Sociocultural Influences on the Feeling of Loneliness of Family Caregivers of People with Dementia: The Role of Kinship
Abstract
1. Introduction
2. Method
2.1. Participants
2.2. Measures
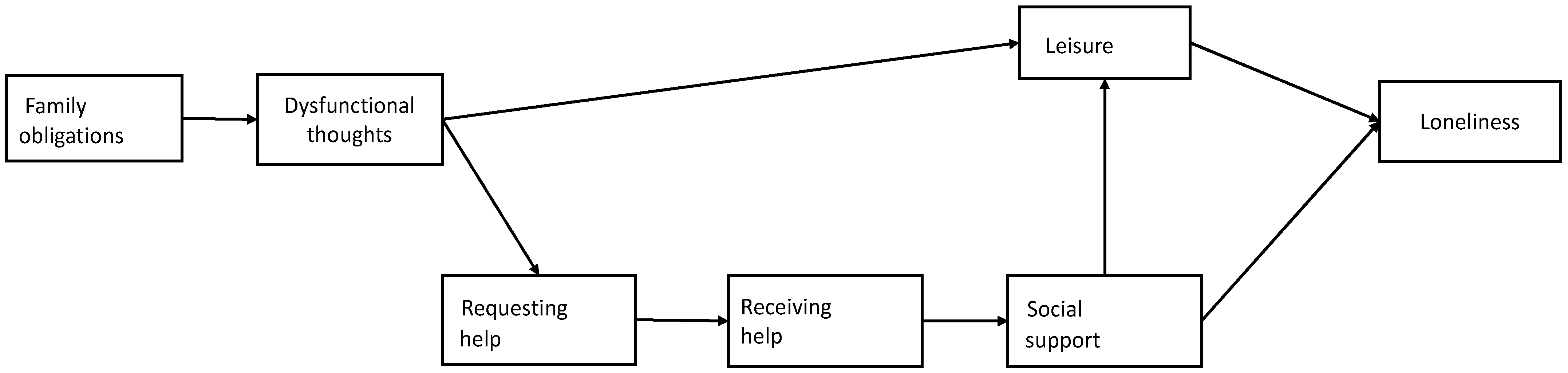
2.3. Data Analysis
3. Results
3.1. Sample Characteristics by Kinship
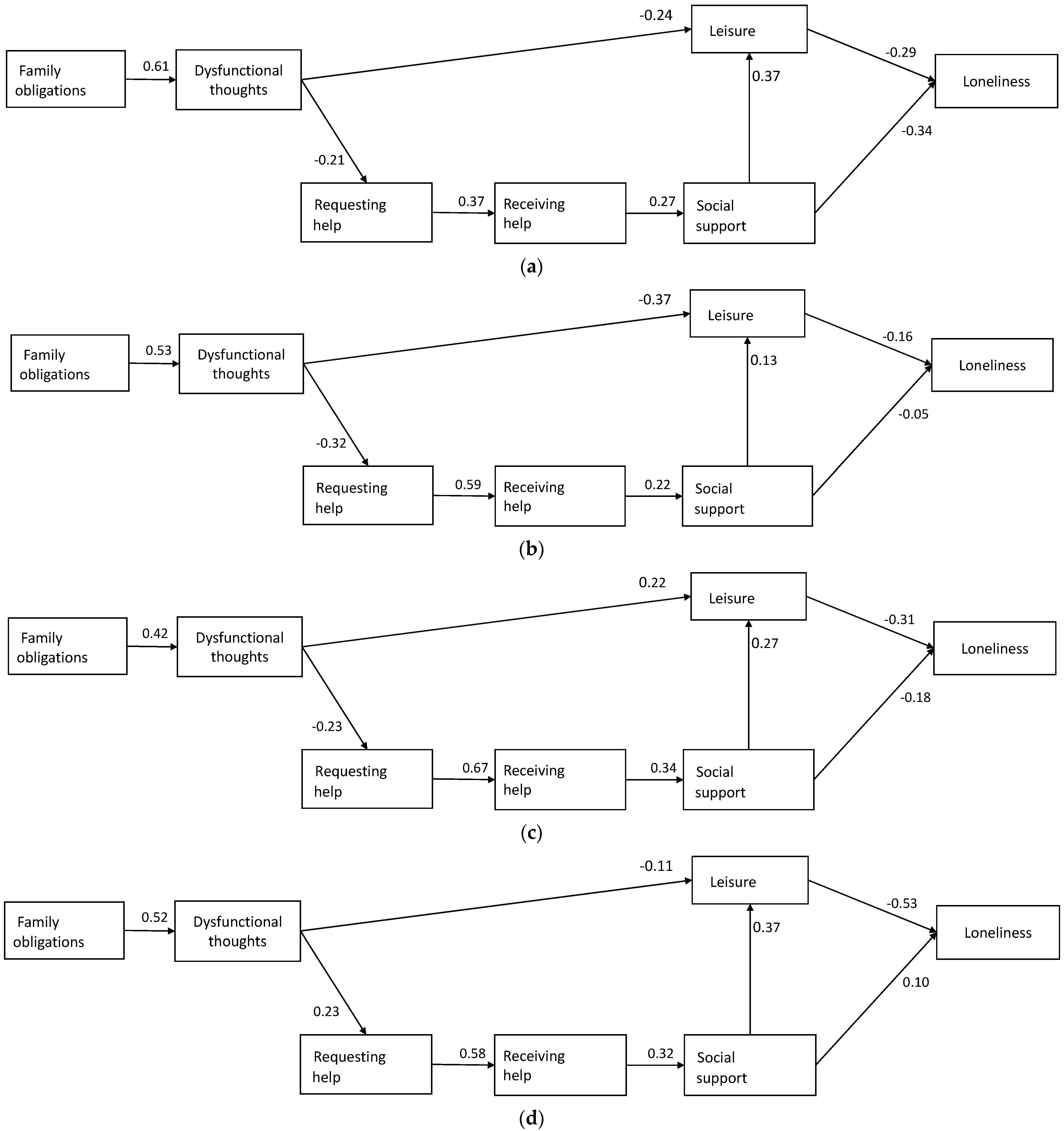
3.2. Model Fit and Associations by Kinship Group
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Dementia: A Public Health Priority. Available online: https://www.who.int/mental_health/publications/dementia_report_2012/en/ (accessed on 27 April 2021).
- Christensen, K.; Doblhammer, G.; Rau, R.; Vaupel, J.W. Ageing populations: The challenges ahead. Lancet 2009, 374, 1196–1208. [Google Scholar] [CrossRef]
- Schulz, R.; Beach, S.R.; Czaja, S.J.; Martire, L.M.; Monin, J.K. Family Caregiving for Older Adults. Annu. Rev. Psychol. 2020, 71, 635–659. [Google Scholar] [CrossRef]
- Collins, R.N.; Kishita, N. Prevalence of depression and burden among informal care-givers of people with dementia: A meta-analysis. Ageing Soc. 2020, 40, 2355–2392. [Google Scholar] [CrossRef]
- Beeson, R.A. Loneliness and depression in spousal caregivers of those with Alzheimer’s disease versus non-caregiving spouses. Arch. Psychiatr. Nurs. 2003, 17, 135–143. [Google Scholar] [CrossRef]
- Ekwall, A.K.; Sivberg, B.; Hallberg, I.R. Loneliness as a predictor of quality of life among older caregivers. J. Adv. Nurs. 2005, 49, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Kovaleva, M.; Spangler, S.; Clevenger, C.; Hepburn, K. Chronic Stress, Social Isolation, and Perceived Loneliness in Dementia Caregivers. J. Psychosoc. Nurs. Ment. Health Serv. 2018, 56, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M.; Sörensen, S. Gender Differences in Caregiver Stressors, Social Resources, and Health: An Updated Meta-Analysis. J. Gerontol. Ser. B 2006, 61, P33–P45. [Google Scholar] [CrossRef] [PubMed]
- Conde-Sala, J.L.; Garre-Olmo, J.; Turró-Garriga, O.; Vilalta-Franch, J.; López-Pousa, S. Quality of Life of Patients with Alzheimer’s Disease: Differential Perceptions between Spouse and Adult Child Caregivers. Dement. Geriatr. Cogn. Disord. 2010, 29, 97–108. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Knight, B.G.; Sayegh, P. Cultural Values and Caregiving: The Updated Sociocultural Stress and Coping Model. J. Gerontol. Ser. B 2009, 65B, 5–13. [Google Scholar] [CrossRef]
- Losada, A.; Márquez-González, M.; Knight, B.G.; Yanguas, J.; Sayegh, P.; Romero-Moreno, R. Psychosocial factors and caregivers’ distress: Effects of familism and dysfunctional thoughts. Aging Ment. Health 2010, 14, 193–202. [Google Scholar] [CrossRef]
- Sabogal, F.; Marín, G.; Otero-Sabogal, R.; Marín, B.V.; Perez-Stable, E.J. Hispanic Familism and Acculturation: What Changes and What Doesn’t? Hisp. J. Behav. Sci. 1987, 9, 397–412. [Google Scholar] [CrossRef]
- Mendez-Luck, C.A.; Anthony, K.P. Marianismoand Caregiving Role Beliefs Among U.S.-Born and Immigrant Mexican Women. J. Gerontol. Ser. B 2015, 71, 926–935. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Chakrabarti, S.; Grover, S. Gender differences in caregiving among family—Caregivers of people with mental illnesses. World J. Psychiatry 2016, 6, 7–17. [Google Scholar] [CrossRef]
- Losada, A.; Montorio, I.; Knight, B.; Márquez, M.; Izal, M. Explanation of caregivers distress from the cognitive model: The role of dysfunctional thoughts. Psicol. Conduct. 2006, 14, 115. [Google Scholar]
- Baron, R.S.; Cutrona, C.E.; Hicklin, D.; Russell, D.W.; Al, E. Social support and immune function among spouses of cancer patients. J. Pers. Soc. Psychol. 1990, 59, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Stefani, D.; Seidmann, S.; Pano, C.; Acrich, L.; Pupko, V.B. Los cuidadores familiares de enfermos crónicos: Sentimiento de soledad, aislamiento social y estilos de afrontamiento. Rev. Latinoam. Psicol. 2003, 35, 55–65. [Google Scholar]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index: A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md. State Med. J. 1965, 4, 61–65. [Google Scholar]
- Teri, L.; Truax, P.; Logsdon, R.; Uomoto, J.; Zarit, S.; Vitaliano, P.P. Assessment of behavioral problems in dementia: The revised memory and behavior problems checklist. Psychol. Aging 1992, 7, 622–631. [Google Scholar] [CrossRef]
- Losada, A.; Márquez-González, M.; Vara-García, C.; Barrera-Caballero, S.; Cabrera, I.; Gallego-Alberto, L.; Olmos, R.; Romero-Moreno, R. Measuring familism in dementia family caregivers: The revised familism scale. Aging Ment. Health 2019, 24, 784–788. [Google Scholar] [CrossRef]
- Losada, A.; Montorio, I.; Izal, M.; Márquez-González, M. Estudio e Intervencion Sobre el Malestar Psicológico de los Cuidadores de Personas con Demencia: El Papel de los Pensamientos Disfuncionales. Study and Intervention on Dementia Caregiving Distress: The Role of Dysfunctional Thoughts; IMSERSO: Madrid, Spain, 2006. [Google Scholar]
- Reig, A.; Ribera, D.; Miquel, J. Psychological support and daily stress in non-institutionalized elderly. Evaluación Psicológica 1991, 7, 191–200. [Google Scholar]
- Stevens, A.B.; Coon, D.; Wisniewski, S.; Vance, D.; Arguelles, S.; Belle, S.; Mendelsohn, A.; Ory, M.; Haley, W. Measurement of leisure time satisfaction in family caregivers. Aging Ment. Health 2004, 8, 450–459. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D Scale. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Cacioppo, J.T. A Short Scale for Measuring Loneliness in Large Surveys. Res. Aging 2004, 26, 655–672. [Google Scholar] [CrossRef]
- Losada, A.; Márquez-González, M.; García-Ortiz, L.; Gómez-Marcos, M.A.; Fernández-Fernández, V.; Rodríguez-Sánchez, E. Loneliness and Mental Health in a Representative Sample of Community-Dwelling Spanish Older Adults. J. Psychol. 2012, 146, 277–292. [Google Scholar] [CrossRef]
- Segel-Karpas, D.; Ayalon, L.; Lachman, M.E. Loneliness and depressive symptoms: The moderating role of the transition into retirement. Aging Ment. Health 2016, 22, 135–140. [Google Scholar] [CrossRef]
- Miller, B.; Guo, S. Social Support for Spouse Caregivers of Persons With Dementia. J. Gerontol. Ser. B 2000, 55, S163–S172. [Google Scholar] [CrossRef]
- Vikström, S.; Josephsson, S.; Stigsdotter-Neely, A.; Nygård, L. Engagement in activities: Experiences of persons with dementia and their caregiving spouses. Dementia 2008, 7, 251–270. [Google Scholar] [CrossRef]
- Robinson-Whelen, S.; Tada, Y.; Maccallum, R.C.; McGuire, L.; Kiecolt-Glaser, J.K. Long-term caregiving: What happens when it ends? J. Abnorm. Psychol. 2001, 110, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Yee, J.L.; Schulz, R. Gender Differences in Psychiatric Morbidity Among Family Caregivers. Gerontologist 2000, 40, 147–164. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, R.J.V. Gender differences in patterns of child–parent caregiving relationships. In Gender, Families, and Elder Care; Sage Focus Editions; Dwyer, J.W., Coward, R.T., Eds.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1992; Volume 138, pp. 65–83. [Google Scholar]
- Hanlon, N. Masculinities, Care and Equality: Identity and Nurture in Men’s Lives; Palgrave Macmillan: London, UK, 2012. [Google Scholar]
- Cheng, S.-T.; Au, A.; Losada, A.; Thompson, L.W.; Gallagher-Thompson, D. Psychological Interventions for Dementia Caregivers: What We Have Achieved, What We Have Learned. Curr. Psychiatry Rep. 2019, 21, 1–12. [Google Scholar] [CrossRef]
| Variables | 0. Daughters | 1. Wives | 2. Husbands | 3. Sons | F/χ2 (sig) | Diff. | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n = 117) | (n = 67) | (n = 56) | (n = 33) | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Age | 54.07 | 8.22 | 72.34 | 8.06 | 75.21 | 6.64 | 52.87 | 9.94 | 98.49 (0.00) | 1 & 2 > 0 & 3 |
| Loneliness never (%) | 43.5 | 46.2 | 57 | 48.5 | 10.75 (0.29) | n.s. | ||||
| Loneliness sometimes (%) | 30.8 | 22.3 | 19.6 | 24.2 | ||||||
| Loneliness occasionally (%) | 17.1 | 10.4 | 10.8 | 15.2 | ||||||
| Loneliness most or all of the time (%) | 8.5 | 20.1 | 12.5 | 12.2 | ||||||
| Work outside home (% yes) | 51.29 | 10.5 | 1.8 | 60.6 | 89.64 (0.00) | 0 & 3 > 1 & 2 | ||||
| Live with children (% yes) | 41.1 | 17.9 | 7.2 | 24.3 | 25.32 (0.00) | 0 > 1, 2 & 3 | ||||
| Care for other relatives (% yes) | 35.1 | 11.9 | 3.6 | 9.1 | 34.87 (0.00) | 0 > 1, 2 & 3 | ||||
| Hours of care | 11.1 | 8.46 | 16.1 | 7.50 | 16.59 | 7.44 | 8.68 | 9.16 | 12.04 | 0 & 3 < 1 & 2 |
| Frequency of disruptive behaviors | 37.21 | 13.98 | 32.31 | 12.23 | 32.89 | 11.42 | 31.93 | 11.17 | 2.78 (0.03) | 0 > 1, 2 & 3 |
| Functional capacity of person cared for | 61.96 | 27.77 | 71.65 | 26.17 | 7663 | 23.82 | 65.61 | 31.07 | 3.52 (0.01) | 0 < 1 & 2 |
| Family obligations | 6.39 | 3.51 | 10.00 | 4.12 | 9.82 | 4.55 | 8.60 | 3.52 | 13.02 (0.00) | 0 < 1, 2 & 3 |
| Dysfunctional thoughts | 19.03 | 11.12 | 34.78 | 15.47 | 37.98 | 12.18 | 25.06 | 12.29 | 27.94 (0.00) | 1 & 2 > 0 & 3 |
| Requesting help | 2.95 | 0.71 | 1.83 | 0.97 | 2.05 | 1.02 | 2.18 | 0.91 | 2.52 (0.04) | 0 > 1, 2 & 3 |
| Receiving help | 2.83 | 1.17 | 2.85 | 1.39 | 2.98 | 1.31 | 2.93 | 1.15 | 2.08 (0.08) | n.s |
| Social support | 11.52 | 3.68 | 11.13 | 3.72 | 10.77 | 4.57 | 8.72 | 3.95 | 3.34 (0.01) | 3 < 0, 1 & 2 |
| Leisure | 5.71 | 2.78 | 5.43 | 2.70 | 6.48 | 2.80 | 6.12 | 2.67 | 1.26 (0.29) | n.s |
| Daughters | |||||
| Unstandardized Estimates | S.E. | C.R. | |||
| Family obligations | → | Dysfunctional thoughts | 1.942 ** | 0.233 | 8.339 |
| Dysfunctional thoughts | → | Requesting help | −0.013 * | 0.006 | −2.269 |
| Requesting help | → | Receiving help | 0.614 ** | 0.147 | 4.183 |
| Receiving help | → | Social support | 0.855 ** | 0.284 | 3.008 |
| Dysfunctional thoughts | → | Leisure | −0.060 ** | 0.021 | −2.867 |
| Social support | → | Leisure | 0.282 ** | 0.063 | 4.492 |
| Leisure | → | Feeling of loneliness | −0.101 ** | 0.030 | −3.358 |
| Social support | → | Feeling of loneliness | −0.089 ** | 0.023 | −3.911 |
| Sons | |||||
| Unstandardized Estimates | S.E. | C.R. | |||
| Family obligations | → | Dysfunctional thoughts | 1.802 ** | 0.523 | 3.442 |
| Dysfunctional thoughts | → | Requesting help | 0.018 | 0.013 | 1.376 |
| Requesting help | → | Receiving help | 0.744 ** | 0.187 | 3.984 |
| Receiving help | → | Social support | 1.093 † | 0.572 | 1.910 |
| Dysfunctional thoughts | → | Leisure | −0.023 | 0.035 | −0.665 |
| Social support | → | Leisure | 0.251 * | 0.109 | 2.307 |
| Leisure | → | Feeling of loneliness | −0.214 ** | 0.066 | −3.256 |
| Social support | → | Feeling of loneliness | 0.026 | 0.044 | 0.587 |
| Wives | |||||
| Unstandardized Estimates | S.E. | C.R. | |||
| Family obligations | → | Dysfunctional thoughts | 1.992 ** | 0.392 | 5.076 |
| Dysfunctional thoughts | → | Requesting help | −0.020 ** | 0.007 | −2.722 |
| Requesting help | → | Receiving help | 0.842 ** | 0.147 | 5.710 |
| Receiving help | → | Social support | 0.580 † | 0.331 | 1.751 |
| Dysfunctional thoughts | → | Leisure | −0.065 ** | 0.020 | −3.300 |
| Social support | → | Leisure | 0.093 | 0.082 | 1.141 |
| Leisure | → | Feeling of loneliness | −0.069 | 0.054 | −1.265 |
| Social support | → | Feeling of loneliness | −0.015 | 0.039 | −0.394 |
| Husbands | |||||
| Unstandardized Estimates | S.E. | C.R. | |||
| Family obligations | → | Dysfunctional thoughts | 1.117 ** | 0.327 | 3.413 |
| Dysfunctional thoughts | → | Requesting help | −0.019 | 0.011 | −1.759 |
| Requesting help | → | Receiving help | 0.863 ** | 0.132 | 6.536 |
| Receiving help | → | Social support | 1.194 ** | 0.448 | 2.663 |
| Dysfunctional thoughts | → | Leisure | −0.050 | 0.029 | −1.745 |
| Social support | → | Leisure | 0.166 * | 0.077 | 2.170 |
| Leisure | → | Feeling of loneliness | −0.119 * | 0.050 | −2.394 |
| Social support | → | Feeling of loneliness | −0.042 | 0.030 | −1.397 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huertas-Domingo, C.; Márquez-González, M.; Cabrera, I.; Barrera-Caballero, S.; Pedroso-Chaparro, M.d.S.; Romero-Moreno, R.; Losada-Baltar, A. Sociocultural Influences on the Feeling of Loneliness of Family Caregivers of People with Dementia: The Role of Kinship. Int. J. Environ. Res. Public Health 2021, 18, 4700. https://doi.org/10.3390/ijerph18094700
Huertas-Domingo C, Márquez-González M, Cabrera I, Barrera-Caballero S, Pedroso-Chaparro MdS, Romero-Moreno R, Losada-Baltar A. Sociocultural Influences on the Feeling of Loneliness of Family Caregivers of People with Dementia: The Role of Kinship. International Journal of Environmental Research and Public Health. 2021; 18(9):4700. https://doi.org/10.3390/ijerph18094700
Chicago/Turabian StyleHuertas-Domingo, Cristina, María Márquez-González, Isabel Cabrera, Samara Barrera-Caballero, María del Sequeros Pedroso-Chaparro, Rosa Romero-Moreno, and Andrés Losada-Baltar. 2021. "Sociocultural Influences on the Feeling of Loneliness of Family Caregivers of People with Dementia: The Role of Kinship" International Journal of Environmental Research and Public Health 18, no. 9: 4700. https://doi.org/10.3390/ijerph18094700
APA StyleHuertas-Domingo, C., Márquez-González, M., Cabrera, I., Barrera-Caballero, S., Pedroso-Chaparro, M. d. S., Romero-Moreno, R., & Losada-Baltar, A. (2021). Sociocultural Influences on the Feeling of Loneliness of Family Caregivers of People with Dementia: The Role of Kinship. International Journal of Environmental Research and Public Health, 18(9), 4700. https://doi.org/10.3390/ijerph18094700





