Biomechanical Exposure to Upper Extremity Musculoskeletal Disorder Risk Factors in Hospital Laboratories
Abstract
1. Introduction
2. Methods
2.1. Study Site and Subjects
2.2. Job Documentation
2.3. PATH Data Collection
2.4. Data Management
2.5. Data Analysis
3. Results
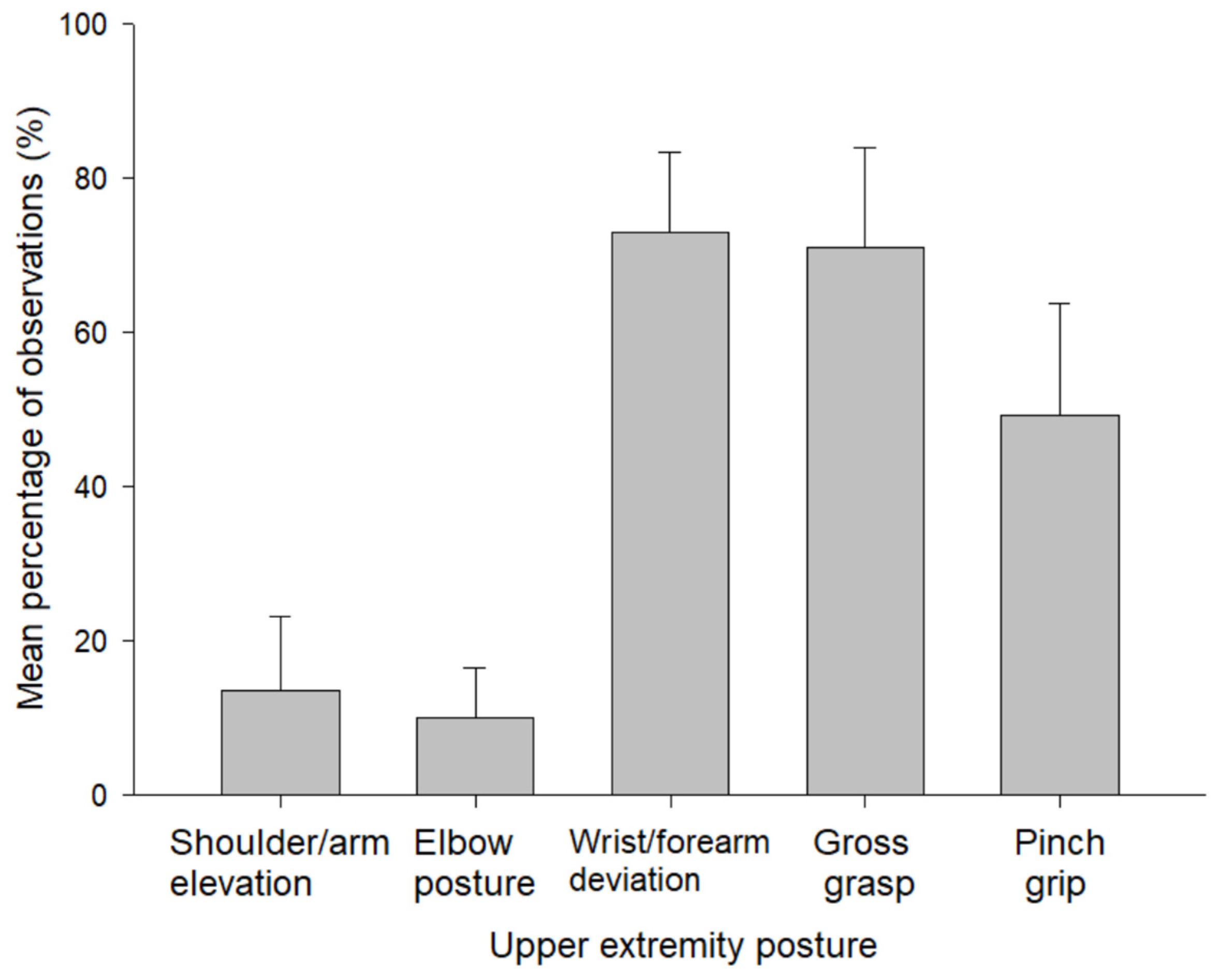
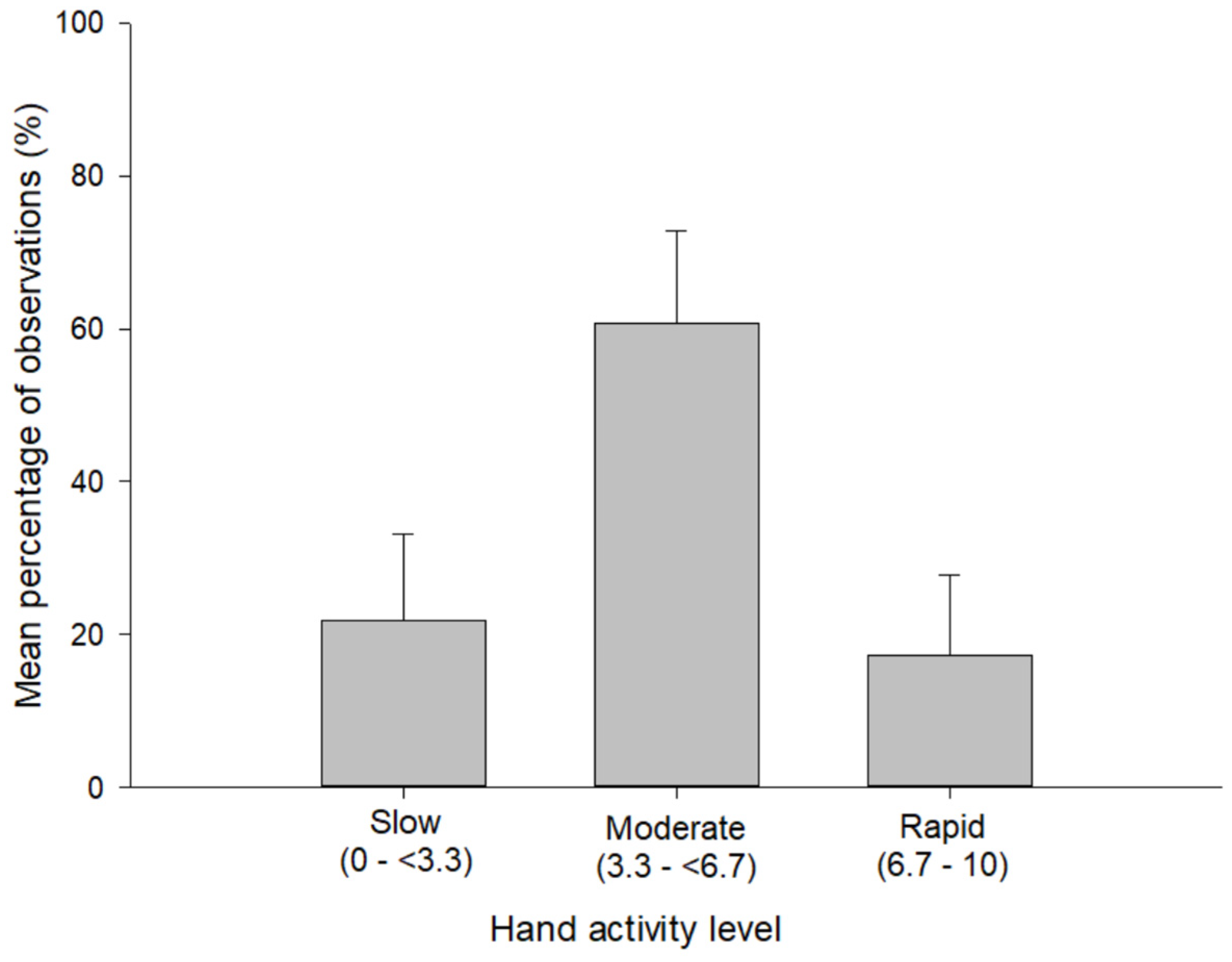
3.1. Exposure to Biomechanical Risk Factors
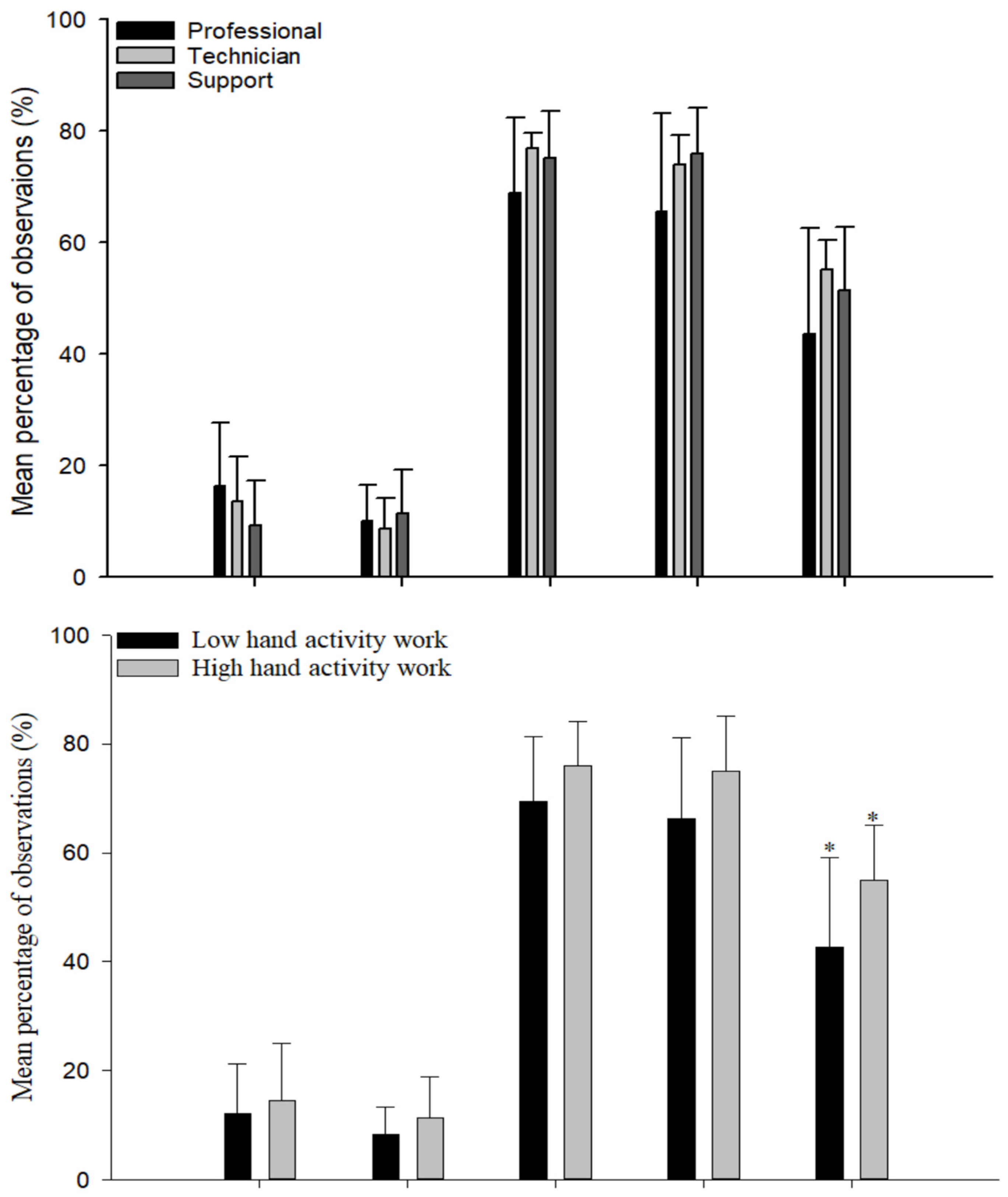
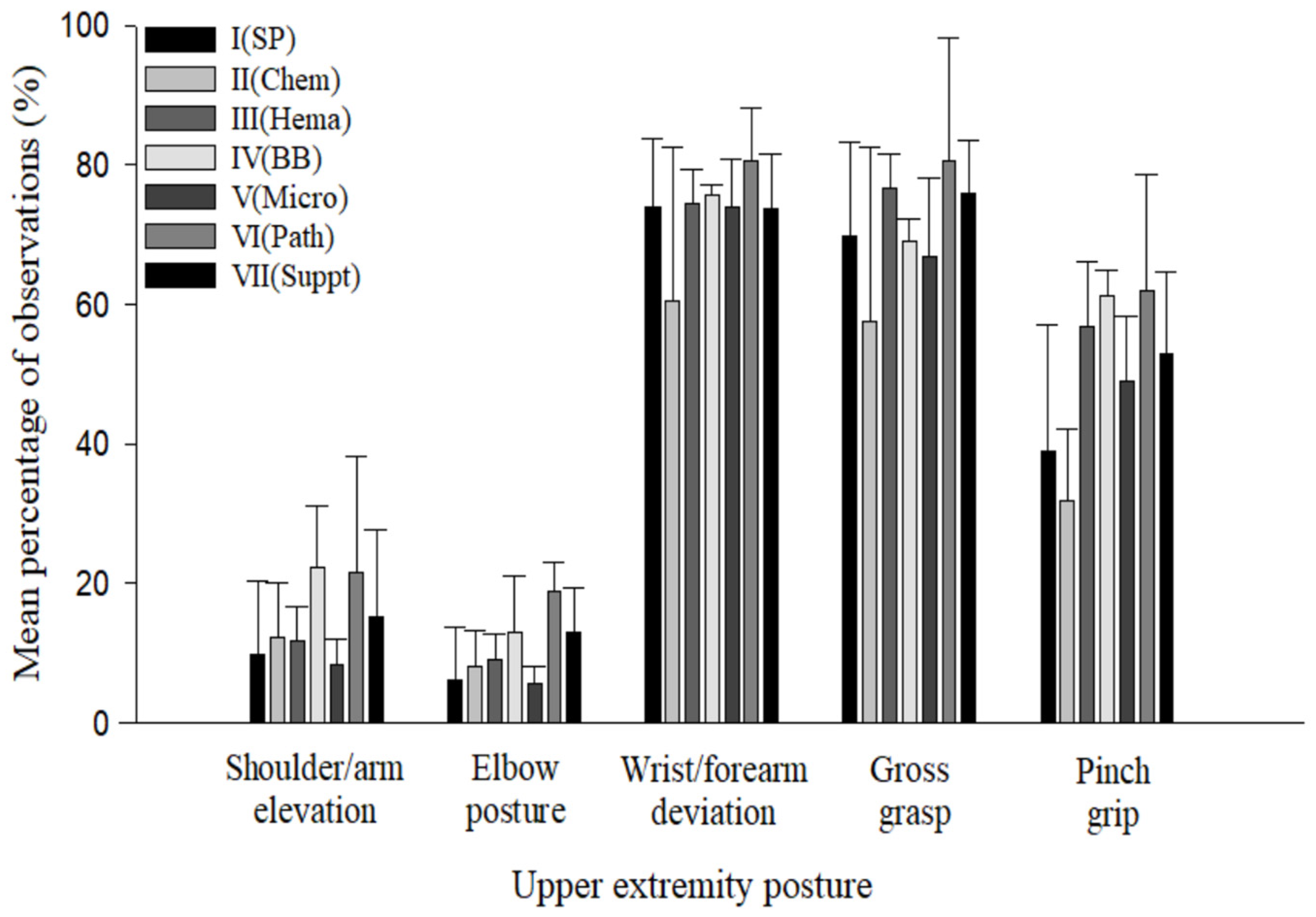
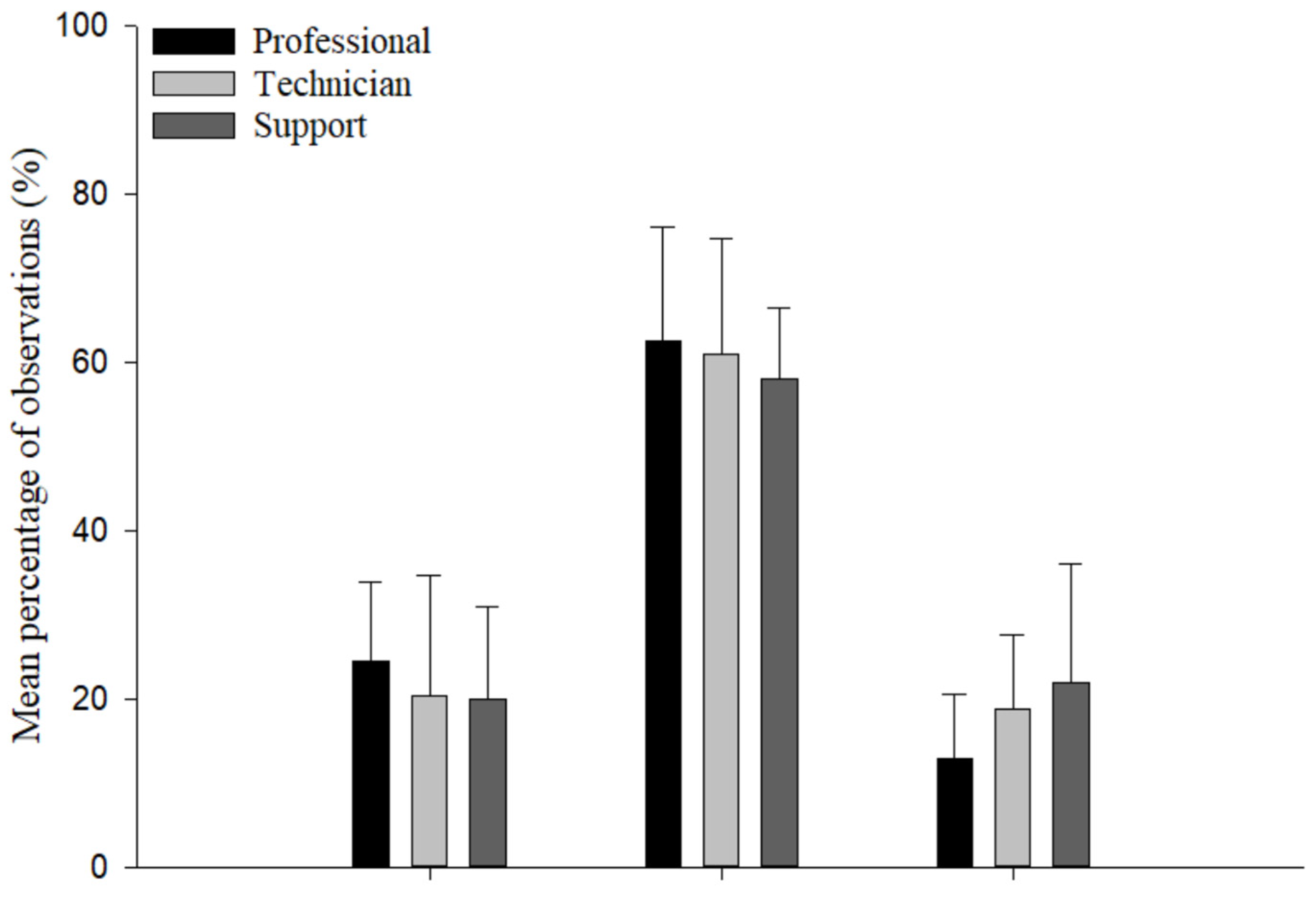
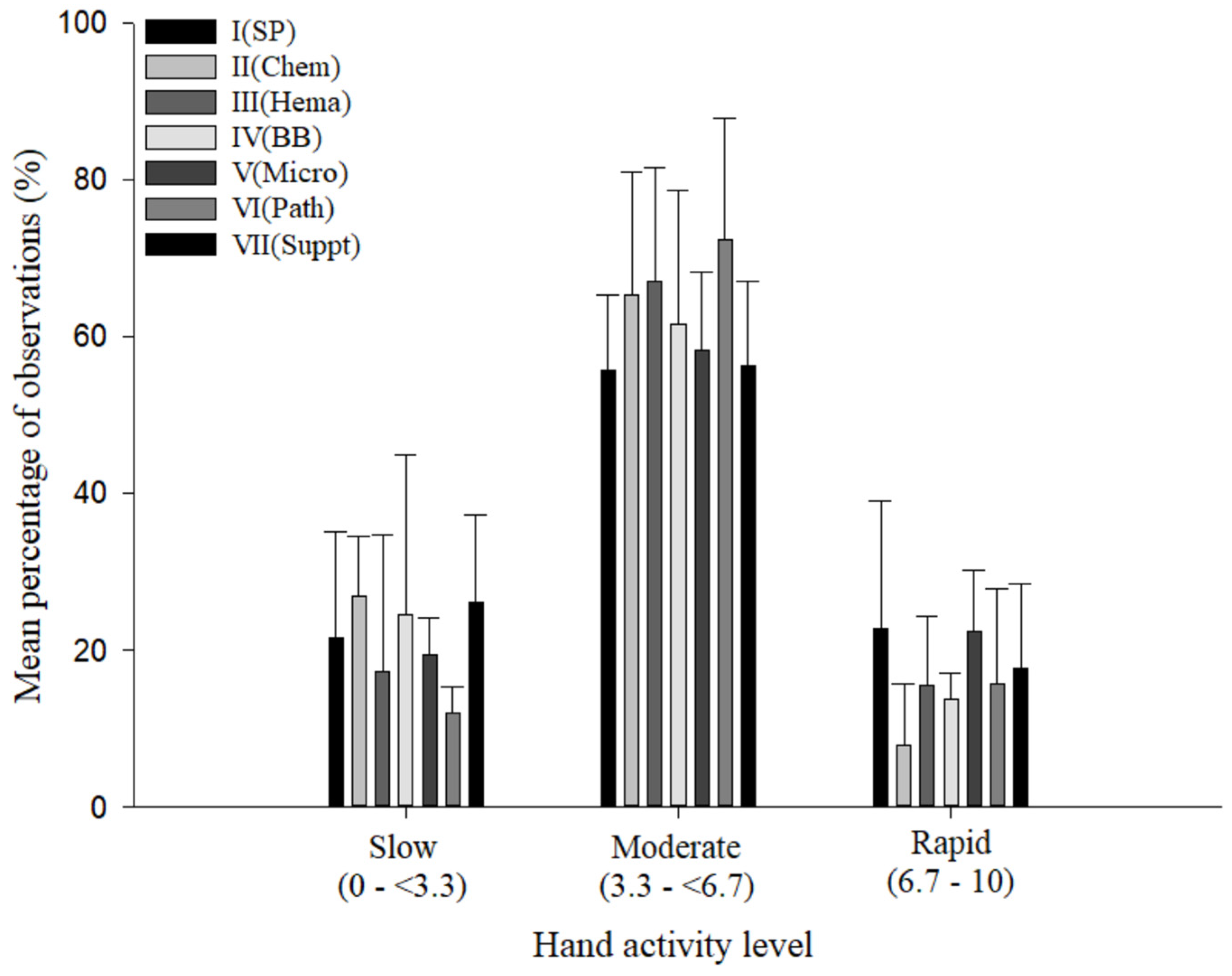
3.2. Comparison of Measures by Exposure Variable
4. Discussion
4.1. Findings and Implications
4.2. Exposure Assessment and Methodological Issues
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Observation Period (Work Shift) | Subject * | Whole Body Template | Hand/Forearm Template | Hand Activity Template | Obs. Duration, min | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Obs. No. | Shoulder/Arm Elevation, % | Elbow Posture, % | Obs. No. | Wrist/ Forearm Deviation, % | Gross Grasp, % | Pinch Grip, % | Obs. No. | Slow, % | Moderate, % | Rapid, % | |||
| 1 | A | 63 | 12 | 7 | 80 | 73 | 55 | 35 | 80 | 22 | 61 | 17 | 165 |
| 2 | A | 115 | 7 | 8 | 137 | 64 | 61 | 50 | 137 | 17 | 68 | 15 | 380 |
| 3 | B | 62 | 35 | 15 | 58 | 78 | 78 | 50 | 58 | 38 | 41 | 21 | 122 |
| 4 | C | 44 | 33 | 22 | 45 | 86 | 93 | 74 | 45 | 10 | 83 | 7 | 120 |
| 5 | D | 38 | 19 | 11 | 39 | 84 | 86 | 38 | 39 | 19 | 81 | 0 | 111 |
| 6 | E | 150 | 24 | 17 | 155 | 72 | 60 | 52 | 155 | 18 | 55 | 27 | 375 |
| 7 | E | 115 | 14 | 12 | 114 | 58 | 44 | 38 | 114 | 28 | 65 | 7 | 260 |
| 8 | F | 52 | 4 | 2 | 50 | 40 | 42 | 20 | 50 | 34 | 50 | 16 | 157 |
| 9 | F | 69 | 6 | 1 | 65 | 62 | 57 | 12 | 65 | 22 | 69 | 9 | 215 |
| 10 | G | 131 | 8 | 5 | 125 | 72 | 80 | 67 | 125 | 37 | 52 | 11 | 316 |
| 11 | H | 150 | 16 | 7 | 143 | 75 | 71 | 59 | 143 | 39 | 49 | 12 | 335 |
| 12 | H | 70 | 29 | 19 | 69 | 77 | 67 | 64 | 69 | 10 | 74 | 16 | 181 |
| 13 | I | 137 | 11 | 2 | 129 | 78 | 81 | 55 | 129 | 24 | 45 | 31 | 354 |
| 14 | I | 138 | 4 | 5 | 139 | 80 | 71 | 56 | 139 | 14 | 60 | 26 | 335 |
| 15 | J | 40 | 18 | 13 | 44 | 80 | 71 | 55 | 44 | 10 | 80 | 10 | 122 |
| 16 | K | 139 | 9 | 6 | 129 | 77 | 78 | 49 | 129 | 40 | 49 | 11 | 302 |
| 17 | L | 44 | 9 | 9 | 44 | 72 | 79 | 49 | 44 | 5 | 69 | 26 | 105 |
| 18 | M | 76 | 9 | 5 | 79 | 58 | 73 | 70 | 79 | 16 | 59 | 25 | 154 |
| 19 | N | 89 | 0 | 0 | 97 | 85 | 84 | 43 | 97 | 7 | 49 | 44 | 255 |
| 20 | O | 65 | 10 | 16 | 73 | 75 | 68 | 50 | 73 | 14 | 62 | 24 | 200 |
| 21 | P | 124 | 26 | 10 | 120 | 77 | 71 | 60 | 120 | 42 | 53 | 5 | 375 |
| 22 | Q | 113 | 9 | 17 | 111 | 76 | 66 | 35 | 111 | 23 | 58 | 19 | 259 |
| 23 | R | 63 | 3 | 8 | 65 | 74 | 87 | 48 | 65 | 21 | 74 | 5 | 153 |
| 24 | R | 78 | 8 | 23 | 76 | 80 | 81 | 55 | 76 | 16 | 52 | 32 | 190 |
| Mean | - | - | 13 | 10 | - | 73 | 71 | 49 | - | 22 | 61 | 17 | - |
| Total | - | 2165 | - | - | 2186 | - | - | - | 2186 | - | - | - | - |
References
- Agrawal, P.R.; Maiya, A.G.; Kamath, V.; Kamath, A. Work related musculoskeletal disorders among medical laboratory professionals: A narrative review. Int. J. Res. Med. Sci. 2014, 2, 1262–1266. [Google Scholar] [CrossRef][Green Version]
- Maulik, S.; Iqbal, R.; De, A.; Chandra, A.M. Evaluation of the working posture and prevalence of musculoskeletal symptoms among medical laboratory technicians. J. Back. Musculoskelet. Rehabil. 2014, 27, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Holm, J.W.; Mortensen, O.S.; Gyntelberg, F. Upper limb disorders among biomedical laboratory workers using pipettes. Cogent Med. 2016, 3, 1256849. [Google Scholar] [CrossRef]
- El-Helaly, M.; Balkhy, H.H.; Vallenius, L. Carpal tunnel syndrome among laboratory technicians in relation to personal and ergonomic factors at work. J. Occup. Health 2017, 59, 513–520. [Google Scholar] [CrossRef] [PubMed]
- US Bureau of Labor Statistics (US BLS). Rate and Number of Cases of Disorders Associated with Repeated Trauma by Industry in 2001. Available online: https://www.bls.gov/iif/oshwc/osh/os/ostb1128.pdf (accessed on 12 November 2021).
- Lopez-Gonzalez, M.J.; Gonzalez, S.; Gonzalez-Menendez, E. Prevalence of musculoskeletal problems in laboratory technicians. Int. J. Occup. Saf. Ergon. 2021, 27, 840–851. [Google Scholar] [CrossRef]
- Sadeghian, F.; Kasaeian, A.; Noroozi, P.; Taiebi, J.V.S.H. Psychosocial and individual characteristics and musculoskeletal complaints among clinical laboratory workers. Int. J. Occup. Saf. Ergon. 2014, 20, 355–361. [Google Scholar] [CrossRef]
- Fritzsche, F.R.; Ramach, C.; Soldini, D.; Caduff, R.; Tinguely, M.; Cassoly, E.; Moch, H.; Stewart, A. Occupational health risks of pathologists—Results from a nationwide online questionnaire in Switzerland. BMC Public Health 2012, 12, 1054. [Google Scholar] [CrossRef]
- Tak, S.; Buchholz, B.; Punnett, L.; Moir, S.; Paquet, V.; Fulmer, S.; Marucci-Wellman, H.; Wegman, D. Physical ergonomic hazards in highway tunnel construction: Overview from the Construction Occupational Health Program. Appl. Ergon. 2011, 42, 665–671. [Google Scholar] [CrossRef]
- Buchholz, B.; Paquet, V.; Punnett, L.; Lee, D.; Moir, S. PATH: A work sampling-based approach to ergonomic job analysis for construction and other non-repetitive work. Appl. Ergon. 1996, 27, 177–187. [Google Scholar] [CrossRef]
- Dasgupta, P.S.; Fulmer, S.; Jing, X.; Buchholz, B. Assessing the ergonomic hazards for pile drivers. Work 2012, 43, 417–425. [Google Scholar] [CrossRef]
- Dasgupta, P.S.; Punnett, L.; Moir, S.; Khun, S.; Buhholz, B. Does drywall installers’ innovative idea reduce the ergonomic exposures of ceiling installation: A field case study. Appl. Ergon. 2016, 55, 183–193. [Google Scholar] [CrossRef]
- Beheshti, M.H.; Javan, Z.; Yarahmadi, G. Ergonomic Evaluation of Musculoskeletal Disorders in Construction Workers Using Posture, Activity, Tools, Handling (PATH) Method. Int. J. Occup. Hyg. 2016, 8, 110–115. Available online: http://ijoh.tums.ac.ir/index.php/ijoh/issue/view/26 (accessed on 12 November 2021).
- Howard, N.L. The Development of Exposure Assessment Models for Ergonomic Stressors to the Hip and Knee in Dairy Farming. Master’s Thesis, Department of Work Environment, University of Massachusetts Lowell, Lowell, MA, USA, 1997. [Google Scholar]
- Pan, C.S.; Gardner, L.I.; Landsittel, P.; Hendricks, S.A.; Chiou, S.S.; Punnett, L. Ergonomic exposure assessment: An application of the PATH systematic observation method to retail workers. Int. J. Occup. Environ. Health 1999, 5, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Fulmer, S.; Punnett, L.; Slingerland, D.T.; Earle-Richardson, G. Ergonomic exposures in apple harvesting: Preliminary observations. Am. J. Ind. Med. 2002, 42 (Suppl. 2), 3–9. [Google Scholar] [CrossRef] [PubMed]
- Park, J.K.; Boyer, J.; Tessler, J.; Casey, J.; Schemm, L.; Gore, R.; Punnett, L.; Healthy, P. Inter-rater reliability of PATH observations for assessment of ergonomic risk factors in hospital work. Ergonomics 2009, 52, 820–829. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-K.; Han, Y.-S. Exposure assessment of musculoskeletal disorder risk factors in non-routinized work: An application of PATH-KOSHA tool to hospital workers. J. Korean Soc. Occup. Environ. Hyg. 2009, 19, 410–420. (In Korean) [Google Scholar]
- Kurowski, A.; Boyer, J.; Fulmer, S.; Gore, R.; Punnett, L. Changes in ergonomic exposures of nursing assistants after the introduction of a safe resident handling program in nursing homes. Int. J. Ind. Ergon. 2012, 42, 525–532. [Google Scholar] [CrossRef]
- Kurowski, A.; Buchholz, B.; ProCare Research Team; Punnett, L. A physical workload index to evaluate a safe resident handling program for nursing home personnel. Hum. Factors 2014, 56, 669–683. [Google Scholar] [CrossRef]
- Kim, D.-S.; Park, J.-K.; Han, Y.-S. Exposure assessment of musculoskeletal disorder risk factors in non-routinized work: An application of PATH-KOSHA tool to hotel workers. Hanyang Med. Rev. 2009, 28, 83–89. (In Korean) [Google Scholar]
- Kucera, K.L.; Lipscomb, H.J. Assessment of physical risk factors for the shoulder using the posture, activity, tools, and handling (PATH) method in small-scale commercial crab pot fishing. J. Agromed. 2010, 15, 394–404. [Google Scholar] [CrossRef]
- Paquet, V.; Punnett, L.; Buchholz, B. An evaluation of manual materials handling in highway construction work. Int. J. Ind. Ergon. 1999, 24, 431–444. [Google Scholar] [CrossRef]
- Moir, S.; Paquet, V.; Punnett, L.; Buchholz, B.; Wegman, D. Making sense of highway construction: A taxonomic framework for ergonomic exposure assessment and intervention research. Appl. Occup. Environ. Hyg. 2003, 18, 256–267. [Google Scholar] [CrossRef]
- Park, J.-K. Features of work and posture analysis outputs in general hospital nurses. J. Korean Soc. Occup. Environ. Hyg. 2019, 29, 375–382. (In Korean) [Google Scholar] [CrossRef]
- Gold, J.E.; Park, J.-S.; Punnett, L. Work routinization and implications for ergonomic exposure assessment. Ergonomics 2006, 49, 12–27. [Google Scholar] [CrossRef]
- d’Errico, A.; Punnett, L.; Cifuentes, M.; Boyer, J.; Tessler, J.; Gore, R.; Scollin, P.; Slatin, C. Hospital injury rates in relation to socioeconomic status and working conditions. Occup. Environ. Med. 2007, 4, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Cifuentes, M.; Boyer, J.; Gore, R.; d’Errico, A.; Tessler, J.; Scollin, P.; Lerner, D.; Kriebel, D.; Punnett, L.; Slatin, C. Inter-method agreement between O*NET and survey measures of psychosocial exposure among healthcare industry employees. Am. J. Ind. Med. 2007, 50, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Cifuentes, M.; Boyer, J.; Gore, R.; d’Errico, A.; Scollin, P.; Tessler, J.; Lerner, D.; Kriebel, D.; Punnett, L.; Slatin, C. Job strain predicts survey response in healthcare industry workers. Am. J. Ind. Med. 2008, 51, 281–289. [Google Scholar] [CrossRef]
- Boyer, J.; Galizzi, M.; Cifuentes, M.; d’Errico, A.; Gore, R.; Punnett, L.; Slatin, C. Ergonomic and socioeconomic risk factors for hospital workers’ compensation injury claims. Am. J. Ind. Med. 2009, 52, 551–562. [Google Scholar] [CrossRef] [PubMed]
- US Bureau of Labor Statistics (US BLS). 2018 Standard Occupational Classification (SOC) System. Available online: https://www.bls.gov/soc/2018/major_groups.htm (accessed on 14 November 2021).
- US Census Bureau (US CB). Equal Employment Opportunity (EEO) Tabulation Guidance for Data Users, EEO 2014–2018 Occupation Crosswalk to Other Occupation Groups. Available online: https://www.census.gov/topics/employment/equal-employment-opportunity-tabulation/guidance/2014-2018-eeo.html (accessed on 14 November 2021).
- Latko, W.A.; Armstrong, T.J.; Foulke, J.A.; Herrin, J.D.; Rabourn, R.A.; Ulin, S.S. Development and evaluation of an observational method for assessing repetition in hand tasks. Am. Ind. Hyg. Assoc. J. 1997, 8, 278–285. [Google Scholar] [CrossRef]
- Latko, W.A.; Armstrong, T.J.; Franzblau, A.; Ulin, S.S.; Werner, R.A.; Albers, J.W. Cross-sectional study of the relationship between repetitive work and the prevalence of upper limb musculoskeletal disorders. Am. J. Ind. Med. 1999, 6, 248–259. [Google Scholar] [CrossRef]
- Haslegrave, C.M.; Corlett, E.N. Evaluating work conditions and risk of injury-techniques for field surveys. In Evaluation of Human Work: A Practical Ergonomics Methodology, 2nd ed.; Wilson, J.R., Corlett, E.N., Eds.; Taylor and Francis: London, UK, 1990; pp. 892–920. [Google Scholar]
- Mathiassen, S.E.; Jackson, J.A.; Punnett, L. Statistical performance of observational work sampling for assessment of categorical exposure variables: A simulation approach illustrated using PATH data. Ann. Occup. Hyg. 2014, 58, 294–316. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Laboratory Type | Operation | Description | Example Work Element |
|---|---|---|---|
| Specimen processing | Pre-sample processing | Specimens are received from different places including departments of a facility, local clinics (laboratories), and residents. Specimens are registered (each accession number is assigned). | Sample manual handling (reception; capping and decapping of specimen tubes); VDU (keyboarding for registration); opening specimen bullets (a delivery box); labeling/writing; phone. |
| Sample processing | Samples are preliminarily prepared using instruments (e.g., centrifuge or stirrer) or tools (e.g., pipette) before delivery. Minor testing is performed. | Sample manual handling (capping and decapping of specimen tubes); pipetting; VDU (result recording; test report); instrument use or operation; labeling/writing; phone. | |
| Post-sample processing | Specimens are delivered to lab sections, using VDU to track specimens and make sure they have been properly handled. | VDU (tracking, result report); sample manual handling (delivery to lab sections); phone. | |
| Laboratory chemistry | Automated chemistry | Placing specimens on the appropriate instrument according to the tests ordered. | Pipetting; instrument operating (sample analysis, result report); phone |
| Manual chemistry | Like osmometry and acetone testing, specimens are tested manually. Blood and gas samples are analyzed. | Sample manual handling (sample preparation); pipetting; labeling/writing; phone. | |
| Hematology | Automated hematology | Placing test tubes on the appropriate instrument for analysis. | Instrument operating (sample analysis, result report); sample manual handling (sample preparation); pipetting; phone. |
| Manual hematology | CBC (complete blood count), differentials, and urine microscopy are performed. Dipstick urines are performed on a CLINITEK. | Sample manual handling (sample preparation); pipetting; microscopy (making test slides; microscope use); VDU (result report); Instrument operating (centrifuging; sample test), labeling/writing; phone. | |
| Blood bank | Blood testing (type, cross match, HIV) | Blood type (ABO/RH) and cross-match are tested. HIV testing is conducted on semi-automated equipment. | Sample manual handling (sample preparation); pipetting; Instrument operating; VDU (record results, result report); labeling/writing; phone |
| Blood bank database review | Record or review blood information in blood bank database (paperwork and statistics) | VDU (record or review database; check stock status). | |
| Microbiology | Automated microbiology | Tests performed on instrumentation; some biochemical tests on bacteria. | Sample manual handling (sample preparation); instrument operating; pipetting; VDU (result review and report); phone. |
| Manual microbiology | Agar plates are inoculated with various specimens and examined for the presence of bacteria; gram stains, ova, and parasite examinations are performed. Other work (immunology/serology) may exist. | Sample manual handling (inoculating culture plates; storage; opening and closing plates; reading plates); pipetting; microscopy (microscope use); labeling and writing; VDU (result review and report); phone. | |
| Pathology (histology, cytology) | Automated sample preparation | Tissue samples are prepared as ordered for analysis by fixation or staining. | Sample manual handling (sample preparation; fixation; staining); instrument operating; VDU (result review and report); phone. |
| Manual sample preparation | Sample preparation includes cutting and cover mounting. During preliminary examination, samples are handled on a microscope (gross examination may be conducted). | Sample manual handling (cutting tissues; cover mounting); microscopy (pre-examination); instrument operating; VDU (result review and report); labeling and writing; phone. | |
| Administration and laboratory support services | Staffing | Workforce is managed for shifts and rotation work; supervision. | VDU (data review and report); phone. |
| Planning and budgeting | Planning and budgeting for lab department; coordinating with other departments. | VDU (data review and report); phone. | |
| Phlebotomy | Blood is sampled from outpatients and inpatients by phlebotomists. Information of patients is recorded and reviewed in the databases. | Specimen sampling (e.g., drawing blood); sample handling (blood rocker); VDU (record or review patient information); phone. | |
| Specimen transport | Samples are delivered to the specimen processing section (manually or mechanically). | Carrying delivery box; lifting and lowering; preparing and loading specimens to the pneumatic transport system (“the bullet”). | |
| Material stock | Supply and storage of lab materials; inventory and ordering. | Push-pull carts; carrying lab materials; VDU (data review, material order, and report); phone. | |
| Data processing | Information on phlebotomy work or specimen transport will be entered at PCs. | Document and record review; VDU work; phone |
| Laboratory Type | Operation | %Time: Mean ± Standard Deviation ** | Number of Observation Period (Work Shift) | |
|---|---|---|---|---|
| Name | Notation * | |||
| Specimen processing | Pre-sample processing | M | 47 ± 32 | 4 |
| Sample processing | SA | 33 ± 31 | ||
| Post-sample processing | M | 10 ± 4 | ||
| Others | M | 10 ± 7 | ||
| Laboratory chemistry | Automated chemistry | A | 85 ± 13 | 3 |
| Manual chemistry | M | - | ||
| Others | M | 15 ± 13 | ||
| Hematology | Automated hematology | A | 52 ± 48 | 3 |
| Manual hematology | M | 40 ± 40 | ||
| Others | M | 8 ± 10 | ||
| Blood bank | Blood testing (type, cross match, or HIV) | SA | 94 ± 6 | 2 |
| Blood bank database review | M | - | ||
| Others | M | 6 ± 6 | ||
| Microbiology | Automated microbiology | A | - | 4 |
| Manual microbiology | M | 93 ± 12 | ||
| Others | M | 7 ± 2 | ||
| Pathology (histology or cytology) | Automated tissue preparation | A | - | 2 |
| Manual sample preparation | M | 95 ± 0 | ||
| Others | M | 5 ± 0 | ||
| Administration and laboratory support services | Staffing | M | 5 ± 12 | 6 |
| Planning and budgeting | M | 9 ± 22 | ||
| Phlebotomy | M | 25 ± 39 | ||
| Specimen transport | SA | 2 ± 4 | ||
| Material management and stock | M | 16 ± 41 | ||
| Data processing | M | 35 ± 47 | ||
| Others | M | 8 ± 8 | ||
| Total | 24 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-K.; Boyer, J.; Punnett, L. Biomechanical Exposure to Upper Extremity Musculoskeletal Disorder Risk Factors in Hospital Laboratories. Int. J. Environ. Res. Public Health 2022, 19, 499. https://doi.org/10.3390/ijerph19010499
Park J-K, Boyer J, Punnett L. Biomechanical Exposure to Upper Extremity Musculoskeletal Disorder Risk Factors in Hospital Laboratories. International Journal of Environmental Research and Public Health. 2022; 19(1):499. https://doi.org/10.3390/ijerph19010499
Chicago/Turabian StylePark, Jung-Keun, Jon Boyer, and Laura Punnett. 2022. "Biomechanical Exposure to Upper Extremity Musculoskeletal Disorder Risk Factors in Hospital Laboratories" International Journal of Environmental Research and Public Health 19, no. 1: 499. https://doi.org/10.3390/ijerph19010499
APA StylePark, J.-K., Boyer, J., & Punnett, L. (2022). Biomechanical Exposure to Upper Extremity Musculoskeletal Disorder Risk Factors in Hospital Laboratories. International Journal of Environmental Research and Public Health, 19(1), 499. https://doi.org/10.3390/ijerph19010499






