Feasibility, Effectiveness, and Mechanisms of a Brief Mindfulness- and Compassion-Based Program to Reduce Stress in University Students: A Pilot Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
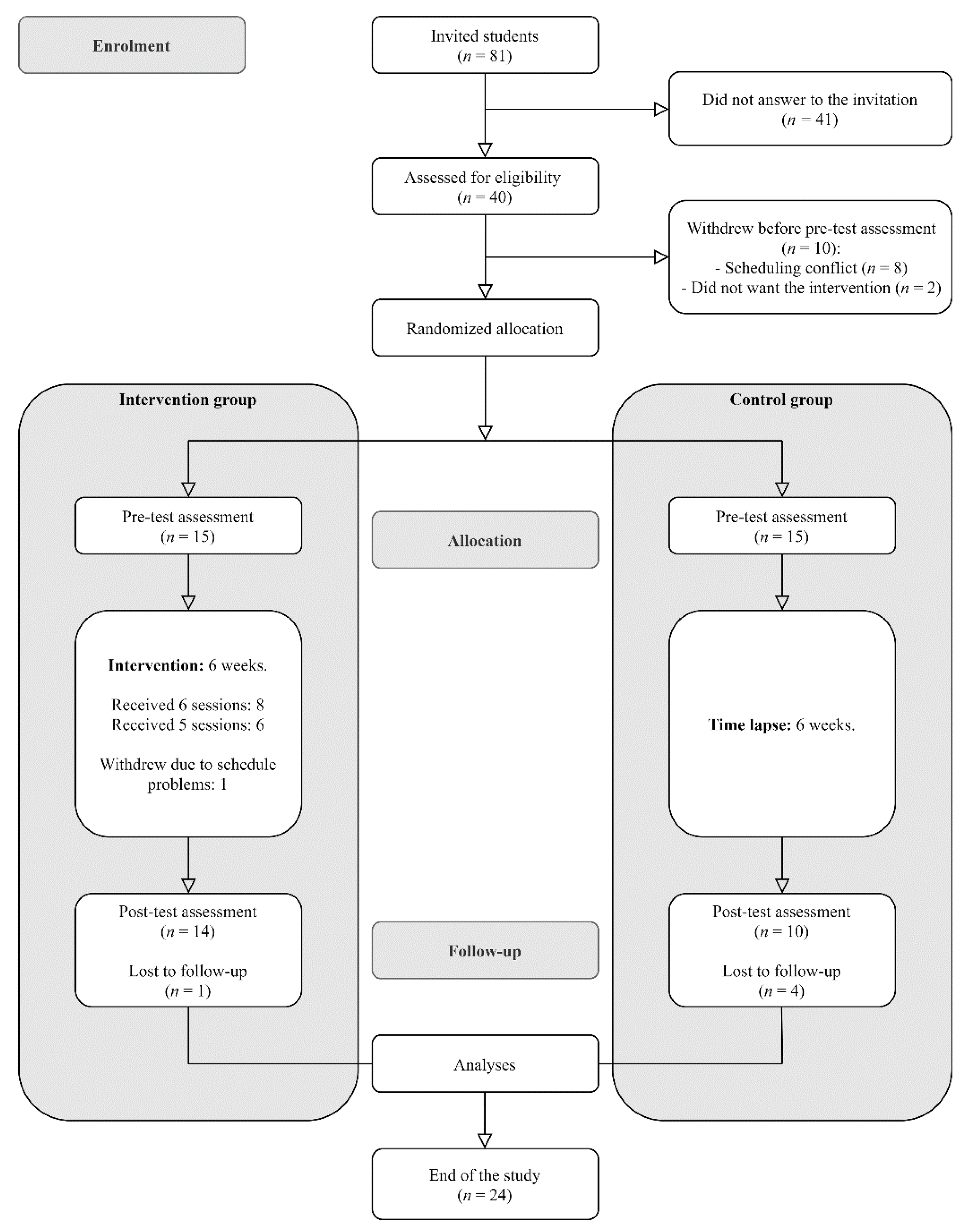
2.1. Participants
2.2. Procedure
2.3. Mindfulness- and Compassion-Based Program: MCBP for University Life
2.4. Measures
2.4.1. Sociodemographic Information
2.4.2. Feasibility
2.4.3. Main Outcomes
2.4.4. Mechanistic Variables
2.5. Data Analysis
3. Results
3.1. Feasibility
3.2. Effectiveness of the MBP
3.3. Correlations between Variables and Change Scores
3.4. Mediating Role of Mindfulness Skills, Decentering, Self-Compassion, and Experiential Avoidance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Auerbach, R.P.; Alonso, J.; Axinn, W.G.; Cuijpers, P.; Ebert, D.D.; Green, J.G.; Hwang, I.; Kessler, R.C.; Liu, H.; Mortier, P. Mental Disorders among College Students in the World Health Organization World Mental Health Surveys. Psychol. Med. 2016, 46, 2955–2970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheldon, E.; Simmonds-Buckley, M.; Bone, C.; Mascarenhas, T.; Chan, N.; Wincott, M.; Gleeson, H.; Sow, K.; Hind, D.; Barkham, M. Prevalence and Risk Factors for Mental Health Problems in University Undergraduate Students: A Systematic Review with Meta-Analysis. J. Affect. Disord. 2021, 287, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Drakos, A.; Zuo, Q.K.; Huang, E. The Prevalence of Depressive Symptoms, Anxiety Symptoms and Sleep Disturbance in Higher Education Students during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Psychiatry Res. 2021, 301, 113863. [Google Scholar] [CrossRef] [PubMed]
- Hoyt, L.T.; Cohen, A.K.; Dull, B.; Maker Castro, E.; Yazdani, N. “Constant Stress Has Become the New Normal”: Stress and Anxiety Inequalities Among U.S. College Students in the Time of COVID-19. J. Adolesc. Health 2021, 68, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Karaman, M.A.; Lerma, E.; Vela, J.C.; Watson, J.C. Predictors of Academic Stress Among College Students. J. Coll. Couns. 2019, 22, 41–55. [Google Scholar] [CrossRef] [Green Version]
- Sharp, J.; Theiler, S. A Review of Psychological Distress Among University Students: Pervasiveness, Implications and Potential Points of Intervention. Int. J. Adv. Couns. 2018, 40, 193–212. [Google Scholar] [CrossRef]
- Dawson, A.F.; Brown, W.W.; Anderson, J.; Datta, B.; Donald, J.N.; Hong, K.; Allan, S.; Mole, T.B.; Jones, P.B.; Galante, J. Mindfulness-Based Interventions for University Students: A Systematic Review and Meta-Analysis of randomized Controlled Trials. Appl. Psychol. Health Well-Being 2020, 12, 384–410. [Google Scholar] [CrossRef] [PubMed]
- Regehr, C.; Glancy, D.; Pitts, A. Interventions to Reduce Stress in University Students: A Review and Meta-Analysis. J. Affect. Disord. 2013, 148, 1–11. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Full Catastrophe Living, Revised Edition: How to Cope with Stress, Pain and Illness Using Mindfulness Meditation; Piatkus: London, UK, 2013. [Google Scholar]
- Segal, Z.V.; Williams, J.M.G.; Teasdale, J.D. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse; Guilford Press: New York, NY, USA, 2002. [Google Scholar]
- Querstret, D.; Morison, L.; Dickinson, S.; Cropley, M.; John, M. Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy for Psychological Health and Well-Being in Nonclinical Samples: A Systematic Review and Meta-Analysis. Int. J. Stress Manag. 2020, 27, 394–411. [Google Scholar] [CrossRef]
- Bishop, S.R.; Lau, M.; Shapiro, S.; Carlson, L.; Anderson, N.D.; Carmody, J.; Segal, Z.V.; Abbey, S.; Speca, M.; Velting, D. Mindfulness: A Proposed Operational Definition. Clin. Psychol. Sci. Pract. 2004, 11, 230. [Google Scholar] [CrossRef]
- Crane, R.S.; Brewer, J.; Feldman, C.; Kabat-Zinn, J.; Santorelli, S.; Williams, J.M.G.; Kuyken, W. What Defines Mindfulness-Based Programs? The Warp and the Weft. Psychol. Med. 2017, 47, 990–999. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hervás, G.; Cebolla, A.; Soler, J. Intervenciones Psicológicas Basadas En Mindfulness y Sus Beneficios: Estado Actual de La Cuestión. Clínica. Y. Salud. 2016, 27, 115–124. [Google Scholar] [CrossRef] [Green Version]
- Gu, J.; Strauss, C.; Bond, R.; Cavanagh, K. How Do Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction Improve Mental Health and Wellbeing? A Systematic Review and Meta-Analysis of Mediation Studies. Clin. Psychol. Rev. 2015, 37, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Zhang, Y.; Cui, Z. Mindfulness-Based Interventions for Prevention of Depressive Symptoms in University Students: A Meta-Analytic Review. Mindfulness 2019, 10, 2209–2224. [Google Scholar] [CrossRef]
- Galante, J.; Dufour, G.; Vainre, M.; Wagner, A.P.; Stochl, J.; Benton, A.; Lathia, N.; Howarth, E.; Jones, P.B. A Mindfulness-Based Intervention to Increase Resilience to Stress in University Students (the Mindful Student Study): A Pragmatic randomized Controlled Trial. Lancet Public Health 2018, 3, e72–e81. [Google Scholar] [CrossRef] [Green Version]
- Medlicott, E.; Phillips, A.; Crane, C.; Hinze, V.; Taylor, L.; Tickell, A.; Montero-Marin, J.; Kuyken, W. The Mental Health and Wellbeing of University Students: Acceptability, Effectiveness, and Mechanisms of a Mindfulness-Based Course. Int. J. Environ. Res. Public Health 2021, 18, 6023. [Google Scholar] [CrossRef]
- Modrego-Alarcón, M.; López-del-Hoyo, Y.; García-Campayo, J.; Pérez-Aranda, A.; Navarro-Gil, M.; Beltrán-Ruiz, M.; Morillo, H.; Delgado-Suarez, I.; Oliván-Arévalo, R.; Montero-Marin, J. Efficacy of a Mindfulness-Based program with and without Virtual Reality Support to Reduce Stress in University Students: A Randomized Controlled Trial. Behav. Res. Ther. 2021, 142, 103866. [Google Scholar] [CrossRef]
- Alsubaie, M.; Abbott, R.; Dunn, B.; Dickens, C.; Keil, T.F.; Henley, W.; Kuyken, W. Mechanisms of Action in Mindfulness-Based Cognitive Therapy (MBCT) and Mindfulness-Based Stress Reduction (MBSR) in People with Physical and/or Psychological Conditions: A Systematic Review. Clin. Psychol. Rev. 2017, 55, 74–91. [Google Scholar] [CrossRef]
- Martínez-Rubio, D.; Martínez-Brotons, C.; Monreal-Bartolomé, A.; Barceló-Soler, A.; Campos, D.; Pérez-Aranda, A.; Colomer-Carbonell, A.; Cervera-Torres, S.; Solé, S.; Moreno, Y. Protective Role of Mindfulness, Self-Compassion and Psychological Flexibility on the Burnout Subtypes among Psychology and Nursing Undergraduate Students. J. Adv. Nurs. 2021, 77, 3398–3411. [Google Scholar] [CrossRef]
- Brito-Pons, G.; Campos, D.; Cebolla, A. Implicit or Explicit Compassion? Effects of Compassion Cultivation Training and Comparison with Mindfulness-Based Stress Reduction. Mindfulness 2018, 9, 1494–1508. [Google Scholar] [CrossRef]
- Dahl, C.J.; Lutz, A.; Davidson, R.J. Reconstructing and Deconstructing the Self: Cognitive Mechanisms in Meditation Practice. Trends Cogn. Sci. 2015, 19, 515–523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strauss, C.; Taylor, B.L.; Gu, J.; Kuyken, W.; Baer, R.; Jones, F.; Cavanagh, K. What Is Compassion and How Can We Measure It? A Review of Definitions and Measures. Clin. Psychol. Rev. 2016, 47, 15–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loucks, E.; Crane, R.S.; Sanghvi, M.A.; Montero-Marín, J.; Proulx, J.; Brewer, J.A.; Kuyken, W. Mindfulness-Based Programs: Why, When, and How to Adapt? Glob. Adv. Health Med. 2021, in press.
- Demarzo, M.; Montero-Marin, J.; Puebla-Guedea, M.; Navarro-Gil, M.; Herrera-Mercadal, P.; Moreno-González, S.; Calvo-Carrión, S.; Bafaluy-Franch, L.; Garcia-Campayo, J. Efficacy of 8-and 4-Session Mindfulness-Based Interventions in a Non-Clinical Population: A Controlled Study. Front. Psychol. 2017, 8, 1343. [Google Scholar] [CrossRef] [Green Version]
- Berghoff, C.R.; Wheeless, L.E.; Ritzert, T.R.; Wooley, C.M.; Forsyth, J.P. Mindfulness Meditation Adherence in a College Sample: Comparison of a 10-Min versus 20-Min 2-Week Daily Practice. Mindfulness 2017, 8, 1513–1521. [Google Scholar] [CrossRef]
- Gilbert, P. The Origins and Nature of Compassion Focused Therapy. Br. J. Clin. Psychol. 2014, 53, 6–41. [Google Scholar] [CrossRef]
- Ash, M.; Harrison, T.; Pinto, M.; DiClemente, R.; Negi, L.T. A model for cognitively-based compassion training: Theoretical underpinnings and proposed mechanisms. Soc. Theory Health 2021, 19, 43–67. [Google Scholar] [CrossRef] [Green Version]
- Pace, T.W.; Negi, L.T.; Adame, D.D.; Cole, S.P.; Sivilli, T.I.; Brown, T.D.; Issa, M.J.; Raison, C.L. Effect of Compassion Meditation on Neuroendocrine, Innate Immune and Behavioral Responses to Psychosocial Stress. Psychoneuroendocrinology 2009, 34, 87–98. [Google Scholar] [CrossRef] [Green Version]
- Neff, K.D.; Germer, C.K. A Pilot Study and Randomized Controlled Trial of the Mindful Self-Compassion Program. J. Clin. Psychol. 2013, 69, 28–44. [Google Scholar] [CrossRef]
- O’Cathain, A.; Croot, L.; Duncan, E.; Rousseau, N.; Sworn, K.; Turner, K.M.; Yardley, L.; Hoddinott, P. Guidance on How to Develop Complex Interventions to Improve Health and Healthcare. BMJ Open 2019, 9, e029954. [Google Scholar] [CrossRef] [Green Version]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Remor, E. Psychometric Properties of a European Spanish Version of the Perceived Stress Scale (PSS). Span. J. Psychol. 2006, 9, 86–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldberg, D.P.; Williams, P. A User’s Guide to the General Health Questionnaire; NFER-Nelson: Windsor, UK, 1988. [Google Scholar]
- Rocha, K.B.; Pérez, K.; Rodríguez-Sanz, M.; Borrell, C.; Obiols, J.E. Propiedades Psicométricas y Valores Normativos Del General Health Questionnaire (GHQ-12) En Población General Española. Int. J. Clin. Health Psychol. 2011, 11, 125–139. [Google Scholar]
- Gu, J.; Strauss, C.; Crane, C.; Barnhofer, T.; Karl, A.; Cavanagh, K.; Kuyken, W. Examining the Factor Structure of the 39-Item and 15-Item Versions of the Five Facet Mindfulness Questionnaire before and after Mindfulness-Based Cognitive Therapy for People with Recurrent Depression. Psychol. Assess. 2016, 28, 791. [Google Scholar] [CrossRef] [Green Version]
- Feliu-Soler, A.; Pérez-Aranda, A.; Luciano, J.V.; Demarzo, M.; Mariño, M.; Soler, J.; Van Gordon, W.; García-Campayo, J.; Montero-Marín, J. Psychometric Properties of the 15-Item Five Facet Mindfulness Questionnaire in a Large Sample of Spanish Pilgrims. Mindfulness 2021, 12, 852–862. [Google Scholar] [CrossRef]
- Fresco, D.M.; Moore, M.T.; van Dulmen, M.H.; Segal, Z.V.; Ma, S.H.; Teasdale, J.D.; Williams, J.M.G. Initial Psychometric Properties of the Experiences Questionnaire: Validation of a Self-Report Measure of Decentering. Behav. Ther. 2007, 38, 234–246. [Google Scholar] [CrossRef]
- Soler, J.; Franquesa, A.; Feliu-Soler, A.; Cebolla, A.; García-Campayo, J.; Tejedor, R.; Demarzo, M.; Baños, R.; Pascual, J.C.; Portella, M.J. Assessing Decentering: Validation, Psychometric Properties, and Clinical Usefulness of the Experiences Questionnaire in a Spanish Sample. Behav. Ther. 2014, 45, 863–871. [Google Scholar] [CrossRef] [Green Version]
- Raes, F.; Pommier, E.; Neff, K.D.; Van Gucht, D. Construction and Factorial Validation of a Short Form of the Self-Compassion Scale. Clin. Psychol. Psychother. 2011, 18, 250–255. [Google Scholar] [CrossRef]
- Neff, K.D.; Tóth-Király, I.; Yarnell, L.M.; Arimitsu, K.; Castilho, P.; Ghorbani, N.; Guo, H.X.; Hirsch, J.K.; Hupfeld, J.; Hutz, C.S.; et al. Examining the Factor Structure of the Self-Compassion Scale in 20 Diverse Samples: Support for Use of a Total Score and Six Subscale Scores. Psychol. Assess. 2019, 31, 27–45. [Google Scholar] [CrossRef]
- Garcia-Campayo, J.; Navarro-Gil, M.; Andrés, E.; Montero-Marin, J.; López-Artal, L.; Demarzo, M.M.P. Validation of the Spanish Versions of the Long (26 Items) and Short (12 Items) Forms of the Self-Compassion Scale (SCS). Health Qual. Life Outcomes 2014, 12, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Bond, F.W.; Hayes, S.C.; Baer, R.A.; Carpenter, K.M.; Guenole, N.; Orcutt, H.K.; Waltz, T.; Zettle, R.D. Preliminary Psychometric Properties of the Acceptance and Action Questionnaire–II: A Revised Measure of Psychological Inflexibility and Experiential Avoidance. Behav. Ther. 2011, 42, 676–688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruiz, F.J.; Herrera, Á.I.L.; Luciano, C.; Cangas, A.J.; Beltrán, I. Measuring Experiential Avoidance and Psychological Inflexibility: The Spanish Version of the Acceptance and Action Questionnaire-II. Psicothema 2013, 25, 123–129. [Google Scholar] [PubMed]
- DeVellis, R.F. Scale Development: Theory and Applications; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2011. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences. Stat. Power Anal. Behav. Sci. 1988, 31, 499–500. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process. Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Fairchild, A.J.; MacKinnon, D.P.; Taborga, M.P.; Taylor, A.B. R 2 Effect-Size Measures for Mediation Analysis. Behav. Res. Methods 2009, 41, 486–498. [Google Scholar] [CrossRef] [Green Version]
- Feise, R.J. Do Multiple Outcome Measures Require P-Value Adjustment? BMC Med. Res. Methodol. 2002, 2, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Chang, V.Y.; Palesh, O.; Caldwell, R.; Glasgow, N.; Abramson, M.; Luskin, F.; Gill, M.; Burke, A.; Koopman, C. The Effects of a Mindfulness-Based Stress Reduction Program on Stress, Mindfulness Self-Efficacy, and Positive States of Mind. Stress Health 2004, 20, 141–147. [Google Scholar] [CrossRef]
- Breedvelt, J.J.; Amanvermez, Y.; Harrer, M.; Karyotaki, E.; Gilbody, S.; Bockting, C.L.; Cuijpers, P.; Ebert, D.D. The Effects of Meditation, Yoga, and Mindfulness on Depression, Anxiety, and Stress in Tertiary Education Students: A Meta-Analysis. Front. Psychiatry 2019, 10, 193. [Google Scholar] [CrossRef]
- Phang, C.K.; Chiang, K.C.; Ng, L.O.; Keng, S.-L.; Oei, T.P.S. Effects of Brief Group Mindfulness-Based Cognitive Therapy for Stress Reduction among Medical Students in a Malaysian University. Mindfulness 2016, 7, 189–197. [Google Scholar] [CrossRef]
- Galante, J.; Stochl, J.; Dufour, G.; Vainre, M.; Wagner, A.P.; Jones, P.B. Effectiveness of Providing University Students with a Mindfulness-Based Intervention to Increase Resilience to Stress: 1-Year Follow-up of a Pragmatic randomized Controlled Trial. J. Epidemiol. Community Health 2021, 75, 151–160. [Google Scholar] [CrossRef]
- van der Velden, A.M.; Kuyken, W.; Wattar, U.; Crane, C.; Pallesen, K.J.; Dahlgaard, J.; Fjorback, L.O.; Piet, J. A Systematic Review of Mechanisms of Change in Mindfulness-Based Cognitive Therapy in the Treatment of Recurrent Major Depressive Disorder. Clin. Psychol. Rev. 2015, 37, 26–39. [Google Scholar] [CrossRef] [Green Version]
- Chiesa, A.; Anselmi, R.; Serretti, A. Mechanisms of Mindfulness-Based Interventions: What Do We Know? Holist. Nurs. Pract. 2014, 28, 124–148. [Google Scholar] [CrossRef] [PubMed]


| Baseline Characteristic | MBP Condition (n = 15) | WL Condition (n = 15) | Full Sample (n = 30) | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| Age | 22.08 | 3.65 | 22.5 | 4.64 | 22.29 | 4.17 |
| n | % | n | % | n | % | |
| Gender | ||||||
| Female | 11 | 73 | 14 | 93 | 25 | 83 |
| Male | 4 | 27 | 1 | 7 | 5 | 17 |
| Marital status | ||||||
| Single | 8 | 53 | 9 | 60 | 17 | 57 |
| Committed relationship | 7 | 47 | 6 | 40 | 13 | 43 |
| Perceived parental support | ||||||
| Insufficient | 2 | 13 | 0 | 0 | 2 | 7 |
| Good | 8 | 53 | 8 | 53 | 16 | 53 |
| Very good | 5 | 34 | 7 | 47 | 12 | 40 |
| Perceived social support a | 12 | 80 | 10 | 67 | 22 | 73 |
| Previous participation in stress management programs a | 1 | 6 | 1 | 6 | 2 | 7 |
| Having a chronic disease a | 2 | 13 | 3 | 20 | 5 | 17 |
| Previous medication a | 2 | 13 | 1 | 6 | 3 | 10 |
| Session | Program Topic | Meditations and Practices |
|---|---|---|
| Session 1 | Introduction to the basics | Mindful raisin-eating meditation The 3-step breathing space |
| Session 2 | Obstacles to practice | Body Scan (breath–body) Conscious movements |
| Session 3 | The breath and the body | Mindfulness of breathing focusing on the belly Mindfulness of nose-focused breathing |
| Session 4 | Thoughts and emotions | The samurai and the fly (video) Attentive listening 50/50 |
| Session 5 | Kindness and compassion | Sounds and thoughts Compassion (and self-compassion) |
| Session 6 | Mindfulness for life | Group reflection on key learning points Guidelines to keep practicing independently in our daily lives |
| Measurement | MCBP Condition | WL Condition | ANCOVA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Test | Post-Test | t (13) | p | d | Pre-Test | Post-Test | t (9) | p | d | F (1, 21) | p | ηp2 | |
| PSS | 27.86 (8.05) | 18.14 (4.35) | 4.49 | <0.001 | 1.20 | 30.30 (4.92) | 27.50 (6.72) | 2.01 | 0.076 | 0.63 | 15.82 | <0.001 | 0.43 |
| GHQ-12 | 16.21 (6.53) | 5.93 (5.53) | 5.06 | <0.001 | 1.35 | 14.29 (6.29) | 14.00 (6.33) | 0.33 | 0.749 | 0.10 | 14.19 | 0.001 | 0.40 |
| FFMQ-SF | 48.36 (7.96) | 56.07 (4.27) | −5.04 | <0.001 | −1.35 | 46.57 (8.83) | 47.00 (9.29) | −0.36 | 0.729 | −0.11 | 18.25 | <0.001 | 0.47 |
| EQ | 36.29 (6.64) | 44.36 (4.13) | −5.99 | <0.001 | −1.60 | 32.36 (5.42) | 33.80 (5.57) | −1.63 | 0.137 | −0.52 | 19.22 | <0.001 | 0.48 |
| SCS-SF | 3.19 (0.51) | 3.86 (0.34) | −6.75 | <0.001 | −1.80 | 2.53 (0.65) | 2.71 (0.75) | −1.49 | 0.170 | −0.47 | 14.77 | <0.001 | 0.41 |
| AAQII | 24.21 (8.53) | 16.08 (6.34) | 4.44 | <1.001 | 1.23 | 24.64 (1.10) | 27.00 (9.85) | −0.40 | 0.698 | −0.13 | 37.06 | <0.001 | 0.47 |
| ∆ PSS | ∆ GHQ-12 | |
|---|---|---|
| ∆ FFMQ-SF | −0.58 ** | −0.45 * |
| ∆ EQ | −0.60 ** | −0.64 ** |
| ∆ SCS-SF | −0.75 ** | −0.58 ** |
| ∆ AAQII | 0.58 ** | 0.29 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Rubio, D.; Navarrete, J.; Montero-Marin, J. Feasibility, Effectiveness, and Mechanisms of a Brief Mindfulness- and Compassion-Based Program to Reduce Stress in University Students: A Pilot Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 154. https://doi.org/10.3390/ijerph19010154
Martínez-Rubio D, Navarrete J, Montero-Marin J. Feasibility, Effectiveness, and Mechanisms of a Brief Mindfulness- and Compassion-Based Program to Reduce Stress in University Students: A Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(1):154. https://doi.org/10.3390/ijerph19010154
Chicago/Turabian StyleMartínez-Rubio, David, Jaime Navarrete, and Jesus Montero-Marin. 2022. "Feasibility, Effectiveness, and Mechanisms of a Brief Mindfulness- and Compassion-Based Program to Reduce Stress in University Students: A Pilot Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 1: 154. https://doi.org/10.3390/ijerph19010154
APA StyleMartínez-Rubio, D., Navarrete, J., & Montero-Marin, J. (2022). Feasibility, Effectiveness, and Mechanisms of a Brief Mindfulness- and Compassion-Based Program to Reduce Stress in University Students: A Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(1), 154. https://doi.org/10.3390/ijerph19010154








