Dissatisfaction with Local Medical Services for Middle-Aged and Elderly in China: What Is Relevant?
Abstract
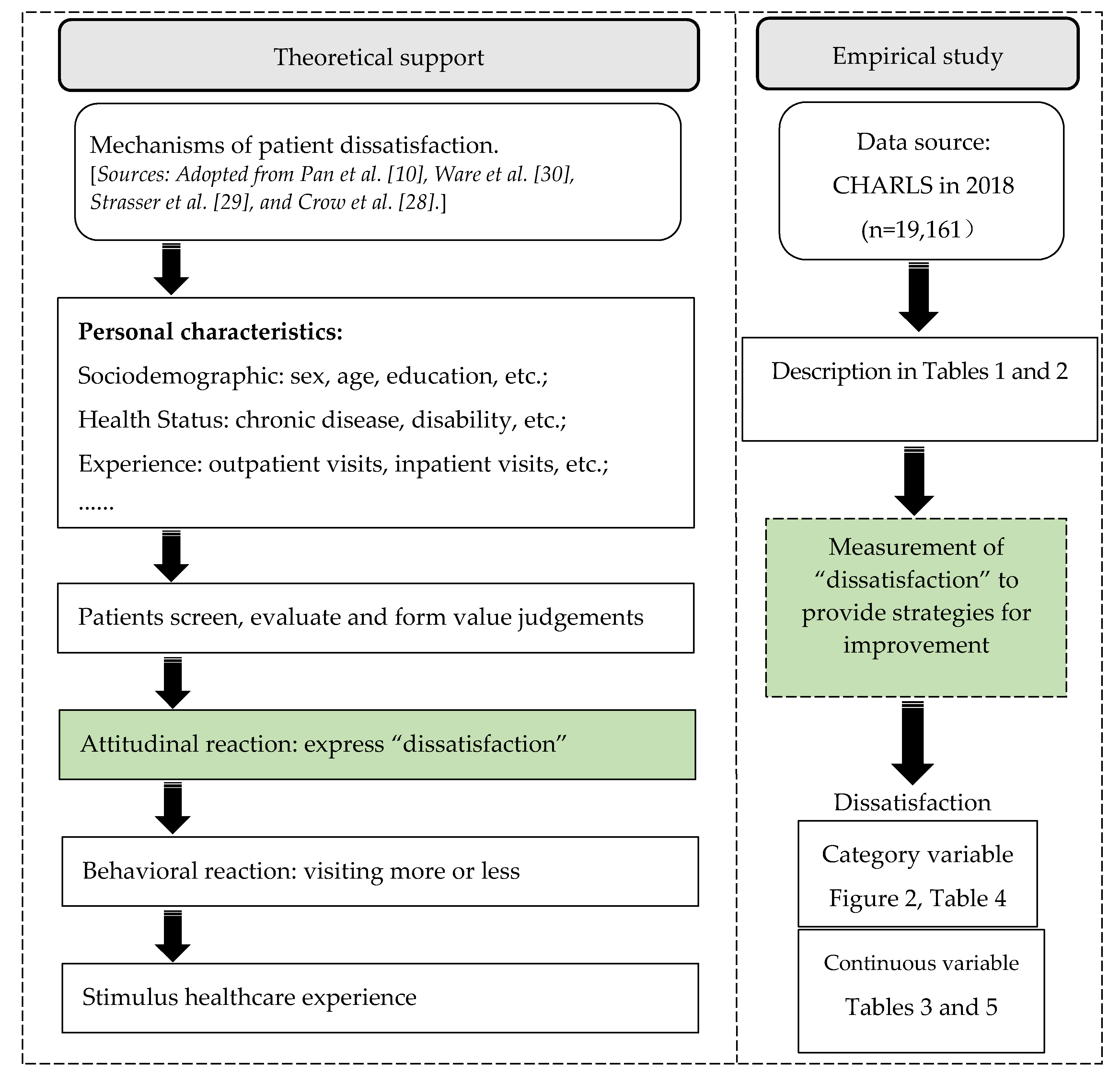
1. Introduction
2. Methods
2.1. Data Sources
2.2. Variables
2.3. Data Analysis
3. Results
3.1. Descriptive Statistics
3.2. Regression Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bleich, S.N.; Ozaltin, E.; Murray, C.J.L. How does satisfaction with the health-care system relate to patient experience? B World Health Organ. 2009, 87, 271–278. [Google Scholar] [CrossRef]
- Ruggieri, T.G.; Berta, P.; Murante, A.M.; Nuti, S. Patient satisfaction, patients leaving hospital against medical advice and mortality in Italian university hospitals: A cross-sectional analysis. BMC Health Serv. Res. 2018, 18, 51. [Google Scholar] [CrossRef]
- Gunaratne, R.; Pratt, D.N.; Banda, J.; Fick, D.P.; Khan, R.J.; Robertson, B.W. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J. Arthroplast. 2017, 32, 3854–3860. [Google Scholar] [CrossRef] [PubMed]
- Coulter, A. Can patients assess the quality of health care? Patients’ surveys should ask about real experiences of medical care. Brit. Med. J. 2006, 333, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Jameel, A.; Asif, M.; Hussain, A.; Hwang, J.; Bukhari, M.H.; Mubeen, S.; Kim, I. Improving Patient behavioral Consent through Different Service Quality Dimensions: Assessing the Mediating Role of Patient Satisfaction. Int. J. Environ. Res. Public Health 2019, 16, 4736. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Xie, T.; Ning, W. The influence of medical service quality on patients’ perception of doctor-patient relationship: Mediating effect analysis based on patient satisfaction. J. Xi’an Jiaotong Univ. (Soc. Sci.) 2020, 40, 119–127. [Google Scholar]
- Sun, J.; Zhang, L.; Yu, Y.; Ma, N.; He, C. Interpretation of the behavioral economics and countermeasures of the risk in doctor-patient relationship. Acta Univ. Med. Nanjing (Soc. Sci.) 2016, 16, 141–145. [Google Scholar]
- Perneger, T.V.; Peytremann-Bridevaux, I.; Combescure, C. Patient satisfaction and survey response in 717 hospital surveys in Switzerland: A cross-sectional study. BMC Health Serv. Res. 2020, 20, 158. [Google Scholar] [CrossRef]
- Shan, L.; Li, Y.; Ding, D.; Wu, Q.; Liu, C.; Jiao, M.; Hao, Y.; Han, Y.; Gao, L.; Hao, J.; et al. Patient Satisfaction with Hospital Inpatient Care: Effects of Trust, Medical Insurance and Perceived Quality of Care. PLoS ONE 2016, 11, e0164366. [Google Scholar] [CrossRef]
- Pan, J.; Liu, D.; Ali, S. Patient dissatisfaction in China: What Matters. Soc. Sci. Med. 2015, 143, 145–153. [Google Scholar] [CrossRef]
- Stevens, L.M. “We have to be mythbusters”: Clinician attitudes about the legitimacy of patient concerns and dissatisfaction with contraception. Soc. Sci. Med. 2018, 212, 145–152. [Google Scholar] [CrossRef]
- Minnick, A.F.; Roberts, M.J.; Young, W.B.; Kleinpell, R.M.; Marcantonio, R.J. What influences patients’ reports of three aspects of hospital services? Med. Care 1997, 35, 399–409. [Google Scholar] [CrossRef]
- Geberu, D.M.; Biks, G.A.; Gebremedhin, T.; Mekonnen, T.H. Factors of patient satisfaction in adult outpatient departments of private wing and regular services in public hospitals of Addis Ababa, Ethiopia: A comparative cross-sectional study. BMC Health Serv. Res. 2019, 19, 1–13. [Google Scholar] [CrossRef]
- Cohen, G. Age and health status in a patient satisfaction survey. Soc. Sci. Med. 1996, 42, 1085–1093. [Google Scholar] [CrossRef]
- Aziz, M.M.; Ji, W.; Masood, I.; Farooq, M.; Malik, M.Z.; Chang, J.; Jiang, M.; Atif, N.; Fang, Y. Patient Satisfaction with Community Pharmacies Services: A Cross-Sectional Survey from Punjab; Pakistan. Int. J. Environ. Res. Public Health 2018, 15, 2914. [Google Scholar] [CrossRef] [PubMed]
- Jalil, A.; Zakar, R.; Zakar, M.Z.; Fischer, F. Patient satisfaction with doctor-patient interactions: A mixed methods study among diabetes mellitus patients in Pakistan. BMC Health Serv. Res. 2017, 17, 1–13. [Google Scholar] [CrossRef]
- Wu, D.; Huang, X.; Hu, C.; Yan, S.; Zhang, Y. Satisfaction influencing factors of family doctors’ contracted services among contracted patients with chronic diseases. J. Nanjing Med. Univ. (Soc. Sci.) 2020, 20, 71–76. [Google Scholar]
- Yang, Y.; Zhu, Z.; Jiang, Y.; Yu, J.; Luan, W.; Shi, W. Analysis of the effectiveness of in and out hospital services and patient satisfaction in a tertiary public hospital. Chin. Hosp. Manag. 2021, 41, 63–66. [Google Scholar]
- Key Data Release of the Sixth National Population Census. Available online: http://www.stats.gov.cn/ztjc/zdtjgz/zgrkpc/dlcrkpc/dcrkpcyw/201104/t20110428_69407.htm (accessed on 28 April 2011).
- Corder, L.S.; Woodbury, M.A.; Manton, K.G. Proxy response patterns among the aged: Effects on estimates of health status and medical care utilization from the 1982–1984 long-term care surveys. J. Clin. Epidemiol. 1996, 49, 173–182. [Google Scholar] [CrossRef]
- McFadden, E.; Luben, R.; Bingham, S.; Wareham, N.; Kinmonth, A.-L.; Khaw, K.-T. Social inequalities in self-rated health by age: Cross-sectional study of 22 457 middle-aged men and women. BMC Public Health 2008, 8, 230. [Google Scholar] [CrossRef]
- Wu, F.; Guo, Y.; Kowal, P.; Jiang, Y.; Yu, M.; Li, X.; Zheng, Y.; Xu, J. Prevalence of Major Chronic Conditions among Older Chinese Adults: The Study on Global AGEing and Adult Health (SAGE) Wave 1. PLoS ONE 2013, 8, e74176. [Google Scholar] [CrossRef]
- Wang, R.; Yan, Z.; Liang, Y.; Tan, E.C.K.; Cai, C.; Jiang, H.; Song, A.; Qiu, C. Prevalence and Patterns of Chronic Disease Pairs and Multimorbidity among Older Chinese Adults Living in a Rural Area. PLoS ONE 2015, 10, e0138521. [Google Scholar] [CrossRef]
- Hu, B.; Peng, D.Y.; Zhang, Y.D.; Yu, J.Y. Rural population aging and the hospital utilization in cties: The rise of medical tourism in China. Int. J. Environ. Res. Public Health 2020, 17, 4790. [Google Scholar] [CrossRef]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort Profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Oshio, T. The impact of social insurance on health among middle-aged and older adults in rural China: A longitudinal study using a three-wave nationwide survey. BMC Public Health 2020, 20, 1842. [Google Scholar]
- Zhao, Y.; Strauss, J.; Yang, G.; Giles, J.; Hu, P.P.; Hu, Y.; Lei, X.; Park, A.; Smith, J.P.; Wang, Y. China Health and Retirement Longitudinal Study, 2011–2012 National Baseline Users’ Guide; Peking University: Beijing, China, 2013; p. 8. [Google Scholar]
- Crow, R.; Gage, H.; Hampson, S.; Hart, J.; Kimber, A.; Storey, L.; Thomas, H. The measurement of satisfaction with healthcare: Implications for practice from a systematic review of the literature. Health Technol. Assess. 2002, 6, 1–244. [Google Scholar] [CrossRef]
- Strasser, S.; Aharony, L.; Greenberger, D. The Patient Satisfaction Process: Moving Toward a Comprehensive Model. Med Care Rev. 1993, 50, 219–248. [Google Scholar] [CrossRef]
- Ware, J.E.; Snyder, M.K.; Wright, W.; Davies, A.R. Defining and measuring patient satisfaction with medical care. Eval. Program Plan. 1983, 6, 247–263. [Google Scholar] [CrossRef]
- Wang, J.; Okoli, C.T.; He, H.; Feng, F.; Li, J.; Zhuang, L.; Lin, M. Factors associated with compassion satisfaction, burnout, and secondary traumatic stress among Chinese nurses in tertiary hospitals: A cross-sectional study. Int. J. Nurs. Stud. 2020, 102, 103472. [Google Scholar] [CrossRef]
- DeVoe, J.E.; Wallace, L.S.; Fryer, G.E. Patient age influences perceptions about health care communication. Fam. Med. 2009, 41, 126–133. [Google Scholar]
- Javed, S.A.; Liu, S.; Mahmoudi, A.; Nawaz, M. Patients’ satisfaction and public and private sectors’ health care service quality in Pakistan: Application of grey decision analysis approaches. Int. J. Health Plan. Manag. 2019, 34, e168–e182. [Google Scholar] [CrossRef]
- Kleefstra, S.M.; Zandbelt, L.C.; De Haes, H.J.C.J.M.; Kool, R.B. Trends in patient satisfaction in Dutch university medical centers: Room for improvement for all. BMC Health Serv. Res. 2015, 15, 112. [Google Scholar] [CrossRef]
- Mfinanga, S.G.; Kahwa, A.; Kimaro, G.; Kilale, A.; Kivuyo, S.; Senkoro, M.; Ngowi, B.; Mtandu, R.; Mutayoba, B.; Ngadaya, E.; et al. Patient’s dissatisfaction with the public and private laboratory services in conducting HIV related testing in Tanzania. BMC Health Serv. Res. 2008, 8, 167. [Google Scholar] [CrossRef]
- Satghare, P.; Mahesh, M.V.; Abdin, E.; Chong, S.A.; Subramaniam, M. The Relative Associations of Body Image Dissatisfaction among Psychiatric Out-Patients in Singapore. Int. J. Environ. Res. Public Health 2019, 16, 5162. [Google Scholar] [CrossRef]
- Popa, D.; Druguș, D.; Leașu, F.; Azoicăi, D.; Repanovici, A.; Rogozea, L.M. Patients’ perceptions of healthcare professionalism-a Romanian experience. BMC Health Serv. Res. 2017, 17, 463. [Google Scholar] [CrossRef]
- Hussain, A.; Asif, M.; Jameel, A.; Hwang, J. Measuring OPD Patient Satisfaction with Different Service Delivery Aspects at Public Hospitals in Pakistan. Int. J. Environ. Res. Public Health 2019, 16, 2340. [Google Scholar] [CrossRef] [PubMed]
- Omer, K.; Cockcroft, A.; Andersson, N. Impact of a hospital improvement initiative in Bangladesh on patient experiences and satisfaction with services: Two cross-sectional studies. BMC Health Serv. Res. 2011, 11, S10. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.; Asif, M.; Jameel, A.; Hwang, J.; Sahito, N.; Kanwel, S. Promoting OPD Patient Satisfaction through Different Healthcare Determinants: A Study of Public Sector Hospitals. Int. J. Environ. Res. Public Health 2019, 16, 3719. [Google Scholar] [CrossRef]
- Liu, M.; Liu, W.; Tao, S.; Xue, Y.; Liang, L. Analysis of the patients’ satisfaction of treatment links in public hospitals. Chin. Hosp. Manag. 2019, 39, 28–30. [Google Scholar]
- Marcinowicz, L.; Chlabicz, S.; Grebowski, R. Patient satisfaction with healthcare provided by family doctors: Primary dimensions and an attempt at typology. BMC Health Serv. Res. 2009, 9, 63. [Google Scholar] [CrossRef][Green Version]

| Variables | Description and Value |
|---|---|
| Dissatisfaction | Binary variable: 0 = Yes (somewhat dissatisfied and very dissatisfied); 1 = No (very satisfied, somewhat satisfied and neutral) |
| Continuous variable, ranging from score 1 to 5 | |
| Type of residence | 0 = Rural; 1 = Urban |
| Sex | 0 = Male; 1 = Female |
| Age (years) | 1 = 45–50; 2 = 51–60; 3 = 61–70; 4 = ≥71 |
| Education | 0 = Illiterate; 1 = ≤Elementary school; 2 = ≥Middle school |
| Living status | 0 = Live with others; 1 = Live alone |
| Economic status | 1 = Low; 2 = Middle; 3 = High |
| Chronic diseases | 0 = No; 1 = Yes |
| Utilizing outpatients in the last month | 0 = No; 1 = Yes |
| Utilizing inpatients in the past year | 0 = No; 1 = Yes |
| Utilizing paid family doctor services | 0 = No; 1 = Yes |
| Variables | Rural (n = 14,263) | Urban (n = 4898) | Total | ||
|---|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | ||
| Sex | |||||
| Male | 6772 | 47.48 | 2326 | 47.49 | 9098 |
| Female | 7491 | 52.52 | 2572 | 52.51 | 10,063 |
| Age (years) | |||||
| 45–50 | 1749 | 12.26 | 679 | 13.86 | 2428 |
| 51–60 | 4596 | 32.22 | 1716 | 35.03 | 6312 |
| 61–70 | 4752 | 33.32 | 1513 | 30.89 | 6265 |
| ≥71 | 3166 | 22.20 | 990 | 20.22 | 4156 |
| Education | |||||
| Illiterate | 3934 | 27.58 | 457 | 9.33 | 4391 |
| ≤Elementary school | 6694 | 46.93 | 1524 | 31.11 | 8218 |
| ≥Middle school | 3635 | 25.49 | 2917 | 59.55 | 6552 |
| Living status | |||||
| Live with others | 11,131 | 78.04 | 3878 | 79.18 | 15,009 |
| Live alone | 3132 | 21.96 | 1020 | 20.82 | 4152 |
| Economic status | |||||
| Low | 4143 | 29.05 | 444 | 9.06 | 4587 |
| Middle | 7536 | 52.84 | 2089 | 42.65 | 9625 |
| High | 2583 | 18.11 | 2365 | 48.29 | 4948 |
| Chronic diseases | |||||
| No | 8034 | 56.33 | 2612 | 53.33 | 10,646 |
| Yes | 6229 | 43.67 | 2286 | 46.67 | 8515 |
| Utilizing outpatients | |||||
| No | 11,920 | 83.58 | 4075 | 83.23 | 15,995 |
| Yes | 2342 | 16.42 | 821 | 16.77 | 3163 |
| Utilizing inpatients | |||||
| No | 11,885 | 83.33 | 4019 | 82.09 | 15,904 |
| Yes | 2377 | 16.67 | 877 | 17.91 | 3254 |
| Utilizing paid family doctor services | |||||
| No | 13,603 | 95.38 | 4760 | 97.24 | 18,363 |
| Yes | 659 | 4.62 | 135 | 2.76 | 794 |
| Variables | Rural (n = 14,263) | Urban (n = 4898) | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | t/F | p | Mean ± SD | t/F | p | |
| Utilizing outpatients | ||||||
| No | 2.65 ± 1.10 | −3.42 | <0.001 | 2.88 ± 1.00 | −2.90 | 0.002 |
| Yes | 2.74 ± 1.08 | 2.99 ± 1.08 | ||||
| Utilizing inpatients | ||||||
| No | 2.67 ± 1.09 | 0.20 | 0.420 | 2.89 ± 1.01 | −1.77 | 0.039 |
| Yes | 2.67 ± 1.13 | 2.95 ± 1.07 | ||||
| Utilizing paid family doctor services | ||||||
| No | 2.68 ± 1.10 | 6.79 | <0.001 | 2.91 ± 1.02 | 4.52 | <0.001 |
| Yes | 2.38 ± 1.04 | 2.50 ± 1.00 | ||||
| Sex | ||||||
| Male | 2.74 ± 1.11 | 7.10 | <0.001 | 2.97 ± 1.03 | 4.14 | <0.001 |
| Female | 2.60 ± 1.09 | 2.84 ± 1.01 | ||||
| Age (years) | ||||||
| 45–50 | 2.80 ± 0.99 | 31.74 | <0.001 | 2.95 ± 0.98 | 3.31 | 0.019 |
| 51–60 | 2.75 ± 1.07 | 2.88 ± 0.98 | ||||
| 61–70 | 2.62 ± 1.13 | 2.95 ± 1.07 | ||||
| ≥71 | 2.55 ± 1.13 | 2.83 ± 1.04 | ||||
| Education | ||||||
| Illiterate | 2.49 ± 1.16 | 78.57 | <0.001 | 2.70 ± 1.16 | 14.70 | <0.001 |
| ≤Elementary school | 2.70 ± 1.08 | 2.85 ± 1.06 | ||||
| ≥Middle school | 2.79 ± 1.04 | 2.96 ± 0.97 | ||||
| Living status | ||||||
| Live with others | 2.68 ± 1.09 | 1.62 | 0.053 | 2.91 ± 1.00 | 1.77 | 0.039 |
| Live alone | 2.64 ± 1.13 | 2.85 ± 1.10 | ||||
| Economic status | ||||||
| Low | 2.68 ± 1.15 | 1.08 | 0.341 | 2.77 ± 1.18 | 3.98 | 0.019 |
| Middle | 2.66 ± 1.11 | 2.93 ± 1.04 | ||||
| High | 2.68 ± 1.00 | 2.90 ± 0.97 | ||||
| Chronic diseases | ||||||
| No | 2.62 ± 1.07 | −5.73 | <0.001 | 2.84 ± 1.01 | −3.91 | <0.001 |
| Yes | 2.73 ± 1.13 | 2.96 ± 1.02 | ||||
| Variables | Rural (n = 14,263) | Urban (n = 4898) | ||||
|---|---|---|---|---|---|---|
| No | Yes | p | No | Yes | p | |
| Utilizing outpatients | ||||||
| No | 9711 (84.83) | 1736 (15.17) | 0.130 | 3165 (81.87) | 701 (18.13) | 0.001 |
| Yes | 1925 (83.59) | 378 (16.41) | 622 (76.70) | 189 (23.30) | ||
| Utilizing inpatients | ||||||
| No | 9700 (84.83) | 1734 (15.17) | 0.131 | 3118 (81.79) | 694 (18.21) | 0.003 |
| Yes | 1936 (83.59) | 380 (16.41) | 669 (77.34) | 196 (22.66) | ||
| Utilizing paid family doctor services | ||||||
| No | 11,051 (84.37) | 2048 (15.63) | <0.001 | 3669 (80.71) | 877 (19.29) | 0.007 |
| Yes | 585 (89.86) | 66 (10.14) | 118 (90.08) | 13 (9.92) | ||
| Sex | ||||||
| Male | 5413 (82.78) | 1126 (17.22) | <0.001 | 1751 (79.52) | 451 (20.48) | 0.017 |
| Female | 6223 (86.30) | 988 (13.70) | 2036 (82.26) | 439 (17.74) | ||
| Age (years) | ||||||
| 45–50 | 1461 (85.64) | 245 (14.36) | 0.224 | 519 (81.09) | 121 (18.91) | 0.007 |
| 51–60 | 3739 (84.02) | 711 (15.98) | 1370 (83.03) | 280 (16.97) | ||
| 61–70 | 3882 (84.32) | 722 (15.68) | 1135 (78.17) | 317 (21.83) | ||
| ≥71 | 2554 (85.42) | 436 (14.58) | 763 (81.60) | 172 (18.40) | ||
| Education | ||||||
| Illiterate | 3231 (86.30) | 513 (13.70) | 0.001 | 351 (82.78) | 73 (17.22) | 0.568 |
| ≤Elementary school | 5477 (84.50) | 1005 (15.50) | 1180 (81.10) | 275 (18.90) | ||
| ≥Middle school | 2928 (83.09) | 596 (16.91) | 2256 (80.63) | 542 (19.37) | ||
| Living status | ||||||
| Live with others | 9143 (84.62) | 1662 (15.38) | 0.964 | 3038 (81.36) | 696 (18.64) | 0.177 |
| Live alone | 2493 (84.65) | 452 (15.35) | 749 (79.43) | 194 (20.57) | ||
| Economic status | ||||||
| Low | 3305 (83.06) | 674 (16.91) | 0.001 | 337 (81.20) | 78 (18.80) | 0.391 |
| Middle | 6168 (84.85) | 1101 (15.15) | 1591 (80.07) | 396 (19.93) | ||
| High | 2162 (86.45) | 339 (13.55) | 1859 (81.71) | 416 (18.29) | ||
| Chronic diseases | ||||||
| No | 6655 (86.27) | 1059 (13.73) | <0.001 | 2047 (82.71) | 428 (17.29) | 0.001 |
| Yes | 4981 (82.52) | 1055 (17.48) | 1740 (79.02) | 462 (20.98) | ||
| Variables | Rural | Urban | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||||||
| OR | 95% CL | p | β | 95% CL | p | OR | 95% CL | p | β | 95% CL | p | |
| Utilizing outpatients | 1.06 | 0.93, 1.21 | 0.357 | 0.07 | 0.02, 0.12 | 0.008 | 1.41 | 1.17, 1.72 | <0.001 | 0.12 | 0.04, 0.20 | 0.002 |
| Utilizing inpatients | 1.02 | 0.90, 1.16 | 0.775 | −0.003 | −0.05, 0.05 | 0.910 | 1.21 | 1.00, 1.47 | 0.056 | 0.04 | −0.04, 0.11 | 0.323 |
| Utilizing paid family doctor services | ||||||||||||
| 0.58 | 0.45, 0.76 | <0.001 | −0.31 | −0.39, −0.22 | <0.001 | 0.46 | 0.25, 0.84 | 0.011 | −0.39 | −0.57, −0.22 | <0.001 | |
| Female | 0.75 | 0.67, 0.83 | <0.001 | −0.11 | −0.15, −0.07 | <0.001 | 0.80 | 0.68, 0.93 | 0.004 | −0.11 | −0.17, −0.06 | <0.001 |
| Age (51–60 years) | 1.07 | 0.91, 1.26 | 0.417 | −0.07 | −0.13, −0.01 | 0.017 | 0.85 | 0.67, 1.10 | 0.225 | −0.07 | −0.16, 0.02 | 0.120 |
| Age (61–70 years) | 1.05 | 0.89, 1.24 | 0.576 | −0.18 | −0.24, −0.12 | <0.001 | 1.14 | 0.87, 1.46 | 0.311 | −0.03 | −0.12, 0.07 | 0.602 |
| Age (≥71 years) | 0.95 | 0.79, 1.14 | 0.580 | −0.24 | −0.31, −0.17 | <0.001 | 0.89 | 0.67, 1.18 | 0.410 | −0.11 | −0.22, −0.01 | 0.035 |
| ≤Elementary school | 1.07 | 0.94, 1.22 | 0.282 | 0.13 | 0.08, 0.18 | <0.001 | 1.08 | 0.79, 1.46 | 0.625 | 0.10 | −0.01, 0.22 | 0.064 |
| ≥Middle school | 1.18 | 1.01, 1.38 | 0.036 | 0.19 | 0.13, 0.25 | <0.001 | 1.17 | 0.86, 1.59 | 0.304 | 0.20 | 0.09, 0.32 | <0.001 |
| Live alone | 1.04 | 0.92, 1.17 | 0.526 | 0.02 | −0.03, 0.06 | 0.443 | 1.19 | 0.98, 1.44 | 0.083 | −0.03 | −0.10, 0.05 | 0.492 |
| Middle economic status | 0.84 | 0.75, 0.94 | 0.003 | −0.06 | −0.10, −0.01 | 0.008 | 0.99 | 0.75, 1.33 | 0.927 | 0.08 | −0.02, 0.19 | 0.120 |
| High economic status | 0.73 | 0.63, 0.85 | <0.001 | −0.09 | −0.14, −0.03 | 0.004 | 0.86 | 0.64, 1.15 | 0.298 | 0.01 | −0.10, 0.12 | 0.878 |
| Chronic diseases | 1.33 | 1.20, 1.46 | <0.001 | 0.12 | 0.09, 0.16 | <0.001 | 1.23 | 1.06, 1.44 | 0.009 | 0.12 | 0.06, 0.18 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, X.; Su, M.; Zhao, Y.; Wang, D. Dissatisfaction with Local Medical Services for Middle-Aged and Elderly in China: What Is Relevant? Int. J. Environ. Res. Public Health 2021, 18, 3931. https://doi.org/10.3390/ijerph18083931
Fan X, Su M, Zhao Y, Wang D. Dissatisfaction with Local Medical Services for Middle-Aged and Elderly in China: What Is Relevant? International Journal of Environmental Research and Public Health. 2021; 18(8):3931. https://doi.org/10.3390/ijerph18083931
Chicago/Turabian StyleFan, Xiaojing, Min Su, Yaxin Zhao, and Duolao Wang. 2021. "Dissatisfaction with Local Medical Services for Middle-Aged and Elderly in China: What Is Relevant?" International Journal of Environmental Research and Public Health 18, no. 8: 3931. https://doi.org/10.3390/ijerph18083931
APA StyleFan, X., Su, M., Zhao, Y., & Wang, D. (2021). Dissatisfaction with Local Medical Services for Middle-Aged and Elderly in China: What Is Relevant? International Journal of Environmental Research and Public Health, 18(8), 3931. https://doi.org/10.3390/ijerph18083931





