Competency Model for the Middle Nurse Manager (MCGE-Logistic Level)
Abstract
1. Introduction
- Reach a consensus on the competencies required for a middle nurse manager.
- Establish a consensus on the degree of development of each of the competencies required for a middle nurse manager.
- Achieve consensus about the training required to develop each competency.
- Assess the structural validity of the proposed model.
2. Materials and Methods
2.1. Revision of the Literature
2.2. Delphi Methodology
2.2.1. Consensus
2.2.2. Participants
2.2.3. Variables
2.2.4. Delphi Surveys
2.2.5. Degree of Development
- Novice: a middle nurse manager who has no prior experience in a competency associated with a professional role or situation. In many instances, this is the starting point for a nurse manager, as they would be in possession of clinical competencies, yet lack knowledge and skills in management.
- Advanced novice: someone who is able to contribute partial solutions to unknown or complex situations. Although an advanced novice may be able to perform the functions required for the nurse manager position, they may or may not have the ability to understand the context and actions required.
- Competent: implies an adequate understanding of the context and situation. The competent middle nurse manager may be able to cope with situations associated with the nurse executive role, although they may lack analytical skills and an understanding of complex situations.
- Very competent: the middle nurse manager focuses on a comprehensive understanding of situations at every level, and is someone who is able to anticipate problems and make appropriate decisions.
- Expert one who demonstrates the behavior of the model of competencies. The expert nurse manager anticipates problems, understands them at an instinctive level and proposes correct and appropriate solutions [49].
2.3. Principal Component Analysis
3. Results
3.1. Demographic Data of the Panel of Experts
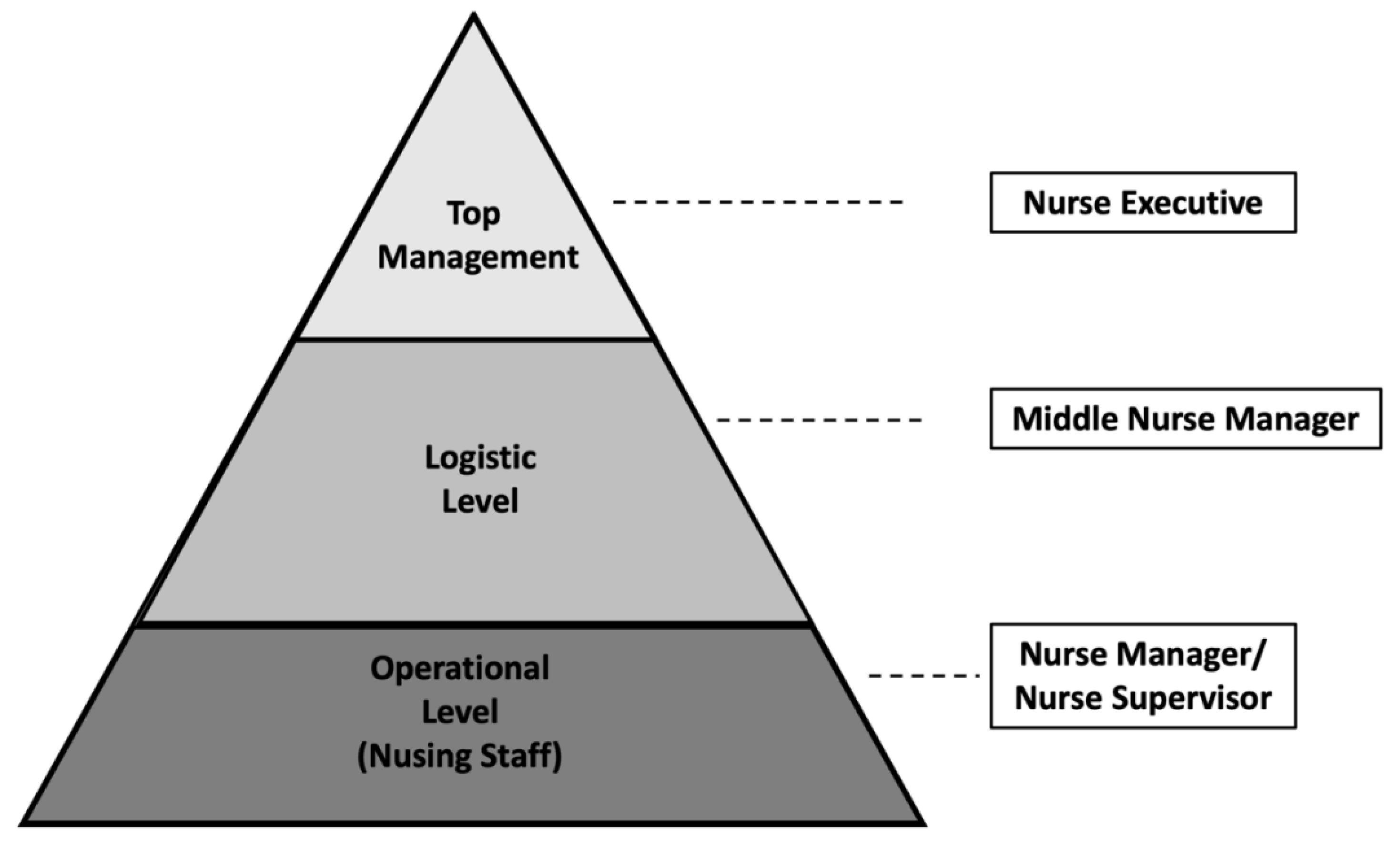
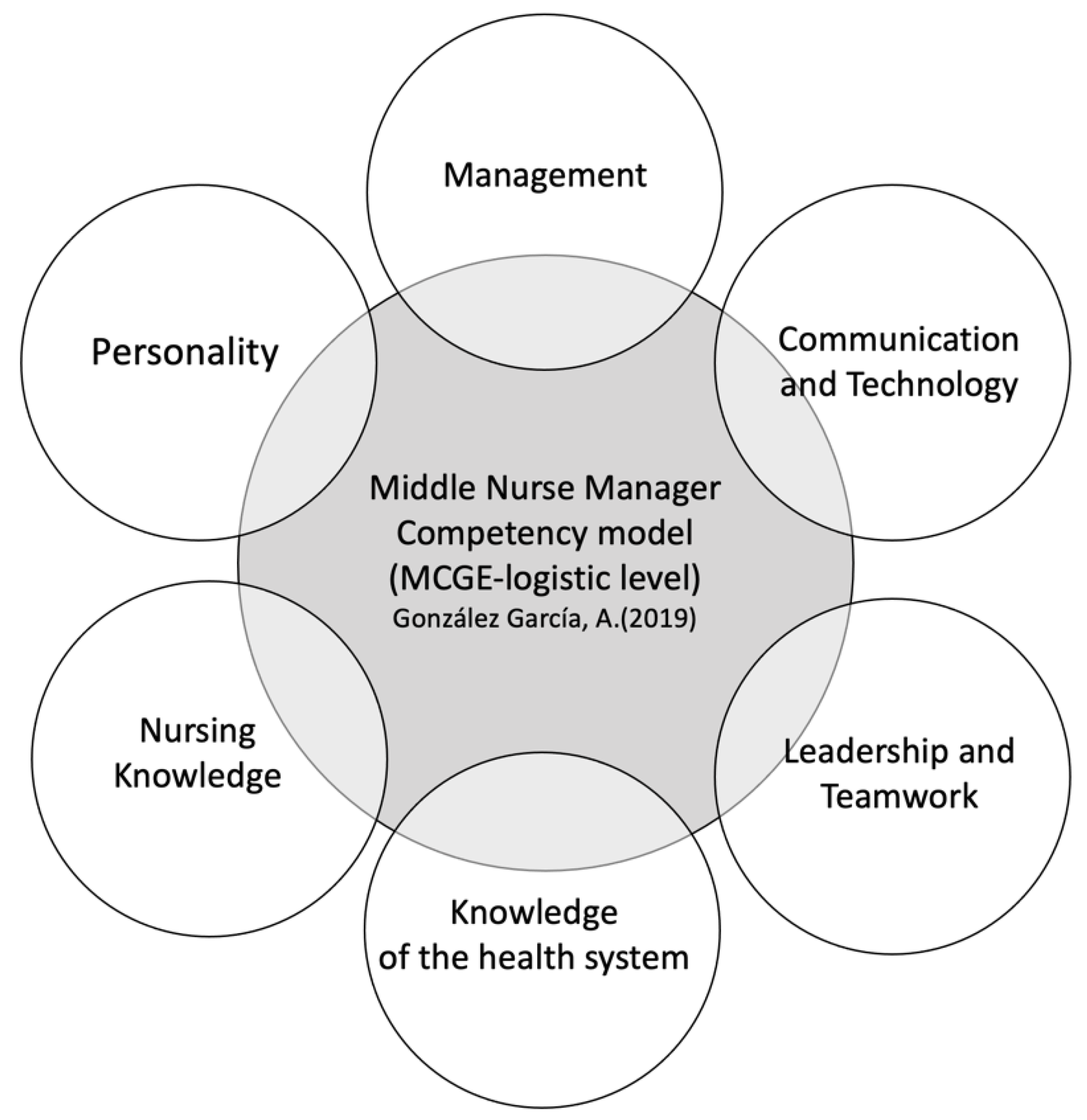
3.2. Model of Competencies for the Middle Nurse Manager
3.3. Principal Component Analysis
4. Discussion
5. Conclusions
Implications for Nursing Management
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leontiou, I.; Merkouris, A.; Papastavrou, E.; Middletton, N. Self-efficacy, empowerment and power of middle nurse managers in Cyprus: A correlational study. J. Nurs. Manag. 2021, 11, 1–11. [Google Scholar]
- Kantanen, K.; Kaunonen, M.; Helminen, M.; Suominen, T. Leadership and management competencies of head nurses and directors of nursing in Finnish social and health care. J. Res. Nurs. 2017, 22, 228–244. [Google Scholar] [CrossRef]
- Cathcart, E.B.; Greenspan, M. A new window into nurse manager development. J. Nurs. Adm. 2012, 42, 557–561. [Google Scholar] [CrossRef]
- Kleinman, S.C. Leadership Roles, Competencies, and Education: How Prepared Are Our Nurse Managers? J. Nurs. Adm. 2003, 33, 451–455. [Google Scholar] [CrossRef]
- Ding, B.; Liu, W.; Tsai, S.B.; Gu, D.; Bian, F.; Shao, X. Effect of patient participation on nurse and patient outcomes in inpatient healthcare. Int. J. Environ. Res. Public Health 2019, 16, 1344. [Google Scholar] [CrossRef]
- Van Dyk, J.; Siedlecki, S.L.; Fitzpatrick, J.J. Frontline nurse managers’ confidence and self-efficacy. J. Nurs. Manag. 2016, 24, 533–539. [Google Scholar] [CrossRef]
- Thorne, S. Nursing now or never. Nurs. Inq. 2019, 26, e12326. [Google Scholar] [CrossRef]
- Aiken, L.H.; Cimiotti, J.P.; Sloane, D.M.; Smith, H.L.; Flynn, L.; Neff, D.F. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med. Care 2011, 49, 1047–1053. [Google Scholar] [CrossRef]
- Savage, C.; Kub, J. Public health and nursing: A natural partnership. Int. J. Environ. Res. Public Health 2009, 6, 2843–2848. [Google Scholar] [CrossRef]
- Whitt, M.; Baird, B.; Wilbanks, P.; Esmail, P. Tracking decisions with shared governance. Nurse Lead. 2011, 9, 53–55. [Google Scholar] [CrossRef]
- Ho, E.; Principi, E.; Cordon, C.P.; Amenudzie, Y.; Kotwa, K.; Holt, S.; Macphee, M. The Synergy Tool: Making Important Quality Gains within One Healthcare Organization. Adm. Sci. 2017, 7, 32. [Google Scholar] [CrossRef]
- McHugh, G.A.; Horne, M.; Chalmers, K.I.; Luker, K.A. Specialist community nurses: A critical analysis of their role in the management of long-term conditions. Int. J. Environ. Res. Public Health 2009, 6, 2550–2567. [Google Scholar] [CrossRef]
- Seabold, K.; Sarver, W.; Kline, M.; McNett, M. Impact of intensive leadership training on nurse manager satisfaction and perceived importance of competencies. Nurs. Manag. 2020, 51, 34–42. [Google Scholar] [CrossRef]
- Duffield, C.; Gardner, G.; Doubrovsky, A.; Wise, S. Manager, clinician or both? Nurse managers’ engagement in clinical care activities. J. Nurs. Manag. 2019, 27, 1538–1545. [Google Scholar] [CrossRef]
- Kodama, Y.; Fukahori, H. Nurse managers’ attributes to promote change in their wards: A qualitative study. Nurs. Open 2017, 4, 209–217. [Google Scholar] [CrossRef]
- Boyatzis, R.E. The Competent Manager: A Model for Effective Performance; John Wiley & Sons: Toronto, ON, Canada, 1982; ISBN 0-471-09031-X. [Google Scholar]
- Groves, K. Talent management best practices: How exemplary health care organizations create value in a down economy. Health Care Manag. Rev. 2011, 3, 227–240. [Google Scholar] [CrossRef]
- Kerfoot, K.M.; Luquire, R. Alignment of the system’s chief nursing officer: Staff or direct line structure? Nurs. Adm. Q. 2012, 36, 325–331. [Google Scholar] [CrossRef]
- MacMillan-Finlayson, S. Competency development for nurse executives: Meeting the challenge. J. Nurs. Adm. 2010, 40, 254–257. [Google Scholar] [CrossRef]
- Yoder-Wise, Y.; Scott, E.; Sullivan, D. Expanding leadership capacity: Educational levels for nurse leaders. J. Nurs. Adm. 2013, 43, 326–328. [Google Scholar] [CrossRef] [PubMed]
- Warshawsky, N.E.; Caramanica, L.; Cramer, E. Organizational Support for Nurse Manager Role Transition and Onboarding: Strategies for Success. J. Nurs. Adm. 2020, 50, 254–260. [Google Scholar] [CrossRef]
- Institute of Medicine of the National Academies. The Future of Nursing: Leading change, advancing health. Rep. Brief 2010, 40, 1–4. [Google Scholar]
- West, M. Evaluation of a nurse leadership development programme. Nurs. Manag. 2016, 22, 1–6. [Google Scholar] [CrossRef]
- Herrin, D.; Jones, K.; Krepper, R.; Sherman, R.; Reineck, C. Future nursing administration graduate curricula, Part 2: Foundation and strategies. J. Nurs. Adm. 2006, 36, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Meadows, M.T.; Dwyer, C. AONE continues to guide leadership expertise with post-acute competencies. Nurse Lead. 2015, 13, 21–25. [Google Scholar] [CrossRef]
- Baxter, C.; Warshawsky, N. Exploring the acquisition of nurse manager competence. Nurse Lead. 2014, 12, 46–59. [Google Scholar] [CrossRef]
- Chase, L.K. Are you confidently competent? Nurs. Manag. 2012, 43, 50–53. [Google Scholar] [CrossRef]
- DeOnna, J. Developing and Validating an Instrument to Measure the Perceived Job Competencies Linked to Performance and Staff Retention of First-Line Nurse Managers Employed in a Hospital Setting. Ph.D. Thesis, The Pennsylvania State University, College of Education, State College, PA, USA, 2006. [Google Scholar]
- Gunawan, J.; Aungsuroch, Y.; Fisher, M.L.; McDaniel, A.M. Development and Psychometric Properties of Managerial Competence Scale for First-Line Nurse Managers in Indonesia. SAGE Open Nurs. 2019, 5, 1–12. [Google Scholar] [CrossRef]
- Gunawan, J.; Aungsuroch, Y.; Fisher, M.L.; McDaniel, A.M. Managerial Competence of First-Line Nurse Managers in Public Hospitals in Indonesia. J. Multidiscip. Healthc. 2020, 13, 1017–1025. [Google Scholar] [CrossRef]
- New, E.G. Reflections A three-tier model of organizational competencies. J. Manag. Psychol. 1996, 11, 44–51. [Google Scholar] [CrossRef]
- Hudak, R.P.; Brooke, P.; Finstuen, K. Identifying management competencies for health care executives: Review of a series of Delphi studies. J. Health Adm. Educ. 2000, 18, 213–219. [Google Scholar]
- Holden, L.; Roberts, I. The depowerment of European middle managers: Challenges and uncertainties. J. Manag. Psychol. 2004, 19, 269–287. [Google Scholar] [CrossRef]
- Lalleman, P.; Smid, G.; Lagerwey, M.D.; Oldenhof, L.; Schuurmans, M.J. Nurse middle managers’ dispositions of habitus a bourdieusian analysis of supporting role behaviors in Dutch and American hospitals. Adv. Nurs. Sci. 2015, 38, E1–E16. [Google Scholar] [CrossRef]
- Scoble, K.B.; Russell, G. Vision 2020, Part I: Profile of the future nurse leader. J. Nurs. Adm. 2003, 33, 324–330. [Google Scholar] [CrossRef]
- AONE. Competencies Assessment. Available online: http://www.aone.org/resources/online-assessments.shtml (accessed on 18 September 2020).
- Carney, M. Understanding organizational culture: The key to successful middle manager strategic involvement in health care delivery? J. Nurs. Manag. 2006, 14, 23–33. [Google Scholar] [CrossRef]
- Engle, R.L.; Lopez, E.R.; Gormley, K.E.; Chan, J.A.; Charns, M.P.; van Deusen Lukas, C. What roles do middle managers play in implementation of innovative practices? Health Care Manag. Rev. 2017, 42, 14–27. [Google Scholar] [CrossRef]
- Ofei, A.M.A.; Paarima, Y.; Barnes, T. Exploring the management competencies of nurse managers in the Greater Accra Region, Ghana. Int. J. Afr. Nurs. Sci. 2020, 13, 100248. [Google Scholar]
- Chase, L. Nurse Manager Competencies; University of Iowa: Iowa City, IA, USA, 2010. [Google Scholar]
- González-García, A. Modelo de Competencias para la Gestora Enfermera; European University of Madrid: Madrid, Spain, 2019. [Google Scholar]
- Gonzalez Garcia, A.; Pinto-Carral, A.; Sanz Villorejo, J.; Marqués-Sánchez, P. Nurse Manager Core Competencies: A Proposal in the Spanish Health System. Int. J. Environ. Res. Public Health 2020, 17, 3173. [Google Scholar] [CrossRef]
- Pillay, R. The skills gap in nursing management in the South African public health sector. Public Health Nurs. 2011, 28, 176–185. [Google Scholar] [CrossRef]
- Meadows, M.T. New Competencies for System Chief Nurse Executives. J. Nurs. Adm. 2016, 46, 235–237. [Google Scholar] [CrossRef]
- Vance, M. Scotland the brave: Statutory supervision transformed. Pract. Midwife 2009, 12, 16–77. [Google Scholar]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. Theory Pract. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Varela-Ruiz, M.; Díaz-Bravo, L.; García-Durán, R. Descripción y usos del método Delphi en investigaciones del área de la salud. Investig. Educ. Méd. 2012, 1, 90–95. [Google Scholar]
- Linstone, H.A.; Turoff, M.; Helmer, O. The Delphi Method; Addison-Wesley: Redeading, MA, USA, 1975; ISBN 0-201-04294-0. [Google Scholar]
- Shirey, M.R. Competencies and tips for effective leadership: From novice to expert. J. Nurs. Adm. 2007, 37, 167–170. [Google Scholar] [CrossRef]
- Sewell, M. Principal Component Analysis; University College London: London, UK, 2008. [Google Scholar]
- Thurstone, L.L. Multiple Factor Analysis, 5th ed.; University of Chicago Press: Chicago, IL, USA, 1957. [Google Scholar]
- Thurstone, L.L. Multiple factor analysis. Psychol. Rev. 1931, 38, 406–427. [Google Scholar] [CrossRef]
- Kaiser, H.F. The Application of Electronic Computers to Factor Analysis. Educ. Psychol. Meas. 1960, 20, 141–151. [Google Scholar] [CrossRef]
- Cattell, R.B. The scree test for the number of factors. Multivar. Behav. Res. 1966, 1, 245–276. [Google Scholar] [CrossRef]
- McCarthy, G.; Fitzpatrick, J.J. Development of a Competency Framework for Nurse Managers in Ireland. J. Contin. Educ. Nurs. 2009, 40, 346–350. [Google Scholar] [CrossRef]
- American Organization of Nurse Executives. AONE Nurse Manager Competencies; The American Organization of Nurse Executives: Chicago, IL, USA, 2015. [Google Scholar]
- Waxman, K.T.; Roussel, L.; Herrin-Griffith, D.; D’Alfonso, J. The AONE Nurse Executive Competencies: 12 Years Later. Nurse Lead. 2017, 15, 120–126. [Google Scholar] [CrossRef]
- Crawford, C.L.; Omery, A.; Spicer, J. An Integrative Review of 21st-Century Roles, Responsibilities, Characteristics, and Competencies of Chief Nurse Executives: A Blueprint for the Next Generation. Nurs. Adm. Q. 2017, 41, 297–309. [Google Scholar] [CrossRef]
- Kuraoka, Y. The relationship between experiential learning and nursing management competency. J. Nurs. Adm. 2019, 49, 99–104. [Google Scholar] [CrossRef]
- Rizany, I.; Hariyati, R.T.S.; Handayani, H. Factors that affect the development of nurses’ competencies: A systematic review. Enferm. Clin. 2018, 28, 154–157. [Google Scholar] [CrossRef]
- American Nurses Credentialing Center. ANCCMagnet Recognition Program. Available online: https://www.nursingworld.org/organizational-programs/%0Dmagnet/ (accessed on 18 September 2020).
- Loreggia, A.; Mattei, N.; Rossi, F.; Venable, K.B. Preferences and Ethical Principles in Decision Making. In Proceedings of the 2018 AAAI/ACM Conference on AI, Ethics and Society-AIES’18, New York, NY, USA, 2–3 February 2018. [Google Scholar]
- Berrios Martos, P.; Lopez Zafra, E.; Aguilar Luzon, M.C.; Auguste, J.M. Relationship between leadership style and attitude toward working groups. Int. J. Psychol. 2008, 43, 444. [Google Scholar]
- Garman, A.N.; Fitz, K.D.; Fraser, M.M. Communication and relations management. J. Healthc. Manag. 2006, 51, 291–294. [Google Scholar]
| Characteristics | Range/Category | Frequency | Percentage |
|---|---|---|---|
| Age | <40 | 10 | 20 |
| 40–50 | 15 | 30 | |
| 51–60 | 18 | 36 | |
| >60 | 7 | 14 | |
| Sex | Female | 32 | 64 |
| Male | 18 | 36 | |
| Education | Master’s degree | 34 | 68 |
| Ph.D | 14 | 28 | |
| Expert group 1 | Minister of Health | 3 | 6.1 |
| Expert group 2 | Head of the Health Department | 5 | 10 |
| Expert group 3 | General Council of Nurses | 3 | 6 |
| Expert group 4 | Scientific Association | 4 | 8 |
| Expert group 5 | Trade Union | 3 | 6 |
| Expert group 6 | General Manager | 5 | 10 |
| Expert group 6 | Medical Director | 2 | 4 |
| Expert group 6 | Nurse Executive | 5 | 10 |
| Expert group 6 | Management Director | 1 | 2 |
| Expert group 7 | Middle Nurse manager | 2 | 4.1 |
| Expert group 8 | Nursing supervisor | 3 | 6.1 |
| Expert group 9 | Nurse | 3 | 6.1 |
| Expert group 9 | Doctor | 2 | 4.1 |
| Expert group 9 | Assistant Nursing Care Technician | 2 | 4.1 |
| Expert group 10 | Nursing Degree Students | 2 | 4.1 |
| Expert group 11 | Research/Teaching | 4 | 8.2 |
| Expert group 12 | Lawyer | 1 | 1 |
| I. Management 1. Analytical thinking (V. COMP) 2. Decision-making (V. COMP) 3. Innovation (V. COMP) 4.Strategic management (V. COMP) 5. Human resources management (V. COMP) 6. Legal aspects (V. COMP) 7. Organizational management (COMP) 8. Result orientation (V. COMP) II. Communication and technology 9. Communication skills (V. COMP) 10. Feedback (V. COMP) 11. Evaluation of information and its sources (V. COMP) 12 Listening (V. COMP) 13. Information systems and computers (EXP) 14. Technology (COMP) 15. English medium level of writing (COMP) III. Leadership and teamwork 16. Relationship management (V. COMP) 17. Leadership (COMP) 18. Career planning (V. COMP) 19. Influence (V. COMP) 20. Change management (V. COMP) 21. Delegation (V. COMP) 22. Conflict management (V. COMP) 23. Ethical principles (V. COMP) 24. Power and empowerment (V. COMP) 25. Critical thinking (EXP) 26. Collaboration and team management skills (V. COMP) 27. Interpersonal relations (EXP) 28. Multi-professional management (V. COMP) 29. Team-building strategies (V. COMP) 30. Talent management (COMP) | IV. Knowledge of the healthcare system 31. Care management systems (V. COMP) 32. User care skills (V. COMP) 33. Health policy (COMP) 34. Identification and responsibility with organization (V. COMP) 35. Knowledge of the health environment (V. COMP) 36. Quality and safety (V. COMP) 37. Quality and improvement processes (V. COMP) V. Nursing knowledge 38. Clinical skills (V. COMP) 39. Standard Nursing Practice (COMP) 40. Nurse Research (COMP) 41. Nursing Theories (COMP) 42. Care Planning (COMP) 43. Nursing training planning (V. COMP) 44. Professionalism (COMP) VI. Personality 45. Serve as a model (V. COMP) 46. Awareness of personal strengths and weaknesses (EXP) 47. Strategic vision (V. COMP) 48. Personal and professional balance (V. COMP) 49. Compassion (V. COMP) 50. Emotional intelligence (V. COMP) 51. Integrity (EXP) |
| Univ. Ext. | Cont. Ed | Univ. Exp. | Univ. Spec. D | Master | Ph.D. | |
|---|---|---|---|---|---|---|
| Novice | 100% | |||||
| Novice Advanced | 90% | 98% | ||||
| Competent | 90% | 90% | 96% | |||
| Very Competent | 96% | 100% | 96% | 96% | ||
| Expert | 96% | 96% |
| Management Dimension | |||||
|---|---|---|---|---|---|
| CP1 | CP2 | CP3 | CP4 | ||
| Result orientation | 0.789 | ||||
| Strategic management | 0.725 | ||||
| Innovation | 0.710 | ||||
| Legal aspects | 0.936 | ||||
| Analytical thinking | 0.554 | ||||
| Organizational management | 0.968 | ||||
| Decision-making | 0.980 | ||||
| Explained variance | 32.325% | 18.075% | 12.822% | 11.569% | |
| Eigenvalue | 2.263 | 1.265 | 0.898 | 0.810 | |
| α Cronbach | 0.631 | ||||
| Communication and Technology Dimension | |||||
| CP1 | CP2 | CP3 | CP4 | ||
| Listening | 0.905 | ||||
| Information systems and computers | 0.679 | ||||
| English medium level of writing | 0.874 | ||||
| Technology | 0.636 | ||||
| Feedback | 0.88 | ||||
| Communication skills | 0.589 | ||||
| Evaluation of information and its sources | 0.826 | ||||
| Explained variance | 31.326% | 17.341% | 16.065% | 13.076% | |
| Eigenvalue | 2.193 | 1.214 | 1.125 | 0.915 | |
| α Cronbach | 0.6 | ||||
| Leadership and Teamwork Dimension | |||||
| CP1 | CP2 | CP3 | CP4 | ||
| Change management | 0.812 | ||||
| Influence | 0.802 | ||||
| Leadership | 0.703 | ||||
| Delegation | 0.696 | ||||
| Collaboration and team management skills | 0.85 | ||||
| Critical thinking | 0.786 | ||||
| Team-building strategies | 0.736 | ||||
| Career planning | 0.707 | ||||
| Ethical principles | 0.885 | ||||
| Power and empowerment | 0.765 | ||||
| Conflict management | 0.936 | ||||
| Explained variance | 46.309% | 12.796% | 10.286% | 8.17% | |
| Eigenvalue | 5.094 | 1.408 | 1.131 | 0.899 | |
| α Cronbach | 0.876 | ||||
| Knowledge of the Healthcare System | |||||
| CP1 | CP2 | ||||
| Quality and safety | 0.971 | ||||
| Quality and improvement processes | 0.948 | ||||
| Identification and responsibility with the organization | 0.917 | ||||
| Health policy | 0.838 | ||||
| Explained variance | 57.954% | 29.970% | |||
| Eigenvalue | 2.318 | 1.199 | |||
| α Cronbach | 0.749 | ||||
| Nursing Knowledge | |||||
| CP1 | |||||
| Nursing training planning | 0.918 | ||||
| Nurse research | 0.910 | ||||
| Nursing theories | 0.822 | ||||
| Clinical skills | 0.777 | ||||
| Explained variance | 73.733% | ||||
| Eigenvalue | 2.949 | ||||
| α Cronbach | 0.808 | ||||
| Personality | |||||
| CP1 | CP2 | ||||
| Awareness of personal strengths and weaknesses | 0.905 | ||||
| Strategic vision | 0.891 | ||||
| Personal and professional balance | 0.836 | ||||
| Compassion | 0.884 | ||||
| Emotional intelligence | 0.735 | ||||
| Explained variance | 54.76% | 21.705% | |||
| Eigenvalue | 2.738 | 1.085 | |||
| α Cronbach | 0.809 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-García, A.; Pinto-Carral, A.; Villorejo, J.S.; Marqués-Sánchez, P. Competency Model for the Middle Nurse Manager (MCGE-Logistic Level). Int. J. Environ. Res. Public Health 2021, 18, 3898. https://doi.org/10.3390/ijerph18083898
González-García A, Pinto-Carral A, Villorejo JS, Marqués-Sánchez P. Competency Model for the Middle Nurse Manager (MCGE-Logistic Level). International Journal of Environmental Research and Public Health. 2021; 18(8):3898. https://doi.org/10.3390/ijerph18083898
Chicago/Turabian StyleGonzález-García, Alberto, Arrate Pinto-Carral, Jesús Sanz Villorejo, and Pilar Marqués-Sánchez. 2021. "Competency Model for the Middle Nurse Manager (MCGE-Logistic Level)" International Journal of Environmental Research and Public Health 18, no. 8: 3898. https://doi.org/10.3390/ijerph18083898
APA StyleGonzález-García, A., Pinto-Carral, A., Villorejo, J. S., & Marqués-Sánchez, P. (2021). Competency Model for the Middle Nurse Manager (MCGE-Logistic Level). International Journal of Environmental Research and Public Health, 18(8), 3898. https://doi.org/10.3390/ijerph18083898







