1.98(1.04–3.74) | 1.64(0.78–3.45) | |
| 40–49 | 0.53(0.36–0.80) | 0.87(0.47–1.58) | 1.26(0.69–2.29) | 2.38(1.25–4.55) | 2.66(1.29–5.50) | |
| 50–59 | 0.35(0.23–0.54) | 1.07(0.59–1.96) | 2.06(1.13–3.75) | 3.19(1.68–6.06) | 3.98(1.93–8.22) | |
| 60–69 | 0.34(0.22–0.52) | 0.88(0.47–1.64) | 1.28(0.69–2.39) | 2.36(1.23–4.54) | 2.97(1.43–6.18) | |
| 70+ | 0.21(0.13–0.35) | 0.52(0.24–1.11) | 1.09(0.54–2.25) | 1.50(1.23–4.54) | 2.70(1.20–6.07) | |
| Kessler (Ref–Well) | Mild | 1.99(1.40–2.82) | 0.60(0.35–1.04) | 0.53(0.31–0.90) | 0.64(0.37–1.08) | 0.56(0.31–1.01) |
| Moderate | 1.93(1.07–3.49) | 0.53(0.23–1.24) | 0.43(0.18–1.02) | 0.59(0.24–1.43) | 0.86(0.39–1.87) | |
| Severe | 1.95(1.03–3.70) | 1.13(0.47–2.71) | 0.38(0.14–1.07) | 0.35(0.14–0.92) | 1.01(0.39–2.66) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bozic, S.; Vicendese, D.; Livingston, M.; Erbas, B. Mapping Problematic Drinking Trends over Time in Urban, Semi-Urban, and Rural Populations. Int. J. Environ. Res. Public Health 2022, 19, 589. https://doi.org/10.3390/ijerph19010589
Bozic S, Vicendese D, Livingston M, Erbas B. Mapping Problematic Drinking Trends over Time in Urban, Semi-Urban, and Rural Populations. International Journal of Environmental Research and Public Health. 2022; 19(1):589. https://doi.org/10.3390/ijerph19010589
Chicago/Turabian StyleBozic, Stefan, Don Vicendese, Michael Livingston, and Bircan Erbas. 2022. "Mapping Problematic Drinking Trends over Time in Urban, Semi-Urban, and Rural Populations" International Journal of Environmental Research and Public Health 19, no. 1: 589. https://doi.org/10.3390/ijerph19010589
APA StyleBozic, S., Vicendese, D., Livingston, M., & Erbas, B. (2022). Mapping Problematic Drinking Trends over Time in Urban, Semi-Urban, and Rural Populations. International Journal of Environmental Research and Public Health, 19(1), 589. https://doi.org/10.3390/ijerph19010589





