Medical Treatment Behaviour of the Elderly Population in Shanghai: Group Features and Influencing Factor Analysis
Abstract
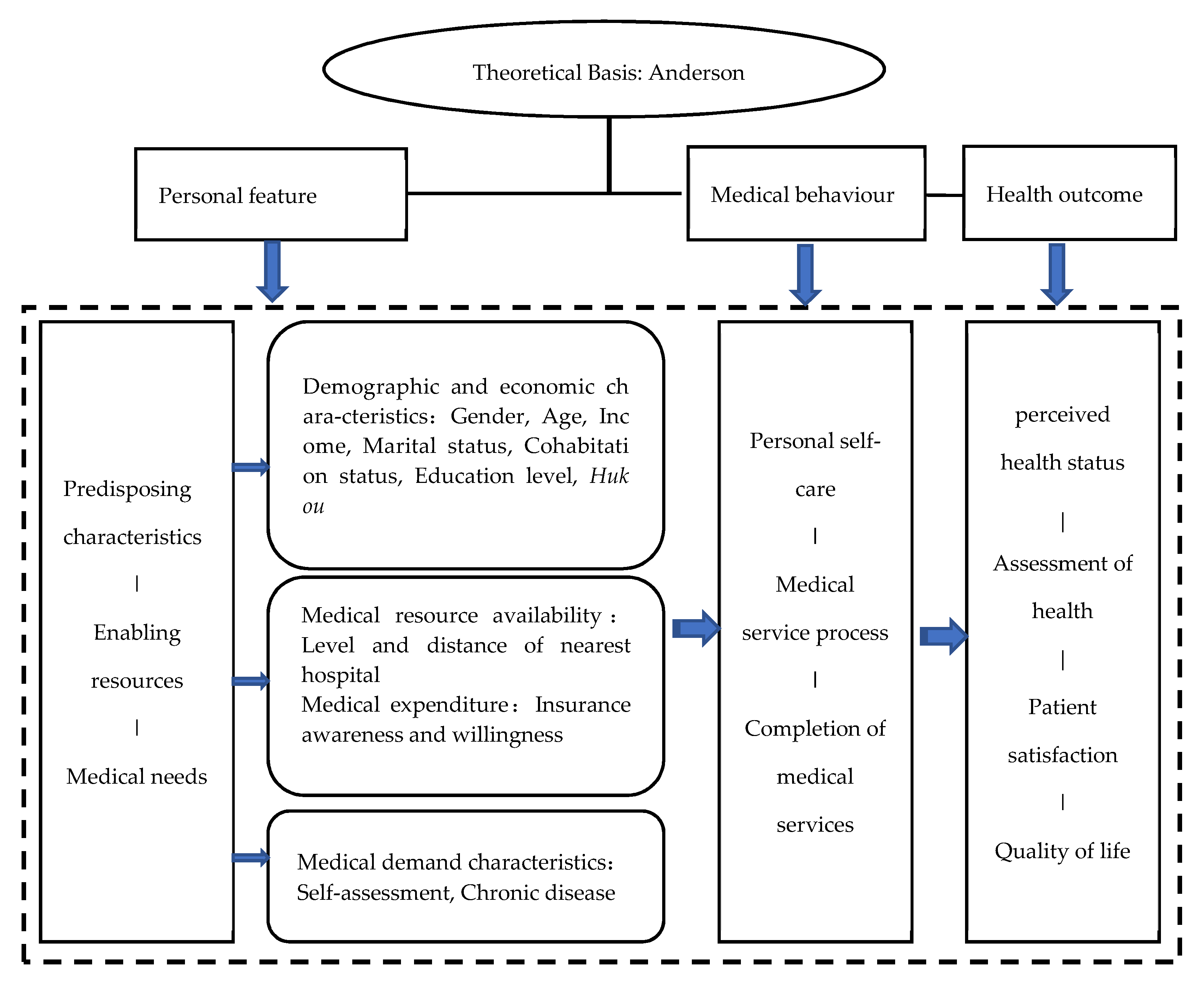
1. Introduction
2. Method
2.1. Study Population: Shanghai Elderly Medical Demand Characteristics Questionnaire
- Personal information in order to understand basic demographic characteristics (gender, age, marital status, and relationship);
- Hukou (the Hukou system is one of the major tools of social control employed by the state. The Chinese system was designed not merely to provide population statistics and identify personal status, but also to directly regulate the population distribution and serve many other important objectives desired by the state. If a person holds Shanghai hukou, it means he is a Shanghai native and enjoys institutional benefits within the Shanghainese jurisdiction. In terms of medical insurance, the gap between local hukou and non-local hukou in enjoying medical services is even more obvious. Shanghai clearly stipulates that the non-local hukou population cannot hold the medical insurance card for urban residents in Shanghai and therefore, they cannot enjoy Shanghai’s basic medical security rights) place and residential place;
- Socioeconomic status (education level, employment, and income);
- Health status in order to understand the reason for the medical service (self-evaluation of physical health and whether it involves chronic disease (common chronic diseases are mainly cardiovascular and cerebrovascular diseases, cancer, diabetes, chronic respiratory diseases, among which cardiovascular and cerebrovascular diseases include hypertension, stroke, and coronary heart disease);
- Medical preference and expectation in order to understand medical habits and behavioural choices;
- Satisfaction of hospitals and medical services in order to understand the current situation of the hospital and medical service supply; and
- Medical insurance mode and the level of success in using it in order to understand medical security status (whether basic medical insurance is held).
- (1)
- A number of districts in the city’s central area, suburbs, and outer suburban areas; then
- (2)
- A number of streets in each district; and then
- (3)
- Neighbourhood committees in each street.
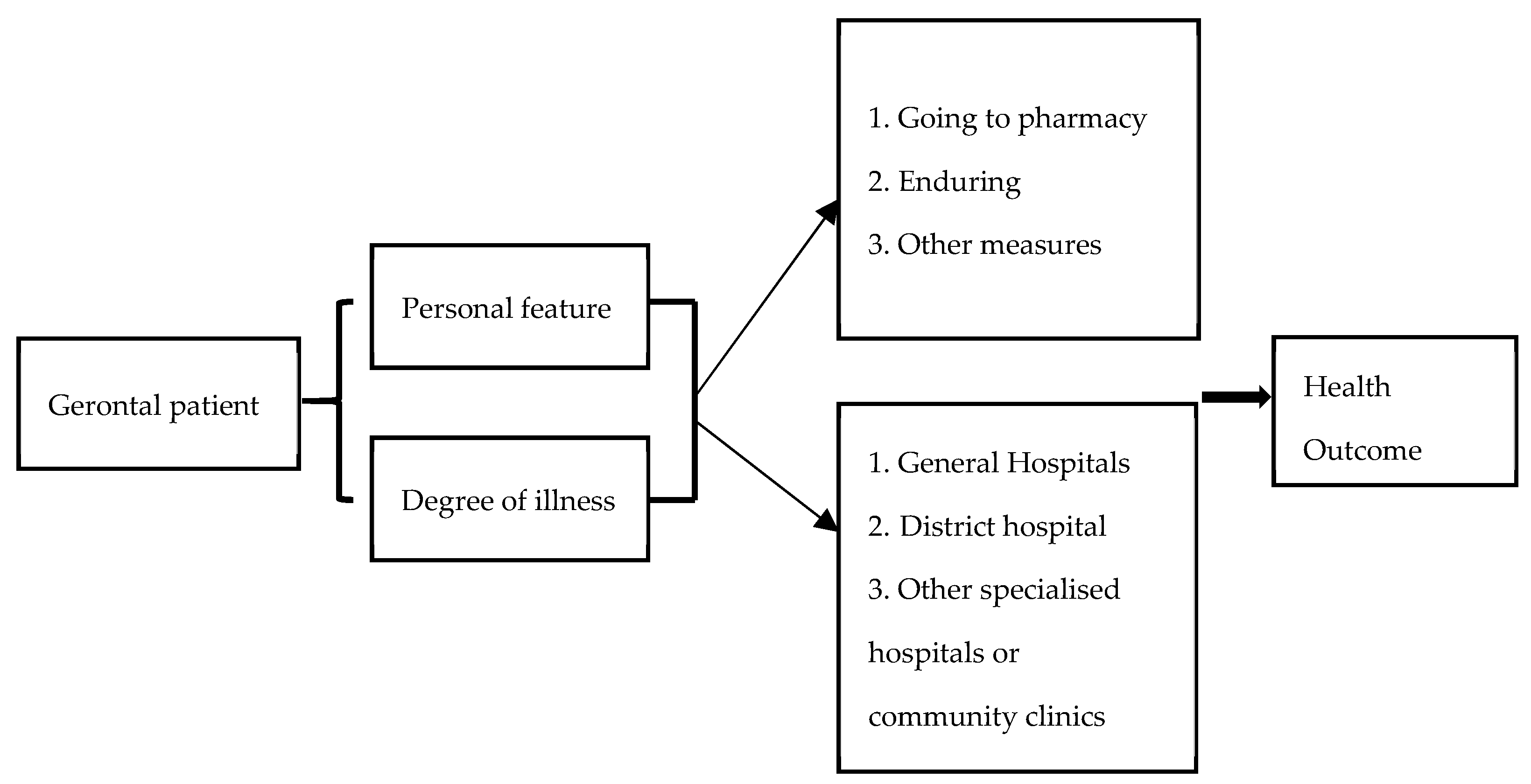
2.2. Dependent Variable
2.3. Independent Variables
2.4. Modelling and Estimation Methods
3. Results
3.1. Characteristics and Options
3.2. The Influencing Factors of Medical Treatment Choices for Physical Discomfort
3.3. The Influencing Factors of Medical Institution Choices in the Condition of General Disease and Severe Disease
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CHN | China |
| MLR | Multinomial Logistic Regression |
| CHNS | China Health and Nutrition Survey |
| NHS | National Health Service |
| IIA | Independence of Irrelevant Alternatives |
| MLE | Maximum Likelihood Estimation |
Appendix A
| Characteristics | General Disease | Severe Disease | ||||
|---|---|---|---|---|---|---|
| General Hospital N = 97 (22.10%) | District Hospital N = 163 (37.13%) | Specialised Hospitals or Community Clinic N = 179 (40.78%) | General Hospital N = 312 (71.07%) | District Hospital N = 65 (14.81%) | Specialised Hospitals or Community Clinic N = 62 (14.12%) | |
| Gender | ||||||
| Male | 46.83 | 34.22 | 32.23 | 35.71 | 40.40 | 31.52 |
| Female | 53.17 | 65.78 | 67.77 | 64.29 | 59.60 | 68.48 |
| Age | ||||||
| 60–64 years old | 30.16 | 29.33 | 28.21 | 28.34 | 28.28 | 33.70 |
| 65–69 years old | 36.50 | 30.67 | 29.31 | 33.64 | 30.31 | 20.65 |
| 70–74 years old | 14.29 | 19.11 | 22.34 | 18.66 | 21.21 | 21.74 |
| 75–79 years old | 5.50 | 13.78 | 9.52 | 8.53 | 11.11 | 17.39 |
| 80 years old and above | 13.49 | 7.11 | 10.62 | 10.83 | 9.09 | 6.52 |
| Income (retirement pension) | ||||||
| <1000 Yuan | 3.17 | 3.11 | 6.62 | 4.61 | 6.12 | 3.26 |
| 1000–1999 Yuan | 8.73 | 18.22 | 19.85 | 15.21 | 29.60 | 11.96 |
| 2000–2999 Yuan | 11.11 | 9.33 | 8.82 | 8.53 | 11.22 | 11.96 |
| 3000–3999 Yuan | 34.13 | 40.88 | 39.71 | 40.55 | 26.53 | 45.65 |
| 4000–4999 Yuan | 23.02 | 17.33 | 14.34 | 17.05 | 16.33 | 18.48 |
| 5000–5999 Yuan | 8.73 | 6.22 | 4.78 | 6.45 | 4.08 | 6.52 |
| 6000 Yuan and above | 11.11 | 4.89 | 5.88 | 7.60 | 6.12 | 2.17 |
| Marital status | ||||||
| Unmarried | 2.38 | 1.34 | 1.83 | 1.84 | 1.01 | 2.17 |
| Married | 75.40 | 81.69 | 82.42 | 79.91 | 85.86 | 79.35 |
| Divorced | 3.17 | 2.68 | 0.73 | 1.62 | 4.04 | 1.09 |
| Widowed | 19.05 | 14.29 | 15.02 | 16.63 | 9.09 | 17.39 |
| Cohabitation status | ||||||
| Living alone | 7.94 | 8.44 | 9.89 | 9.45 | 5.05 | 10.87 |
| Living with spouse | 47.62 | 46.22 | 52.38 | 47.93 | 56.57 | 46.75 |
| With elder (same generation) | 5.55 | 3.11 | 2.56 | 2.99 | 3.03 | 5.43 |
| With children | 30.95 | 28.45 | 23.81 | 26.27 | 27.27 | 30.43 |
| With three generations | 7.94 | 13.78 | 11.36 | 13.36 | 8.08 | 6.52 |
| Education level | ||||||
| Primary school and below | 14.40 | 23.56 | 21.98 | 19.17 | 32.32 | 17.39 |
| Middle school | 40.80 | 40.00 | 45.05 | 43.42 | 36.36 | 44.56 |
| High school or technical secondary school | 31.20 | 24.00 | 20.88 | 24.48 | 23.24 | 22.83 |
| Junior college | 13.60 | 12.44 | 12.09 | 12.93 | 8.08 | 15.22 |
| Rural or Urban | ||||||
| Urban | 96.83 | 89.29 | 84.50 | 89.84 | 79.59 | 93.41 |
| Rural | 3.17 | 10.71 | 15.50 | 10.16 | 20.41 | 6.59 |
| Shanghai Hukou | ||||||
| Yes | 96.00 | 95.11 | 94.83 | 94.47 | 94.90 | 98.89 |
| No | 4.00 | 4.89 | 5.17 | 5.53 | 5.10 | 1.11 |
| Health condition | ||||||
| Healthy | 53.97 | 40.63 | 42.49 | 42.49 | 45.46 | 50.00 |
| Basic level of health | 34.92 | 46.88 | 43.22 | 42.73 | 42.42 | 43.48 |
| Unhealthy | 11.11 | 12.49 | 14.29 | 14.78 | 12.12 | 6.52 |
| Chronic disease | ||||||
| no | 33.60 | 31.56 | 31.14 | 30.48 | 30.30 | 39.13 |
| Yes | 66.40 | 68.44 | 68.86 | 69.52 | 69.70 | 60.87 |
| The level of the subjectively nearest hospital from home | ||||||
| level-2 | 31.58 | 48.28 | 46.47 | 40.75 | 50.60 | 53.95 |
| level-3 | 68.42 | 51.72 | 53.53 | 59.25 | 49.40 | 46.05 |
| The subjective distance to the nearest hospital | ||||||
| <1 km | 2.83 | 9.04 | 6.63 | 5.64 | 13.33 | 4.41 |
| 1–2 km | 33.95 | 29.38 | 19.39 | 25.52 | 22.67 | 33.82 |
| 2–5 km | 39.62 | 35.59 | 38.27 | 39.76 | 26.67 | 39.71 |
| 5–10 km | 8.49 | 7.91 | 7.65 | 7.42 | 12.00 | 5.88 |
| 10 km and above | 15.09 | 18.08 | 28.06 | 21.66 | 25.33 | 16.18 |
| The level of the objectively nearest hospital from home | ||||||
| level-2 | 65.08 | 77.78 | 76.92 | 70.97 | 80.81 | 86.96 |
| level-3 | 34.92 | 22.22 | 23.08 | 29.03 | 19.19 | 13.04 |
| The objective distance to the nearest hospital | ||||||
| <1 km | 51.59 | 39.56 | 32.97 | 39.41 | 35.35 | 41.30 |
| 1–2 km | 30.16 | 36.00 | 30.03 | 35.48 | 24.24 | 26.09 |
| 2–5 km | 11.11 | 14.22 | 25.64 | 17.74 | 21.22 | 19.57 |
| 5 km and above | 7.14 | 10.22 | 11.36 | 7.37 | 19.19 | 13.04 |
| Understand medical insurance reimbursement policy | ||||||
| Yes | 66.67 | 70.40 | 67.77 | 70.44 | 58.59 | 70.33 |
| No | 33.33 | 29.60 | 32.23 | 29.56 | 41.41 | 29.67 |
| Prefer medical institutions with higher reimbursement rate | ||||||
| Yes | 33.33 | 35.71 | 43.95 | 37.79 | 45.45 | 37.36 |
| No | 38.10 | 33.93 | 28.21 | 32.72 | 33.33 | 28.57 |
| Not sure | 28.57 | 30.36 | 27.84 | 29.49 | 21.22 | 34.07 |
References
- Luo, J.; Zhang, X.; Jin, C.; Wang, D. Inequality of access to health care among the urban elderly in northwestern China. Health Policy 2009, 93, 111–117. [Google Scholar] [CrossRef]
- Qin, S.; Ding, Y. Why not see a doctor when ill? Evidence from the Chinese elderly. BMC Health Serv. Res. 2019, 19, 1–8. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Zhou, Y.; Wushouer, H.; Vuillermin, D.; Ni, B.; Guan, X.; Shi, L. Medical insurance and healthcare utilization among the middle-aged and elderly in China: Evidence from the China health and retirement longitudinal study 2011, 2013 and 2015. BMC Health Serv. Res. 2020, 20, 1–9. [Google Scholar] [CrossRef]
- Tian, Y.L.; Xiao, N.H.; Zhen, Z.Z. Identifying community healthcare supports for the elderly and the factors affecting their aging care model preference: Evidence from three districts of Beijing. BMC Health Serv. Res. 2016, 16, 83–92. [Google Scholar]
- Liu, Y. Annual Report on Elderly Health in China [2018]; Social Sciences Academic Press: Beijing, China, 2019. [Google Scholar]
- Shanghai Bureau of Statistics: The Present Situation of Population Aging in Shanghai. 2018. Available online: http://tjj.sh.gov.cn/tjfx/20181123/0014-1002033.html (accessed on 1 December 2018).
- Deb, P.; Trivedi, P.K. The structure of demand for health care: Latent class versus two-part models. J. Health Econ. 2002, 21, 601–625. [Google Scholar] [CrossRef]
- Thomas, C.P.; Ritter, G.; Wallack, S.S. Growth in prescription drug spending among insured elders. Health Aff. 2001, 20, 265–277. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.; Mao, Y. Intergenerational Support, Social Capital and Medical Service Utilization—An Empirical Analysis Using CHARSL Data. Soc. Secur. Stud. 2017, 3, 48–59. [Google Scholar]
- Wu, Z.; Hart, R. The effects of marital and nonmarital union transition on health. J. Marriage Fam. 2002, 64, 420–432. [Google Scholar] [CrossRef]
- Morris, S.; Sutton, M.; Gravelle, H. Inequity and inequality in the use of health care in England: An empirical investigation. Soc. Sci. Med. 2005, 60, 1251–1266. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, A. The demand for health: Some new empirical evidence. J. Health Econ. 1986, 5, 195–233. [Google Scholar] [CrossRef]
- Timmins, N. Letter from Britain: Across The Pond, Giant New Waves of Health Reform. Health Aff. 2010, 29, 2138–2141. [Google Scholar] [CrossRef]
- Altenstetter, C. Health Care Reform in Germany: Patchwork Change within Established Governance Structures. J. Health Politics Policy Law 2005, 30, 121–142. [Google Scholar] [CrossRef] [PubMed]
- Ham, C. Values and Health Policy: The Case of Singapore. J. Health Politics Policy Law 2001, 26, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.E. Origins of American Health Insurance; Yale University Press: New Haven, CT, USA; London, UK, 2007. [Google Scholar]
- Wang, F. Socioeconomic Status, Lifestyle and Health Inequality. Chin. J. Sociol. 2012, 32, 125–222. [Google Scholar]
- Xie, B.; Han, J.S. Impacts of Basic Medical Insurance on Household Expenditure in Urban and Rural China. J. Bus. Econ. 2015, 5, 79–87. [Google Scholar]
- David, R. Williams: Socioeconomic Differentials in Health: A Review and Redirection. Soc. Psychol. Q. 1990, 53, 81–99. [Google Scholar]
- MacKenbach, J.P.; Stirbu, I.; Roskam, A.-J.R.; Schaap, M.M.; Menvielle, G.; Leinsalu, M.; Kunst, A.E. Socioeconomic Inequalities in Health in 22 European Countries. N. Engl. J. Med. 2008, 358, 2468–2481. [Google Scholar] [CrossRef] [PubMed]
- Northridge, M.E.; Kumar, A.; Kaur, R. Disparities in Access to Oral Health Care. Annu. Rev. Public Health 2020, 41, 513–535. [Google Scholar] [CrossRef]
- Liu, J.; Wan, X. The Research on Government Payment Mechanism of Chinese Public Hospital. Chin. Health Econ. 2009, 28, 31–34. [Google Scholar]
- Liu, J.; Zhang, W. The thought on finance compensation for public hospital and the discussion on feasibility of the separated management of income and expenses. Health Econ. Res. 2007, 2, 11–13. [Google Scholar]
- Chen, Y.; Xu, S. Health Status, Welfare Demand and Prospects of Elderly Population in China. Popul. J. 2011, 2, 34–39. [Google Scholar]
- Song, M.; Yang, B.; Shi, T. Spatial Characteristics and Influencing Factors of Regional Differences in Basic Public Health Service Levels in China. Rev. Econ. Manag. 2014, 30, 133–141. [Google Scholar]
- Gu, S.; Wu, H.; Cao, D. Strategic Thinking on Rationalizing Aged Care Service System in China. Popul. Res. 2017, 41, 3–14. [Google Scholar]
- Yu, M.; He, S.; Wu, D.; Zhu, H.; Webster, C. Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China. Int. J. Environ. Res. Public Health 2019, 16, 2813. [Google Scholar] [CrossRef]
- Zhang, L.; Li, L. Study on the Equilibrium of Spatial Allocation of Medical Resources at Different Levels in Shanghai. Urban Dev. Stud. 2019, 26, 1–6. [Google Scholar]
- Bao, Y.; Tao, M.; Liu, W. Analysis on Intention of Visiting Doctor and Affecting Factors in Community Residents of Shanghai. Chin. J. Gen. Pract. 2009, 7, 551–554. [Google Scholar]
- Sun, M.; Han, H. Individuals’ First Health Care Choice in Rural China: Empirical Study Based on the Survey of Gansu, Henan and Guangdong Province. Econ. Rev. 2013, 2, 40–50. [Google Scholar]
- Gertler, P.; Locay, L.; Sanderson, W. Are user fees regressive? The welfare implications of health care financing proposals in Peru. J. Econom. 1987, 36, 67–88. [Google Scholar] [CrossRef]
- Gertler, P.; Gaag, J.V.D. The Willingness to Pay for Medical Care: Evidence from Two Developing Countries; Johns Hopkins University Press: Baltimore, MD, USA, 1990. [Google Scholar]
- Mwabu, G.; Ainsworth, M.; Nyamete, A. Quality of medical care and choice of medical treatment in Kenya: An empirical analysis. J. Hum. Resour. 1993, 28, 838–862. [Google Scholar] [CrossRef]
- Wang, J.; Chang, Z.; Liu, H. Health Care Demand and Choice of Medical Treatment. Econ. Res. J. 2008, 7, 105–117. [Google Scholar]
- China State Council. China’s Mid- and Long-Term Plan for the Prevention and Treatment of Chronic Diseases (2017–2025). Available online: www.gov.cn/zhengce/content/2017-02/14/content_5167886.htm?gs_ws=weixin_636366584577181978 (accessed on 12 December 2018).
- Andersen, R.; Newman, J.F. Societal and individual determinants of medical care utilization in the United States. The Milbank Memorial Fund Quarterly. Health Soc. 1973, 51, 95–124. [Google Scholar]
- Liao, X.; Luo, J.; Luo, Y. The Effect of Intergenerational Support on Medical Service Utilization among Rural Elderly—An Empirical from Hunan. Popul. Dev. 2017, 6, 87–95. [Google Scholar]
| Characteristics | Going to Hospital N = 284 (64.69%) | Going to Pharmacy N = 111 (25.28%) | Enduring N = 30 (6.83%) | Other Measures N = 14 (3.19%) |
|---|---|---|---|---|
| Gender | ||||
| Male | 36.16 | 38.16 | 25.53 | 36.00 |
| Female | 63.84 | 61.84 | 74.47 | 64.00 |
| Age | ||||
| 60–64 years old | 25.69 | 36.84 | 27.66 | 40.00 |
| 65–69 years old | 31.17 | 30.92 | 29.79 | 36.00 |
| 70–74 years old | 20.70 | 15.13 | 25.53 | - |
| 75–79 years old | 11.22 | 8.55 | 12.77 | 16.00 |
| 80 years old and above | 11.22 | 8.56 | 4.25 | 8.00 |
| Income (retirement pension) | ||||
| <1000 Yuan | 4.75 | 4.61 | 6.38 | - |
| 1000–1999 Yuan | 15.50 | 24.34 | 10.64 | 8.00 |
| 2000–2999 Yuan | 7.25 | 15.79 | 10.64 | 4.00 |
| 3000–3999 Yuan | 40.75 | 30.26 | 57.45 | 32.00 |
| 4000–4999 Yuan | 18.50 | 14.47 | 8.50 | 28.00 |
| 5000–5999 Yuan | 6.25 | 5.92 | 2.13 | 12.00 |
| 6000 Yuan and above | 7.00 | 4.61 | 4.26 | 16.00 |
| Marital status | ||||
| Unmarried | 0.25 | 3.31 | 2.13 | 16.00 |
| Married | 81.05 | 82.12 | - | - |
| Divorced | 2.49 | 1.32 | 80.85 | 68.00 |
| Widowed | 16.21 | 13.25 | 17.02 | 16.00 |
| Cohabitation status | ||||
| Living alone | 8.24 | 7.89 | 10.64 | 24.00 |
| Living with spouse | 51.87 | 46.05 | 42.55 | 36.00 |
| With elder (same generation) | 2.74 | 2.64 | 8.51 | 8.00 |
| With children | 26.68 | 26.97 | 29.79 | 28.00 |
| With three generations | 10.47 | 16.45 | 8.51 | 4.00 |
| Education level | ||||
| Primary school and below | 19.00 | 27.63 | 19.15 | 16.00 |
| Middle school | 43.75 | 42.76 | 40.43 | 24.00 |
| High school or technical secondary school | 25.50 | 19.08 | 21.28 | 36.00 |
| Junior college | 11.75 | 10.53 | 19.14 | 24.00 |
| Rural or Urban | ||||
| Urban | 89.45 | 84.21 | 95.74 | 92.00 |
| Rural | 10.55 | 15.79 | 4.26 | 8.00 |
| Shanghai Hukou | ||||
| Yes | 97.49 | 90.73 | 93.62 | 88.00 |
| No | 2.51 | 9.27 | 6.38 | 12.00 |
| Health condition | ||||
| Healthy | 42.00 | 53.29 | 29.79 | 48.00 |
| Basic level of health | 45.00 | 33.55 | 51.06 | 48.00 |
| Unhealthy | 13.00 | 13.16 | 19.15 | 4.00 |
| Chronic disease | ||||
| No | 28.00 | 38.82 | 27.66 | 56.00 |
| Yes | 72.00 | 61.18 | 72.34 | 44.00 |
| The level of the subjectively nearest hospital from home | ||||
| level-2 | 42.78 | 48.23 | 41.03 | 42.11 |
| level-3 | 57.22 | 51.77 | 58.97 | 57.89 |
| The subjective distance to the nearest hospital | ||||
| <1 km | 5.71 | 6.90 | 8.83 | 20.00 |
| 1–2 km | 27.31 | 28.45 | 11.76 | 20.00 |
| 2–5 km | 37.78 | 31.90 | 58.83 | 33.33 |
| 5–10 km | 8.57 | 6.03 | 8.83 | 6.67 |
| 10 km and above | 20.63 | 26.72 | 11.76 | 20.00 |
| The level of the objectively nearest hospital from home | ||||
| level-2 | 75.31 | 73.03 | 76.60 | 76.00 |
| level-3 | 24.69 | 26.97 | 23.40 | 24.00 |
| The objective distance to the nearest level-3 hospital | ||||
| <1 km | 37.40 | 40.13 | 55.32 | 28.00 |
| 1–2 km | 33.67 | 29.61 | 25.53 | 40.00 |
| 2–5 km | 16.96 | 22.37 | 17.02 | 24.00 |
| 5 km and above | 11.97 | 7.89 | 2.13 | 8.00 |
| Understand medical insurance reimbursement policy | ||||
| Yes | 66.17 | 65.79 | 87.23 | 88.00 |
| No | 33.83 | 34.21 | 12.77 | 12.00 |
| Prefer medical institutions with higher reimbursement rate | ||||
| Yes | 39.25 | 42.76 | 29.79 | 28.00 |
| No | 32.75 | 30.92 | 31.91 | 32.00 |
| Not sure | 28.00 | 26.32 | 38.30 | 40.00 |
| Characteristics | Going to Pharmacy | Enduring | Other Measures | |||
|---|---|---|---|---|---|---|
| Odds Ratio | 95%CI | Odds Ratio | 95%CI | Odds Ratio | 95%CI | |
| Demographic and economic characteristics: | ||||||
| Gender | ||||||
| Male | Reference | Reference | Reference | |||
| Female | 0.76 | (0.40, 1.45) | 0.65 | (0.21, 2.01) | 0.90 | (0.07, 11.05) |
| Age | ||||||
| 60–64 years old | Reference | Reference | Reference | |||
| 65–69 years old | 0.72 | (0.37, 1.38) | 0.64 | (0.18, 2.18) | 0.25 | (0.02, 2.9) |
| 70–74 years old | 0.46 * | (0.20, 1.06) | 0.61 | (0.15, 2.46) | 0.74 | (0.05, 11.87) |
| 75–79 years old | 0.59 | (0.22, 1.55) | 1.32 | (0.27, 6.53) | 0.00 | (0.00, .) |
| 80 years old and above | 0.27 ** | (0.09, 0.88) | 0.17 | (0.01, 2.20) | 0.19 | (0.00, 10.77) |
| Income(retirement pension) | ||||||
| <1000 Yuan | Reference | Reference | Reference | |||
| 1000–1999 Yuan | 6.92 ** | (1.20, 39.97) | 1.68 | (0.07, 40.69) | 7.25 × 106 | (0.00, .) |
| 2000–2999 Yuan | 2.02 | (0.35, 11.73) | 2.45 | (0.11, 53.73) | 2.70 × 107 | (0.00, .) |
| 3000–3999 Yuan | 1.07 | (0.20, 5.79) | 1.80 | (0.09, 36.34) | 7.41 × 108 | (0.00, .) |
| 4000–4999 Yuan | 1.06 | (0.18, 6.31) | 0.62 | (0.02, 16.46) | 7.32 × 108 | (0.00, .) |
| 5000–5999 Yuan | 1.10 | (0.17, 7.29) | 0.52 | (0.01, 19.53) | 7.23 × 109 | (0.00, .) |
| 6000 Yuan and above | 0.78 | (0.11, 5.76) | 0.68 | (0.02, 21.91) | 2.09 × 109 | (0.00, .) |
| Marital status | ||||||
| Unmarried | 17.85 ** | (1.37, 232.55) | 0.00 | (0, .) | 13.71 | (0.11, 1739.55) |
| Married | Reference | Reference | Reference | |||
| Divorced | 0.15 | (0.02, 1.48) | 0.00 | (0.00, .) | 0.00 | (0.00, .) |
| Widowed | 0.99 | (0.35, 2.77) | 0.61 | (0.09, 4.27) | 0.15 | (0.00, 7.09) |
| Cohabitation status | ||||||
| Living alone | 1.31 | (0.36, 4.83) | 4.70 | (0.50, 44.18) | 97.47 ** | (2.70, 3518.98) |
| Living with spouse | Reference | Reference | Reference | |||
| With elder (same generation) | 0.96 | (0.18, 5.16) | 2.01 | (0.22, 18.67) | 4.99 | (0.1, 253.48) |
| With children | 1.25 | (0.65, 2.41) | 0.73 | (0.20, 2.67) | 3.83 | (0.5, 29.16) |
| With three generations | 1.18 | (0.51, 2.71) | 0.71 | (0.16, 3.23) | 0.00 | (0.00, .) |
| Education level | ||||||
| Primary school and below | Reference | Reference | Reference | |||
| Middle school | 0.72 | (0.33, 1.57) | 0.44 | (0.10, 1.92) | 0.37 | (0.01, 9.86) |
| High school or technical secondary school | 0.47 | (0.19, 1.20) | 0.69 | (0.14, 3.41) | 0.37 | (0.01, 10.31) |
| Junior college | 0.83 | (0.27, 2.59) | 1.27 | (0.18, 8.99) | 1.61 | (0.03, 75.17) |
| Rural or Urban | ||||||
| Urban | 1.02 | (0.18, 5.61) | 1.01 | (0.03, 36.54) | 0.04 | (0.00, 390.24) |
| Rural | Reference | Reference | Reference | |||
| Shanghai Hukou | ||||||
| Yes | 0.11 *** | (0.02, 0.49) | 0.06 ** | (0.00, 0.68) | 4080.37 | (0.00, .) |
| No | Reference | Reference | Reference | |||
| Medical demand characteristics: | ||||||
| Health condition | ||||||
| Healthy | Reference | Reference | Reference | |||
| Basic level of health | 1.04 | (0.60, 1.81) | 1.07 | (0.37, 3.07) | 1.95 | (0.30, 12.51) |
| Unhealthy | 1.15 | (0.51, 2.59) | 2.23 | (0.63, 7.94) | 5.35 | (0.18, 156.41) |
| Chronic disease | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 0.54 ** | (0.31, 0.93) | 0.74 | (0.26, 2.09) | 0.11 ** | (0.02, 0.84) |
| Medical resource availability: | ||||||
| The level of the subjectively nearest hospital from home | ||||||
| level-2 | Reference | Reference | Reference | |||
| level-3 | 0.57 | (0.06, 5.23) | 0.00 | (0.00, .) | 0.04 | (0.00,21.82) |
| The subjective distance to the nearest hospital | ||||||
| Distance from Level-3 hospital <1 km | Reference | Reference | Reference | |||
| 1–2 km | 0.66 | (0.10, 4.53) | 1.36 × 107 | (0.00, .) | 0.04 | (0.00, 52.06) |
| 2–5 km | 0.91 | (0.14, 5.76) | 5.24 × 107 | (0.00, .) | 1.04 | (0.00, 326.2) |
| 5–10 km | 0.31 | (0.04, 2.59) | 1.21 × 107 | (0.00, .) | 0.00 | (0.00, .) |
| 10 km and above | 0.51 | (0.06, 3.99) | 2.45 × 107 | (0.00, .) | 3.66 | (0.01, 1371.82) |
| Distance from Level-2 hospital <1 km | Reference | Reference | Reference | |||
| 1–2 km | 0.93 | (0.24, 3.55) | 0.00 | (0.00, .) | 0.01 ** | (0.00, 0.48) |
| 2–5 km | 0.31 | (0.07, 1.48) | 1.62 | (0.18, 14.39) | 0.00 ** | (0.00, 0.57) |
| 5–10 km | 0.27 | (0.02, 3.94) | 44.07* | (0.66, 2920.79) | 37.07 | (0.09, 14,913.39) |
| 10 km and above | 0.22 * | (0.04, 1.32) | 2.11 | (0.08, 55.02) | 0.06 | (0.00, 6.64) |
| The level of the objectively nearest hospital from home | ||||||
| level-2 | Reference | Reference | Reference | |||
| level-3 | 1.36 | (0.44, 4.15) | 1.09 | (0.20, 6.10) | 0.00 | (0.00, .) |
| The objective distance to the nearest level-3 hospital | ||||||
| Distance from Level-3 hospital <1 km | Reference | Reference | Reference | |||
| 1–2 km | 0.75 | (0.21, 2.65) | 0.31 | (0.03, 2.82) | 2.17 × 107 | (0.00, .) |
| 2–5 km | 0.56 | (0.07, 4.56) | 0.16 | (0.00, 5.72) | 2.91 × 107 | (0.00, .) |
| 5 km and above | 0.00 | (0.00, .) | 0.00 | (0.00, .) | 1.84 × 106 | (0.00, .) |
| Distance from Level-2 hospital <1 km | Reference | Reference | Reference | |||
| 1–2 km | 0.85 | (0.36, 2.00) | 0.15 ** | (0.03, 0.76) | 1.11 | (0.07, 18.32) |
| 2–5 km | 1.97 | (0.54, 7.18) | 0.05 * | (0.00, 1.13) | 1.28 | (0.04, 37.65) |
| 5 km and above | 0.16** | (0.03, 0.91) | 0.09 | (0.00, 2.70) | 0.00 | (0.00, .) |
| Medical expenditure: | ||||||
| Understand medical insurance reimbursement policy | ||||||
| Yes | 0.87 | (0.50, 1.52) | 0.26 ** | (0.07, 0.93) | 0.16 | (0.01, 2.00) |
| No | Reference | Reference | Reference | |||
| Prefer medical institutions with higher reimbursement rate | ||||||
| Yes | Reference | Reference | Reference | |||
| No | 0.96 | (0.52, 1.77) | 1.48 | (0.44, 4.95) | 0.70 | (0.05, 10.24) |
| Not sure | 0.86 | (0.46, 1.62) | 2.37 | (0.77, 7.31) | 7.86 * | (0.92, 67.02) |
| Constant | 20.51 ** | (1.02, 411.47) | 11.11 | (0.06, 2029.61) | 0.00 | (0.00, .) |
| Observations | 439 | 439 | 439 | |||
| r2_p | 0.219 | 0.219 | 0.219 | |||
| General Disease | Severe Disease | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | District Hospital | Other Specialised Hospitals or Community Clinics | District Hospital | Other Specialised Hospitals or Community Clinics | ||||
| Odds Ratio | 95%CI | Odds Ratio | 95%CI | Odds Ratio | 95%CI | Odds Ratio | 95%CI | |
| Demographic and economic characteristics: | ||||||||
| Gender | ||||||||
| Male | Reference | Reference | Reference | Reference | ||||
| Female | 1.73 | (0.82, 3.67) | 1.37 | (0.64, 2.90) | 1.59 | (0.72, 3.49) | 0.97 | (0.42, 2.21) |
| Age | ||||||||
| 60–64 years old | Reference | Reference | Reference | Reference | ||||
| 65–69 years old | 0.65 | (0.30, 1.40) | 0.54 | (0.25, 1.17) | 0.73 | (0.31, 1.71) | 0.55 | (0.23, 1.31) |
| 70–74 years old | 1.68 | (0.65, 4.31) | 1.98 | (0.77, 5.12) | 1.31 | (0.49, 3.5) | 0.92 | (0.34, 2.48) |
| 75–79 years old | 2.83 * | (0.87, 9.24) | 1.43 | (0.41, 4.97) | 2.95* | (0.88, 9.92) | 1.48 | (0.47, 4.65) |
| 80 years old and above | 0.77 | (0.21, 2.85) | 1.42 | (0.41, 4.84) | 2.14 | (0.58, 7.95) | 0.26 | (0.04, 1.75) |
| Income (retirement pension) | ||||||||
| <1000 Yuan | Reference | Reference | Reference | Reference | ||||
| 1000–1999 Yuan | 0.54 | (0.04, 8.09) | 0.47 | (0.03, 7.24) | 0.21 * | (0.03, 1.23) | 1.27 × 106 | (0.00, .) |
| 2000–2999 Yuan | 0.27 | (0.02, 3.46) | 0.19 | (0.01, 2.59) | 0.13 * | (0.02, 1.06) | 2.53 × 106 | (0.00, .) |
| 3000–3999 Yuan | 0.71 | (0.06, 8.79) | 0.76 | (0.06, 9.82) | 0.43 | (0.07, 2.52) | 1.88 × 106 | (0.00, .) |
| 4000–4999 Yuan | 0.47 | (0.04, 6.01) | 0.40 | (0.03, 5.39) | 0.26 | (0.04, 1.72) | 1.02 × 106 | (0.00, .) |
| 5000–5999 Yuan | 0.32 | (0.02, 4.45) | 0.27 | (0.02, 3.97) | 0.07 ** | (0.01, 0.71) | 6.80 × 106 | (0.00, .) |
| 6000 Yuan and above | 0.39 | (0.03, 5.81) | 0.31 | (0.02, 4.89) | 0.36 | (0.04, 3.11) | 1.19 × 105 | (0.00, .) |
| Marital status | ||||||||
| Unmarried | 0.67 | (0.06, 7.20) | 1.14 | (0.09, 15.29) | 0.64 | (0.04, 10.97) | 1.08 | (0.13, 8.90) |
| Married | Reference | Reference | Reference | Reference | ||||
| Divorced | 0.18** | (0.03, 0.98) | 0.11 ** | (0.01, 0.78) | 3.23 | (0.58, 17.89) | 0.45 | (0.04, 4.61) |
| Widowed | 0.42 | (0.13, 1.33) | 0.60 | (0.19, 1.94) | 0.55 | (0.14, 2.22) | 0.88 | (0.26, 3.02) |
| Cohabitation status | ||||||||
| Living alone | 2.18 | (0.52, 9.19) | 2.26 | (0.55, 9.19) | 0.91 | (0.17, 4.8) | 1.43 | (0.32, 6.32) |
| Living with spouse | Reference | Reference | Reference | Reference | ||||
| With elder (same generation) | 1.22 | (0.25, 6.02) | 0.30 | (0.05, 1.92) | 1.27 | (0.12, 13.07) | 2.02 | (0.43, 9.61) |
| With children | 2.29** | (1.04, 5.07) | 1.28 | (0.57, 2.85) | 1.45 | (0.6, 3.47) | 1.30 | (0.58, 2.93) |
| With three generations | 2.59* | (0.89, 7.55) | 2.15 | (0.72, 6.44) | 0.30 * | (0.08, 1.07) | 1.20 | (0.36, 4.08) |
| Education level | ||||||||
| Primary school and below | Reference | Reference | Reference | Reference | ||||
| Middle school | 0.87 | (0.32, 2.35) | 1.55 | (0.56, 4.24) | 0.77 | (0.30, 1.95) | 0.99 | (0.32, 3.03) |
| High school or technical secondary school | 0.70 | (0.24, 2.05) | 0.87 | (0.29, 2.62) | 0.90 | (0.30, 2.71) | 0.80 | (0.22, 2.90) |
| Junior college | 1.07 | (0.30, 3.85) | 1.29 | (0.34, 4.81) | 1.13 | (0.30, 4.27) | 2.18 | (0.54, 8.72) |
| Rural or Urban | ||||||||
| Urban | 0.33 | (0.03, 3.21) | 0.59 | (0.06, 5.78) | 0.17 * | (0.02, 1.28) | 6.18 | (0.47, 81.41) |
| Rural | Reference | Reference | Reference | Reference | ||||
| Hukou | ||||||||
| Yes | 0.58 | (0.07, 5.02) | 0.52 | (0.06, 4.75) | 0.46 | (0.08, 2.64) | 2.65 × 106 | (0.00, .) |
| No | Reference | Reference | Reference | Reference | ||||
| Medical demand characteristics: | ||||||||
| Health condition | ||||||||
| Healthy | Reference | Reference | Reference | Reference | ||||
| Basic level of health | 2.12 ** | (1.10, 4.06) | 1.79 * | (0.93, 3.46) | 1.24 | (0.62, 2.48) | 0.97 | (0.50, 1.88) |
| Unhealthy | 1.30 | (0.48, 3.49) | 1.62 | (0.61, 4.30) | 0.99 | (0.35, 2.75) | 0.09 ** | (0.01, 0.80) |
| Chronic disease | ||||||||
| No | Reference | Reference | Reference | Reference | ||||
| Yes | 0.95 | (0.49, 1.84) | 0.72 | (0.37, 1.39) | 1.31 | (0.63, 2.73) | 0.67 | (0.33, 1.34) |
| Medical resource availability: | ||||||||
| The level of the subjectively nearest hospital from home | ||||||||
| level-2 | Reference | Reference | Reference | Reference | ||||
| level-3 | 0.00 | (0.00, .) | 0.00 | (0.00, .) | 2.29 | (0.18, 29.03) | 4.23 | (0.15, 123.22) |
| The subjective distance to the nearest hospital | ||||||||
| Distance from Level-3 hospital <1 km | Reference | Reference | Reference | Reference | ||||
| 1–2 km | 1.42 | (0.16, 12.62) | 0.44 | (0.05, 3.72) | 0.05 ** | (0.00, 0.67) | 0.32 | (0.02, 4.58) |
| 2–5 km | 1.46 | (0.17, 12.27) | 1.01 | (0.13, 7.71) | 0.07 ** | (0.01, 0.73) | 0.37 | (0.03, 4.88) |
| 5–10 km | 0.92 | (0.09, 9.55) | 0.35 | (0.04, 3.47) | 0.13 | (0.01, 1.66) | 0.24 | (0.01, 4.46) |
| 10 km and above | 1.27 | (0.12, 13.23) | 0.70 | (0.07, 6.62) | 0.16 | (0.01, 1.94) | 0.07 * | (0.00, 1.54) |
| Distance from Level-2 hospital <1 km | Reference | Reference | Reference | Reference | ||||
| 1–2 km | 0.00 | (0.00, .) | 0.00 | (0.00, .) | 0.24 ** | (0.06, 0.96) | 3.23 | (0.34, 31.2) |
| 2–5 km | 0.00 | (0.00, .) | 0.00 | (0.00, .) | 0.12 ** | (0.02, 0.61) | 1.51 | (0.13, 16.96) |
| 5–10 km | 0.00 | (0.00, .) | 0.00 | (0.00, .) | 5.05 | (0.30, 84.72) | 0.00 | (0.00, .) |
| 10 km and above | 0.00 | (0.00, .) | 0.00 | (0.00, .) | 0.17 * | (0.02, 1.24) | 1.62 | (0.11, 23.88) |
| The level of the objectively nearest hospital from home | ||||||||
| level-2 | Reference | Reference | Reference | Reference | ||||
| level-3 | 0.32 * | (0.1, 1) | 0.19 ** | (0.05, 0.73) | 0.00 | (0.00, .) | 1.21 | (0.31, 4.72) |
| The objective distance to the nearest level hospital | ||||||||
| Distance from Level-3 hospital <1 km | Reference | Reference | Reference | Reference | ||||
| 1–2 km | 3.21 * | (0.88, 11.70) | 5.17 ** | (1.2, 22.32) | 4.65 × 106 | (0.00, .) | 0.63 | (0.13, 2.99) |
| 2–5 km | 6.10 | (0.40, 94.03) | 44.85 *** | (2.78, 724.03) | 4.42 × 106 | (0.00, .) | 0.00 | (0.00, .) |
| 5 km and above | 10.78 | (0.00, .) | 0.00 | (0.00, .) | 1.58 × 1016 | (0.00, .) | 2.58 × 106 | (0.00, .) |
| Distance from Level-2 hospital <1 km | Reference | Reference | Reference | Reference | ||||
| 1–2 km | 2.60 * | (0.97, 6.99) | 2.30 | (0.84, 6.32) | 0.81 | (0.28, 2.37) | 1.59 | (0.58, 4.30) |
| 2–5 km | 1.18 | (0.25, 5.49) | 3.35 * | (0.81, 13.88) | 0.42 | (0.06, 3.18) | 4.59 ** | (1.00, 20.96) |
| 5 km and above | 4.49 | (0.57, 35.40) | 6.52 * | (0.82, 51.57) | 0.76 | (0.09, 6.43) | 3.36 | (0.40, 28.24) |
| Medical expenditure: | ||||||||
| Understand medical insurance reimbursement policy | ||||||||
| Yes | 1.10 | (0.56, 2.16) | 1.20 | (0.61, 2.34) | 1.68 | (0.85, 3.29) | 1.78 | (0.83, 3.80) |
| No | Reference | Reference | Reference | Reference | ||||
| Prefer medical institutions with higher reimbursement rate | ||||||||
| Yes | Reference | Reference | Reference | Reference | ||||
| No | 0.76 | (0.37, 1.57) | 0.46 ** | (0.22, 0.95) | 1.30 | (0.63, 2.69) | 0.85 | (0.38, 1.93) |
| Not sure | 0.76 | (0.35, 1.61) | 0.62 | (0.29, 1.31) | 0.53 | (0.23, 1.23) | 1.37 | (0.63, 2.98) |
| Constant | 3.82 × 107 | (0.00, .) | 2.59 × 107 | (0.00, .) | 18.82 * | (0.61, 581.28) | 0.00 | (0.00, .) |
| Observations | 439 | 439 | 439 | 439 | ||||
| r2_p | 0.147 | 0.147 | 0.21 | 0.21 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, S.; Wang, D.; Li, C.; Wang, C.; Wang, M. Medical Treatment Behaviour of the Elderly Population in Shanghai: Group Features and Influencing Factor Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4108. https://doi.org/10.3390/ijerph18084108
Yang S, Wang D, Li C, Wang C, Wang M. Medical Treatment Behaviour of the Elderly Population in Shanghai: Group Features and Influencing Factor Analysis. International Journal of Environmental Research and Public Health. 2021; 18(8):4108. https://doi.org/10.3390/ijerph18084108
Chicago/Turabian StyleYang, Shangguang, Danyang Wang, Chen Li, Chunlan Wang, and Mark Wang. 2021. "Medical Treatment Behaviour of the Elderly Population in Shanghai: Group Features and Influencing Factor Analysis" International Journal of Environmental Research and Public Health 18, no. 8: 4108. https://doi.org/10.3390/ijerph18084108
APA StyleYang, S., Wang, D., Li, C., Wang, C., & Wang, M. (2021). Medical Treatment Behaviour of the Elderly Population in Shanghai: Group Features and Influencing Factor Analysis. International Journal of Environmental Research and Public Health, 18(8), 4108. https://doi.org/10.3390/ijerph18084108






