The Influence of Increasing Levels of Provider-Patient Discussion on Quit Behavior: An Instrumental Variable Analysis of a National Survey
Abstract
1. Introduction
2. Methods
2.1. Data Sources and Study Population
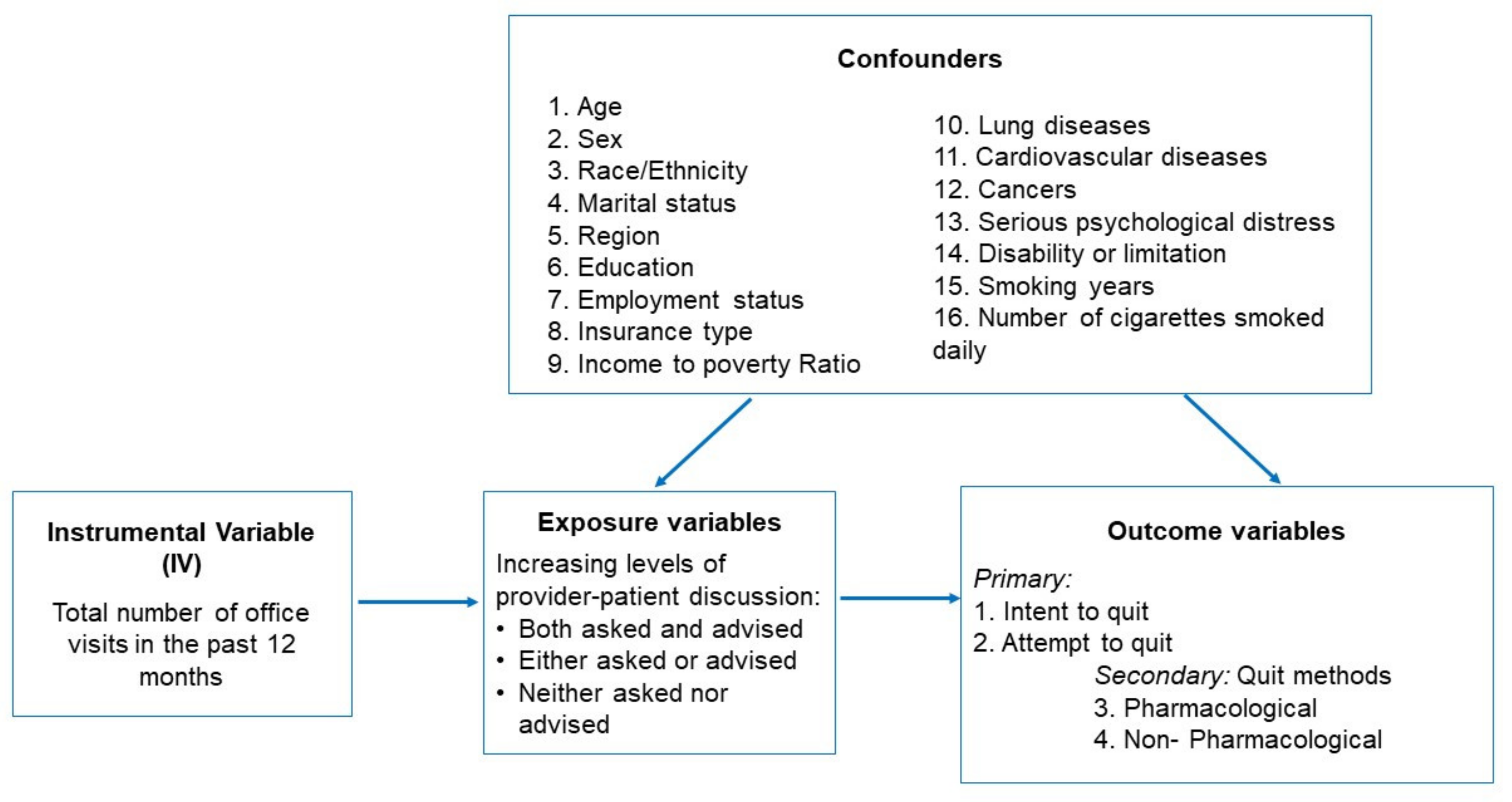
2.2. Outcome Variables
2.3. Exposure Variables
2.4. Covariates
2.5. Instrumental Variable
2.6. Statistical Analysis
2.6.1. Instrumental Variable (IV) Analysis
2.6.2. Sensitivity Analysis
3. Results
3.1. Sample Characteristics
3.2. Associations between Provider-Patient Discussion and Quit Behavior
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Public Health Service, Office of the Surgeon General. Smoking Cessation: A Report of the Surgeon General; U.S. Department of Health and Human Services: Rockville, MD, USA, 2020. Available online: https://www.hhs.gov/sites/default/files/2020-cessation-sgr-full-report.pdf (accessed on 31 January 2020).
- O’Connor, R.J. Non-cigarette tobacco products: What have we learnt and where are we headed? Tob. Control 2012, 21, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Toll, B.A.; Rojewski, A.M.; Duncan, L.R.; Latimer-Cheung, A.E.; Fucito, L.M.; Boyer, J.L.; Malley, S.S.; Salovey, P.; Herbst, R.S. “Quitting Smoking Will Benefit Your Health”: The Evolution of Clinician Messaging to Encourage Tobacco Cessation. Clin. Cancer Res. 2014, 20, 301. [Google Scholar] [CrossRef]
- Pacek, L.R.; Villanti, A.C.; McClernon, F.J. Not Quite the Rule, But No Longer the Exception: Multiple Tobacco Product Use and Implications for Treatment, Research, and Regulation. Nicotine Tob. Res. 2019, 22, 2114–2117. [Google Scholar] [CrossRef]
- Chase, E.C.; McMenamin, S.B.; Halpin, H.A. Medicaid Provider Delivery of the 5A’s for Smoking Cessation Counseling. Nicotine Tob. Res. 2007, 9, 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Huo, J.; Chung, T.H.; Kim, B.; Deshmukh, A.A.; Salloum, R.G.; Bian, J. Provider-Patient Discussions About Smoking and the Impact of Lung Cancer Screening Guidelines: NHIS 2011–2015. J. Gen. Intern. Med. 2020, 35, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Huo, J.; Hong, Y.-R.; Bian, J.; Guo, Y.; Wilkie, D.J.; Mainous, A.G. Low Rates of Patient-Reported Physician–Patient Discussion about Lung Cancer Screening among Current Smokers: Data from Health Information National Trends Survey. Cancer Epidemiol. Biomarks Prev. 2019, 28, 963–973. [Google Scholar] [CrossRef] [PubMed]
- Kruger, J.; Shaw, L.; Kahende, J.; Frank, E. Health care providers’ advice to quit smoking, National Health Interview Survey, 2000, 2005, and 2010. Prev. Chronic Dis. 2012, 9, E130. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tan, A.S.L.; Young-Wolff, K.C.; Carter-Harris, L.; Salloum, R.G.; Banerjee, S.C. Disparities in the Receipt of Tobacco Treatment Counseling within the US Context of the Affordable Care Act and Meaningful Use Implementation. Nicotine Tob. Res. 2018, 20, 1474–1480. [Google Scholar] [CrossRef]
- Bao, Y.; Duan, N.; Fox, S.A. Is some provider advice on smoking cessation better than no advice? An instrumental variable analysis of the 2001 National Health Interview Survey. Health Serv. Res. 2006, 41, 2114–2135. [Google Scholar] [CrossRef] [PubMed]
- Stanton, C.A.; Sharma, E.; Edwards, K.C.; Halenar, M.J.; Taylor, K.A.; Kasza, K.A.; Day, H.; Anic, G.; Gardner, L.D.; Hammad, H.T.; et al. Longitudinal transitions of exclusive and polytobacco electronic nicotine delivery systems (ENDS) use among youth, young adults and adults in the USA: Findings from the PATH Study Waves 1–3 (2013–2016). Tob. Control 2020, 29 (Suppl 3), s147. [Google Scholar] [CrossRef]
- Cokkinides, V.E.; Halpern, M.T.; Barbeau, E.M.; Ward, E.; Thun, M.J. Racial and Ethnic Disparities in Smoking-Cessation Interventions: Analysis of the 2005 National Health Interview Survey. Am. J. Prev. Med. 2008, 34, 404–412. [Google Scholar] [CrossRef]
- Lopez-Quintero, C.; Crum, R.M.; Neumark, Y.D. Racial/ethnic disparities in report of physician-provided smoking cessation advice: Analysis of the 2000 National Health Interview Survey. Am. J. Public Health 2006, 96, 2235–2239. [Google Scholar] [CrossRef]
- Henley, S.J.; Asman, K.; Momin, B.; Gallaway, M.S.; Culp, M.B.; Ragan, K.R.; Richards, T.B.; Babb, S. Smoking cessation behaviors among older U.S. adults. Prev. Med. Rep. 2019, 16, 100978. [Google Scholar] [CrossRef]
- Kruger, J.; O’Halloran, A.; Rosenthal, A.C.; Babb, S.D.; Fiore, M.C. Receipt of evidence-based brief cessation interventions by health professionals and use of cessation assisted treatments among current adult cigarette-only smokers: National Adult Tobacco Survey, 2009–2010. BMC Public Health 2016, 16, 141. [Google Scholar] [CrossRef]
- Quinn, V.P.; Hollis, J.F.; Smith, K.S.; Rigotti, N.A.; Solberg, L.I.; Hu, W.; Stevens, V.J. Effectiveness of the 5-As Tobacco Cessation Treatments in Nine HMOs. J. Gen. Intern. Med. 2008, 24, 149. [Google Scholar] [CrossRef] [PubMed]
- Quinn, V.P.; Stevens, V.J.; Hollis, J.F.; Rigotti, N.A.; Solberg, L.I.; Gordon, N.; Ritzwoller, D.; Smith, K.S.; Hu, W.; Zapka, J. Tobacco-Cessation Services and Patient Satisfaction in Nine Nonprofit HMOs. Am. J. Prev. Med. 2005, 29, 77–84. [Google Scholar] [CrossRef]
- King, B.A.; Dube, S.R.; Babb, S.D.; McAfee, T.A. Patient-reported recall of smoking cessation interventions from a health professional. Prev. Med. 2013, 57, 715–717. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Babb, S.; Schauer, G.; Asman, K.; Xu, X.; Malarcher, A. Cessation Behaviors and Treatment Use Among U.S. Smokers by Insurance Status, 2000–2015. Am. J. Prev. Med. 2019, 57, 478–486. [Google Scholar] [CrossRef]
- Malarcher, A.M.; Ford, E.S.; Nelson, D.E.; Chrismon, J.H.; Mowery, P.; Merritt, R.K.; Herman, W.H. Trends in Cigarette Smoking and Physicians’ Advice to Quit Smoking Among People with Diabetes in the U.S. Diabetes Care 1995, 18, 694. [Google Scholar] [CrossRef] [PubMed]
- Tong, E.K.; Ong, M.K.; Vittinghoff, E.; Pérez-Stable, E.J. Nondaily Smokers Should Be Asked and Advised to Quit. Am. J. Prev. Med. 2006, 30, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Coups, E.J.; Dhingra, L.K.; Heckman, C.J.; Manne, S.L. Receipt of Provider Advice for Smoking Cessation and Use of Smoking Cessation Treatments Among Cancer Survivors. J. Gen. Intern. Med. 2009, 24, 480. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tomar, S.L.; Husten, C.G.; Manley, M.W. Do dentists and physicians advise tobacco users to quit? J. Am. Dent. Assoc. 1996, 127, 259–265. [Google Scholar] [CrossRef]
- NCHS, National Health Interview Survey (NHIS). U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. 2016. Available online: https://www.cdc.gov/nchs/nhis/1997-2018.htm (accessed on 5 February 2020).
- Linda, M.; Collins, S.T.L. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences; Wiley: Hoboken, NJ, USA, 2009. [Google Scholar]
- Babb, S.; Malarcher, A.; Schauer, G.; Asman, K.; Jamal, A. Quitting Smoking Among Adults—United States, 2000–2015. MMWR Morb. Mortal W 2017, 65, 1457–1464. [Google Scholar] [CrossRef] [PubMed]
- Lousdal, M.L. An introduction to instrumental variable assumptions, validation and estimation. Emerg. Themes Epidemiol. 2018, 15, 1. [Google Scholar] [CrossRef] [PubMed]
- Rassen, J.A.; Schneeweiss, S.; Glynn, R.J.; Mittleman, M.A.; Brookhart, M.A. Instrumental Variable Analysis for Estimation of Treatment Effects with Dichotomous Outcomes. Am. J. Epidemiol. 2008, 169, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Rao, J.N.K.; Scott, A.J. On Simple Adjustments to Chi-Square Tests with Sample Survey Data. Ann. Stat. 1987, 15, 385–397. [Google Scholar] [CrossRef]
- Geraci, A.; Fabbri, D.; Monfardini, C. Testing Exogeneity of Multinomial Regressors in Count Data Models: Does Two Stage Residual Inclusion Work? J. Econom. Methods 2018, 7, 1–19. [Google Scholar] [CrossRef]
- Terza, J.V.; Basu, A.; Rathouz, P.J. Two-stage residual inclusion estimation: Addressing endogeneity in health econometric modeling. J. Health Econ. 2008, 27, 531–543. [Google Scholar] [CrossRef] [PubMed]
- Angrist, J.D.; Imbens, G.W.; Rubin, D.B. Identification of Causal Effects Using Instrumental Variables. J. Am. Stat. Assoc. 1996, 91, 444–455. [Google Scholar] [CrossRef]
- Stock, J.; Yogo, M. Testing for Weak Instruments in Linear IV Regression. In Identification and Inference for Econometric Models; Andrews, D.W.K., Ed.; Cambridge University Press: New York, NY, USA, 2005; pp. 80–108. [Google Scholar]
- Keele, L.; Zhao, Q.; Kelz, R.R.; Small, D. Falsification Tests for Instrumental Variable Designs with an Application to Tendency to Operate. Med. Care 2019, 57, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.R.; Rubin, D.B. The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70, 41–55. [Google Scholar] [CrossRef]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef]
- Austin, P.C.; Jembere, N.; Chiu, M. Propensity score matching and complex surveys. Stat. Methods Med. Res. 2016, 27, 1240–1257. [Google Scholar] [CrossRef] [PubMed]
- Ridgeway, G.; Kovalchik Stephanie, A.; Griffin Beth, A.; Kabeto Mohammed, U. Propensity Score Analysis with Survey Weighted Data. J. Causal Inference 2015, 3, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Gallaway, M.S.; Glover-Kudon, R.; Momin, B.; Puckett, M.; Lunsford, N.B.; Ragan, K.R.; Rohan, E.A.; Babb, S. Smoking cessation attitudes and practices among cancer survivors—United States, 2015. J. Cancer Surviv. 2019, 13, 66–74. [Google Scholar] [CrossRef]
- Villanti, A.C.; Johnson, A.L.; Ambrose, B.K.; Cummings, K.M.; Stanton, C.A.; Rose, S.W.; Feirman, S.P.; Tworek, C.; Glasser, A.M.; Pearson, J.L.; et al. Flavored Tobacco Product Use in Youth and Adults: Findings from the First Wave of the PATH Study (2013-2014). Am. J. Prev. Med. 2017, 53, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Aveyard, P.; Begh, R.; Parsons, A.; West, R. Brief opportunistic smoking cessation interventions: A systematic review and meta-analysis to compare advice to quit and offer of assistance. Addiction 2012, 107, 1066–1073. [Google Scholar] [CrossRef] [PubMed]
- Newhouse, M.B.M.J.P. Overview of the special supplement issue. Health Serv. Res. 2000, 35, 1061–1069. [Google Scholar]
- Huang, H.H.; Cagle, P.J., Jr.; Mazumdar, M.; Poeran, J. Statistics in Brief: Instrumental Variable Analysis: An Underutilized Method in Orthopaedic Research. Clin. Orthop. Relat. Res. 2019, 477, 1750–1755. [Google Scholar] [CrossRef] [PubMed]
- Hyland, A.; Kasza, K.A.; Borek, N.; Kimmel, H.L.; Taylor, K.A.; Compton, W.M.; Day, H.; Donaldson, E.A.; Sharma, E.; Anic, G.; et al. Overview of tobacco use transitions for population health. Tob. Control 2020, 29, S134–S138. [Google Scholar] [CrossRef] [PubMed]
- Vidrine, J.I.; Shete, S.; Cao, Y.; Greisinger, A.; Harmonson, P.; Sharp, B.; Miles, L.; Zbikowski, S.M.; Wetter, D.W. Ask-Advise-Connect: A new approach to smoking treatment delivery in health care settings. JAMA Intern. Med. 2013, 173, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.S.; Andrews, J.A.; Crews, K.M.; Payne, T.J.; Severson, H.H. The 5A’s vs 3A’s plus proactive quitline referral in private practice dental offices: Preliminary results. Tob. Control 2007, 16, 285–288. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, S.A. What to do with a patient who smokes. JAMA J. Am. Med. Assoc. 2005, 294, 482–487. [Google Scholar] [CrossRef] [PubMed]
- Kalkhoran, S.; Appelle, N.A.; Napoles, A.M.; Munoz, R.F.; Lum, P.J.; Alvarado, N.; Gregorich, S.E.; Satterfield, J.M. Beyond the Ask and Advise: Implementation of a Computer Tablet Intervention to Enhance Provider Adherence to the 5As for Smoking Cessation. J. Subst. Abus. Treat. 2016, 60, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Notley, C.; Gentry, S.; Livingstone-Banks, J.; Bauld, L.; Perera, R.; Hartmann-Boyce, J. Incentives for smoking cessation. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef] [PubMed]
| Levels of Discussion | Asked and Advised (n = 2219) | Asked or Advised (n = 735) | Neither Asked or Advised (n = 1179) | |
|---|---|---|---|---|
| Categorical Variables | N (weighted%) | N (weighted%) | N (weighted%) | p-value a |
| Sex | <0.001 | |||
| Female | 1202 (51.26) | 414 (55.2) | 563 (43.14) | |
| Male | 1017 (48.74) | 321 (44.8) | 616 (56.86) | |
| Race/Ethnicity | <0.001 | |||
| White Non-Hispanic | 1591 (78.09) | 490 (71.5) | 753 (65.36) | |
| Black Non-Hispanic | 310 (11.29) | 135 (15.58) | 150 (12.68) | |
| Hispanic | 197 (6.22) | 68 (8.88) | 172 (14.61) | |
| Others | 121 (4.4) | 42 (4.03) | 104 (7.34) | |
| Marital Status b | 0.007 | |||
| Yes | 958 (56.16) | 287 (50.36) | 464 (48.79) | |
| No | 1261 (43.84) | 448 (49.64) | 715 (51.21) | |
| Region | <0.001 | |||
| Northeast | 405 (19.07) | 95 (13.67) | 148 (12.23) | |
| Midwest | 535 (29.11) | 173 (24.47) | 305 (26.8) | |
| South | 772 (35.05) | 287 (41.69) | 408 (38.03) | |
| West | 507 (16.77) | 180 (20.18) | 318 (22.94) | |
| Education | 0.706 | |||
| Less than High School | 538 (24.03) | 205 (28.37) | 284 (25.3) | |
| High School Graduate | 598 (26.65) | 191 (26.69) | 300 (26.21) | |
| Some College | 519 (23.29) | 170 (22.93) | 292 (23.43) | |
| College or Above | 564 (26.03) | 169 (22.01) | 303 (25.07) | |
| Employment | <0.001 | |||
| Yes | 1083 (54.53) | 397 (56.79) | 737 (66.43) | |
| No | 1136 (45.47) | 338 (43.21) | 442 (33.57) | |
| Insurance | <0.001 | |||
| Private | 806 (44.17) | 288 (42.54) | 505 (47.36) | |
| Medicaid | 434 (17.54) | 153 (21.62) | 215 (17.18) | |
| Medicare | 555 (19.5) | 147 (17.61) | 134 (8.76) | |
| Others | 210 (8.56) | 52 (4.95) | 61 (5) | |
| Uninsured | 214 (10.23) | 95 (13.28) | 264 (21.7) | |
| Income/poverty ratio | 0.860 | |||
| <1.00 | 576 (19.42) | 191 (22.56) | 307 (21.51) | |
| 1.00–1.99 | 569 (23.92) | 194 (23.5) | 288 (23.14) | |
| 2.00–3.99 | 633 (31.27) | 206 (29.95) | 343 (31.71) | |
| 4.00 and over | 441 (25.38) | 144 (23.99) | 241 (23.65) | |
| Lung Disease c | <0.001 | |||
| Yes | 1279 (53.09) | 312 (38.24) | 386 (29.27) | |
| No | 940 (46.91) | 423 (61.76) | 793 (70.73) | |
| CVD d | <0.001 | |||
| Yes | 310 (12.07) | 65 (7.83) | 63 (4.29) | |
| No | 1909 (87.93) | 670 (92.17) | 1116 (95.72) | |
| Cancer e | <0.001 | |||
| Tobacco Related | 87 (3.09) | 17 (2.13) | 20 (0.93) | |
| Non-tobacco Related | 152 (6.3) | 43 (4.66) | 33 (2.68) | |
| None | 1980 (90.61) | 675 (93.21) | 1126 (96.39) | |
| Serious psychological distress f | <0.001 | |||
| Yes (Kessler score ≥ 13) | 272 (13.43) | 76 (9.69) | 82 (6.61) | |
| No (Kessler score < 13) | 1947 (86.57) | 659 (90.31) | 1097 (93.39) | |
| Disability/limitation g | <0.001 | |||
| Yes | 854 (31.38) | 196 (23.75) | 205 (12.9) | |
| No | 1365 (68.62) | 539 (76.25) | 974 (87.1) | |
| Continuous variables | Weighted Mean (SD) | Weighted Mean (SD) | Weighted Mean (SD) | p-value a |
| Age (years) | 47.69 (14.74) | 44.23 (15.9) | 40.88 (15.12) | <0.001 |
| Smoking length h (year) | 29.9 (15.19) | 26.06 (16.12) | 22.59 (15.37) | <0.001 |
| Number of cigarettes smoked daily | 13.37 (9.32) | 11.08 (9.25) | 9.57 (8.07) | <0.001 |
| Outcome Variable | Exposure Variable: Level of Discussion | Outcome Events/Total | Weighted % of Outcome Events | Odds Ratio (95% CI) |
|---|---|---|---|---|
| Intent to Quit (Yes vs. No) | Both Asked and Advised | 1611/2184 | 74% | 1.65 (1.63–1.66) Funding: |
| Either Asked or Advised | 479/727 | 66% | 1.02 (0.99–1.05) | |
| Neither | 726/1162 | 65% | Reference | |
| Attempt to Quit (Yes vs. No) | Both Asked and Advised | 1177/2219 | 54% | 1.76 (1.75–1.77) |
| Either Asked or Advised | 359/735 | 47% | 1.60 (1.57–1.63) | |
| Neither | 549/1179 | 46% | Reference | |
| Pharmacological quit methods (Yes vs. No) | Both Asked and Advised | 488/1177 | 40% | 1.99 (1.97–2.02) |
| Either Asked or Advised | 109/359 | 31% | 1.56 (1.49–1.63) | |
| Neither | 111/549 | 18% | Reference | |
| Non-pharmacological quit methods (Yes vs. No) | Both Asked and Advised | 137/1177 | 10% | 2.01 (1.94–2.08) |
| Either Asked or Advised | 32/359 | 11% | 2.91 (2.74–3.08) | |
| Neither | 24/549 | 4% | Reference |
| Outcome | Exposure Variable: Level of Discussion | Propensity Score Weighted Model ORs (95% CI) a | Multivariable Logistic Model OR (95% CI) b |
|---|---|---|---|
| Intent to Quit (Yes vs. No) | Both Asked and Advised | 1.74 (1.31–2.30) | 1.68 (1.32–2.14) |
| Either Asked or Advised | 1.04 (0.77–1.414) | 0.97 (0.75–1.25) | |
| Neither | Reference | Reference | |
| Attempt to Quit (Yes vs. No) | Both Asked and Advised | 1.88 (1.49–2.38) | 1.80 (1.47–2.21) |
| Either Asked or Advised | 1.24 (0.94–1.64) | 1.19 (0.92–1.55) | |
| Neither | Reference | Reference | |
| Pharmacological quit methods (Yes vs. No) | Both Asked and Advised | 2.01 (1.44–2.82) | 1.95 (1.41–2.70) |
| Either Asked or Advised | 1.72 (1.12–2.64) | 1.54 (1.00–2.36) | |
| Neither | Reference | Reference | |
| Non-pharmacological quit methods (Yes vs. No) | Both Asked and Advised | 1.92 (1.01–3.66) | 1.97 (0.97–3.99) |
| Either Asked or Advised | 2.57 (1.17–5.67) | 2.40 (1.09–5.30) | |
| Neither | Reference | Reference |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, B.; Zhan, S.; Wilson, K.M.; Mazumdar, M.; Li, L. The Influence of Increasing Levels of Provider-Patient Discussion on Quit Behavior: An Instrumental Variable Analysis of a National Survey. Int. J. Environ. Res. Public Health 2021, 18, 4593. https://doi.org/10.3390/ijerph18094593
Liu B, Zhan S, Wilson KM, Mazumdar M, Li L. The Influence of Increasing Levels of Provider-Patient Discussion on Quit Behavior: An Instrumental Variable Analysis of a National Survey. International Journal of Environmental Research and Public Health. 2021; 18(9):4593. https://doi.org/10.3390/ijerph18094593
Chicago/Turabian StyleLiu, Bian, Serena Zhan, Karen M. Wilson, Madhu Mazumdar, and Lihua Li. 2021. "The Influence of Increasing Levels of Provider-Patient Discussion on Quit Behavior: An Instrumental Variable Analysis of a National Survey" International Journal of Environmental Research and Public Health 18, no. 9: 4593. https://doi.org/10.3390/ijerph18094593
APA StyleLiu, B., Zhan, S., Wilson, K. M., Mazumdar, M., & Li, L. (2021). The Influence of Increasing Levels of Provider-Patient Discussion on Quit Behavior: An Instrumental Variable Analysis of a National Survey. International Journal of Environmental Research and Public Health, 18(9), 4593. https://doi.org/10.3390/ijerph18094593








