Predictors of Recurrent High Emergency Department Use among Patients with Mental Disorders
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting and Data Collection
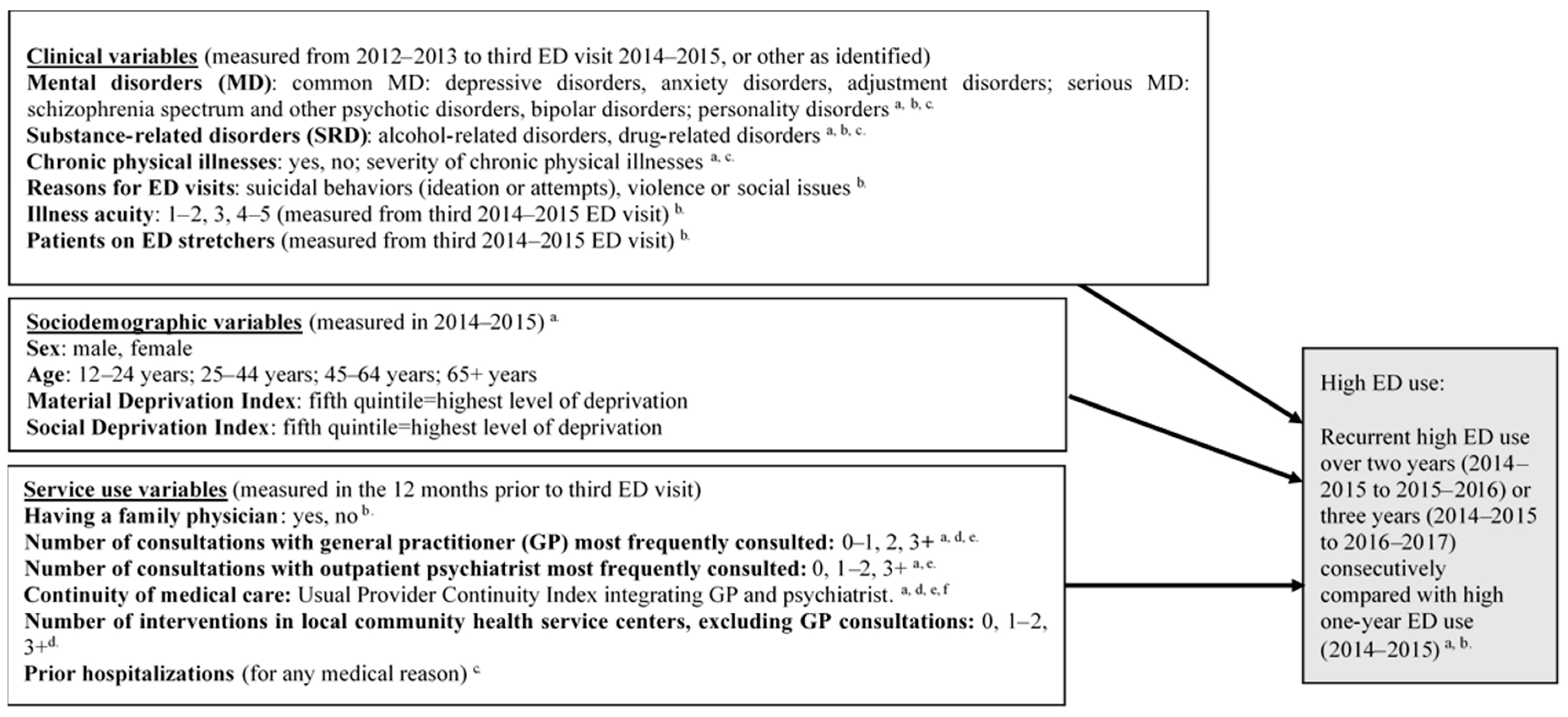
2.2. Variables
2.3. Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| BDCU | Emergency department database (Banque de données commune des urgences) |
| CLSC | Local community health service centers |
| ED | Emergency departments |
| GP | General practitioners |
| ICC | Intraclass correlation coefficient |
| ICD | International Classification of Diseases |
| I-CLSC | Public primary care database (Système d’information clinique et administrative des centres locaux de services communautaires) |
| MED-ÉCHO | Hospitalization database (Maintenance et exploitation des données pour l’étude de la clientèle hospitalière) |
| MD | Mental disorders |
| SRD | Substance-related disorders |
| RAMQ | Quebec Health Insurance Regime (Régie de l’assurance maladie du Québec) |
| VIF | Variance inflation factors |
References
- Bodenmann, P.; Baggio, S.; Iglesias, K.; Althaus, F.; Velonaki, V.S.; Stucki, S.; Ansermet, C.; Paroz, S.; Trueb, L.; Hugli, O.; et al. Characterizing the vulnerability of frequent emergency department users by applying a conceptual framework: A controlled, cross-sectional study. Int. J. Equity Health 2015, 14, 146. [Google Scholar] [CrossRef]
- Aagaard, J.; Aagaard, A.; Buus, N. Predictors of frequent visits to a psychiatric emergency room: A large-scale register study combined with a small-scale interview study. Int. J. Nurs. Stud. 2014, 51, 1003–1013. [Google Scholar] [CrossRef]
- Brennan, J.J.; Chan, T.C.; Hsia, R.Y.; Wilson, M.P.; Castillo, E.M. Emergency department utilization among frequent users with psychiatric visits. Acad. Emerg. Med. 2014, 21, 1015–1022. [Google Scholar] [CrossRef]
- Slankamenac, K.; Heidelberger, R.; Keller, D.I. Prediction of Recurrent Emergency Department Visits in Patients With Mental Disorders. Front. Psychiatry 2020, 11, 48. [Google Scholar] [CrossRef]
- McCarthy, M.L.; Zeger, S.L.; Ding, R.; Levin, S.R.; Desmond, J.S.; Lee, J.; Aronsky, D. Crowding delays treatment and lengthens emergency department length of stay, even among high-acuity patients. Ann. Emerg. Med. 2009, 54, 492–503.e4. [Google Scholar] [CrossRef]
- Bernstein, S.L.; Aronsky, D.; Duseja, R.; Epstein, S.; Handel, D.; Hwang, U.; McCarthy, M.; John McConnell, K.; Pines, J.M.; Rathlev, N.; et al. The effect of emergency department crowding on clinically oriented outcomes. Acad. Emerg. Med. 2009, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chang, G.; Weiss, A.P.; Orav, E.J.; Rauch, S.L. Predictors of frequent emergency department use among patients with psychiatric illness. Gen. Hosp. Psychiatry 2014, 36, 716–720. [Google Scholar] [CrossRef]
- Krieg, C.; Hudon, C.; Chouinard, M.C.; Dufour, I. Individual predictors of frequent emergency department use: A scoping review. BMC Health Serv. Res. 2016, 16, 594. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.A.; Tsai, W.C.; Chen, Y.C.; Hu, W.H.; Yang, D.Y. Factors associated with frequent use of emergency services in a medical center. J. Form. Med. Assoc. 2003, 102, 222–228. [Google Scholar]
- Billings, J.; Raven, M.C. Dispelling an urban legend: Frequent emergency department users have substantial burden of disease. Health Aff. (Millwood) 2013, 32, 2099–2108. [Google Scholar] [CrossRef]
- LaCalle, E.; Rabin, E. Frequent users of emergency departments: The myths, the data, and the policy implications. Ann. Emerg. Med. 2010, 56, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Mandelberg, J.H.; Kuhn, R.E.; Kohn, M.A. Epidemiologic analysis of an urban, public emergency department’s frequent users. Acad. Emerg. Med. 2000, 7, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Griswold, S.K.; Nordstrom, C.R.; Clark, S.; Gaeta, T.J.; Price, M.L.; Camargo, C.A., Jr. Asthma exacerbations in North American adults: Who are the “frequent fliers“ in the emergency department? Chest 2005, 127, 1579–1586. [Google Scholar] [CrossRef] [PubMed]
- Richard-Lepouriel, H.; Weber, K.; Baertschi, M.; DiGiorgio, S.; Sarasin, F.; Canuto, A. Predictors of recurrent use of psychiatric emergency services. Psychiatr. Serv. 2015, 66, 521–526. [Google Scholar] [CrossRef]
- Andrén, K.G.; Rosenqvist, U. Heavy users of an emergency department—A two year follow-up study. Soc. Sci. Med. 1987, 25, 825–831. [Google Scholar] [CrossRef]
- Rask, K.J.; Williams, M.V.; McNagny, S.E.; Parker, R.M.; Baker, D.W. Ambulatory health care use by patients in a public hospital emergency department. J. Gen. Intern. Med. 1998, 13, 614–620. [Google Scholar] [CrossRef]
- Hudon, C.; Courteau, J.; Krieg, C.; Vanasse, A. Factors associated with chronic frequent emergency department utilization in a population with diabetes living in metropolitan areas: A population-based retrospective cohort study. BMC Health Serv. Res. 2017, 17, 525. [Google Scholar] [CrossRef]
- Chiu, Y.M.; Vanasse, A.; Courteau, J.; Chouinard, M.C.; Dubois, M.F.; Dubuc, N.; Elazhary, N.; Dufour, I.; Hudon, C. Persistent frequent emergency department users with chronic conditions: A population-based cohort study. PLoS ONE 2020, 15, e0229022. [Google Scholar] [CrossRef]
- Saarento, O.; Hakko, H.; Joukamaa, M. Repeated use of psychiatric emergency out-patient services among new patients: A 3-year follow-up study. Acta. Psychiatr. Scand. 1998, 98, 276–282. [Google Scholar] [CrossRef]
- Vu, F.; Daeppen, J.B.; Hugli, O.; Iglesias, K.; Stucki, S.; Paroz, S.; Canepa Allen, M.; Bodenmann, P. Screening of mental health and substance users in frequent users of a general Swiss emergency department. BMC Emerg. Med. 2015, 15, 27. [Google Scholar] [CrossRef]
- Brunero, S.; Fairbrother, G.; Lee, S.; Davis, M. Clinical characteristics of people with mental health problems who frequently attend an Australian emergency department. Aust. Health Rev. 2007, 31, 462–470. [Google Scholar] [CrossRef]
- Fleury, M.J.; Rochette, L.; Grenier, G.; Huynh, C.; Vasiliadis, H.M.; Pelletier, E.; Lesage, A. Factors associated with emergency department use for mental health reasons among low, moderate and high users. Gen. Hosp. Psychiatry 2019, 60, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Poremski, D.; Kunjithapatham, G.; Koh, D.; Lim, X.Y.; Alexander, M.; Lee, C. Lost Keys: Understanding Service Providers‘ Impressions of Frequent Visitors to Psychiatric Emergency Services in Singapore. Psychiatr. Serv. 2017, 68, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Arfken, C.L.; Zeman, L.L.; Yeager, L.; White, A.; Mischel, E.; Amirsadri, A. Case-control study of frequent visitors to an urban psychiatric emergency service. Psychiatr. Serv. 2004, 55, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Gaulin, M.; Simard, M.; Candas, B.; Lesage, A.; Sirois, C. Combined impacts of multimorbidity and mental disorders on frequent emergency department visits: A retrospective cohort study in Quebec, Canada. CMAJ 2019, 191, E724–E732. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Canadian Association of Emergency Physicians. Canadian Triage Acuity Scale. Available online: https://caepca/wp-content/uploads/2017/06/module_I_slides_v25_2012pdf. (accessed on 23 January 2020).
- Pampalon, R.; Hamel, D.; Gamache, P. Health Inequalities, Deprivation, Immigration and Aboriginality in Canada: A Geographic Perspective. Can. J. Public Health 2010, 101, 470–474. [Google Scholar] [CrossRef]
- Rodriguez, H.P.; Marshall, R.E.; Rogers, W.H.; Safran, D.G. Primary care physician visit continuity: A comparison of patient-reported and administratively derived measures. J. Gen. Intern. Med. 2008, 23, 1499–1502. [Google Scholar] [CrossRef]
- Dreiher, J.; Comaneshter, D.S.; Rosenbluth, Y.; Battat, E.; Bitterman, H.; Cohen, A.D. The association between continuity of care in the community and health outcomes: A population-based study. Isr. J. Health Policy Res. 2012, 1, 21. [Google Scholar] [CrossRef]
- Hermann, R.C.; Chan, J.A.; Provost, S.E.; Chiu, W.T. Statistical benchmarks for process measures of quality of care for mental and substance use disorders. Psychiatr. Serv. 2006, 57, 1461–1467. [Google Scholar] [CrossRef]
- Hermann, R.C.; Mattke, S.; Somekh, D.; Silfverhielm, H.; Goldner, E.; Glover, G.; Pirkis, J.; Mainz, J.; Chan, J.A. Quality indicators for international benchmarking of mental health care. Int. J. Qual. Health Care 2006, 18 (Suppl. 1), 31–38. [Google Scholar] [CrossRef]
- Ionescu-Ittu, R.; McCusker, J.; Ciampi, A.; Vadeboncoeur, A.M.; Roberge, D.; Larouche, D.; Verdon, J.; Pineault, R. Continuity of primary care and emergency department utilization among elderly people. CMAJ 2007, 177, 1362–1368. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Window, Version 24.0; IBM Corp.: Armonk, NY, USA, 2015. [Google Scholar]
- Carleton, R.N.; Duranceau, S.; Freeston, M.H.; Boelen, P.A.; McCabe, R.E.; Antony, M.M. “But it might be a heart attack”: Intolerance of uncertainty and panic disorder symptoms. J. Anxiety Disord 2014, 28, 463–470. [Google Scholar] [CrossRef]
- Senn, N.; Cohidon, C.; Breton, M.; Levesque, J.F.; Zuchuat, J.C. Patterns of patient experience with primary care access in Australia, Canada, New Zealand and Switzerland: A comparative study. Int. J. Qual. Health Care 2019, 31, G126–G132. [Google Scholar] [CrossRef] [PubMed]
- Corscadden, L.; Levesque, J.F.; Lewis, V.; Strumpf, E.; Breton, M.; Russell, G. Factors associated with multiple barriers to access to primary care: An international analysis. Int. J. Equity Health 2018, 17, 28. [Google Scholar] [CrossRef] [PubMed]
- Ellison, J.M.; Blum, N.R.; Barsky, A.J. Frequent repeaters in a psychiatric emergency service. Hosp. Community Psychiatry 1989, 40, 958–960. [Google Scholar] [CrossRef] [PubMed]
- Amato, S.; Nobay, F.; Amato, D.P.; Abar, B.; Adler, D. Sick and unsheltered: Homelessness as a major risk factor for emergency care utilization. Am. J. Emerg. Med. 2019, 37, 415–420. [Google Scholar] [CrossRef]
- Cheung, A.; Somers, J.M.; Moniruzzaman, A.; Patterson, M.; Frankish, C.J.; Krausz, M.; Palepu, A. Emergency department use and hospitalizations among homeless adults with substance dependence and mental disorders. Addict. Sci. Clin. Pract. 2015, 10, 17. [Google Scholar] [CrossRef] [PubMed]
- Svoboda, T. Difficult behaviors in the emergency department: A cohort study of housed, homeless and alcohol dependent individuals. PLoS ONE 2014, 10, e0124528. [Google Scholar] [CrossRef]
- Bradley, K.A.; Kivlahan, D.R. Bringing patient-centered care to patients with alcohol use disorders. JAMA 2014, 311, 1861–1862. [Google Scholar] [CrossRef]
- Borg, B.; Douglas, I.S.; Hull, M.; Keniston, A.; Moss, M.; Clark, B.J. Alcohol misuse and outpatient follow-up after hospital discharge: A retrospective cohort study. Addict. Sci. Clin. Pract. 2018, 13, 24. [Google Scholar] [CrossRef] [PubMed]
- Barker, L.C.; Sunderji, N.; Kurdyak, P.; Stergiopoulos, V.; Gonzalez, A.; Kopp, A.; Vigod, S.N. Urgent Outpatient Care Following Mental Health ED Visits: A Population-Based Study. Psychiatr. Serv. 2020, 71, 616–619. [Google Scholar] [CrossRef]
- van Boekel, L.C.; Brouwers, E.P.; van Weeghel, J.; Garretsen, H.F. Comparing stigmatising attitudes towards people with substance use disorders between the general public, GPs, mental health and addiction specialists and clients. Int. J. Soc. Psychiatry 2015, 61, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.J.; Perreault, M.; Grenier, G.; Imboua, A.; Brochu, S. Implementing Key Strategies for Successful Network Integration in the Quebec Substance-Use Disorders Programme. Int. J. Integr. Care 2016, 16, 7. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.; Sanchez-Walker, E.; Evans, L.J.; Harris, V.; Pegler, R.; Cross, S. Characteristics of people who rapidly and frequently reattend the emergency department for mental health needs. Eur. J. Emerg. Med. 2016, 23, 351–355. [Google Scholar] [CrossRef]
- Kogstad, R.E.; Monness, E.; Sorensen, T. Social networks for mental health clients: Resources and solution. Community Ment. Health J. 2013, 49, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.J.; Grenier, G.; Bamvita, J.M.; Perreault, M.; Caron, J. Determinants associated with the utilization of primary and specialized mental health services. Psychiatr. Q 2012, 83, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.J.; Grenier, G.; Caron, J.; Lesage, A. Patients‘ report of help provided by relatives and services to meet their needs. Community Ment. Health J. 2008, 44, 271–281. [Google Scholar] [CrossRef]
- Fleury, M.J.; Grenier, G.; Vallee, C.; Aube, D.; Farand, L. Implementation of Integrated Service Networks under the Quebec Mental Health Reform: Facilitators and Barriers associated with Different Territorial Profiles. Int. J. Integr. Care 2017, 17, 3. [Google Scholar] [CrossRef]
- Fleury, M.J.; Grenier, G.; Vallee, C.; Aube, D.; Farand, L.; Bamvita, J.M.; Cyr, G. Implementation of the Quebec mental health reform (2005–2015). BMC Health Serv. Res. 2016, 16, 586. [Google Scholar] [CrossRef]
- van Boekel, L.C.; Brouwers, E.P.; van Weeghel, J.; Garretsen, H.F. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug Alcohol Depend. 2013, 131, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, L.; Nieweglowski, K.; Corrigan, P. The Stigma of Personality Disorders. Curr. Psychiatry Rep. 2016, 18, 11. [Google Scholar] [CrossRef] [PubMed]
- Marshall, K.L.; Deane, F.P. General practitioners‘ detection and management of patients with a dual diagnosis: Implications for education and training. Drug Alcohol Rev. 2004, 23, 455–462. [Google Scholar] [CrossRef]
- Loeb, D.F.; Bayliss, E.A.; Binswanger, I.A.; Candrian, C.; deGruy, F.V. Primary care physician perceptions on caring for complex patients with medical and mental illness. J. Gen. Intern. Med. 2012, 27, 945–952. [Google Scholar] [CrossRef]
- Jego, M.; Debaty, E.; Ouirini, L.; Carrier, H.; Beetlestone, E. Caring for patients with mental disorders in primary care: A qualitative study on French GPs‘ views, atittudes and needs. Fam. Pract. 2019, 36, 72–76. [Google Scholar] [CrossRef]
- Kisely, S.; Campbell, L.A. Taking consultation-liaison psychiatry into primary care. Int J. Psychiatry Med. 2007, 37, 383–391. [Google Scholar] [CrossRef]
- Stringer, B.; van Meijel, B.; Karman, P.; Koekkoek, B.; Kerkhof, A.J.; Beekman, A.T. Collaborative Care for Patients With Severe Personality Disorders: Analyzing the Execution Process in a Pilot Study (Part II). Perspect. Psychiatr. Care 2015, 51, 220–227. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, S.J.; Crowther, E.; Keating, C.; Kulkarni, J. What is needed to deliver collaborative care to address comorbidity more effectively for adults with a severe mental illness? Aust. N. Z. J. Psychiatry 2013, 47, 333–346. [Google Scholar] [CrossRef]
- Department of Health. No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy of All Ages; National Health Services: London, UK, 2011.
- Comnonwealht of Australia. Fourth National Mental Health Plan—An Agenda for Collaborative Government Action in Mental Health 2009–2004; Commonwealth of Australia, Autralian government: Canberra, Australia, 2009.
- Omer, S.; Priebe, S.; Giacco, D. Continuity across inpatient and outpatient mental health care or specialisation of teams? A systematic review. Eur. Psychiatry 2015, 30, 258–270. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Chakravarthy, B.; Yoon, J.; Snowden, L.; Bruckner, T.A. Psychiatric-related Revisits to the Emergency Department Following Rapid Expansion of Community Mental Health Services. Acad. Emerg. Med. 2019, 26, 1336–1345. [Google Scholar] [CrossRef]
- Mitton, C.R.; Adair, C.E.; McDougall, G.M.; Marcoux, G. Continuity of care and health care costs among persons with severe mental illness. Psychiatr. Serv. 2005, 56, 1070–1076. [Google Scholar] [CrossRef] [PubMed]
- Addington, D.; Anderson, E.; Kelly, M.; Lesage, A.; Summerville, C. Canadian Practice Guidelines for Comprehensive Community Treatment for Schizophrenia and Schizophrenia Spectrum Disorders. Can. J. Psychiatry 2017, 62, 662–672. [Google Scholar] [CrossRef] [PubMed]
- Moe, J.; Kirkland, S.W.; Rawe, E.; Ospina, M.B.; Vandermeer, B.; Campbell, S.; Rowe, B.H. Effectiveness of Interventions to Decrease Emergency Department Visits by Adult Frequent Users: A Systematic Review. Acad. Emerg. Med. 2017, 24, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Glover, G.; Arts, G.; Babu, K.S. Crisis resolution/home treatment teams and psychiatric admission rates in England. Br. J. Psychiatry 2006, 189, 441–445. [Google Scholar] [CrossRef] [PubMed]
| Diagnoses | International Classification of Diseases, Ninth Revision (ICD-9) | International Classification of Diseases, Tenth Revision, Canada (ICD-10-CA) |
|---|---|---|
| Schizophrenia spectrum and other psychotic disorders | 295, 297, 298 | F20, F21, F22, F23, F24, F25, F28, F29, F32.3, F33.3, F44.89 |
| Bipolar disorders | 296.0–296.6, 296.8, 296.9 | F30.0–F30.2, F30.8, F30.9, F31.0–F31.9 |
| Depressive disorders | 300.4, 311.9 | F32.0- F32.3, F32.8, F32.9, F33.0–F33.3, F33.8, F33.9, F34.8, F34.9, F38.0, F38.1, F38.8, F39, F41.2 |
| Anxiety disorders | 300 (except 300.4) | F40–F48, F68 |
| Personality disorders | 301 | F60, F07.0, F34.0, F341, F48.8, F61 |
| Adjustment disorders | 309.0–309.4, 309.8, 309.9 | F43.0–F43.2, F43.8, F43.9 |
| Alcohol-related disorders | 303.0, 303.9, 305.0 (alcohol abuse or dependence); 291, 357.5, 425.5, 535.3, 571.0–571.3 (alcohol-induced disorders); 980.0, 980.1, 980,8, 980.9 (alcohol intoxication) | F10.1, F10.2 (alcohol abuse or dependence); F10.3–F10.9, K70.0–K70.4, K70.9, G62.1, I42.6, K29.2, K85.2, K86.0, E24.4, G31.2, G72.1, O35.4 (alcohol-induced disorders); F10.0, T51.0, T51.1, T51.8, T51.9 (alcohol intoxication) |
| Drug-related disorders | 304.0–304.9, 305.2–305.7, 305.9 (drug abuse or dependence); 292 (drug-induced disorders); 965.0, 965.8, 967.0, 967.6, 967.8, 967.9, 969.4–969.9, 970.8, 982.0, 982.8 (drug intoxication) | F11.1, F12.1, F13.1, F14.1, F15.1, F16.1, F18.1, F19.1, F11.2, F12.2, F13.2, F14.2, F15.2, F16.2, F18.2, F19.2, F55 (drug abuse or dependence); F11.3–F11.9, F12.3–F12.9, F13.3–F13.9, F14.3–F14.9, F15.3–F15.9, F16.3–F16.9, F18.3–F18.9, F19.3–F19.9 (drug-induced MD); F11.0, F12.0, F13.0, F14.0, F15.0, F16.0, F18.0, F19.0, T40.0–T40.9, T42.3, T42.4, T42.6, T42.7, T43.5, T43.6, T43.8, T43.9, T50.9, T52.8, T52.9 (drug intoxication) |
| Characteristics Overall | Total High ED Users in 2014–2015 (Index Year) | High One-Year ED Users | Recurrent High ED Users for Two Consecutive Years (2014–2015 and 2015–2016) | Recurrent High ED Users for Three Consecutive Years (2014–2015 to 2016–2017) | p-Value |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | ||
| 3121 (100) | 2289 (100) | 468 (100) | 364 (100) | ||
| Clinical variables (2012–2013 to third ED visit in 2014–2015) or other, as specified | |||||
| Mental disorders (MD) a | |||||
| Common MD | |||||
| Depressive disorders | 1510 (48.4) | 1114 (48.7) | 220 (47.0) | 176 (48.4) | 0.807 |
| Anxiety disorders | 1740 (55.8) | 1239 (54.1) 3 | 260 (55.6) 3 | 241 (66.2) 1,2 | 0.000 |
| Adjustment disorders | 1347 (43.2) | 983 (42.9) | 207 (44.2) | 157 (43.1) | 0.877 |
| Serious MD | |||||
| Schizophrenia spectrum and other psychotic disorders | 1292 (41.4) | 926 (40.5) | 209 (44.7) | 157 (43.1) | 0.188 |
| Bipolar disorders | 1169 (37.5) | 850 (37.1) | 168 (35.9) | 151 (41.5) | 0.212 |
| Personality disorders | 913 (29.3) | 600 (26.2) 2,3 | 161 (34.4) 1,3 | 152 (41.8) 1,2 | 0.000 |
| Substance-related disorders (SRD) | |||||
| Alcohol-related disorders | 715 (22.9) | 478 (20.9) 3 | 116 (24.8) 3 | 121 (33.2) 1,2 | 0.000 |
| Drug-related disorders | 573 (18.4) | 373 (16.3) 2,3 | 94 (20.1) 1,3 | 106 (29.1) 1,2 | 0.000 |
| Chronic physical illnesses | 1563 (50.1) | 1089 (47.6) 3 | 244 (52.1) 3 | 230 (63.2) 1,2 | 0.000 |
| Elixhauser Comorbidity Index b | 0.025 | ||||
| 0 | 2331 (74.7) | 1738 (75.9)3 | 350 (74.8) | 243 (66.8) 1 | |
| 1 | 315 (10.1) | 222 (9.7) | 44 (9.4) | 49 (13.5) | |
| 2 | 200 (6.4) | 138 (6.0) | 32 (6.8) | 30 (8.2) | |
| 3+ | 275 (8.8) | 191 (8.3) | 42 (9.0) | 42 (11.5) | |
| Reasons for emergency department (ED) visits | |||||
| Suicidal behaviors (ideation or attempts) | 1401 (45.0) | 973 (42.6) 3 | 216 (46.2) 3 | 212 (58.4) 1,2 | 0.000 |
| Violence or social issues | 168 (5.4) | 109 (4.8) 3 | 21 (4.5) 3 | 38 (10.4) 1,2 | 0.000 |
| Illness acuity (triage priority levels) c | 0.154 | ||||
| Level 1–2 (immediate or very urgent care) | 525 (16.8) | 403 (17.6) | 66 (14.1) | 56 (15.4) | |
| Level 3 (urgent care) | 1000 (32.0) | 742 (32.4) | 141 (30.1) | 117 (32.1) | |
| Level 4–5 (less urgent or non-urgent care) | 1596 (51.1) | 1144 (50.0) | 261 (55.8) | 191 (52.5) | |
| ED patients on stretchers c | 1780 (57.0) | 1332 (58.2) 3 | 258 (55.1) | 190 (52.2) 1 | 0.067 |
| Sociodemographic variables (2014–2015) | |||||
| Age | 0.750 | ||||
| 12–24 years | 665 (21.3) | 478 (20.9) | 98 (20.9) | 89 (24.5) | |
| 25–44 years | 1166 (37.4) | 852 (37.2) | 182 (38.9) | 132 (36.3) | |
| 45–64 years | 887 (28.4) | 661 (28.9) | 131 (28.0) | 95 (26.1) | |
| 65+ years | 403 (12.9) | 298 (13.0) | 57 (12.2) | 48 (13.2) | |
| Sex | 0.174 | ||||
| Male | 1683 (53.9) | 1221 (53.3) | 249 (53.2) | 151 (41.5) | |
| Female | 1438 (46.1) | 1068 (46.7) | 219 (46.8) | 213 (58.5) | |
| Material Deprivation Index | 0.666 | ||||
| 1–2: least deprived | 1060 (34.0) | 788 (34.4) | 151 (32.3) | 121 (33.2) | |
| 3 | 570 (18.3) | 426 (18.6) | 82 (17.5) | 62 (17.0) | |
| 4–5: most deprived or not assigned d | 1491 (47.8) | 1075 (47.0) | 235 (50.2) | 181 (49.8) | |
| Social Deprivation Index | 0.039 | ||||
| 1–2: least deprived | 615 (19.7) | 469 (20.5) 3 | 92 (19.7) | 54 (14.8) 1 | |
| 3 | 409 (13.1) | 312 (13.6) | 56 (12.0) | 92 (19.7) | |
| 4–5: most deprived or not assigned d | 2097 (67.2) | 1508 (65.9)3 | 320 (68.4) | 269 (73.9) 1 | |
| Service use variables (12 months prior to third ED visit in 2014–2015) | |||||
| Having a family physician | 1469 (47.1) | 1067 (46.7) | 223 (47.6) | 179 (49.3) | 0.632 |
| Number of consultations with general practitioner (GP) most frequently consulted e | 0.894 | ||||
| 0 consultations | 634 (20.3) | 464 (20.3) | 97 (20.7) | 73 (20.1) | |
| 1–2 consultations | 731 (23.4) | 538 (23.5) | 114 (24.4) | 79 (21.7) | |
| 3+ consultations | 1756 (56.3) | 1287 (56.2) | 257 (54.9) | 212 (58.2) | |
| Number of consultations with psychiatrist most frequently consulted f | 0.002 | ||||
| 0 consultations | 1193 (38.2) | 913 (39.9) 3 | 174 (37.2) | 120 (33.0) 1 | |
| 1–2 consultations | 374 (12.0) | 274 (12.0) | 57 (12.2) | 43 (11.8) | |
| 3+ consultations | 1554 (49.8) | 1102 (48.1) 3 | 237 (50.6) | 201 (55.2) 1 | |
| Usual Provider Continuity Index integrating GP and psychiatrist g | |||||
| ≥0.80 | 580 (18.6) | 451 (19.7) 3 | 87 (18.6) 3 | 42 (11.5) 1,2 | 0.001 |
| Number of interventions in local community health service centers (excluding GP interventions) | 0.001 | ||||
| 0 interventions | 1784 (57.2) | 1337 (58.4) 3 | 272 (58.1) 3 | 175 (48.1) 1,2 | |
| 1–2 interventions | 600 (19.2) | 444 (19.4) | 79 (16.9) | 77 (21.2) | |
| 3+ interventions | 737 (23.6) | 508 (22.2) 3 | 117 (25.0) | 112 (30.8) 1 | |
| Prior hospitalizations (any medical reason) | 2082 (66.7) | 1479 (64.6) 3 | 321 (68.6) 3 | 282 (77.5) 1,2 | 0.000 |
| Recurrent High ED Use for Two Consecutive Years (2014–2015 and 2015–2016) | Recurrent High ED Use for Three Consecutive Years (2014–2015 to 2016–2017) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | β | p-Value | OR | 95% CI | β | p-Value | OR | 95% CI | ||
| Clinical variables (2012–2013 to third ED visit in 2014–2015, or other as specified) a,b | ||||||||||
| Mental disorders (MD) | ||||||||||
| Common MD | ||||||||||
| Anxiety disorders | 0.020 | 0.845 | 1.021 | 0.833 | 1.251 | 0.326 | 0.009 | 1.385 | 1.085 | 1.768 |
| Serious MD | ||||||||||
| Personality disorders | 0.367 | 0.001 | 1.443 | 1.153 | 1.805 | 0.352 | 0.006 | 1.422 | 1.107 | 1.827 |
| Substance-related disorders (SRD) | ||||||||||
| Alcohol-related disorders | 0.155 | 0.221 | 1.167 | 0.911 | 1.495 | 0.542 | 0.000 | 1.720 | 1.326 | 2.230 |
| Drug-related disorders | 0.170 | 0.214 | 1.186 | 0.906 | 1.551 | 0.596 | 0.000 | 1.814 | 1.379 | 2.387 |
| Chronic physical illnesses | 0.168 | 0.124 | 1.182 | 0.955 | 1.463 | 0.549 | 0.000 | 1.731 | 1.347 | 2.223 |
| Reasons for emergency department (ED) visits | ||||||||||
| Suicidal behaviors (ideation or attempts) | 0.120 | 0.263 | 1.128 | 0.914 | 1.392 | 0.604 | 0.000 | 1.826 | 1.433 | 2.335 |
| Violence or social issues | −0.047 | 0.852 | 0.955 | 0.586 | 1.555 | 0.837 | 0.000 | 2.310 | 1.505 | 3.544 |
| ED patients on stretchers c | −0.181 | 0.217 | 0.835 | 0.627 | 1.112 | −0.177 | 0.357 | 0.838 | 0.575 | 1.221 |
| Sociodemographic variables (2014–2015) | ||||||||||
| Social Deprivation Index (ref. 1–2: least deprived) | ||||||||||
| 3 | −0.076 | 0.682 | 0.927 | 0.644 | 1.334 | 0.154 | 0.498 | 1.167 | 0.747 | 1.823 |
| 4–5: most deprived or not assigned d | 0.098 | 0.458 | 1.102 | 0.852 | 1.426 | 0.468 | 0.005 | 1.597 | 1.155 | 2.208 |
| Service use variables (12 months prior to third ED visit) | ||||||||||
| Number of outpatient psychiatric consultations with usual medical provider; (ref.: 0 consultations) e | ||||||||||
| 1–2 consultations | 0.037 | 0.834 | 1.036 | 0.742 | 1.448 | 0.134 | 0.514 | 1.143 | 0.765 | 1.707 |
| 3+ consultations | 0.036 | 0.748 | 1.038 | 0.827 | 1.303 | 0.377 | 0.006 | 1.458 | 1.114 | 1.908 |
| Continuity of medical care: Usual Provider Continuity Index integrating GP and psychiatrist (≥0.8) f | −0.045 | 0.738 | 0.956 | 0.735 | 1.243 | −0.550 | 0.002 | 0.577 | 0.405 | 0.821 |
| Number of interventions in local community health service centers, excluding GP consultations; (ref.: 0) | ||||||||||
| 1–2 interventions | −0.242 | 0.109 | 0.785 | 0.584 | 1.055 | 0.027 | 0.872 | 1.027 | 0.743 | 1.419 |
| 3+ interventions | 0.048 | 0.639 | 1.049 | 0.828 | 1.328 | 0.298 | 0.028 | 1.347 | 1.033 | 1.757 |
| Prior hospitalizations (for any medical reason) | 0.134 | 0.267 | 1.144 | 0.902 | 1.450 | 0.309 | 0.037 | 1.362 | 1.018 | 1.823 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gentil, L.; Grenier, G.; Vasiliadis, H.-M.; Huỳnh, C.; Fleury, M.-J. Predictors of Recurrent High Emergency Department Use among Patients with Mental Disorders. Int. J. Environ. Res. Public Health 2021, 18, 4559. https://doi.org/10.3390/ijerph18094559
Gentil L, Grenier G, Vasiliadis H-M, Huỳnh C, Fleury M-J. Predictors of Recurrent High Emergency Department Use among Patients with Mental Disorders. International Journal of Environmental Research and Public Health. 2021; 18(9):4559. https://doi.org/10.3390/ijerph18094559
Chicago/Turabian StyleGentil, Lia, Guy Grenier, Helen-Maria Vasiliadis, Christophe Huỳnh, and Marie-Josée Fleury. 2021. "Predictors of Recurrent High Emergency Department Use among Patients with Mental Disorders" International Journal of Environmental Research and Public Health 18, no. 9: 4559. https://doi.org/10.3390/ijerph18094559
APA StyleGentil, L., Grenier, G., Vasiliadis, H.-M., Huỳnh, C., & Fleury, M.-J. (2021). Predictors of Recurrent High Emergency Department Use among Patients with Mental Disorders. International Journal of Environmental Research and Public Health, 18(9), 4559. https://doi.org/10.3390/ijerph18094559






