Integrating Social Determinants of Health to Precision Medicine through Digital Transformation: An Exploratory Roadmap
Abstract
1. Introduction
2. Literature Review
3. Research Methodology
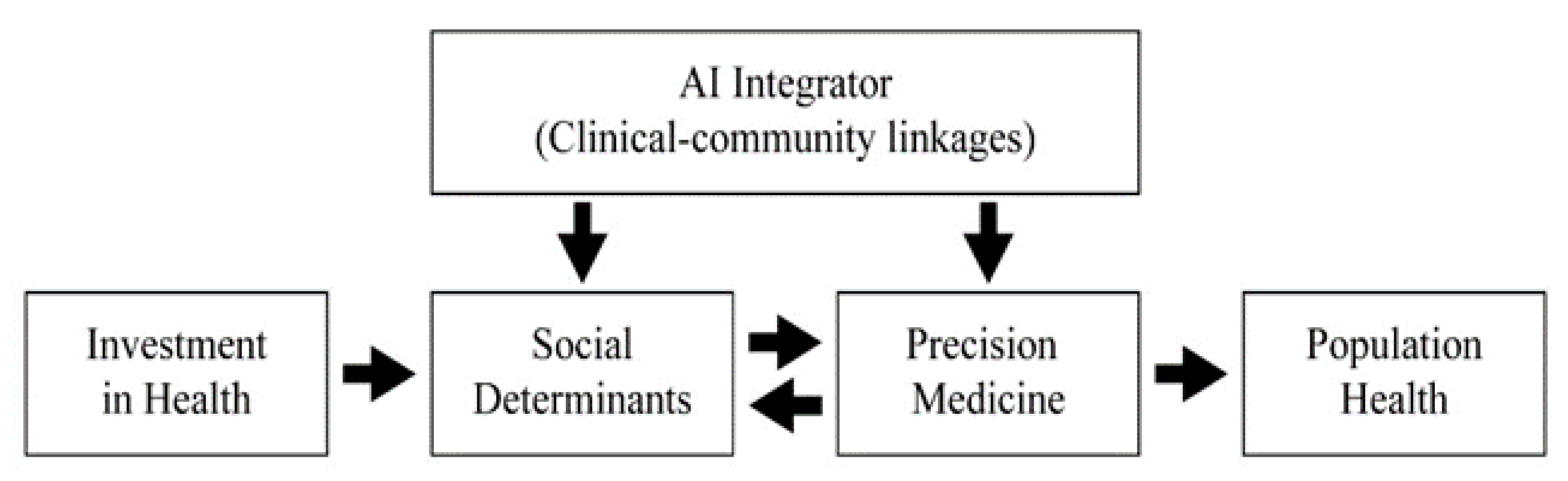
4. Developing an Exploratory Model
4.1. Investing in Health Technology Infrastructure
4.2. Investing in Social Determinants of Health
4.3. Investing in Precision Medicine
4.4. Roles of AI as a Clinical–Community Integrator
5. Discussion and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mehta, M.C.; Katz, I.T.; Jha, A.K. Transform Global Health with AI. NEJM 2020, 382, 791–793. [Google Scholar] [CrossRef] [PubMed]
- Frankel, T. Pandemic Led to Fewer Sports Injuries, More Firework and Power-Tool Accidents. Washington Post, 4 March 2021. Available online: https://www.washingtonpost.com/business/2021/03/04/pandemic-home-injuries (accessed on 26 March 2020).
- Kent, J. How Machine Learning is Transforming Clinical Decision Support Tools. Health IT Analytics. Available online: https://healthitanalytics.com/features/how-machine-learning-is-transforming-clinical-decision-support-tools (accessed on 26 March 2020).
- Stanfill, M.H.; Marc, D.T. Health Information Management: Implications of Artificial Intelligence on Healthcare Data and Information Management. IMIA Yearb. Med. Inform. 2019, 28, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Miriovsky, B.J.; Shulman, L.N.; Abernethy, A.P. Importance of health information technology, electronic health records, and continuously aggregating data to comparative effectiveness research and learning health care. J. Clin. Oncol. 2012, 30, 4243–4248. [Google Scholar] [CrossRef] [PubMed]
- Reddy, M. Digital Transformation in Healthcare in 2021: 7 Key Trends. Digital Authority Partners, 4 January 2021. [Google Scholar]
- Ganguli, I.; Gordon, W.J.; Lupo, C.; Sands-Lincoln, M.; George, J.; Jackson, G.; Rhee, K.; Bates, D.W. Machine Learning and the Pursuit of High-Value Health Care. NEJM Catal. 2021, 1, 1–14. [Google Scholar] [CrossRef]
- Halamka, J.; Cerrato, P. The Digital Reconstruction of Health Care. NEJM Catal. 2021, 1, 1–12. [Google Scholar] [CrossRef]
- Fox, S.; Duggan, M. Health Online 2013. Pew Research Center. 15 January 2013. Available online: https://www.pewresearch.org/internet/2013/01/15/health-online-2013 (accessed on 26 March 2020).
- World Health Organization. Global Strategy on Digital Health 2020–2025; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Kraus, S.; Schiavone, F.; Pluzhnikova, A.; Invernizzi, C.A. Digital transformation in healthcare: Analyzing the current state-of-research. J. Bus. Res. 2021, 123, 558–567. [Google Scholar] [CrossRef]
- Walsh, C.G.; Johnson, K.B.; Ripperger, M.; Sperry, S.; Harris, J.; Clark, N.; Fielstein, E.; Novak, L.; Robinson, K.; Stead, W. Prospective Validation of an Electronic Health Record-Based, Real-Time Suicide Risk Model Prospective Validation of an Electronic Health Record-Based, Real-Time Suicide Risk Model. JAMA Network Open 2021, 4, e211428. [Google Scholar] [CrossRef]
- Zhou, X.; Qui, S.; Joshi, P.S.; Xue, C.; Killiany, R.J.; Mian, A.Z.; Chin, S.P.; Au, R.; Kolachalama, V.B. Enhancing magnetic resonance imaging-driven Alzheimer’s disease classification performance using generative adversarial learning. Alzheimer's Res. Ther. 2021, 13, 1–11. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Social Determinants of Health. 25 September 2017. Available online: www.who.int/social_determinants/sdh_definition/en/ (accessed on 26 March 2020).
- Batheja, C.; Meeting People Where They Really Are. Conference Session at Mayo Clinic Transform 2018, 26 September 2018. Available online: www.youtube.com/watch?v=FUPjbWfl0zM (accessed on 26 March 2020).
- Kim, S.H.; Kwon, I.W.G. Population health from Social Determinants of Health Prospects: A Global Comparison. J. Hosp. Health Care Adm. 2020, 4, 1–9. [Google Scholar] [CrossRef]
- Centers for Medicare & Medicaid Services. Health community Model Health Community Model; CMS: Baltimore, MD, USA, 2015. [Google Scholar]
- Eisenson, H.; Mohta, N.S. Health Care Organizations Can and Must Incorporate Social Determinants. NEJM Catal. 2020, 1, 1–18. [Google Scholar] [CrossRef]
- Elena, D.; Butler, A.B.; Morgan, A.U.; Kangovl, S. Screening for Unmet Social Needs: Patient Engagement or Alienation? NEJM Catal. 2020. [Google Scholar] [CrossRef]
- Fraze, T.K.; Brewster, A.L.; Lewis, V.A.; Beidler, L.B.; Murray, G.F.; Colla, C.H. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by US physician practices and hospitals. JAMA Network Open 2019, 2, e1911514. [Google Scholar] [CrossRef] [PubMed]
- Butler, D.C.; Petterson, S.; Phillips, R.L.; Bazemore, A.W. Measures of Social Deprivation That Predict Health Care Access and Need within a Rational Area of Primary Care Service Delivery. Health Serv. Res. 2013, 48, 539–559. [Google Scholar] [CrossRef]
- Maroko, A.R.; Doan, T.M.; Armo, P.S.; Hubel, M.; Yi, S.; Viola, D. Integrating Social Determinants of Health with Treatment and Prevention: A New Tool to Assess Local Area Deprivation. Preventing Chronic Dis. 2016, 13. [Google Scholar] [CrossRef] [PubMed]
- Snyder, H. Literature review as a research methodology: An overview and guidelines. J. Bus. Res. 2019, 104, 333–339. [Google Scholar] [CrossRef]
- Collier, M.; Fu, R.; Yin, L.; Christiansen, P. Artificial Intelligence (AI): Healthcare’s New Nervous System. Accenture. 2017. Available online: https://www.accenture.com/_acnmedia/PDF-49/Accenture-Health-Artificial-Intelligence.pdf (accessed on 26 March 2020).
- J.D. Power. U.S. Telehealth Satisfaction Study. 2019. Available online: https://www.jdpower.com/business/press-releases/2019-us-telehealth-satisfaction-study (accessed on 28 October 2019).
- Weber, E.; Miller, S.J.; Astha, V.; Janevic, T.; Benn, E. Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J. Am. Med. Inform. Assoc. 2020, 27, 1949–1954. [Google Scholar] [CrossRef] [PubMed]
- American Medical Society. Trends in Health Care Spending. 2019. Available online: https://www.ama-assn.org/about/research/trends-health-care-spending (accessed on 26 March 2020).
- Yednak, C. Will digital show an ROI for Healthcare? PWC Health Research Institute, 18 February 2020. [Google Scholar]
- Crabb, S. Digital Health: Promise, Perils and Perspective. J. AHIMA 90 2019, 5, 32–35. [Google Scholar]
| Domain | Variables |
|---|---|
| Education | % Population aged 25 years or older with less than 9 years of education |
| % Population aged 25 years or older with at least a high school diploma | |
| % Employed population aged 16 years or older in white-collar occupations | |
| Income/employment | Median family income in US dollars |
| Income disparity | |
| % Families below federal poverty level | |
| % Population below 150% of federal poverty level | |
| % Civilian labor force population aged 16 years and older who are unemployed | |
| Housing | Median home value in US dollars |
| Median gross rent in US dollars | |
| Median monthly mortgage in US dollars | |
| % Owner-occupied housing units | |
| % Occupied housing units without complete plumbing | |
| Household characteristics | % Single-parent households with children younger than 18 |
| % Households without a motor vehicle | |
| % Households without a telephone | |
| % Households with more than 1 person per room |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, I.-W.G.; Kim, S.-H.; Martin, D. Integrating Social Determinants of Health to Precision Medicine through Digital Transformation: An Exploratory Roadmap. Int. J. Environ. Res. Public Health 2021, 18, 5018. https://doi.org/10.3390/ijerph18095018
Kwon I-WG, Kim S-H, Martin D. Integrating Social Determinants of Health to Precision Medicine through Digital Transformation: An Exploratory Roadmap. International Journal of Environmental Research and Public Health. 2021; 18(9):5018. https://doi.org/10.3390/ijerph18095018
Chicago/Turabian StyleKwon, Ik-Whan G., Sung-Ho Kim, and David Martin. 2021. "Integrating Social Determinants of Health to Precision Medicine through Digital Transformation: An Exploratory Roadmap" International Journal of Environmental Research and Public Health 18, no. 9: 5018. https://doi.org/10.3390/ijerph18095018
APA StyleKwon, I.-W. G., Kim, S.-H., & Martin, D. (2021). Integrating Social Determinants of Health to Precision Medicine through Digital Transformation: An Exploratory Roadmap. International Journal of Environmental Research and Public Health, 18(9), 5018. https://doi.org/10.3390/ijerph18095018







