Occurrence of Delirium during ECMO Therapy in a Critical Care Unit in Poland—A Cross-Sectional Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Setting
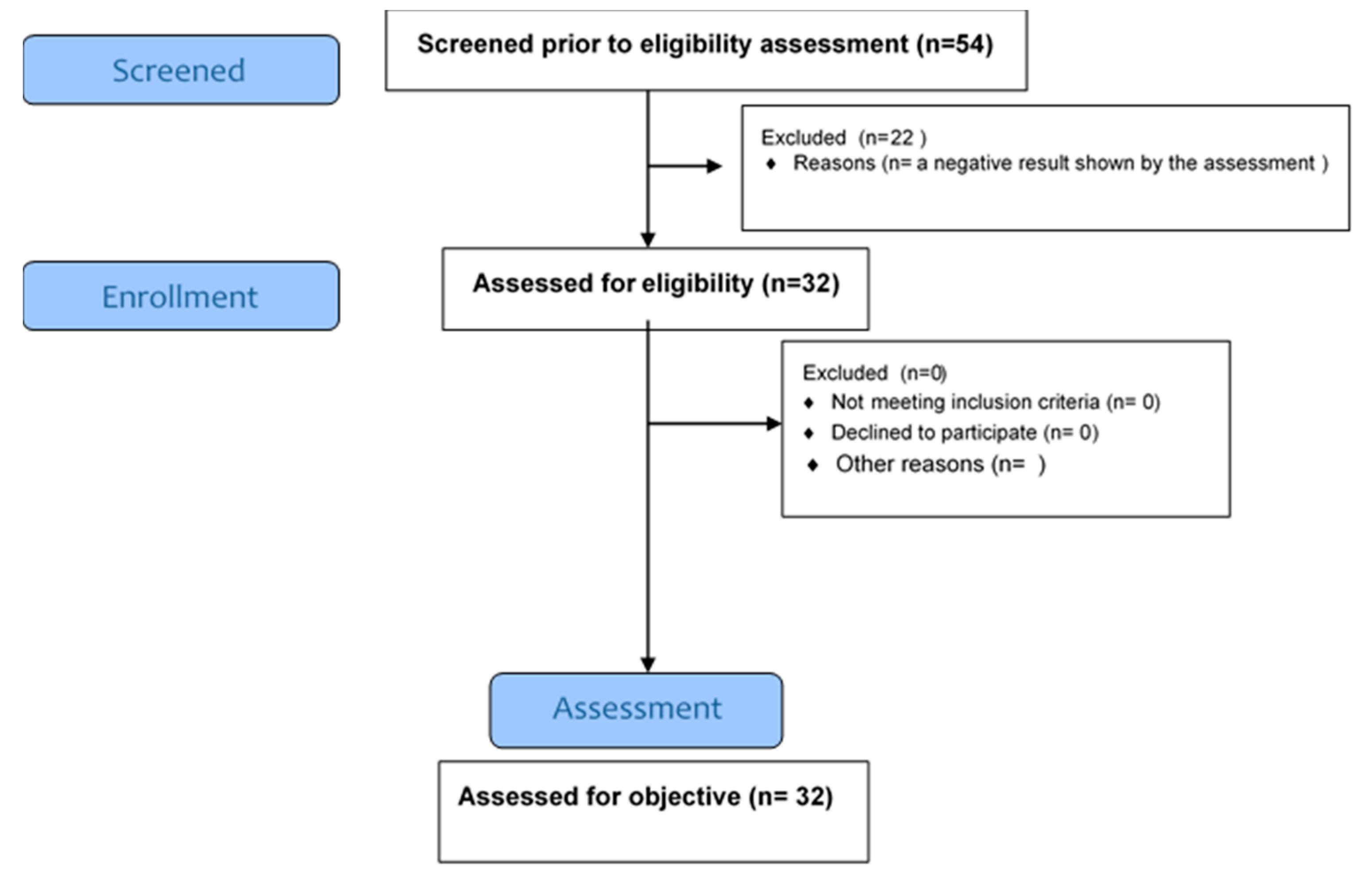
2.3. Participants
2.4. Data Sources/Measurement
2.4.1. Scales for Delirium Testing
2.4.2. Scales Assessing the Effect on the Occurrence of Delirium
2.5. Inclusion and Exclusion Criteria
2.6. Statistical Analysis
3. Results
3.1. Participants
3.2. Delirium Syndrome According to NuDESC and DOSS
3.3. Delirium Syndrome According to Numeric Rating Scale (NRS)
3.4. Delirium Syndrome According to the Richmond Agitation Sedation Scale (RASS) and the Ramsay Sedation Scale (RSS)
3.5. Delirium Syndrome According to the Insomnia Severity Index (ISI)
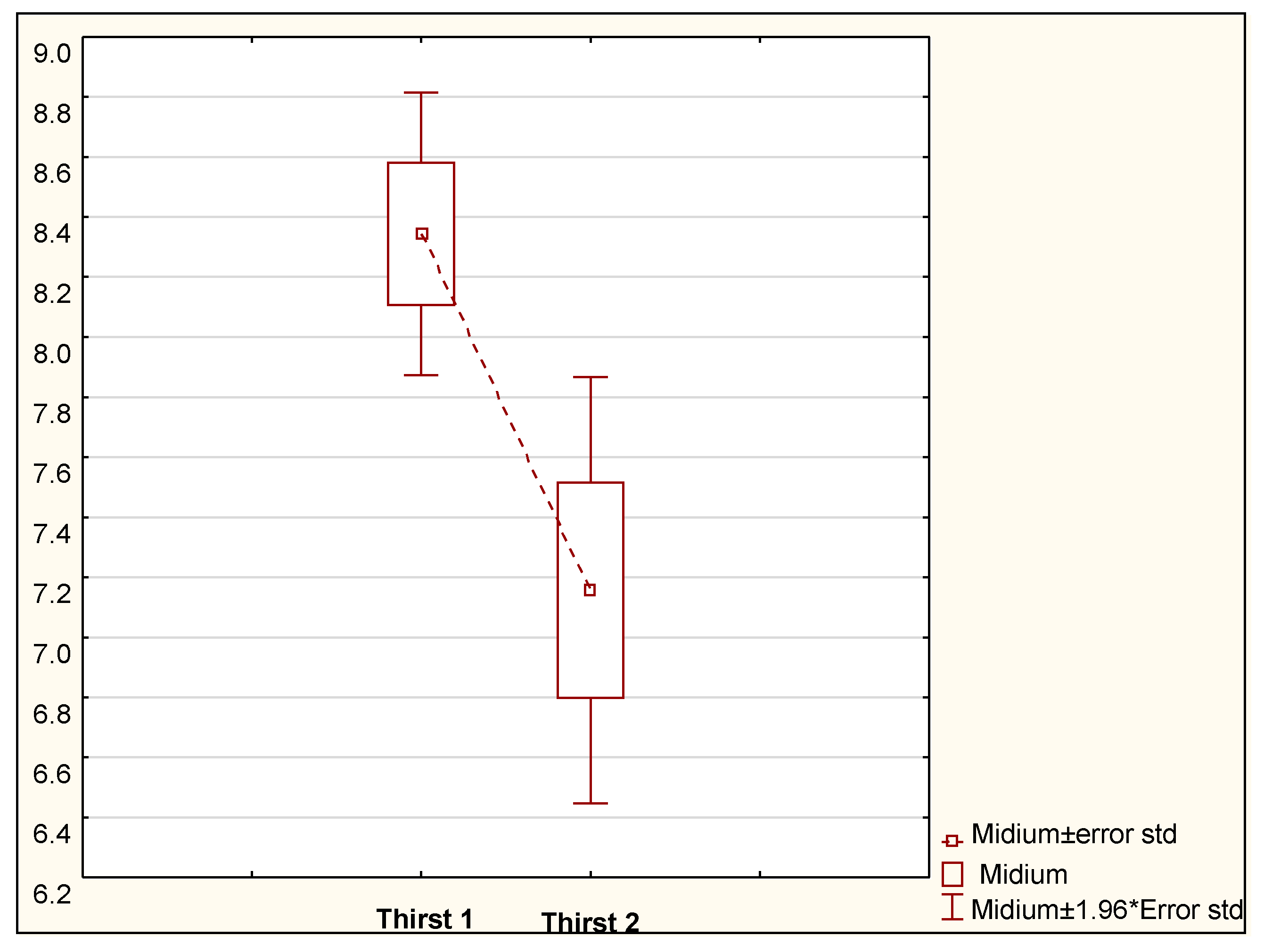
3.6. Delirium Syndrome According to Thirst Scale
4. Discussion
5. Conclusions
6. Implications for Practice
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thomas, F.; Chung, S.; Holt, D.W. Effects of ECMO Simulations and Protocols on Patient Safety. J. Extra-Corporeal. Technol. 2019, 51, 12–19. [Google Scholar]
- Salluh, J.I.F.; Wang, H.; Schneider, E.B.; Nagaraja, N.; Yenokyan, G.; Damluji, A.; Serafim, R.B.; Stevens, R.D. Outcome of delirium in critically ill patients: Systematic review and meta-analysis. BMJ 2015, 350, h2538. [Google Scholar] [CrossRef]
- American Psychiatric Association Neurocognitive Disorders. In Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association Publishing: Washington, DC, USA, 2013.
- Van Velthuijsen, E.L.; Zwakhalen, S.M.; Mulder, W.J.; Verhey, F.R.; Kempen, G.I. Detection and management of hyperactive and hypoactive delirium in older patients during hospitalization: A retrospective cohort study evaluating daily practice. Int. J. Geriatr. Psychiatry 2017, 33, 1521–1529. [Google Scholar] [CrossRef]
- Pun, B.T.; Balas, M.C.; Barnes-Daly, M.A.; Thompson, J.L.; Aldrich, J.M.; Barr, J.; Byrum, D.; Carson, S.S.; Devlin, J.W.; Engel, H.J.; et al. Caring for Critically Ill Patients with the ABCDEF Bundle. Crit. Care Med. 2019, 47, 3–14. [Google Scholar] [CrossRef]
- McPherson, J.A.; Wagner, C.E.; Boehm, L.M.; Hall, J.D.; Johnson, D.C.; Miller, L.R.; Burns, K.M.; Thompson, J.L.; Shintani, A.K.; Ely, E.W.; et al. Delirium in the Cardiovascular ICU. Crit. Care Med. 2013, 41, 405–413. [Google Scholar] [CrossRef]
- Sockalingam, S.; Parekh, N.; Bogoch, I.I.; Sun, J.; Mahtani, R.; Beach, C.; Bollegalla, N.; Turzanski, S.; Seto, E.; Kim, J.; et al. Delirium in the Postoperative Cardiac Patient: A Review. J. Card. Surg. 2005, 20, 560–567. [Google Scholar] [CrossRef]
- Marra, A.; Kotfis, K.; Hosie, A.; MacLullich, A.M.J.; Pandharipande, P.P.; Ely, E.W.; Pun, B.T. Delirium Monitoring: Yes or No? That is the Question. Am. J. Crit. Care 2019, 28, 127–135. [Google Scholar] [CrossRef]
- Barr, J.; Fraser, G.L.; Puntillo, K.; Ely, E.W.; Gélinas, C.; Dasta, J.F.; Davidson, J.E.; Devlin, J.W.; Kress, J.P.; Joffe, A.M.; et al. Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult Patients in the Intensive Care Unit. Crit. Care Med. 2013, 41, 263–306. [Google Scholar] [CrossRef] [PubMed]
- Kotfis, K.; Strzelbicka, M.; Zegan-Barańska, M.; Safranow, K.; Brykczyński, M.; Żukowski, M.; Ely, E.W. Validation of the behavioral pain scale to assess pain intensity in adult, intubated postcardiac surgery patients. Medicine 2018, 97, e12443. [Google Scholar] [CrossRef]
- Kotfis, K.; Zegan-Barańska, M.; Strzelbicka, M.; Safranow, K.; Żukowski, M.; Ely, E.W. Validation of the Polish version of the Critical Care Pain Observation Tool (CPOT) to assess pain intensity in adult, intubated intensive care unit patients: The POL-CPOT study. Arch. Med. Sci. 2017, 13, 880–889. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Gavinski, K.; Carnahan, R.; Weckmann, M. Validation of the delirium observation screening scale in a hospitalized older population. J. Hosp. Med. 2016, 11, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Gaudreau, J.-D.; Gagnon, P.; Harel, F.; Tremblay, A.; Roy, M.-A. Fast, Systematic, and Continuous Delirium Assessment in Hospitalized Patients: The Nursing Delirium Screening Scale. J. Pain Symptom. Manag. 2005, 29, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Schuurmans, M.J.; Shortridge-Baggett, L.M.; Duursma, S.A. The Delirium Observation Screening Scale: A Screening Instrument for Delirium. Res. Theory Nurs. Pr. 2003, 17, 31–50. [Google Scholar] [CrossRef]
- Weckmann, M.; Martin, M. Can the Delirium Observation Scale (DOS) Be Used to Screen for Delirium in the ICU? (S804). J. Pain Symptom. Manag. 2017, 53, 468. [Google Scholar] [CrossRef]
- Balková, M.; Tomagová, M. Use of measurement tools for screening of postoperative delirium in nursing practice. Central Eur. J. Nurs. Midwifery 2018, 9, 897–904. [Google Scholar] [CrossRef]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, P.V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agitation–Sedation Scale. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef]
- Rasheed, A.M.; Amirah, M.F.; Abdallah, M.; Parameaswari, P.J.; Issa, M.; Alharthy, A. Ramsay Sedation Scale and Richmond Agitation Sedation Scale. Dimens. Crit. Care Nurs. 2019, 38, 90–95. [Google Scholar] [CrossRef]
- Capponi, R.; Loguercio, V.; Guerrini, S.; Beltrami, G.; Vesprini, A.; Giostra, F. Does the Numeric Rating Scale (NRS) represent the optimal tool for evaluating pain in the triage process of patients presenting to the ED? Results of a multicenter study. Acta Biomed. 2016, 16, 347–352. [Google Scholar]
- Bastien, C.H.; Vallieres, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Sato, K.; Okajima, M.; Taniguchi, T. Association of Persistent Intense Thirst with Delirium among Critically Ill Patients: A Cross-sectional Study. J. Pain Symptom. Manag. 2019, 57, 1114–1120. [Google Scholar] [CrossRef]
- Lewandowska, K.; Małkiewicz, M.A.; Siemiński, M.; Cubała, W.J.; Winklewski, P.J.; Mędrzycka-Dąbrowska, W.A. The role of melatonin and melatonin receptor agonist in the prevention of sleep disturbances and delirium in intensive care unit—A clinical review. Sleep Med. 2020, 69, 127–134. [Google Scholar] [CrossRef]
- Anderson, J.M.; Boyle, K.B.; Murphy, A.A.; Yaeger, K.A.; LeFlore, J.; Halamek, L.P. Simulating extracorporeal membrane oxygenation emergencies to improve human performance. Part I: Methodologic and technologic innovations. Simul Healthc. 2006, 1, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.; Combes, A.; Rozé, H.; Chevret, S.; Mercat, A.; Roch, A.; Mourvillier, B.; Ara-Somohano, C.; Bastien, O.; Zogheib, E.; et al. Extracorporeal Membrane Oxygenation for Pandemic Influenza A(H1N1)–induced Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2013, 187, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Mędrzycka-Dąbrowska, W.; Dąbrowski, S.; Basiński, A. Perception of barriers to postoperative pain management in elderly patients in Polish hospitals—A multicentre study. J. Nurs. Manag. 2016, 24, 1049–1059. [Google Scholar] [CrossRef]
- Awan, O.; Buhr, R.; Kamdar, B. Delirium. “Unable-to-Assess”? An Electronic Health Record-Based Evaluation of Inappropriate “Unable-to-Assess” Confusion Assessment Method for the Intensive Care Unit (ICU) Documentation in a Medical ICU. In b104. Critical Care: Catch-22—Beyond the Ventilator: The Challenges of Delirium, ICU-Acquired Weakness, and Rehabilitation; American Thoracic Society: Dallas, TX, USA, 2019; Volume A4099. [Google Scholar]
- Dres, M.; Younes, M.; Rittayamai, N.; Kendzerska, T.; Telias, I.; Grieco, D.L.; Pham, T.; Junhasavasdikul, D.; Chau, E.; Mehta, S.; et al. Sleep and Pathological Wakefulness at the Time of Liberation from Mechanical Ventilation (SLEEWE). A Prospective Multicenter Physiological Study. Am. J. Respir. Crit. Care Med. 2019, 199, 1106–1115. [Google Scholar] [CrossRef]
- Sung, C.; Feder, S.L.; Crothers, K.A.; Akgun, K.M. The Intubated Patient’s Experience: Are We Paying Attention? Am. J. Resp. Crit. Care Med. 2019, 199, A6484. [Google Scholar] [CrossRef]
- Krupa, S.; Ozga, D. Review of the Literature on the Occurrence of Delirium after Veno-Venous and Veno-Arterial Extracorporeal Membrane Oxygenation: A Systematic Review. Dement. Geriatr. Cogn. Disord. Extra 2019, 9, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Gutysz-Wojnicka, A.; Dyk, D.; Ozga, D.; Cudak, E. Non-verbal indicators of pain in unconscious, mechanically ventilated patients. Anestezjol. Ratow. 2014, 8, 23–31. [Google Scholar]
- Ozga, D.; Krupa, S.; Witt, P.; Mędrzycka-Dąbrowska, W. Nursing Interventions to Prevent Delirium in Critically Ill Patients in the Intensive Care Unit during the COVID19 Pandemic—Narrative Overview. Health 2020, 8, 578. [Google Scholar] [CrossRef]
- Mędrzycka-Dąbrowska, W.; Dąbrowski, S.; Gutysz-Wojnicka, A.; Basiński, A. Polish nurses’ perceived barriers in using evidence-based practice in pain management. Int. Nurs. Rev. 2016, 63, 316–327. [Google Scholar] [CrossRef] [PubMed]
- Lewandowska, K.; Mędrzycka-Dąbrowska, W.; Pilch, D.; Wach, K.; Fortunato, A.; Krupa, S.; Ozga, D. Sleep Deprivation from the Perspective of a Patient Hospitalized in the Intensive Care Unit—Qualitative Study. Health 2020, 8, 351. [Google Scholar] [CrossRef] [PubMed]
- Ozga, D.; Mędrzycka-Dąbrowska, W.; Gutysz-Wojnicka, A.; Heikkilä, A.; Salminen, L. Requirements for teachers in the context of postgraduate nursing education: Polish experiences. Kontakt 2021, 23, 52–57. [Google Scholar] [CrossRef]
| NuDESC | 12 a.m. | 8 p.m. | p | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| <2 no delirium | 13 | 40.63% | 10 | 31.25% | 0.40933 |
| ≥2 delirium | 19 | 59.38% | 22 | 68.75% | 0.40412 |
| All | 32 | 100% | 32 | 100% | |
| DOSS | 7 a.m. | 3 p.m. | 9 p.m. | p | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| <3 no delirium | 5 | 15.63% | 9 | 28.13% | 23 | 71.88% | 0.000000 |
| ≥3 possible delirium | 27 | 84.38% | 23 | 71.88% | 9 | 28.13% | 0.000016 |
| All | 32 | 100% | 32 | 100% | 32 | 100% | |
| The Use of Direct Coercion | |||||||
|---|---|---|---|---|---|---|---|
| DOSS/Nu Desc | No | Yes | 8 p.m.–9 p.m. | p | |||
| N | % | N | % | N | % | ||
| No delirium | 15 | 100.00% | 11 | 64.71% | 26 | 81.25% | 0.40933 |
| Delirium | 0 | 0.00% | 6 | 35.29% | 6 | 18.75% | 0.40412 |
| All | 15 | 100.00% | 17 | 100.00% | 32 | 100% | |
| 7 a.m. | 3 p.m. | 9 p.m. | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient’s Condition in RASS | Yes | No | Yes | No | Yes | No | ||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Combative +4 | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Very agitated +3 | 0 | 0.00% | 6 | 18.75% | 2 | 6.25% | 4 | 12.50% | 5 | 15.63% | 1 | 3.13% |
| Agitated +2 | 0 | 0.00% | 12 | 37.50% | 1 | 3.13% | 11 | 34.38% | 9 | 28.13% | 3 | 9.38% |
| Restless +1 | 1 | 3.13% | 6 | 18.75% | 5 | 15.63% | 2 | 6.25% | 6 | 18.75% | 1 | 3.13% |
| Alert and calm 0 | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Drowsy –1 | 1 | 3.13% | 1 | 3.13% | 1 | 3.13% | 1 | 3.13% | 1 | 3.13% | 1 | 3.13% |
| Light sedation –2 | 1 | 3.13% | 1 | 3.13% | 0 | 0.00% | 2 | 6.25% | 1 | 3.13% | 1 | 3.13% |
| Moderate sedation –3 | 2 | 6.25% | 1 | 3.13% | 0 | 0.00% | 3 | 9.38% | 1 | 3.13% | 2 | 6.25% |
| Deep sedation –4 | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Unarousable sedation –5 | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Altogether | 12.63164 | df = 5 | p = 0.02709 | 12.35372 | df = 5 | p = 0.03025 | 4.015653 | df = 5 | p = 0.54716 | |||
| Patient Condition by the RASS | Degree of Sedation by Ramsey | All | ||||||
|---|---|---|---|---|---|---|---|---|
| Anxious and Agitated Patient | Cooperative, Tranquil, Oriented Patient | Sleeping Patient Responsive only to Instructions | ||||||
| N | % | N | % | N | % | N | % | |
| Very upset | 6 | 24% | 0 | 0% | 0 | 0% | 6 | 18.75% |
| Upset | 10 | 40% | 2 | 50% | 0 | 0% | 12 | 37.50% |
| Restless | 5 | 20% | 2 | 50% | 0 | 0% | 7 | 21.88% |
| Sleepy | 0 | 0% | 0 | 0% | 2 | 66.67% | 2 | 6.25% |
| Light sedation | 1 | 4% | 0 | 0% | 1 | 33.33% | 2 | 6.25% |
| Moderate sedation | 3 | 12% | 0 | 0% | 0 | 0% | 3 | 9.38% |
| Altogether | 25 | 100% | 4 | 100% | 3 | 100% | 32 | 100.00% |
| ISI Scale | N | % |
|---|---|---|
| 0–7 = No clinically significant insomnia | 8 | 25% |
| 8–14 = Subclinical insomnia | 9 | 28% |
| 15–21 = Clinical insomnia (moderate severity) | 10 | 31% |
| 22–28 = Clinical insomnia (severe) | 5 | 16% |
| All | 32 | 100% |
| Occurrence of Delirium | t | p |
|---|---|---|
| Pain (NRS) | −0.68 | 0.50 |
| Thirst before ice cube | 0.68 | 0.50 |
| Thirst after ice cube | −2.11 | 0.04 |
| ISI | 2.01 | 0.05 |
| Occurrence of Delirium | chi | p |
|---|---|---|
| RASS | 8.89 | 0.11 |
| Ramsey | 4.22 | 0.12 |
| Ice cube | 0.83 | 0.36 |
| ISI (Insomnia Severity Index) | 4.87 | 0.18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krupa, S.; Friganovic, A.; Mędrzycka-Dąbrowska, W. Occurrence of Delirium during ECMO Therapy in a Critical Care Unit in Poland—A Cross-Sectional Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 4029. https://doi.org/10.3390/ijerph18084029
Krupa S, Friganovic A, Mędrzycka-Dąbrowska W. Occurrence of Delirium during ECMO Therapy in a Critical Care Unit in Poland—A Cross-Sectional Pilot Study. International Journal of Environmental Research and Public Health. 2021; 18(8):4029. https://doi.org/10.3390/ijerph18084029
Chicago/Turabian StyleKrupa, Sabina, Adriano Friganovic, and Wioletta Mędrzycka-Dąbrowska. 2021. "Occurrence of Delirium during ECMO Therapy in a Critical Care Unit in Poland—A Cross-Sectional Pilot Study" International Journal of Environmental Research and Public Health 18, no. 8: 4029. https://doi.org/10.3390/ijerph18084029
APA StyleKrupa, S., Friganovic, A., & Mędrzycka-Dąbrowska, W. (2021). Occurrence of Delirium during ECMO Therapy in a Critical Care Unit in Poland—A Cross-Sectional Pilot Study. International Journal of Environmental Research and Public Health, 18(8), 4029. https://doi.org/10.3390/ijerph18084029








