Investigating Key Factors Related to the Decision of a Do-Not-Resuscitate Consent
Abstract
:1. Introduction
2. Materials and Methods
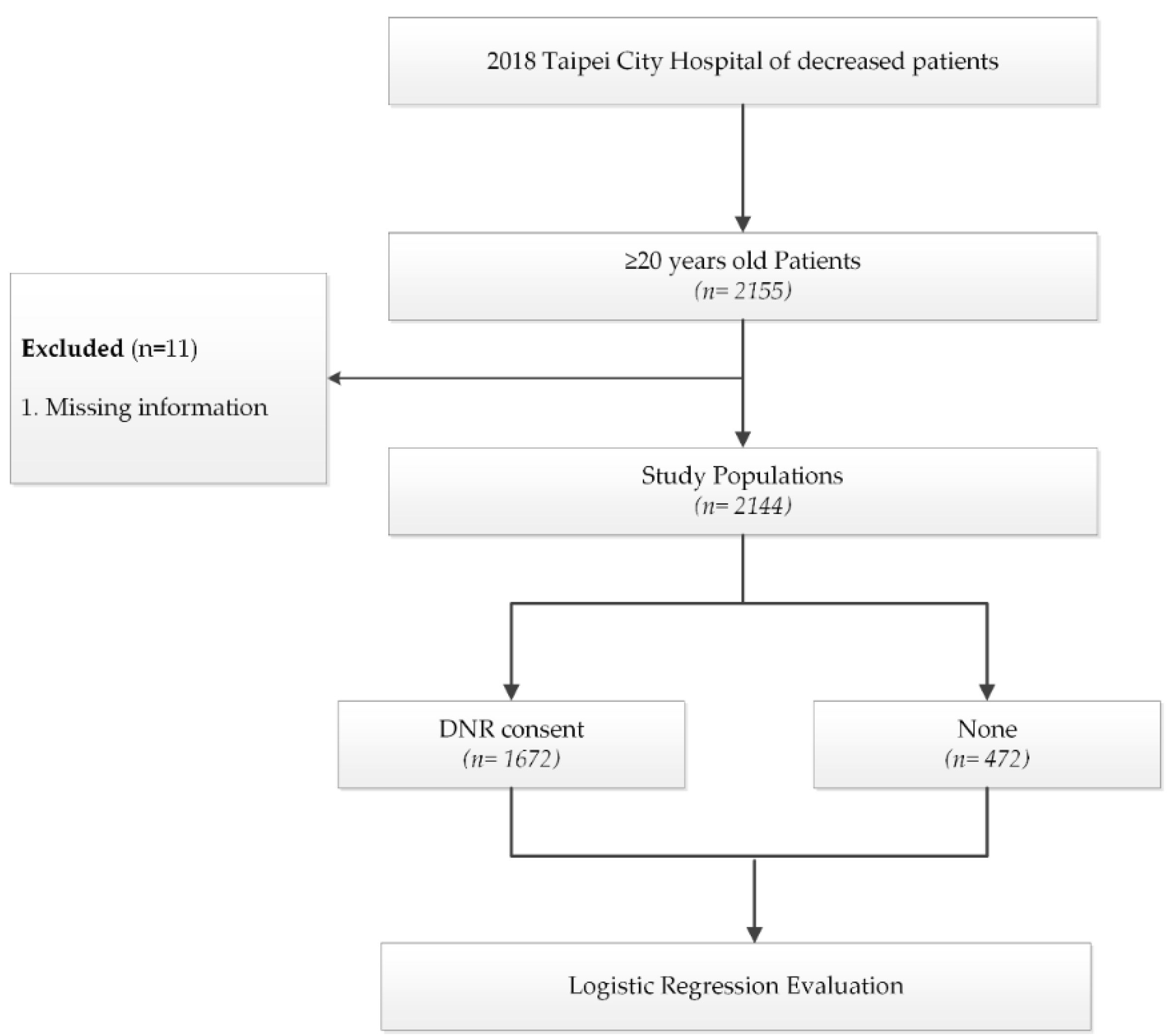
2.1. Study Design and Population
2.2. Baseline Variables
2.3. Statistical Analysis
3. Results
3.1. Study Population Characteristics
3.2. DNR Signature Situation
3.3. Factors Affecting DNR Status
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Quinn, K.; Workman, S. DNR: “Do Not Resuscitate” or “Death Not Reversible”? J. Palliat. Med. 2018, 21, 533–535. [Google Scholar] [CrossRef] [PubMed]
- Yuen, J.K.; Reid, M.C.; Fetters, M.D. Hospital do-not-resuscitate orders: Why they have failed and how to fix them. J. Gen Intern Med. 2011, 26, 791–797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, C.H.; Hu, W.Y.; Chiu, T.Y.; Chen, C.Y. The practicalities of terminally ill patients signing their own DNR orders--a study in Taiwan. J. Med. Ethics 2008, 34, 336–340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, M.T.; Shih, F.Y.; Tsai, C.L.; Tsai, H.B.; Tsai, D.F.; Fang, C.C. Impact of major illnesses and geographic regions on do-not-resuscitate rate and its potential cost savings in Taiwan. PLoS ONE 2019, 14, e0222320. [Google Scholar] [CrossRef] [PubMed]
- Al Ahmadi, J.R.; Aljehani, S.N.; Bahakeem, L.M.; Hijan, B.A.; Mayet, S.A.; Badahdah, Y.A. Knowledge and attitude toward do-not-resuscitate among patients and their relatives visiting outpatient clinics at King Abdulaziz University Hospital, Jeddah, Saudi Arabia. Saudi Med. J. 2020, 41, 53–58. [Google Scholar] [CrossRef]
- Hofmann, J.C.; Wenger, N.S.; Davis, R.B.; Teno, J.; Connors, A.F.; Desbiens, N.; Lynn, J.; Phillips, R.S. Patient preferences for communication with physicians about end-of-life decisions. Ann. Intern. Med. 1997, 127, 1–12. [Google Scholar] [CrossRef]
- Pettersson, M.; Hedström, M.; Höglund, A.T. The ethics of DNR-decisions in oncology and hematology care: A qualitative study. BMC Med Ethics 2020, 21, 1–9. [Google Scholar] [CrossRef]
- Robinson, C.; Kolesar, S.; Boyko, M.; Berkowitz, J.; Calam, B.; Collins, M. Awareness of do-not-resuscitate orders: What do patients know and want? Can. Fam. Physician 2012, 58, e229–e233. [Google Scholar]
- Fan, S.Y.; Hsieh, J.G. The Experience of Do-Not-Resuscitate Orders and End-of-Life Care Discussions among Physicians. Int. J. Environ. Res. Public Health 2020, 17, 6869. [Google Scholar] [CrossRef]
- Ho, Z.J.; Radha Krishna, L.K.; Yee, C.P. Chinese familial tradition and Western influence: A case study in Singapore on decision making at the end of life. J. Pain Symptom. Manag. 2010, 40, 932–937. [Google Scholar] [CrossRef] [PubMed]
- Pang, M.C. Protective truthfulness: The Chinese way of safeguarding patients in informed treatment decisions. J. Med. Ethics 1999, 25, 247–253. [Google Scholar] [CrossRef] [Green Version]
- Back, M.F.; Huak, C.Y. Family centred decision making and non-disclosure of diagnosis in a South East Asian oncology practice. Psychooncology 2005, 14, 1052–1059. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.M.; Kwee, A.K.; Krishna, L. Should Patients and Family be Involved in “Do Not Resuscitate” Decisions? Views of Oncology and Palliative Care Doctors and Nurses. Indian J. Palliat. Care 2012, 18, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Bordbar, M.R.F.; Tavakkoli, K.; Nahidi, M.; Bordbar, A.F. Investigating the attitude of healthcare providers, patients, and their families toward “do not resuscitate” orders in an Iranian Oncology Hospital. Indian J. Palliat. Care 2019, 25, 440. [Google Scholar]
- Chiang, C.-C.; Chang, S.-C.; Fan, S.-Y. The Concerns and Experience of Decision-Making Regarding Do-Not-Resuscitate Orders Among Caregivers in Hospice Palliative Care. Am. J. Hosp. Palliat. Med. 2020, 38, 1049909120933535. [Google Scholar] [CrossRef] [PubMed]
- Scopetti, M.; Santurro, A.; Gatto, V.; Padovano, M.; Manetti, F.; D’Errico, S.; Fineschi, V. Information, Sharing, and Self-Determination: Understanding the Current Challenges for the Improvement of Pediatric Care Pathways. Front. Pediatr. 2020, 8, 371. [Google Scholar] [CrossRef]
- Smith-Howell, E.R.; Hickman, S.E.; Meghani, S.H.; Perkins, S.M.; Rawl, S.M. End-of-life decision making and communication of bereaved family members of African Americans with serious illness. J. Palliat. Med. 2016, 19, 174–182. [Google Scholar] [CrossRef]
- Heyland, D.K.; Allan, D.E.; Rocker, G.; Dodek, P.; Pichora, D.; Gafni, A. Canadian Researchers at the End-of-Life Network (CARENET). Discussing prognosis with patients and their families near the end of life: Impact on satisfaction with end-of-life care. Open Med. 2009, 3, e101. [Google Scholar]
- Lai, Y.L.; Su, W.H. Palliative medicine and the hospice movement in Taiwan. Support. Care Cancer 1997, 5, 348–350. [Google Scholar] [CrossRef]
- Cheng, S.Y.; Dy, S.; Hu, W.Y.; Chen, C.Y.; Chiu, T.Y. Factors affecting the improvement of quality of dying of terminally ill patients with cancer through palliative care: A ten-year experience. J. Palliat. Med. 2012, 15, 854–862. [Google Scholar] [CrossRef]
- Wang, S.S.; Huang, C.M.; Feng, R.C.; Wu, Y.L.; Huang, S.J. Validation of a concise screening tool for the identification of palliative care needs among inpatients: A prospective study in hospital setting. J. Formos. Med. Assoc. 2019, 118, 883–890. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-T.; Hsiao, F.-H. The effects of the interventions on the DNR designation among cancer patients: A systematic review. Palliat. Support. Care 2019, 17, 95–106. [Google Scholar] [CrossRef]
- Pettersson, M.; Höglund, A.T.; Hedström, M. Perspectives on the DNR decision process: A survey of nurses and physicians in hematology and oncology. PLoS ONE 2018, 13, e0206550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bedell, S.E.; Pelle, D.; Maher, P.L.; Cleary, P.D. Do-Not-Resuscitate Orders for Critically III Patients in the Hospital: How Are They Used and What Is Their Impact? Jama 1986, 256, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Levinson, M.; Mills, A. Cardiopulmonary resuscitation-time for a change in the paradigm? Med. J. Aust. 2014, 201, 152–154. [Google Scholar] [CrossRef] [PubMed]
- Sadler, K.; Abudari, G.; Aljawi, D.; Snelling, D. Deaths in the emergency department: An assessment of patient’s end-of-life trajectory and quality of care. Indian J. Palliat. Care 2020, 26, 352. [Google Scholar] [CrossRef]
- Kaneetah, A.H.; Baowaidan, F.O.; Abulaban, B.A.; Sabban, M.F.; Alshehri, A.S. The perspectives of the general population and relatives of Cancer patients with respect to the do-not-resuscitate order. Cureus 2019, 11, e3968. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rafiq, A.; Ullah, W.; Naglak, M.; Schneider, D. Characteristics and Outcomes of Patients with Partial Do Not Resuscitate Orders in a Large Community Hospital. Cureus 2019, 11, e6048. [Google Scholar] [CrossRef] [Green Version]
- Jesus, J.E.; Allen, M.B.; Michael, G.E.; Donnino, M.W.; Grossman, S.A.; Hale, C.P.; Breu, A.C.; Bracey, A.; O’Connor, J.L.; Fisher, J. Preferences for resuscitation and intubation among patients with do-not-resuscitate/do-not-intubate orders. Mayo Clin. Proc. 2013, 88, 658–665. [Google Scholar] [CrossRef]
- Tajari, M.; Jalali, R.; Vafaee, K. Attitudes of patients’ relatives in the end stage of life about do not resuscitate order. J. Fam. Med. Prim. Care 2018, 7, 916–920. [Google Scholar]
- Al Sheef, M.A.; Al Sharqi, M.S.; Al Sharief, L.H.; Takrouni, T.Y.; Mian, A.M. Awareness of do-not-resuscitate orders in the outpatient setting in Saudi Arabia: Perception and implications. Saudi Med. J. 2017, 38, 297. [Google Scholar] [CrossRef] [PubMed]
- Bjorklund, P.; Lund, D.M. Informed consent and the aftermath of cardiopulmonary resuscitation: Ethical considerations. Nurs. Ethics 2019, 26, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Amoudi, A.S.; Albar, M.H.; Bokhari, A.M.; Yahya, S.H.; Merdad, A.A. Perspectives of interns and residents toward do-not-resuscitate policies in Saudi Arabia. Adv. Med. Educ. Pract. 2016, 7, 165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Baseline | N% | (%) | |
|---|---|---|---|
| Sex | Male | 1240 | 57.84 |
| Female | 904 | 42.16 | |
| Age group | <65 | 285 | 13.29 |
| 65–79 | 578 | 26.96 | |
| ≥80 | 1281 | 59.79 | |
| Type of ward | General | 1142 | 53.26 |
| Respiratory care | 18 | 0.84 | |
| Intensive care | 667 | 31.11 | |
| Palliative | 317 | 14.79 | |
| Diagnosis | Cancer | 466 | 21.74 |
| Non-cancer | 1678 | 78.26 | |
| Family palliative care consultation | Yes | 1551 | 72.34 |
| No | 593 | 27.66 | |
| TW–PCST scores | 0–3 | 886 | 41.32 |
| ≥4 | 880 | 37.31 | |
| Unknow TW–PCST | 458 | 21.36 | |
| LOS (days) | 1–10 | 1009 | 47.06 |
| 11–20 | 453 | 21.13 | |
| 21–30 | 276 | 12.87 | |
| >30 | 406 | 18.94 | |
| Baseline | DNR Consent | None | p | |||
|---|---|---|---|---|---|---|
| (n = 1730) | (n = 414) | |||||
| n | % | n | % | |||
| Sex | Male | 989 | 57.17 | 251 | 60.63 | 0.2003 |
| Female | 741 | 42.83 | 163 | 39.37 | ||
| Age group | <65 | 227 | 13.12 | 58 | 14.01 | 0.8886 |
| 65–79 | 468 | 27.05 | 110 | 26.57 | ||
| ≥80 | 1035 | 59.83 | 246 | 59.42 | ||
| Age mean (std) | 80.37 (13.41) | 80.25 (13.86) | 0.8643 | |||
| Type of ward | General | 871 | 52.09 | 271 | 57.42 | 0.1630 |
| Respiratory care | 12 | 0.72 | 6 | 1.270 | ||
| Intensive care | 530 | 31.7 | 137 | 29.03 | ||
| Palliative | 317 | 100 | - | - | ||
| Diagnosis | Cancer | 381 | 22.02 | 85 | 20.53 | 0.5086 |
| Non-cancer | 1349 | 77.98 | 239 | 79.47 | ||
| Family palliative care consultation | Yes | 1298 | 75.03 | 253 | 61.11 | <0.001 |
| No | 432 | 24.97 | 161 | 38.89 | ||
| TW–PCST scores | 0–3 | 682 | 39.42 | 204 | 49.28 | <0.001 |
| 4+ | 645 | 37.28 | 155 | 37.44 | ||
| Unknown TW–PCST | 403 | 23.29 | 55 | 13.29 | ||
| Length of Stay mean (std) | 22.99 (52.53) | 41.36 (124.90) | 0.0035 | |||
| Baseline | Estimate | Error | Pr (>Chi) |
|---|---|---|---|
| Intercept | 0.7275 | 0.4060 | |
| Sex | −0.1979 | 0.1284 | 0.1900 |
| Age | 0.0019 | 0.0046 | 0.6625 |
| Type of ward | 0.4100 | 0.0577 | <0.001 *** |
| Family palliative care consultation | 0.8236 | 0.1331 | <0.001 *** |
| Diagnosis | 0.1665 | 0.1562 | 0.2820 |
| TW–PCST scores | −0.2253 | 0.0869 | 0.0086 ** |
| LOS (days) | −0.0023 | 0.0007 | 0.0010 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, H.-M.; Liu, C.-K.; Huang, Y.-C.; Ho, C.-W.; Chen, M. Investigating Key Factors Related to the Decision of a Do-Not-Resuscitate Consent. Int. J. Environ. Res. Public Health 2022, 19, 428. https://doi.org/10.3390/ijerph19010428
Lin H-M, Liu C-K, Huang Y-C, Ho C-W, Chen M. Investigating Key Factors Related to the Decision of a Do-Not-Resuscitate Consent. International Journal of Environmental Research and Public Health. 2022; 19(1):428. https://doi.org/10.3390/ijerph19010428
Chicago/Turabian StyleLin, Hui-Mei, Chih-Kuang Liu, Yen-Chun Huang, Chieh-Wen Ho, and Mingchih Chen. 2022. "Investigating Key Factors Related to the Decision of a Do-Not-Resuscitate Consent" International Journal of Environmental Research and Public Health 19, no. 1: 428. https://doi.org/10.3390/ijerph19010428
APA StyleLin, H.-M., Liu, C.-K., Huang, Y.-C., Ho, C.-W., & Chen, M. (2022). Investigating Key Factors Related to the Decision of a Do-Not-Resuscitate Consent. International Journal of Environmental Research and Public Health, 19(1), 428. https://doi.org/10.3390/ijerph19010428






