Impact of Health Literacy on the Progression of Frailty after 4 Years among Community-Dwelling Older Adults
Abstract
:1. Introduction
2. Materials and Methods
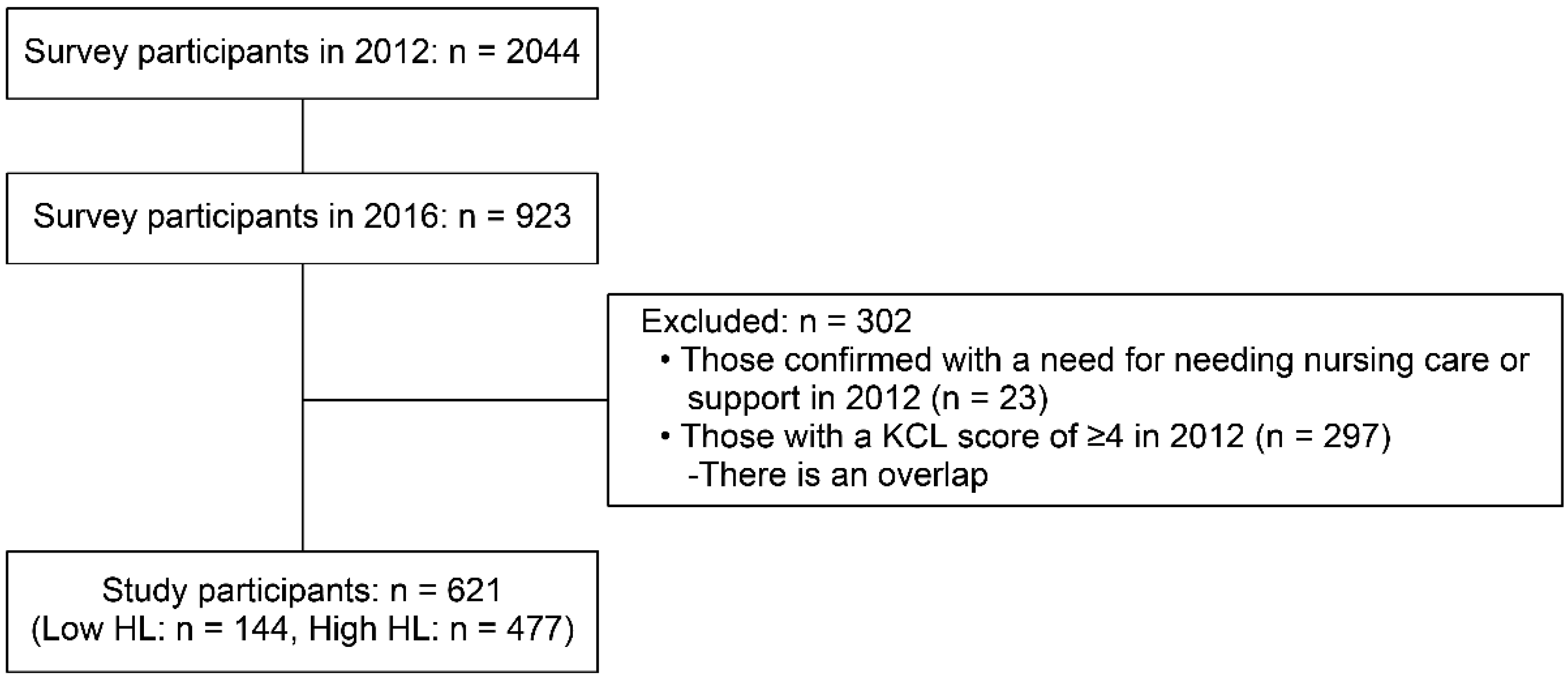
2.1. Research Design and Participants
2.2. Survey Content
2.2.1. Frailty Score
2.2.2. Health Literacy
2.2.3. Other Variables
2.3. Statistical Analysis
3. Results
3.1. Participant’s Baseline Characteristics
3.2. Group Comparison 1: Between the Frailty-Progressing Group and Robust Group in 2016
3.3. Group Comparison 2: Between ‘Low’ and ‘High HL’ Group
3.4. Evaluation of Factors Influencing the Progression of Frailty
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| No | Questions | Answer | ||
|---|---|---|---|---|
| 2012 | 2016 | |||
| 1 | Do you go out by bus or train by yourself? | NO | 15 (2.4%) | 18 (2.9%) |
| 2 | Do you go shopping to buy daily necessities by yourself? | NO | 9 (1.4%) | 15 (2.7%) |
| 3 | Do you manage your own deposits and savings at the bank? | NO | 20 (3.2%) | 67 (10.8%) |
| 4 | Do you sometimes visit your friends? | NO | 133 (21.4%) | 239 (38.5%) |
| 5 | Do you turn to your family or friends for advice? | NO | 20 (3.2%) | 81 (13.1%) |
| 6 | Do you normally climb stairs without using handrail or wall for support? | NO | 74 (11.9%) | 125 (20.2%) |
| 7 | Do you normally stand up from a chair without any aids | NO | 21 (3.4%) | 37 (6.0%) |
| 8 | Do you normally walk continuously for 15 min | NO | 12 (1.9%) | 56 (9.0%) |
| 9 | Have you experienced a fall in the past year | YES | 70 (11.3%) | 153 (24.6%) |
| 10 | Do you have a fear of falling while walking | YES | 101 (16.3%) | 128 (20.7%) |
| 11 | Have you lost 2 kg or more in the past 6 months | YES | 53 (8.5%) | 109 (17.6%) |
| 12 | Height: cm, weight: kg, BMI: kg/m2 (If BMI is less than 18.5, this item is scored.) | YES | 31 (5.0%) | 142 (22.8%) |
| 13 | Do you have any difficulties eating tough foods compared to 6 months ago? | YES | 48 (7.7%) | 87 (14.0%) |
| 14 | Have you choked on your tea or soup recently | YES | 76 (12.2%) | 99 (15.9%) |
| 15 | Do you often experience having a dry mouth | YES | 111 (17.9%) | 165 (26.6%) |
| 16 | Do you go out at least once a week | NO | 23 (3.7%) | 87 (14.0%) |
| 17 | Do you go out less frequently compared to last year | YES | 67 (10.8%) | 140 (22.5%) |
| 18 | Do your family or your friends point out your memory loss? | YES | 42 (6.8%) | 94 (15.2%) |
| e.g., “You ask the same question over and over again.” | ||||
| 19 | Do you make a call by looking up phone numbers | NO | 39 (6.3%) | 85 (13.7%) |
| 20 | Do you find yourself not knowing today’s date | YES | 99 (15.9%) | 100 (16.1%) |
| 21 | In the last 2 weeks have you felt a lack of fulfilment in your daily life? | YES | 36 (5.8%) | 42 (6.8%) |
| 22 | In the last 2 weeks have you felt a lack of joy when doing the things you used to enjoy? | YES | 8 (1.3%) | 23 (3.7%) |
| 23 | In the last 2 weeks have you felt difficulty in doing what you could do easily before? | YES | 32 (5.2%) | 74 (12.0%) |
| 24 | In the last 2 weeks have you felt helpless | YES | 29 (4.7%) | 39 (6.3%) |
| 25 | In the last 2 weeks have you felt tired without a reason | YES | 34 (5.5%) | 66 (10.7%) |
| BMI, body mass index; KCL, Kihon Checklist. | ||||
Appendix B
| No | Questions | Mean ± SD |
|---|---|---|
| 1 | Seeking information from various sources | 4.3 ± 0.7 |
| 2 | Extracting relevant information | 4.2 ± 0.7 |
| 3 | Considering the credibility of the information | 4.0 ± 0.6 |
| 4 | Understanding and communicating the information | 4.1 ± 0.6 |
| 5 | Making decisions based on the information | 4.1 ± 0.7 |
| HL, Health literacy; score range (1–5) |
References
- Cabinet Office, Government of Japan. White Paper on the Aging Society (Summary Version). Available online: https://www8.cao.go.jp/kourei/english/annualreport/2018/2018pdf_e.html (accessed on 30 October 2021).
- Ministry of Health, Labour and Welfare, Government of Japan. Report from the Expert Study Group on Healthy Life Expectancy. Available online: https://www.mhlw.go.jp/content/10904750/00049535323.pdf (accessed on 30 October 2021).
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Morley, J.E.; Vellas, B.; Van Kan, G.A.; Anker, S.D.; Bauer, J.M.; Bernabei, R.; Cesari, M.; Chumlea, W.; Doehner, W.; Evans, J.; et al. Frailty Consensus: A Call to Action. J. Am. Med. Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimada, H.; Makizako, H.; Doi, T.; Yoshida, D.; Tsutsumimoto, K.; Anan, Y.; Uemura, K.; Ito, T.; Lee, S.; Park, H.; et al. Combined Prevalence of Frailty and Mild Cognitive Impairment in a Population of Elderly Japanese People. J. Am. Med. Dir. Assoc. 2013, 14, 518–524. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H.; (HLS-EU) Consortium Health Literacy Project European. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suka, M.; Odajima, T.; Okamoto, M.; Sumitani, M.; Igarashi, A.; Ishikawa, H.; Kusama, M.; Yamamoto, M.; Nakayama, T.; Sugimori, H. Relationship between health literacy, health information access, health behavior, and health status in Japanese people. Patient Educ. Couns. 2015, 98, 660–668. [Google Scholar] [CrossRef]
- Ivanov, L.L.; Wallace, D.C.; Hernández, C.; Hyde, Y. Diabetes risks and health literacy in southern African American and Latino women. J. Community Health Nurs. 2015, 32, 12–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friis, K.; Vind, B.D.; Simmons, R.K.; Maindal, H.T. The Relationship between Health Literacy and Health Behaviour in People with Diabetes: A Danish Population-Based Study. J. Diabetes Res. 2016, 2016, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fabbri, M.; Yost, K.; Rutten, L.J.F.; Manemann, S.M.; Boyd, C.M.; Jensen, D.; Weston, S.A.; Jiang, R.; Roger, V.L. Health Literacy and Outcomes in Patients with Heart Failure: A Prospective Community Study. Mayo Clin. Proc. 2017, 93, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Aaby, A.; Friis, K.; Christensen, B.; Rowlands, G.; Maindal, H.T. Health literacy is associated with health behaviour and self-reported health: A large population-based study in individuals with cardiovascular disease. Eur. J. Prev. Cardiol. 2017, 24, 1880–1888. [Google Scholar] [CrossRef] [Green Version]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low Health Literacy and Health Outcomes: An Updated Systematic Review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Eronen, J.; Paakkari, L.; Portegijs, E.; Saajanaho, M.; Rantanen, T. Assessment of health literacy among older Finns. Aging Clin. Exp. Res. 2018, 31, 549–556. [Google Scholar] [CrossRef] [Green Version]
- Shirooka, H.; Nishiguchi, S.; Fukutani, N.; Adachi, D.; Tashiro, Y.; Hotta, T.; Morino, S.; Nozaki, Y.; Hirata, H.; Yamaguchi, M.; et al. Association between comprehensive health literacy and frailty level in community-dwelling older adults: A cross-sectional study in Japan. Geriatr. Gerontol. Int. 2016, 17, 804–809. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.H.; Lai, Y.-C.; Lee, Y.C.; Teong, X.T.; Kuzuya, M.; Kuo, K.-M. Impact of Health Literacy on Frailty among Community-Dwelling Seniors. J. Clin. Med. 2018, 7, 481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministry of Internal Affairs and Communications, Government of Japan. Report on the 2039 Survey on Trends in Telecommunications Usage. Available online: https://www.soumu.go.jp/main_content/000689455.pdf (accessed on 30 October 2021).
- Kashiwa City, Japanese Cities. Kashiwa City Profile. Available online: https://www.city.kashiwa.lg.jp/databunseki/shiseijoho/about_kashiwa/profile/chirijinko.html (accessed on 27 December 2021).
- Satake, S.; Senda, K.; Hong, Y.-J.; Miura, H.; Endo, H.; Sakurai, T.; Kondo, I.; Toba, K. Validity of the Kihon Checklist for assessing frailty status. Geriatr. Gerontol. Int. 2015, 16, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Nomura, K.; Sato, M.; Yano, E. Developing a measure of communicative and critical health literacy: A pilot study of Japanese office workers. Health Promot. Int. 2008, 23, 269–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batko-Szwaczka, A.; Dudzińska-Griszek, J.; Hornik, B.; Janusz-Jenczeń, M.; Włodarczyk, I.; Wnuk, B.; Szołtysek, J.; Durmała, J.; Wilczyński, K.; Cogiel, A.; et al. Frailty Phenotype: Evidence of Both Physical and Mental Health Components in Community-Dwelling Early-Old Adults. Clin. Interv. Aging 2020, 15, 141–150. [Google Scholar] [CrossRef] [Green Version]
- Gale, C.; Westbury, L.; Cooper, C. Social isolation and loneliness as risk factors for the progression of frailty: The English Longitudinal Study of Ageing. Age Ageing 2017, 47, 392–397. [Google Scholar] [CrossRef] [Green Version]
- Kamdem, B.; Seematter-Bagnoud, L.; Botrugno, F.; Santos-Eggimann, B. Relationship between oral health and Fried’s frailty criteria in community-dwelling older persons. BMC Geriatr. 2017, 17, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshiyuki, N.; Kono, A. Association between frailty in community-dwelling older adults certified as requiring support in the long-term care insurance system and social capital among local neighborhood volunteers. Jpn. J. Public Health 2020, 67, 111–120. [Google Scholar]
- Awata, S.; Bech, P.; Yoshida, S.; Hirai, M.; Suzuki, S.; Yamashita, M.; Ohara, A.; Hinokio, Y.; Matsuoka, H.; Oka, Y. Reliability and validity of the Japanese version of the World Health Organization-Five Well-Being Index in the context of detecting depression in diabetic patients. Psychiatry Clin. Neurosci. 2007, 61, 112–119. [Google Scholar] [CrossRef]
- Kurimoto, A.; Awata, S.; Ohkubo, T.; Tsubota-Utsugi, M.; Asayama, K.; Takahashi, K.; Suenaga, K.; Satoh, H.; Imai, Y. Reliability and validity of the Japanese version of the abbreviated Lubben Social Network Scale. Nippon Ronen Igakkai Zasshi. Jpn. J. Geriatr. 2011, 48, 149–157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naito, M.; Suzukamo, Y.; Nakayama, T.; Hamajima, N.; Fukuhara, S. Linguistic Adaptation and Validation of the General Oral Health Assessment Index (GOHAI) in an Elderly Japanese Population. J. Public Health Dent. 2006, 66, 273–275. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T. Frailty as a clinical and social implication. J. Jpn. Geriat. Soc. 2015, 52, 329–335. [Google Scholar]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Healyh Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef] [Green Version]
- Sagong, H.; Yoon, J. Pathways among Frailty, Health Literacy, Acculturation, and Social Support of Middle-Aged and Older Korean Immigrants in the USA. Int. J. Environ. Res. Public Health 2021, 18, 1245. [Google Scholar] [CrossRef]
- Kickbusch, I.; Maag, D. Health literacy. In International Encyclopedia of Public Health; Kris, H., Stella, Q., Eds.; Academic Press: San Diego, CA, USA, 2008; pp. 204–211. [Google Scholar]
- Kobayashi, L.C.; Wardle, J.; Wolf, M.S.; Von Wagner, C. Aging and Functional Health Literacy: A Systematic Review and Meta-Analysis. J. Gerontol. Ser. B 2016, 71, 445–457. [Google Scholar] [CrossRef]
- Ministry of Health, Lobour and Welfare, Government of Japan. Report from the Future of Community Based Welfare. Available online: https://www.kantei.go.jp/jp/singi/syakaihosyoukokuminkaigi/kaisai/service/dai02/02sankou1.pdf (accessed on 26 December 2021).
- Walters, R.; Leslie, S.J.; Polson, R.; Cusack, T.; Gorely, T. Establishing the efficacy of interventions to improve health literacy and health behaviours: A systematic review. BMC Public Health 2020, 20, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Meng, H.; Tu, N.; Liu, D. The Relationship Between Health Literacy, Social Support, Depression, and Frailty Among Community-Dwelling Older Patients with Hypertension and Diabetes in China. Front. Public Health 2020, 8, 280. [Google Scholar] [CrossRef]
- Shah, A.; Ferri-Guerra, J.; Nadeem, M.Y.; Salguero, D.; Aparicio-Ugarriza, R.; Desir, M.; Ruiz, J.G. The association of health literacy, numeracy and graph literacy with frailty. Aging Clin. Exp. Res. 2019, 31, 1827–1832. [Google Scholar] [CrossRef]
- Ishikawa, H.; Takeuchi, T.; Yano, E. Measuring Functional, Communicative, and Critical Health Literacy Among Diabetic Patients. Diabetes Care 2008, 31, 874–879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machón, M.; Mateo-Abad, M.; Vrotsou, K.; Zupiria, X.; Güell, C.; Rico, L.; Vergara, I. Dietary Patterns and Their Relationship with Frailty in Functionally Independent Older Adults. Nutrients 2018, 10, 406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watts, P.N.; Blane, D.; Netuveli, G. Minimum income for healthy living and frailty in adults over 65 years old in the English Longitudinal Study of Ageing: A population-based cohort study. BMJ Open 2019, 9, e025334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Total | Frailty-Progressing Group | Robust Group | p | |
|---|---|---|---|---|
| N | 621 | 158 (25.4%) | 463 (74.6%) | |
| Age a | 71.6 ± 4.6 | 72.7 ± 4.8 | 71.2 ± 4.4 | <0.001 |
| Sex b | ||||
| Male | 348 (56.0%) | 81 (51.3%) | 267 (57.7%) | 0.16 |
| Female | 273(44.0%) | 77 (48.7%) | 196 (42.3%) | |
| BMI a | 23.0 ± 2.7 | 23 ± 2.9 | 23 ± 2.7 | 0.62 |
| Educational background b | ||||
| Elementary/junior high school graduate | 60 (9.7%) | 18 (11.4%) | 42 (9.1%) | 0.56 |
| High school graduate | 286 (46.1%) | 75 (47.5%) | 211 (45.7%) | |
| University/junior college/college graduate | 274 (44.2%) | 65 (41.1%) | 209 (45.2%) | |
| Household staus b | ||||
| Living with someone | 562 (90.5%) | 141 (89.2%) | 421 (90.9%) | 0.53 |
| Living alone | 59 (9.5%) | 17 (10.8%) | 42 (9.1%) | |
| Income b | ||||
| Low | 317 (51.5%) | 83 (52.9%) | 234 (51%) | 0.68 |
| High | 299 (48.5%) | 74 (47.1%) | 225 (49%) | |
| 2012 KCL score, mean ± SD a | 1.5 ± 1.0 | 2.0 ± 0.9 | 1.3 ± 1.0 | <0.001 |
| 2016 KCL score, mean ± SD a | 2.6 ± 2.2 | 5.7 ± 1.9 | 1.5 ± 1.0 | <0.001 |
| 2012–2016ΔKCL score, mean ± SD a | 1.1 ± 2.1 | 3.7 ± 2.0 | 0.2 ± 1.2 | <0.001 |
| Health literacy b | ||||
| Low | 144 (23.2%) | 52 (32.9%) | 92 (19.9%) | <0.001 |
| High | 477 (76.8%) | 106 (67.1%) | 371 (80.1%) | |
| Mental Health: WHO-5 a | 19.2 ± 3.6 | 17.9 ± 3.7 | 19.7 ± 3.5 | <0.001 |
| Social Support: LSNS-6 a | 17.3 ± 5.6 | 15.6 ± 5.7 | 17.9 ± 5.5 | <0.001 |
| Oral quality of life: GOHAI a | 56.5 ± 4.6 | 55.5 ± 4.8 | 56.8 ± 4.4 | <0.001 |
| Social capital indices b | ||||
| Trust: People in the community can be trusted. | ||||
| 1. Disagree/somewhat disagree | 15 (2.4%) | 6 (3.8%) | 9 (1.9%) | 0.09 |
| 2. Neither agree nor disagree | 125 (20.1%) | 39 (24.7%) | 86 (18.6%) | |
| 3. Agree/somewhat agree | 481 (77.5%) | 113 (71.5%) | 368 (79.5%) | |
| Cohesion: People in the community are very united | ||||
| 1. Disagree/somewhat disagree | 53 (8.5%) | 19 (12%) | 34 (7.3%) | 0.11 |
| 2. Neither agree nor disagree | 223 (35.9%) | 60 (38%) | 163 (35.2%) | |
| 3. Agree/somewhat agree | 345 (55.6%) | 79 (50%) | 266 (57.5%) | |
| Mutual aid: People in the community are willing to assist their neighbors | ||||
| 1. Disagree/somewhat disagree | 35 (5.6%) | 18 (11.5%) | 17 (3.7%) | <0.001 |
| 2. Neither agree nor disagree | 184 (29.7%) | 50 (31.8%) | 134 (28.9%) | |
| 3. Agree/somewhat agree | 401 (64.7%) | 89 (56.7%) | 312 (67.4%) |
| Low HL Group (n = 144) | High HL Group (n = 477) | p | |
|---|---|---|---|
| Age a | 71.4 ± 4.8 | 71.6 ± 4.5 | 0.41 |
| Sex b | |||
| Male | 78 (54.2%) | 270 (56.6%) | 0.61 |
| Female | 66 (45.8%) | 207 (43.4%) | |
| 2012 KCL score a | 1.6 ± 1.0 | 1.4 ± 1.0 | 0.20 |
| 2016 KCL score a | 3.1 ± 2.3 | 2.4 ± 2.2 | <0.001 |
| ΔKCL score a | 1.5 ± 2.1 | 1.0 ± 2.1 | <0.001 |
| Mental health: WHO-5 a | 18.1 ± 3.8 | 19.6 ± 3.5 | <0.001 |
| Social support: LSNS-6 a | 16.4 ± 5.8 | 17.6 ± 5.6 | 0.02 |
| Social capital b | |||
| Mutual aid | |||
| Disagree/Somewhat disagree | 12 (8.3%) | 23 (4.8%) | 0.02 |
| Neither agree nor disagree | 52 (36.1%) | 132 (27.7%) | |
| Agree/Somewhat agree | 80 (55.6%) | 321 (67.4%) |
| Crude Odds Ratio [95% CI] | p | Adjusted Odds Ratio [95% CI]: Model 1 a | p | Adjusted Odds Ratio [95% CI]: Model 2 b | p | |
|---|---|---|---|---|---|---|
| Age a,b | 1.07 [1.03, 1.12] | <0.001 | 1.07 [1.03, 1.12] | <0.001 | 1.09 [1.04, 1.14] | <0.001 |
| Sex (Male) a,b | 0.77 [0.54, 1.11] | 0.16 | 0.51 [0.27, 0.95] | 0.04 | 0.33 [0.17, 0.66] | <0.001 |
| BMI a,b | 1.01 [0.94, 1.08] | 0.81 | 1.01 [0.94, 1.09] | 0.74 | 1.02 [0.94, 1.1] | 0.68 |
| Educational background a,b | ||||||
| Elementary/junior high school graduate | 1.38 [0.74, 2.56] | 0.31 | 1.06 [0.52, 2.17] | 0.88 | 1.04 [0.48, 2.23] | 0.92 |
| High school graduate | 1.14 [0.78, 1.68] | 0.49 | 1.07 [0.69, 1.64] | 0.78 | 1.04 [0.66, 1.64] | 0.87 |
| Household status (not living with family) a,b | 1.21 [0.67, 2.19] | 0.53 | 0.98 [0.5, 1.92] | 0.95 | 0.92 [0.45, 1.88] | 0.82 |
| Income (low) a,b | 1.08 [0.75, 1.55] | 0.68 | 0.68 [0.36, 1.27] | 0.22 | 0.58 [0.30, 1.11] | 0.10 |
| 2012 KCL Score a,b | 2.16 [1.76, 2.64] | <0.001 | 2.19 [1.77, 2.71] | <0.001 | 1.97 [1.57, 2.47] | <0.001 |
| Health literacy (low) | 1.98 [1.32, 2.96] | <0.001 | 2.07 [1.32, 3.24] | <0.001 | 1.72 [1.07, 2.77] | 0.02 |
| Mental health: WHO-5 b | 0.88 [0.83, 0.92] | <0.001 | 0.90 [0.85, 0.96] | <0.001 | ||
| Social support: LSNS-6 b | 0.93 [0.9, 0.96] | <0.001 | 0.95 [0.91, 0.98] | 0.01 | ||
| Oral Quality of Life: GOHAI b | 0.94 [0.91, 0.98] | <0.001 | 0.99 [0.94, 1.03] | 0.53 | ||
| Social capital indices b | ||||||
| Trust: People in the community can be trusted. | ||||||
| Disagree/Somewhat disagree | 2.17 [0.76, 6.23] | 0.15 | 0.98 [0.26, 3.75] | 0.98 | ||
| Cohesion: People in the community are very united | ||||||
| Disagree/Somewhat disagree | 1.88 [1.02, 3.48] | 0.04 | 0.54 [0.21, 1.38] | 0.20 | ||
| Mutual aid: People in the community are willing to help their neighbors | ||||||
| Disagree/Somewhat disagree | 3.71 [1.84, 7.5] | <0.001 | 2.98 [1.09, 8.14] | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoshizawa, Y.; Tanaka, T.; Takahashi, K.; Fujisaki-Sueda-Sakai, M.; Son, B.-k.; Iijima, K. Impact of Health Literacy on the Progression of Frailty after 4 Years among Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 394. https://doi.org/10.3390/ijerph19010394
Yoshizawa Y, Tanaka T, Takahashi K, Fujisaki-Sueda-Sakai M, Son B-k, Iijima K. Impact of Health Literacy on the Progression of Frailty after 4 Years among Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health. 2022; 19(1):394. https://doi.org/10.3390/ijerph19010394
Chicago/Turabian StyleYoshizawa, Yasuyo, Tomoki Tanaka, Kyo Takahashi, Mahiro Fujisaki-Sueda-Sakai, Bo-kyung Son, and Katsuya Iijima. 2022. "Impact of Health Literacy on the Progression of Frailty after 4 Years among Community-Dwelling Older Adults" International Journal of Environmental Research and Public Health 19, no. 1: 394. https://doi.org/10.3390/ijerph19010394
APA StyleYoshizawa, Y., Tanaka, T., Takahashi, K., Fujisaki-Sueda-Sakai, M., Son, B.-k., & Iijima, K. (2022). Impact of Health Literacy on the Progression of Frailty after 4 Years among Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health, 19(1), 394. https://doi.org/10.3390/ijerph19010394






