Factors Influencing Protective Behaviors for Dental Radiation Exposure among Female Korean Dental Hygienists Using Health Belief Model
Abstract
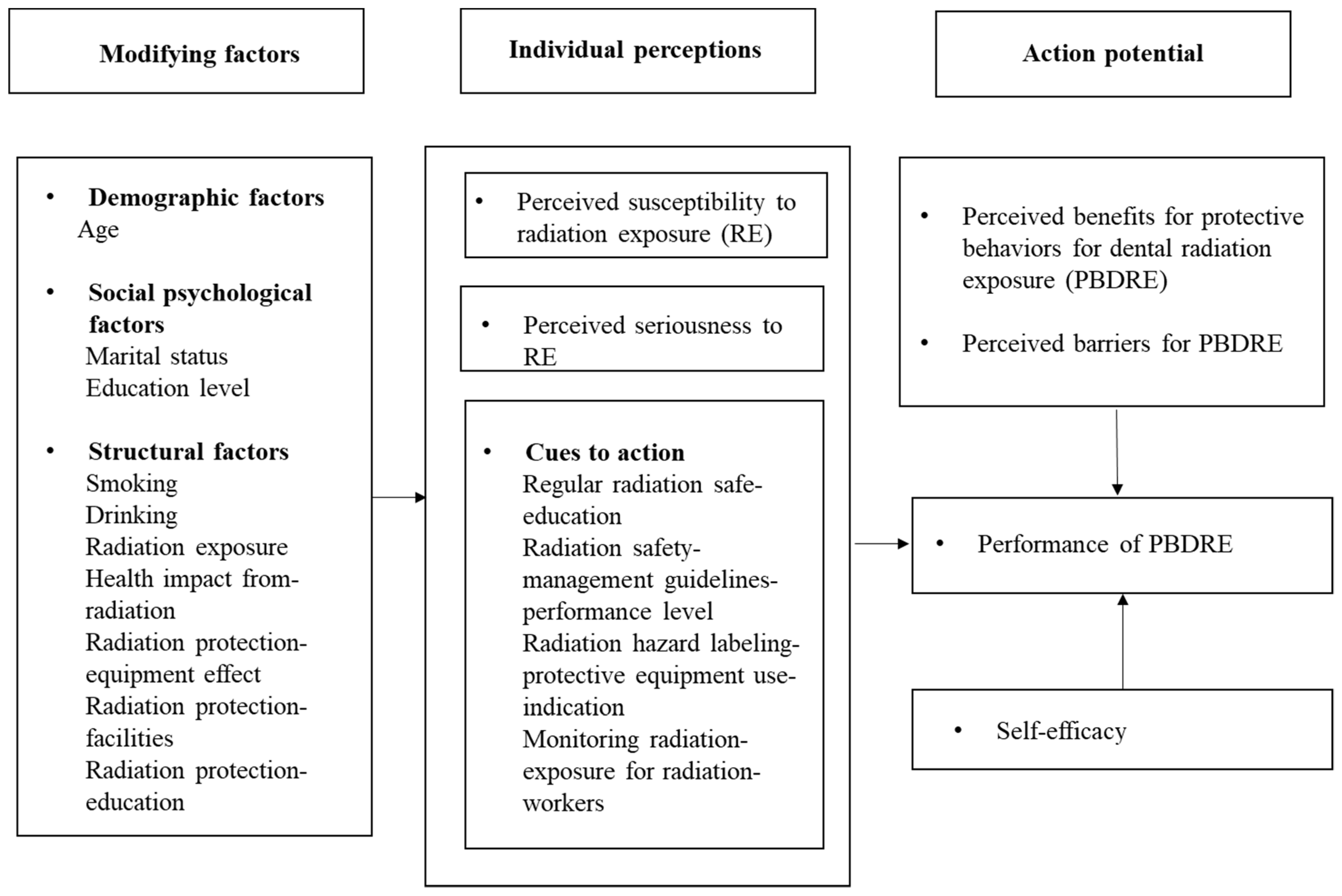
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Consideration
2.2. Participants and Data Collection
2.3. Variables
2.3.1. Modifying Factors
2.3.2. HBM Assessment
2.3.3. Self-Efficacy Assessment
2.3.4. Dependent Variable Assessment
2.4. Statistical Analysis
3. Results
3.1. PBDRE According to General Characteristics
3.2. Component Distribution of HBM
3.3. Correlations among Protective Behaviors for Radiation Exposure Factors of HBM
3.4. Hierarchical Multiple Regression Analysis of Protective Behaviors for Radiation Exposure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wenzel, A.; Gröndahl, H.G. Direct digital radiography in the dental office. Int. Dent. J. 1995, 45, 27–34. [Google Scholar] [PubMed]
- Pakravan, A.H.; Aghamiri, S.M.R.; Bamdadian, T.; Gholami, M.; Moshfeghi, M. Dosimetry of Occupational Radiation around Panoramic X-ray Apparatus. J. Biomed. Phys. Eng. 2019, 9, 525–532. [Google Scholar] [CrossRef]
- Jang, J.-H.; Lee, H.-N.; Lim, C.-H. The effect of occupational exposure on quality of life in dental hygienists. J. Korean Soc. Dent. Hyg. 2010, 10, 717–725. [Google Scholar]
- Wenzel, A. Digital radiography and caries diagnosis. Dentomaxillofac. Radiol. 1998, 27, 3–11. [Google Scholar] [CrossRef]
- Garg, A.K.; Vicari, A. Radiographic modalities for diagnosis and treatment planning in implant dentistry. Implant Soc. 1995, 5, 7–11. [Google Scholar] [PubMed]
- Silva, M.A.G.; Wolf, U.; Heinicke, F.; Bumann, A.; Visser, H.; Hirsch, E. Cone-beam computed tomography for routine orthodontic treatment planning: A radiation dose evaluation. Am. J. Orthod. Dentofacial Orthop. 2008, 133, 640.e1–640.e5. [Google Scholar] [CrossRef] [PubMed]
- Bruks, A.; Enberg, K.; Nordqvist, I.; Hansson, A.S.; Jamsson, L.; Svenson, B. Radiographic examinations as an aid to orthodontic diagnosis and treatment planning. Swed. Dent. J. 1999, 23, 77–85. [Google Scholar]
- Hwang, S.-Y.; Choi, E.-S.; Kim, Y.-S.; Gim, B.-E.; Ha, M.; Kim, H.-Y. Health effects from exposure to dental diagnostic X-ray. Environ. Health Toxicol. 2018, 33, e2018017. [Google Scholar] [CrossRef]
- Roden, J. Revisiting the health belief model: Nurses applying it to young families and their health promotion needs. Nurs. Health Sci. 2004, 6, 1–10. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191. [Google Scholar] [CrossRef]
- Kim, M.-J.; Yun, S.-J. Convergence Study on the Factors Influencing Nursing Students’ Attitudes toward Standard Precautions: Focusing on the Health Belief Model. J. Korea Conv. Soc. 2018, 9, 77–88. [Google Scholar] [CrossRef]
- Kim, M.-J.; Park, J. The association between health beliefs and receiving hepatitis B vaccinations among college students. J. Dig. Conv. 2012, 10, 309–316. [Google Scholar]
- Solhi, M.; Shojaei Zadeh, D.; Seraj, B.; Faghih Zadeh, S. The application of the health belief model in oral health education. Iran. J. Public Health 2010, 39, 114–119. [Google Scholar] [PubMed]
- Goodarzi, A.; Heidarnia, A.; Tavafian, S.S.; Eslami, M. Predicting oral health behaviors among Iranian students by using health belief model. J. Educ. Health Promot. 2019, 8, 10. [Google Scholar] [PubMed]
- Kang, S.G.; Lee, E.N. Knowledge of radiation protection and the recognition and performance of radiation protection behavior among perioperative nurses. J. Muscle Joint Health 2013, 20, 247–257. [Google Scholar] [CrossRef][Green Version]
- Muzzin, K.B.; Flint, D.J.; Schneiderman, E. Dental radiography-prescribing practices: A nationwide survey of dental hygienists. Gen. Dent. 2019, 67, 38–53. [Google Scholar]
- Lintag, K.; Bruhn, A.M.; Tolle, S.L.; Diawara, N. Radiation safety practices of dental hygienists in the United States. J. Dent. Hyg. 2019, 93, 14–23. [Google Scholar]
- Korea Ministry of Health and Welfare and Korea Institute for Health and Social Affairs. Health and Medical Workforce Survey Policy Report from 5th February 2020. Available online: http://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=032901&page=1&CONT_SEQ=352714 (accessed on 27 December 2021).
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. A Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Bohanny, W.; Wu, S.F.; Liu, C.Y.; Yeh, S.H.; Tsay, S.L.; Wang, T.J. Health literacy, self-efficacy, and self-care behaviors in patients with type 2 diabetes mellitus. J. Am. Assoc. Nurse Pract. 2013, 25, 495–502. [Google Scholar] [CrossRef]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the health belief model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef]
- Sherer, M.; Maddux, J.E.; Mercandante, B.; Prentice-Dunn, S.; Jacobs, B.; Rogers, R.W. The self-efficacy scale: Construction and validation. Psychol. Rep. 1982, 51, 663–671. [Google Scholar] [CrossRef]
- Kim, M. Health promoting begaviors and their relationship with self-efficacy of health workers. Iran J. Nurs. 2017, 30, 68–79. [Google Scholar]
- Han, E.O.; Jun, S.H. Relationship between knowledge, attitude, behavior, and self-efficacy on the radiation safety on dental hygienist. J. Radiat. Ind. 2008, 2, 185–192. [Google Scholar]
- Yoon, J.A.; Yoon, Y.-S. Comparing with self-efficacy and knowledge, attitudes about radiation safety management of dental hygienists and students at department of dental hygiene. J. Korean Soc. Dent. Hyg. 2011, 11, 729–739. [Google Scholar]
- Kim, J.; Kim, J.S.; Kim, H. Factors affecting radiation protection behaviors among operating room nurses. Korean J. Adult Nurs. 2016, 28, 680–690. [Google Scholar] [CrossRef]
- Jeong, Y.-H.; Kwon, Y.-O.; Lee, J.-Y.; Heo, S.-E.; Yoon, Y.-S. Factors that affect the behavior on the radiation safety management for dental hygienists. J. Dent. Hhy. Sci. 2011, 11, 471–479. [Google Scholar]
- Yoon, J.A.; Yoon, Y.-S. A survey about the knowledge, attitudes and behavior for radiation safety management of operating room nurse and dental hygienists. J. Dent. Hyg. Sci. 2014, 14, 230–239. [Google Scholar]
- Yoon, J.-A. Comparative study on radiation safety management knowledge, attitudes and behavior of career dental hygienists and new dental hygienists. J. Dent. Hyg. Sci. 2011, 11, 173–179. [Google Scholar]
- Booshehri, M.Z.; Fatemeh, E.-A.; Nozari, H. Evaluation of dentists’ awareness about personnel and patients national protection in Yazd dental office. Health 2012, 4, 490–492. [Google Scholar] [CrossRef]
- Lee, C.I.; Haims, A.H.; Monico, E.P.; Brink, J.A.; Forman, H.P. Diagnostic CT scans: Assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology 2004, 231, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Shiralkar, S.; Rennie, A.; Snow, M.; Galland, R.B.; Lewis, M.H.; Gower-Thoma, K. Doctors’ knowledge of radiation exposure: Questionnaire study. BMJ 2003, 327, 371–372. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.S. The associated factors of protective behaviors for radiation exposure based on health belief model Honam province radiologic technologists. J. Korea Acad-Ind Coop. Soc. 2020, 21, 96–107. [Google Scholar]
| Characteristics | Category | n | Mean | SD | t or F | p-Value (scheff) |
|---|---|---|---|---|---|---|
| Age (in years) | 20~29 a | 130 | 2.87 | 0.79 | 4.36 | 0.014 a,b < c |
| 30~39 a | 64 | 2.94 | 0.78 | |||
| ≥40 b | 9 | 3.70 | 1.28 | |||
| Marital status | Unmarried | 149 | 2.87 | 0.79 | −1.84 | 0.067 |
| Married | 54 | 3.11 | 0.91 | |||
| Education level | College | 179 | 2.88 | 0.81 | −2.60 | 0.016 |
| ≥Graduate school | 24 | 3.34 | 0.83 | |||
| Smoking | No | 200 | 2.93 | 0.82 | 0.74 | 0.459 |
| Yes | 3 | 3.28 | 1.14 | |||
| Drinking | No | 27 | 2.79 | 1.00 | −0.97 | 0.332 |
| Yes | 176 | 2.95 | 0.80 | |||
| Radiation exposure (times/day) | <5 times/day | 56 | 2.94 | 0.88 | 1.89 | 0.133 |
| 6~10 times/day | 94 | 3.05 | 0.75 | |||
| 11~15 times/day | 35 | 2.74 | 0.82 | |||
| ≥16 times/day | 18 | 2.66 | 0.96 | |||
| Health impact from radiation exposure | Very likely a | 81 | 2.76 | 0.78 | 3.20 | 0.043 c < b < a |
| Moderate b | 79 | 3.01 | 0.84 | |||
| Not at all c | 43 | 3.10 | 0.84 | |||
| Radiation protection- equipment effect | Very likely | 135 | 2.97 | 0.80 | 2.36 | 0.097 |
| Moderate | 61 | 2.93 | 0.87 | |||
| Not at all | 7 | 2.27 | 0.80 | |||
| Radiation protection facilities | Sufficient a | 58 | 3.49 | 0.75 | 30.04 | <0.001 c < b < a |
| Moderate b | 86 | 2.88 | 0.79 | |||
| Insufficient c | 59 | 2.45 | 0.59 | |||
| Radiation protection education | Yes | 78 | 3.38 | 0.78 | 6.63 | <0.001 |
| No | 125 | 2.65 | 0.73 |
| Characteristics | Range | Min | Max | Mean ± SD |
|---|---|---|---|---|
| Perceived susceptibility to RE | 1–5 | 1.50 | 5.00 | 3.62 ± 0.65 |
| Perceived seriousness of RE | 1–5 | 1.00 | 5.00 | 3.76 ± 0.99 |
| Perceived benefits of PBDRE | 1–5 | 2.00 | 5.00 | 3.75 ± 0.66 |
| Perceived barriers to PBDRE | 1–5 | 1.00 | 5.00 | 3.41 ± 0.88 |
| Cues to action to PBDRE | 1–5 | 1.00 | 5.00 | 2.78 ± 0.95 |
| PBDRE | 1–5 | 1.00 | 5.00 | 2.93 ± 0.83 |
| Self-efficacy | 1–5 | 1.29 | 4.24 | 2.66 ± 0.48 |
| Characteristics | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Perceived susceptibility to RE | 1 | ||||||
| 2. Perceived seriousness of RE | 0.66 ** | 1 | |||||
| 3. Perceived benefits of PBDRE | 0.15 * | 0.15 * | 1 | ||||
| 4. Perceived barriers to PBDRE | 0.36 ** | 0.40 ** | −0.03 | 1 | |||
| 5. Cues to action to PBDRE | −0.18 | −0.13 | 0.22 ** | −0.33 ** | 1 | ||
| 6. Self-efficacy | 0.07 | 0.07 | −0.12 | 0.21 ** | −0.08 | 1 | |
| 7. PBDRE | −0.18 ** | −0.17 * | 0.28 ** | −0.42 ** | 0.52 ** | 0.10 | 1 |
| Characteristics | Model 1 | Model 2 | Model 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | β | t | p-Value | B | β | t | p-Value | B | β | t | p-Value | |
| Constant | 2.85 | 16.33 | <0.001 | 2.19 | 6.58 | <0.001 | 2.20 | 4.49 | <0.001 | |||
| Age (ref. 20–29) | ||||||||||||
| 30–39 | 0.03 | 0.02 | 0.26 | 0.798 | 0.04 | 0.03 | 0.43 | 0.666 | 0.03 | 0.02 | 0.29 | 0.775 |
| 40–49 | 0.53 | 0.13 | 2.19 | 0.029 | 0.56 | 0.14 | 2.40 | 0.017 | 0.41 | 0.10 | 1.73 | 0.084 |
| Education level (ref. College) | ||||||||||||
| ≥Graduate | 0.28 | 0.11 | 1.78 | 0.077 | 0.25 | 0.10 | 1.69 | 0.092 | 0.18 | 0.07 | 1.21 | 0.228 |
| Radiation protection facilities (ref. Insufficient) | ||||||||||||
| Sufficient | 0.77 | 0.42 | 5.35 | <0.001 | 0.57 | 0.31 | 3.93 | <0.001 | 0.44 | 0.24 | 2.87 | 0.005 |
| Moderate | 0.22 | 0.13 | 1.73 | 0.086 | 0.19 | 0.12 | 1.57 | 0.119 | 0.13 | 0.08 | 1.03 | 0.305 |
| Radiation protection education (ref. Yes) | ||||||||||||
| No | −0.51 | −0.30 | −4.85 | <0.001 | −0.31 | −0.19 | −2.88 | 0.004 | −0.28 | −0.17 | −2.62 | 0.010 |
| Health effect (ref. Not at all) | ||||||||||||
| Very likely | 0.00 | 0.00 | 0.00 | 0.997 | 0.12 | 0.07 | 0.77 | 0.440 | 0.15 | 0.09 | 0.96 | 0.337 |
| Moderate | 0.04 | 0.02 | 0.32 | 0.748 | 0.09 | 0.05 | 0.69 | 0.488 | 0.12 | 0.07 | 0.95 | 0.344 |
| Perceptions | ||||||||||||
| Perceived susceptibility to RE | −0.07 | −0.06 | −0.73 | 0.464 | −0.08 | −0.06 | −0.83 | 0.409 | ||||
| Perceived seriousness of RE | 0.01 | 0.01 | 0.08 | 0.938 | 0.00 | 0.00 | 0.00 | 0.997 | ||||
| Cues to action to PBDRE | 0.28 | 0.32 | 4.76 | <0.001 | 0.24 | 0.28 | 4.16 | <0.001 | ||||
| Likelihood of action | ||||||||||||
| Perceived benefits to PBDRE | 0.21 | 0.17 | 3.02 | 0.003 | ||||||||
| Perceived barriers to PBDRE | −0.11 | −0.12 | −1.68 | 0.095 | ||||||||
| Self-efficacy | −0.09 | −0.06 | −0.94 | 0.351 | ||||||||
| F (p) | 13.24 (p < 0.001) | 12.69 (p < 0.001) | 11.50 (p < 0.001) | |||||||||
| R2 | 0.35 | 0.42 | 0.46 | |||||||||
| Adjusted R2 | 0.33 | 0.39 | 0.42 | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, S.-Y.; Park, J.-E.; Jang, J.-H. Factors Influencing Protective Behaviors for Dental Radiation Exposure among Female Korean Dental Hygienists Using Health Belief Model. Int. J. Environ. Res. Public Health 2022, 19, 518. https://doi.org/10.3390/ijerph19010518
Hwang S-Y, Park J-E, Jang J-H. Factors Influencing Protective Behaviors for Dental Radiation Exposure among Female Korean Dental Hygienists Using Health Belief Model. International Journal of Environmental Research and Public Health. 2022; 19(1):518. https://doi.org/10.3390/ijerph19010518
Chicago/Turabian StyleHwang, Su-Yeon, Jung-Eun Park, and Jong-Hwa Jang. 2022. "Factors Influencing Protective Behaviors for Dental Radiation Exposure among Female Korean Dental Hygienists Using Health Belief Model" International Journal of Environmental Research and Public Health 19, no. 1: 518. https://doi.org/10.3390/ijerph19010518
APA StyleHwang, S.-Y., Park, J.-E., & Jang, J.-H. (2022). Factors Influencing Protective Behaviors for Dental Radiation Exposure among Female Korean Dental Hygienists Using Health Belief Model. International Journal of Environmental Research and Public Health, 19(1), 518. https://doi.org/10.3390/ijerph19010518







