The Impact of War-Related Stress on Coronary Artery Disease Severity in War Survivors: A SYNTAX Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Sampling Technique
2.2. SYNTAX Score and Angiographic Analysis
2.3. Data Collection
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke statistics—2019 update: A report from the American heart association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef]
- Townsend, N.; Wilson, L.; Bhatnagar, P.; Wickramasinghe, K.; Rayner, M.; Nichols, M. Cardiovascular disease in Europe: Epidemiological update 2016. Eur. Heart J. 2016, 37, 3232–3245. [Google Scholar] [CrossRef]
- Okrainec, K.; Banerjee, D.K.; Eisenberg, M.J. Coronary artery disease in the developing world. Am. Heart J. 2004, 148, 7–15. [Google Scholar] [CrossRef]
- Kurd, B.J.; Dar, M.I.; Shoaib, M.; Malik, L.; Aijaz, Z.; Asif, I. Relationship between stress and coronary heart disease. Asian Cardiovasc. Thorac. Ann. 2013, 22, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Kop, W.J. Acute and chronic psychological risk factors for coronary syndromes: Moderating effects of coronary artery disease severity. J. Psychosom. Res. 1997, 43, 167–181. [Google Scholar] [CrossRef]
- Akosile, W.; Colquhoun, D.; Young, R.; Lawford, B.; Voisey, J. The association between post-traumatic stress disorder and coronary artery disease: A meta-analysis. Australas. Psychiatry 2018, 26, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Edmondson, D.; Richardson, S.; Falzon, L.; Davidson, K.W.; Mills, M.A.; Neria, Y. Posttraumatic Stress Disorder Prevalence and Risk of Recurrence in Acute Coronary Syndrome Patients: A Meta-analytic Review. PLoS ONE 2012, 7, e38915. [Google Scholar] [CrossRef] [PubMed]
- Hani, A.B.; Abu Abeeleh, M.; Al Smady, M.; Shaban, M.; Al Kharabsheh, M.; Al-Tamimi, Z.; Eifert, S. Heart Disease in Adult Syrian Refugees: Experience at Jordan University Hospital. Ann. Glob. Health 2019, 85. [Google Scholar] [CrossRef] [PubMed]
- Maziak, W.; Rastam, S.; Mzayek, F.; Ward, K.D.; Eissenberg, T.; Keil, U. Cardiovascular Health among Adults in Syria: A Model from Developing Countries. Ann. Epidemiol. 2007, 17, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Doctors without Borders. A Silent Crisis: Treating Non-Communicable Diseases in Jordan | Doctors without Borders—USA 2015. Available online: https://www.doctorswithoutborders.org/what-we-do/news-stories/story/silent-crisis-treating-non-communicable-diseases-jordan (accessed on 16 March 2020).
- Sibai, A.; Armenian, H.; Alam, S. Wartime determinants of arteriographically confirmed coronary artery dieases in beirut. J. Epidemiol. 1989, 130, 623–631. [Google Scholar] [CrossRef]
- Rizkalla, N.; Arafa, R.; Mallat, N.; Soudi, L.; Adi, S.; Segal, S. Women in refuge: Syrian women voicing health sequelae due to war traumatic experiences and displacement challenges. J. Psychosom. Res. 2020, 129, 109909. [Google Scholar] [CrossRef]
- Chen, J.; Tang, B.; Lin, Y.; Ru, Y.; Wu, M.; Wang, X.; Chen, Q.; Chen, Y.; Wang, J. Validation of the Ability of SYNTAX and Clinical SYNTAX Scores to Predict Adverse Cardiovascular Events After Stent Implantation: A Systematic Review and Meta-Analysis. Angiology 2016, 67, 820–828. [Google Scholar] [CrossRef]
- Kim, Y.-H.; Park, D.-W.; Kim, W.-J.; Lee, J.-Y.; Yun, S.-C.; Kang, S.-J.; Lee, S.-W.; Lee, C.W.; Park, S.-W.; Park, S.-J. Validation of SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) Score for Prediction of Outcomes After Unprotected Left Main Coronary Revascularization. JACC Cardiovasc. Interv. 2010, 3, 612–623. [Google Scholar] [CrossRef] [PubMed]
- Farooq, V.; Girasis, C.; Magro, M.; Onuma, Y.; Morel, M.A.; Heo, J.H.; García-García, H.; Kappetein, A.P.; Brand, M.V.D.; Holmes, D.R.; et al. The CABG SYNTAX Score—An angiographic tool to grade the complexity of coronary disease following coronary artery bypass graft surgery: From the SYNTAX Left Main Angiographic (SYNTAX-LE MANS) substudy. Eurointervention 2013, 8, 1277–1285. [Google Scholar] [CrossRef] [PubMed]
- Collet, C.; Onuma, Y.; Miyazaki, Y.; Morel, M.-A.; Serruys, P.W. Integration of non-invasive functional assessments with anatomical risk stratification in complex coronary artery disease: The non-invasive functional SYNTAX score. Cardiovasc. Diagn. Ther. 2017, 7, 151–158. [Google Scholar] [CrossRef]
- Caixeta, A.; Généreux, P.; Palmerini, T.; Lansky, A.J.; Mehran, R.; Dangas, G.D.; Xu, K.; Brener, S.J.; Stone, G.W. Prognostic Utility of the SYNTAX Score in Patients With Single Versus Multivessel Disease Undergoing Percutaneous Coronary Intervention (from the Acute Catheterization and Urgent Intervention Triage StrategY [ACUITY] Trial). Am. J. Cardiol. 2014, 113, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Yadav, M.; Palmerini, T.; Caixeta, A.; Madhavan, M.V.; Sanidas, E.; Kirtane, A.J.; Stone, G.W.; Généreux, P. Prediction of Coronary Risk by SYNTAX and Derived Scores: Synergy between percutaneous coronary intervention with taxus and cardiac surgery. J. Am. Coll. Cardiol. 2013, 62, 1219–1230. [Google Scholar] [CrossRef] [PubMed]
- Möller, J.; Theorell, T.; De Faire, U.; Ahlbom, A.; Hallqvist, J. Work related stressful life events and the risk of myocardial infarction. Case-control and case-crossover analyses within the Stockholm heart epidemiology programme (SHEEP). J. Epidemiol. Community Health 2005, 59, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Stewart, R.A.H.; Colquhoun, D.M.; Marschner, S.L.; Kirby, A.C.; Simes, J.; Nestel, P.J.; Glozier, N.; O’Neil, A.; Oldenburg, B.; White, H.D.; et al. Persistent psychological distress and mortality in patients with stable coronary artery disease. Heart 2017, 103, 1860–1866. [Google Scholar] [CrossRef] [PubMed]
- Krantz, D.S.; McCeney, M.K. Effects of Psychological and Social Factors on Organic Disease: A Critical Assessment of Research on Coronary Heart Disease. Annu. Rev. Psychol. 2002, 53, 341–369. [Google Scholar] [CrossRef]
- Ho, R.C.M.; Neo, L.F.; Chua, A.N.C.; Cheak, A.A.C.; Mak, A. Research on psychoneuroimmunology: Does stress influence immunity and cause coronary artery disease? Ann. Acad. Med. Singap. 2010, 39, 191–196. [Google Scholar] [PubMed]
- Rozanski, A.; Blumenthal, J.A.; Kaplan, J. Impact of Psychological Factors on the Pathogenesis of Cardiovascular Disease and Implications for Therapy. Circulation 1999, 99, 2192–2217. [Google Scholar] [CrossRef] [PubMed]
- Ramachandruni, S.; Handberg, E.; Sheps, D.S. Acute and chronic psychological stress in coronary disease. Curr. Opin. Cardiol. 2004, 19, 494–499. [Google Scholar] [CrossRef]
- O’Neal, W.T.; Hammadah, M.; Sandesara, P.B.; Almuwaqqat, Z.; Samman-Tahhan, A.; Gafeer, M.M.; Abdelhadi, N.; Wilmot, K.; Al Mheid, I.; Bremner, D.J.; et al. The association between acute mental stress and abnormal left atrial electrophysiology. J. Cardiovasc. Electrophysiol. 2017, 28, 1151–1157. [Google Scholar] [CrossRef]
- Bremner, J.D.; Campanella, C.; Khan, Z.; Shah, M.; Hammadah, M.; Wilmot, K.; Al Mheid, I.; Lima, B.B.; Garcia, E.V.; Nye, J.; et al. Brain Correlates of Mental Stress-Induced Myocardial Ischemia. Psychosom. Med. 2018, 80, 515–525. [Google Scholar] [CrossRef]
- Mihatov, S.; Bergovec, M.; Prpić, H.; Heitzler, V.N.; Batarelo, V.; Rogan, S.; Sjerobabski, V.; Gjurasin, M.; Goldner, V.; Radonić, R. Incidence and hospital mortality of acute coronary artery disease among civilians in Zagreb during air-raid alarms. Acta Med. Croat. Cas. Hravatske Akad. Med. Znan. 1995, 49, 49–52. [Google Scholar]
- Nanda, S.; Singh, A.; Agrawal, S.; Gargya, S.; Saluja, S.; Kumar, A.; Kumar, A.; Kalra, K.; Thind, M.; Saluja, S.; et al. Posttraumatic stress disorder after myocardial infarction and coronary artery bypass grafting. Int. J. Crit. Illn. Inj. Sci. 2017, 7, 84–90. [Google Scholar] [CrossRef]
- Tsutsui, T.; Tanaka, H.; Nishida, A.; Asukai, N. Posttraumatic stress symptoms as predictive of prognosis after acute coronary syndrome. Gen. Hosp. Psychiatry 2017, 45, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Vaccarino, V.; Goldberg, J.; Rooks, C.; Shah, A.J.; Veledar, E.; Faber, T.L.; Votaw, J.R.; Forsberg, C.W.; Bremner, J.D. Post-Traumatic Stress Disorder and Incidence of Coronary Heart Disease: A twin study. J. Am. Coll. Cardiol. 2013, 62, 970–978. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Guo, L.; Huang, D.; Wang, L.; Guo, L.; Geng, Q.; Zhang, M. The Role of the Myocardial Microvasculature in Mental Stress-Induced Myocardial Ischemia. Clin. Cardiol. 2016, 39, 234–239. [Google Scholar] [CrossRef]
- Orth-Gomér, K.; Schneiderman, N.; Wang, H.-X.; Walldin, C.; Blom, M.; Jernberg, T. Stress Reduction Prolongs Life in Women With Coronary Disease: The Stockholm women’s intervention trial for coronary heart disease (SWITCHD). Circ. Cardiovasc. Qual. Outcomes 2009, 2, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Frasure-Smith, N.; Lespérance, F.; Juneau, M. Differential long-term impact of in-hospital symptoms of psychological stress after non-Q-wave and Q-wave acute myocardial infarction. Am. J. Cardiol. 1992, 69, 1128–1134. [Google Scholar] [CrossRef]

| Variables | Category | Low SX Score | Intermediate SX Score | High SX Score | p Value * |
|---|---|---|---|---|---|
| Gender | Male | 10 (14.9%) | 10 (14.9%) | 47 (70.1%) | 0.90 |
| Female | 18 (75.0%) | 3 (12.5%) | 3 (12.5%) | ||
| Age (Years) | 18–44 | 11 (84.6%) | 1 (7.7%) | 1 (7.7%) | 0.45 |
| 45–64 | 41 (70.7%) | 10 (17.2%) | 7 (12.1%) | ||
| ≥65 | 13 (65.0%) | 2 (10.0%) | 5 (25.0%) | ||
| BMI | Normal | 15 (75%) | 2 (10.0%) | 3 (15.0%) | 0.94 |
| Overweight | 25 (67.6%) | 6 (16.2%) | 6 (16.2%) | ||
| Obese | 25 (73.5%) | 5 (14.7%) | 4 (11.8%) | ||
| Location of residence | Urban | 53 (72.6%) | 10 (13.7%) | 10 (13.7%) | 0.88 |
| Refugee Camp | 12 (66.7%) | 3 (16.7%) | 3 (16.7%) | ||
| Income † | Low < 300 | 57 (70.4%) | 12 (14.8%) | 12 (14.8%) | 0.81 |
| Intermediate 300–600 | 8 (80.0%) | 1 (10.0%) | 1 (10.0%) | ||
| Co-morbidities | Hypertension | 57 (70.4%) | 11 (13.6%) | 13 (16.0%) | 0.37 |
| Diabetes Mellitus | 34 (70.8%) | 5 (10.4%) | 9 (18.8%) | 0.28 | |
| Dyslipidemia | 52 (70.3%) | 11 (14.9%) | 11 (14.9%) | 0.87 | |
| Smoker | 40 (75.5%) | 5 (9.4%) | 8 (15.1%) | 0.29 | |
| Peripheral Arterial Disease | 31 (70.5%) | 5 (11.4%) | 8 (18.2%) | 0.49 | |
| Family History of CAD | 30 (70.9%) | 6 (10.9%) | 10 (18.2%) | 0.27 | |
| History of previous myocardial ischemia | 17 (65.4%) | 3 (11.5%) | 6 (23.1%) | 0.30 | |
| History of previous Percutaneous Coronary Intervention (PCI) | 16 (71.4%) | 13 (14.3%) | 13 (14.3%) | 0.26 |
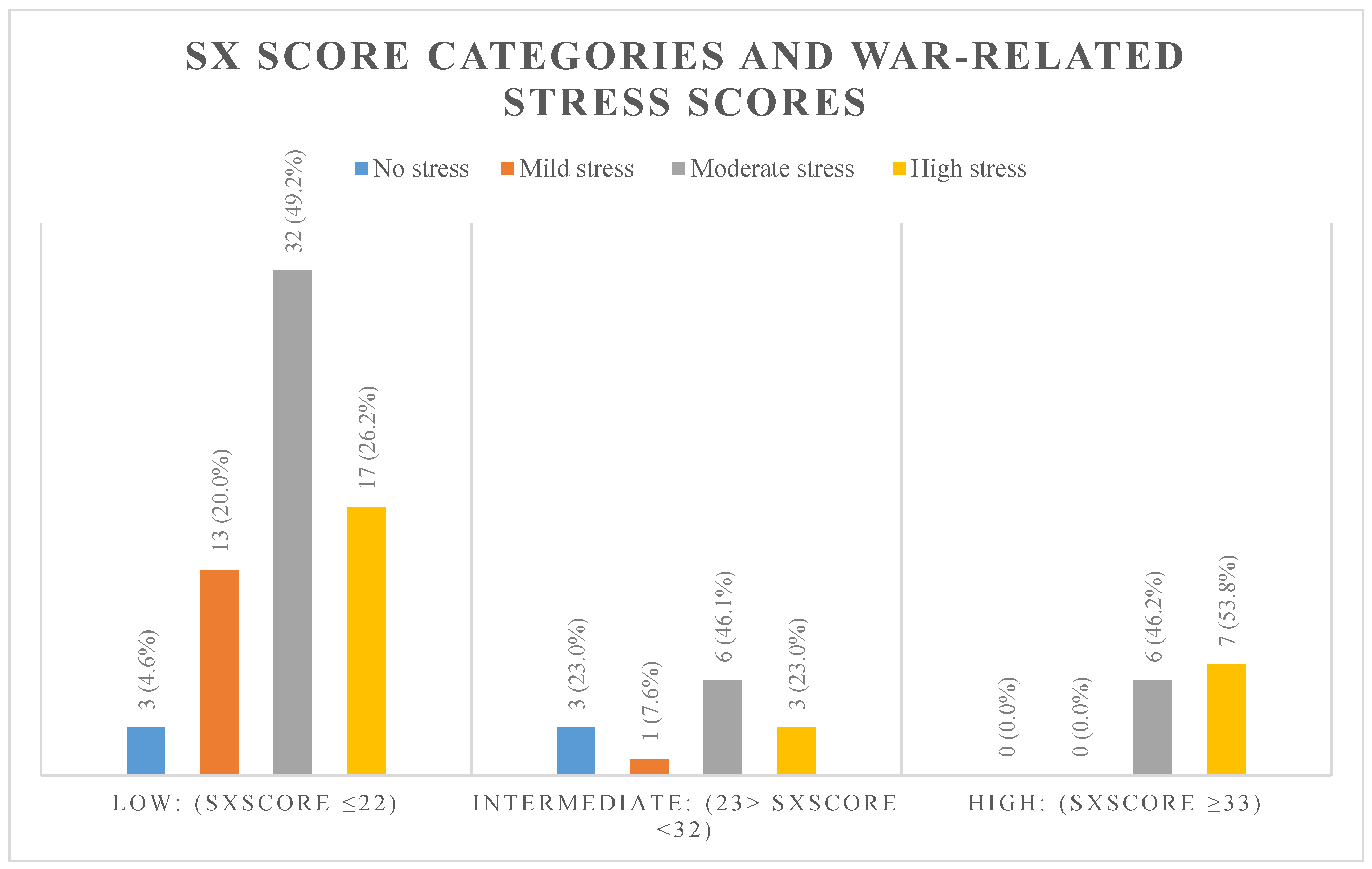
| War Stressors | Total n (%) | Low: (SX Score ≤ 22) | Intermediate: (23 > SX Score < 32) | High: (SX Score ≥ 33) | p Value |
|---|---|---|---|---|---|
| No Stress | 6 (100%) | 3 (50.0%) | 3 (50.0%) | 0 (0.0%) | 0.042 |
| Low Stress | 14 (100%) | 13 (92.9%) | 1 (7.1%) | 0 (0.0%) | |
| Moderate Stress | 44 (100%) | 32 (72.7%) | 6 (13.6%) | 6 (13.6%) | |
| High Stress | 27 (100%) | 17 (63.0%) | 3 (11.1%) | 7 (25.9%) |
| Variable | Beta Coefficient | p-Value | 95% CI |
|---|---|---|---|
| Age | 0.026 | 0.847 | (−) 0.247–0.299 |
| BMI | (−) 0.225 | 0.151 | (−) 0.609–0.098 |
| Smoking status | (−) 6.061 | 0.059 | (−) 11.796–(−) 0.326 |
| Diabetes Mellitus | 0.943 | 0.690 | (−) 3.811–5.698 |
| Hypertension | (−) 3.307 | 0.511 | (−) 13.414–6.801 |
| Dyslipidemia | 3.441 | 0.208 | (−) 2.003–8.885 |
| Family History of CAD | 2.993 | 0.179 | (−) 1.435–7.421 |
| Prior MI | 1.712 | 0.649 | (−) 5.845–9.269 |
| Prior PCI | (−) 0.806 | 0.827 | (−) 8.247–6.635 |
| PAD | (−) 1.938 | 0.467 | (−) 7.279–3.403 |
| War Stressors | 4.411 | 0.004 | 1.496–7.326 |
| 1-vessel disease | (−) 2.770 | 0.559 | (−) 12.304–6.764 |
| 2-vessel disease | 2.193 | 0.664 | (−) 7.958–12.345 |
| 3-vessel disease | 1.229 | 0.816 | (−) 9.383–11.841 |
| Number of stents | (−) 1.069 | 0.494 | (−) 4.208–2.070 |
| Lesions ≥ 20 mm | (−) 2.294 | 0.377 | (−) 7.495–2.908 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Makhamreh, H.; Alkhulaifat, D.; Al-Ani, A.; Mafrachi, B.; Saadeh, A.; Al-Ani, H.; Bani Hani, A.; AlRyalat, S.A. The Impact of War-Related Stress on Coronary Artery Disease Severity in War Survivors: A SYNTAX Study. Int. J. Environ. Res. Public Health 2021, 18, 3233. https://doi.org/10.3390/ijerph18063233
Al-Makhamreh H, Alkhulaifat D, Al-Ani A, Mafrachi B, Saadeh A, Al-Ani H, Bani Hani A, AlRyalat SA. The Impact of War-Related Stress on Coronary Artery Disease Severity in War Survivors: A SYNTAX Study. International Journal of Environmental Research and Public Health. 2021; 18(6):3233. https://doi.org/10.3390/ijerph18063233
Chicago/Turabian StyleAl-Makhamreh, Hanna, Dana Alkhulaifat, Abdallah Al-Ani, Baraa Mafrachi, Aseel Saadeh, Hashim Al-Ani, Amjad Bani Hani, and Saif Aldeen AlRyalat. 2021. "The Impact of War-Related Stress on Coronary Artery Disease Severity in War Survivors: A SYNTAX Study" International Journal of Environmental Research and Public Health 18, no. 6: 3233. https://doi.org/10.3390/ijerph18063233
APA StyleAl-Makhamreh, H., Alkhulaifat, D., Al-Ani, A., Mafrachi, B., Saadeh, A., Al-Ani, H., Bani Hani, A., & AlRyalat, S. A. (2021). The Impact of War-Related Stress on Coronary Artery Disease Severity in War Survivors: A SYNTAX Study. International Journal of Environmental Research and Public Health, 18(6), 3233. https://doi.org/10.3390/ijerph18063233








