Numbers and Mortality Risk of Hypertensive Patients with or without Elevated Body Mass Index in China
Abstract
1. Introduction
2. Methods
2.1. Study Populations
2.2. Measurement
2.3. Hypertension
2.4. Body Mass Index (BMI)
2.5. Assessment of Covariables and Mortality
2.6. Statistical Analysis
3. Results
3.1. Percentage and Numbers of Different Blood Pressure (BP) and BMI Statuses (China Health and Retirement Longitudinal Study (CHARLS) Data)
3.2. Characteristics of the Study Population (China Health and Nutrition Survey (CHNS) Data)
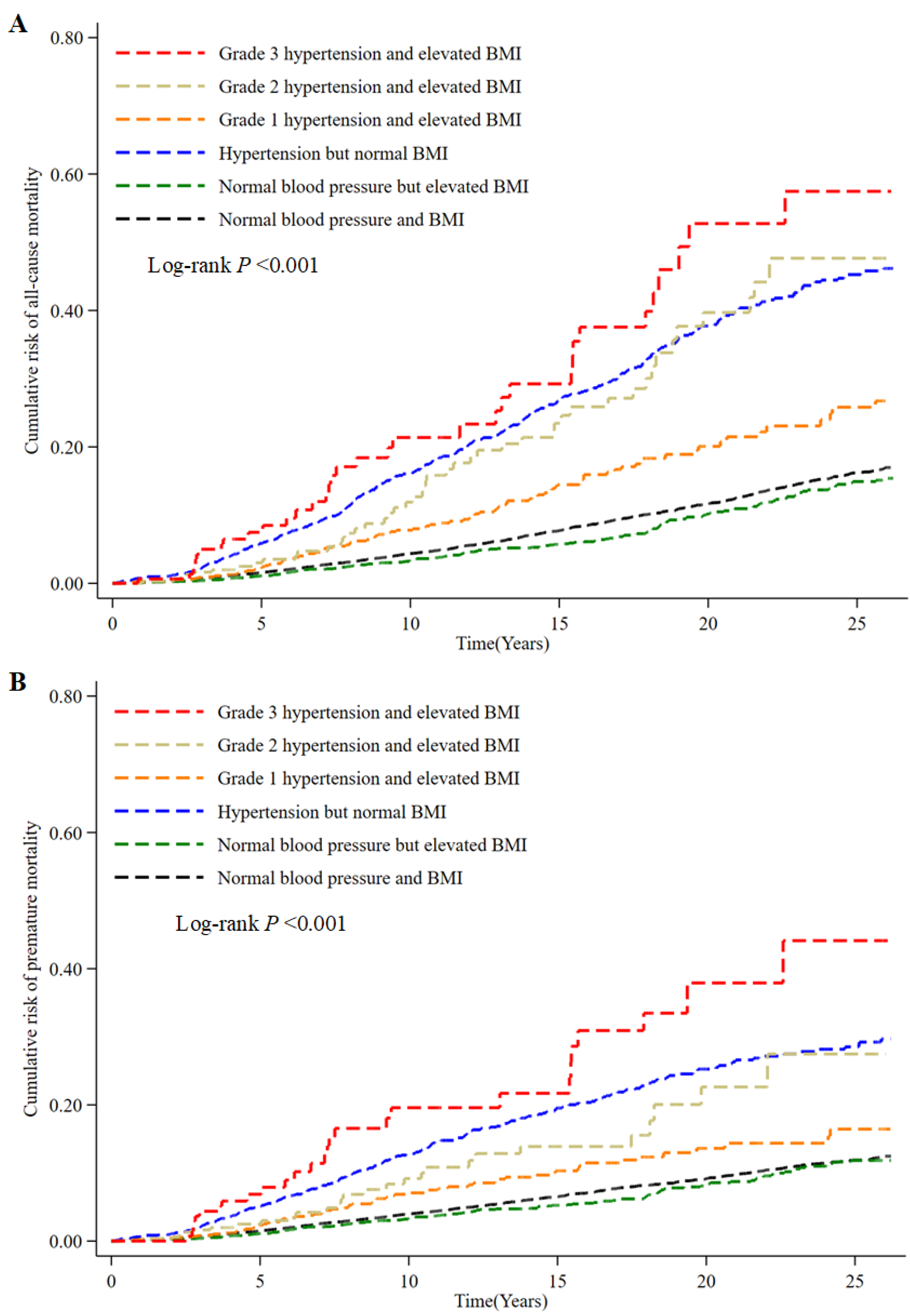
3.3. Associations between Hypertension Categories, BMI, and Mortality (CHNS Data)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| WHO | World Health Organization |
| CVD | Cardiovascular disease |
| CIs | Confidence intervals |
| BMI | Body mass index |
| CHARLS | China Health and Retirement Longitudinal Study |
| CHNS | China Health and Nutrition Survey |
| SBP | Systolic blood pressure |
| DBP | Diastolic blood pressure |
| KM | Kaplan-Meier |
| HRs | Hazard ratios |
| SD | Standard deviation |
| CHL | Chinese Hypertension League |
References
- 2018 Chinese Guidelines for Prevention and Treatment of Hypertension—A Report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J. Geriatr. Cardiol. JGC 2019, 16, 182–241. [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Donald, E.; Casey, J.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [CrossRef]
- World Health Organization. Hypertension. Available online: https://www.who.int/westernpacific/health-topics/hypertension (accessed on 30 August 2021).
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K.; et al. Worldwide Trends in Hypertension Prevalence and Progress in Treatment and Control from 1990 to 2019: A Pooled Analysis of 1201 Population-Representative Studies with 104 Million Participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Narkiewicz, K. Obesity and Hypertension—The Issue Is More Complex than We Thought. Nephrol. Dial. Transplant. 2006, 21, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.-Z.; Lu, W.; Zong, X.-F.; Ruan, H.-Y.; Liu, Y. Obesity and Hypertension. Exp. Ther. Med. 2016, 12, 2395–2399. [Google Scholar] [CrossRef]
- Krauss, R.M.; Winston, M.; Fletcher, B.J.; Grundy, S.M. Obesity: Impact on Cardiovascular Disease. Circulation 1998, 98, 1472–1476. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, Z.; Zhang, L.; Wang, X.; Hao, G.; Zhang, Z.; Shao, L.; Tian, Y.; Dong, Y.; Zheng, C.; et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012–2015. Circulation 2018, 137, 2344–2356. [Google Scholar] [CrossRef]
- Feng, B.Y.; Chen, J.C.; Li, Y.; Huang, J.F.; Li, J.X.; Zhao, L.C.; Cao, J.; Liu, X.Q.; Huang, C.; Deng, Y.; et al. Relationship between overweight/obesity and hypertension among adults in China: A prospective study. Zhonghua Liu Xing Bing Xue Za Zhi 2016, 37, 606–611. [Google Scholar] [CrossRef]
- Li, K.; Yao, C.; Yang, X.; Di, X.; Li, N.; Dong, L.; Xu, L.; Zheng, M. Body Mass Index and the Risk of Cardiovascular and All-Cause Mortality Among Patients With Hypertension: A Population-Based Prospective Cohort Study Among Adults in Beijing, China. J. Epidemiol. 2016, 26, 654–660. [Google Scholar] [CrossRef]
- Dolgalev, I.V.; Brazovskaya, N.G.; Ivanova, A.Y.; Shipkhineeva, A.Y.; Bogajchuk, P.M. Impact of Hypertension, Overweight, Hypertriglyceridemia and Their Combination for Mortality Rate According to the Results of a 27-Year Cohort Prospective Study. Kardiologiia 2019, 59, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, Y.; Qain, Y.; Zhang, J.; Tang, X.; Sun, J.; Zhu, D. Association of Body Mass Index with Cause Specific Deaths in Chinese Elderly Hypertensive Patients: Minhang Community Study. PLoS ONE 2013, 8, e71223. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Xu, W.; Shubina, M.; Goldberg, S.I.; Turchin, A. Body Mass Index and All-Cause Mortality in Patients with Hypertension. Obes. Silver Spring Md. 2015, 23, 1712–1720. [Google Scholar] [CrossRef] [PubMed]
- Jerant, A.; Franks, P. Body Mass Index, Diabetes, Hypertension, and Short-Term Mortality: A Population-Based Observational Study, 2000–2006. J. Am. Board Fam. Med. 2012, 25, 422–431. [Google Scholar] [CrossRef]
- Bender, R.; Jöckel, K.-H.; Richter, B.; Spraul, M.; Berger, M. Body Weight, Blood Pressure, and Mortality in a Cohort of Obese Patients. Am. J. Epidemiol. 2002, 156, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort Profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey—Monitoring and Understanding Socio-Economic and Health Change in China, 1989–2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.-F.; Cooperative Meta-Analysis Group of the Working Group on Obesity in China. Predictive Values of Body Mass Index and Waist Circumference for Risk Factors of Certain Related Diseases in Chinese Adults—Study on Optimal Cut-off Points of Body Mass Index and Waist Circumference in Chinese Adults. Biomed. Environ. Sci. BES 2002, 15, 83–96. [Google Scholar] [PubMed]
- Zhou, B.-F. Effect of Body Mass Index on All-Cause Mortality and Incidence of Cardiovascular Diseases—Report for Meta-Analysis of Prospective Studies Open Optimal Cut-off Points of Body Mass Index in Chinese Adults. Biomed. Environ. Sci. BES 2002, 15, 245–252. [Google Scholar] [PubMed]
- National Bureau of Statistics of China China Statistical Yearbook 2019; China Statistics Press: Beijing, China, 2019.
- Wu, Y.; Huxley, R.; Li, L.; Anna, V.; Xie, G.; Yao, C.; Woodward, M.; Li, X.; Chalmers, J.; Gao, R.; et al. Prevalence, Awareness, Treatment, and Control of Hypertension in China. Circulation 2008, 118, 2679–2686. [Google Scholar] [CrossRef] [PubMed]
- Bell, A.C.; Adair, L.S.; Popkin, B.M. Understanding the Role of Mediating Risk Factors and Proxy Effects in the Association between Socio-Economic Status and Untreated Hypertension. Soc. Sci. Med. 2004, 59, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Wu, X.; Stamler, J.; Rao, X.; Tao, S.; Friedewald, W.T.; Liao, Y.; Tsai, R.; Stamler, R.; He, H. A North-South Comparison of Blood Pressure and Factors Related to Blood Pressure in the People’s Republic of China: A Report from the PRC-USA Collaborative Study of Cardiovascular Epidemiology. J. Hypertens. 1994, 12, 1103–1112. [Google Scholar] [CrossRef]
- Faeh, D.; Braun, J.; Tarnutzer, S.; Bopp, M. Obesity but Not Overweight Is Associated with Increased Mortality Risk. Eur. J. Epidemiol. 2011, 26, 647. [Google Scholar] [CrossRef]
- Alsarah, A.; Alsara, O.; Bachauwa, G. Hypertension Management in the Elderly: What Is the Optimal Target Blood Pressure? Heart Views 2019, 20, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Takami, Y.; Yamamoto, K.; Arima, H.; Sakima, A. Target Blood Pressure Level for the Treatment of Elderly Hypertensive Patients: A Systematic Review and Meta-Analysis of Randomized Trials. Hypertens. Res. 2019, 42, 660–668. [Google Scholar] [CrossRef]
- Pinto, E. Blood Pressure and Ageing. Postgrad. Med. J. 2007, 83, 109–114. [Google Scholar] [CrossRef]
- Chen, Z.; Yu, J.; Song, Y.; Chui, D. Aging Beijing: Challenges and Strategies of Health Care for the Elderly. Ageing Res. Rev. 2010, 9 (Suppl. 1), S2–S5. [Google Scholar] [CrossRef]
- Wang, M.; Xu, P.S.; Liu, W.; Zhang, C.; Zhang, X.; Wang, L.; Liu, J.; Zhu, Z.; Hu, J.; Luo, P.X.; et al. Prevalence and Changes of BMI Categories in China and Related Chronic Diseases: Cross-Sectional National Health Service Surveys (NHSSs) from 2013 to 2018. EClinicalMedicine 2020, 26, 100521. [Google Scholar] [CrossRef]
- Faselis, C.; Doumas, M.; Panagiotakos, D.; Kheirbek, R.; Korshak, L.; Manolis, A.; Pittaras, A.; Tsioufis, C.; Papademetriou, V.; Fletcher, R.; et al. Body Mass Index, Exercise Capacity, and Mortality Risk in Male Veterans with Hypertension. Am. J. Hypertens. 2012, 25, 444–450. [Google Scholar] [CrossRef]

| Description | Elevated BMI but Not Hypertension | Hypertension but Not Elevated BMI | Elevated BMI and Hypertension | |||
|---|---|---|---|---|---|---|
| Percentage (95% CI) % | Numbers (95% CI) Millions | Percentage (95% CI) % | Numbers (95% CI) Millions | Percentage (95% CI) % | Numbers (95% CI) Millions | |
| Total | 20.17 | 103.16 | 19.77 | 101.08 | 23.02 | 117.74 |
| (18.83, 21.58) | (96.48, 109.83) | (18.28, 21.34) | (94.52, 107.65) | (21.10, 25.06) | (108.79, 126.69) | |
| Age < 65 | 23.57 | 88.15 | 14.93 | 55.85 | 21.98 | 82.21 |
| (22.11, 25.10) | (82.09, 94.21) | (13.34, 16.69) | (50.02, 61.68) | (19.94, 24.17) | (74.10, 90.32) | |
| Age ≥ 65 | 10.92 | 15.01 | 32.91 | 45.23 | 25.85 | 35.53 |
| (8.49, 13.93) | (12.06, 17.95) | (30.38, 35.55) | (42.10, 48.38) | (22.84, 29.12) | (31.69, 39.37) | |
| Male | 17.08 | 41.89 | 20.73 | 50.84 | 19.86 | 48.72 |
| (15.65, 18.61) | (38.02, 45.76) | (18.60, 23.03) | (46.41, 55.27) | (17.91, 21.97) | (44.06, 53.38) | |
| Female | 23.02 | 61.27 | 18.88 | 50.24 | 25.94 | 69.02 |
| (21.07, 25.10) | (55.83, 66.70) | (17.09, 20.82) | (45.42, 55.07) | (23.34, 28.71) | (61.54, 76.50) | |
| Total | Normal Blood Pressure and BMI | Elevated BMI but Not Hypertension | Hypertension but Not Elevated BMI | Elevated BMI and Hypertension | p-Value | |
|---|---|---|---|---|---|---|
| Number of participants | 22,867 | 13,640 | 4597 | 2075 | 2555 | |
| Age (years) | 41.08 (14.87) | 36.64 (13.59) | 42.05 (13.10) | 53.13 (14.12) | 53.37 (12.02) | <0.001 |
| Age | <0.001 | |||||
| 18–44 | 14,014 (60.76) | 10,018 (73.45) | 2718 (59.13) | 549 (26.46) | 596 (23.33) | |
| 45–64 | 7283 (31.58) | 3070 (22.51) | 1639 (35.65) | 1045 (50.36) | 1481 (57.96) | |
| 65–75 | 1766 (7.66) | 552 (4.05) | 240 (5.22) | 481 (23.18) | 478 (18.71) | |
| Gender | <0.001 | |||||
| Male | 10,347 (45.25) | 5943 (43.57) | 1920 (41.77) | 1184(57.06) | 1300(50.88) | |
| Female | 12,520 (54.75) | 7697 (56.43) | 2677 (58.23) | 891(42.94) | 1255(49.12) | |
| Educational Level | <0.001 | |||||
| Illiterate | 4775 (21.29) | 2782 (20.83) | 735 (16.48) | 679 (34.09) | 519 (21.29) | |
| Primary school | 4143 (18.47) | 2542 (19.03) | 713 (15.99) | 411 (20.63) | 431 (17.68) | |
| Middle/High school | 11,522 (51.36) | 6930 (51.89) | 2450 (54.95) | 788 (39.56) | 1279 (52.46) | |
| Bachelor or above | 1993 (8.88) | 1102 (8.25) | 561 (12.58) | 114 (5.72) | 209 (8.57) | |
| Marital Status | <0.001 | |||||
| Never | 2700 (11.85) | 2179 (16.17) | 311 (6.87) | 103 (5.03) | 84 (3.32) | |
| Married | 20,077 (88.15) | 11,298 (83.83) | 4216 (93.13) | 1945 (94.97) | 2448 (96.68) | |
| Registered Residence | <0.001 | |||||
| Urban | 9824 (42.60) | 5264 (38.59) | 2233 (48.58) | 937 (45.16) | 1332 (52.13) | |
| Rural | 13,239 (57.40) | 8376 (61.41) | 2364 (51.46) | 1138 (54.84) | 1223 (47.87) | |
| Self-Reported Health (Excellent/Very Good) | <0.001 | |||||
| Yes | 14,883 (64.53) | 9412 (69.00) | 2452 (53.34) | 1418 (68.34) | 1449 (56.71) | |
| No | 8180 (35.47) | 4228 (31.00) | 2145 (46.66) | 657 (31.66) | 1106 (43.29) | |
| Smoking Status | <0.001 | |||||
| Non-smoker | 12,459 (70.27) | 6755 (71.56) | 2882 (73.09) | 1081 (59.76) | 1660 (68.45) | |
| Current smoker | 4903 (27.66) | 2589 (27.43) | 961 (24.37) | 663 (36.65) | 660 (27.22) | |
| Ex-smoker | 367 (2.07) | 96 (1.02) | 100 (2.54) | 65 (3.59) | 105 (4.33) | |
| Drinking Status | <0.001 | |||||
| Non-drinker | 11,695 (65.64) | 6415 (67.49) | 2595 (65.83) | 1111 (60.81) | 1496 (61.61) | |
| Drinker | 6121 (34.36) | 3090 (32.51) | 1347 (34.17) | 716 (39.19) | 932 (38.39) | |
| History of Diseases | ||||||
| Stroke | 121 (0.52) | 12 (0.09) | 13 (0.28) | 40 (1.93) | 56 (2.19) | <0.001 |
| Diabetes | 434 (1.88) | 76 (0.56) | 89 (1.94) | 74 (3.57) | 191 (7.48) | <0.001 |
| Cancer | 101 (0.44) | 32 (0.23) | 26 (0.57) | 18 (0.87) | 25 (0.98) | <0.001 |
| BMI (Kg/m2) | 22.77 (3.67) | 20.86 (1.81) | 26.48 (3.19) | 21.43 (1.88) | 27.44 (3.87) | <0.001 |
| SBP (mmHg) | 118.65 (17.88) | 111.03 (11.52) | 117.29 (10.81) | 141.60 (18.61) | 143.22 (17.69) | <0.001 |
| DBP (mmHg) | 76.63 (11.06) | 72.13 (8.03) | 76.18 (7.17) | 89.94 (10.47) | 90.79 (10.62) | <0.001 |
| Model 1 * | Model 2 † | Model 3 ‡ | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| All-Cause Mortality | ||||||
| Normal BP and BMI | Reference | Reference | Reference | |||
| Normal BP but 1 elevated BMI | 0.82 | 0.70–0.97 | 0.90 | 0.74–1.09 | 0.93 | 0.77–1.13 |
| 2 Hypertension but normal BMI | 3.63 | 3.22–4.09 | 1.65 | 1.44–1.90 | 1.65 | 1.43–1.90 |
| Grade 1 Hypertension and elevated BMI | 1.73 | 1.40–2.13 | 0.95 | 0.75–1.21 | 0.97 | 0.77–1.24 |
| Grade 2 Hypertension and elevated BMI | 3.19 | 2.38–4.28 | 1.41 | 1.03–1.94 | 1.46 | 1.06–2.00 |
| Grade 3 Hypertension and elevated BMI | 4.96 | 3.54–6.96 | 2.24 | 1.56–3.20 | 2.28 | 1.59–3.26 |
| Premature Death | ||||||
| Normal BP and BMI | Reference | Reference | Reference | |||
| Normal BP but elevated BMI | 0.86 | 0.72–1.04 | 0.93 | 0.74–1.16 | 0.97 | 0.77–1.21 |
| Hypertension but normal BMI | 2.99 | 2.59–3.46 | 1.78 | 1.49–2.12 | 1.78 | 1.49–2.12 |
| Grade 1 Hypertension and elevated BMI | 1.48 | 1.16–1.89 | 1.01 | 0.76–1.34 | 1.03 | 0.77–1.36 |
| Grade 2 Hypertension and elevated BMI | 2.20 | 1.49–3.23 | 1.24 | 0.81–1.90 | 1.28 | 0.84–1.96 |
| Grade 3 Hypertension and elevated BMI | 4.61 | 3.14–6.78 | 2.73 | 1.81–4.10 | 2.78 | 1.85–4.18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luo, X.; Yang, H.; He, Z.; Wang, S.; Li, C.; Chen, T. Numbers and Mortality Risk of Hypertensive Patients with or without Elevated Body Mass Index in China. Int. J. Environ. Res. Public Health 2022, 19, 116. https://doi.org/10.3390/ijerph19010116
Luo X, Yang H, He Z, Wang S, Li C, Chen T. Numbers and Mortality Risk of Hypertensive Patients with or without Elevated Body Mass Index in China. International Journal of Environmental Research and Public Health. 2022; 19(1):116. https://doi.org/10.3390/ijerph19010116
Chicago/Turabian StyleLuo, Xiaoqin, Hexiang Yang, Zhangya He, Shanshan Wang, Chao Li, and Tao Chen. 2022. "Numbers and Mortality Risk of Hypertensive Patients with or without Elevated Body Mass Index in China" International Journal of Environmental Research and Public Health 19, no. 1: 116. https://doi.org/10.3390/ijerph19010116
APA StyleLuo, X., Yang, H., He, Z., Wang, S., Li, C., & Chen, T. (2022). Numbers and Mortality Risk of Hypertensive Patients with or without Elevated Body Mass Index in China. International Journal of Environmental Research and Public Health, 19(1), 116. https://doi.org/10.3390/ijerph19010116






