Health Services Use and Health Outcomes among Informal Economy Workers Compared with Formal Economy Workers: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Eligibility Criteria
2.2.1. Types of Populations and Exposures
2.2.2. Types of Comparators
2.2.3. Types of Outcomes
2.2.4. Types of Studies
2.3. Data Extraction
2.4. Assessment of Risk of Bias
2.5. Evidence Synthesis
2.6. Quality of Evidence Assessment
3. Results
3.1. Study Selection
3.2. Characteristics of Included Studies
3.3. Risk of Bias
| Included Study | Selection Bias | Lack of Blinding | Exposure Misclassification | Outcome Misclassification | Incomplete Exposure Data | Incomplete Outcome Data | Selective Reporting of Exposures | Selective Reporting of Outcome | Differences in Numerator and Denominator | Conflict of Interest |
|---|---|---|---|---|---|---|---|---|---|---|
| Any health services use | ||||||||||
| Giatti 2008 * [22] | + | + | + | + | + | + | + | + | ++ | + |
| Giatti 2011 [23] | + | + | + | + | + | + | + | + | ++ | + |
| Le 2015 [24] | - | + | - | + | + | + | ++ | + | ||
| Miquillan 2013 [25] | ++ | + | + | + | + | + | ++ | + | ||
| Fatal occupational injuries | ||||||||||
| Lopez- Bonilla 2011 [26] | + | + | ++ | - | - | + | -- | + | + | |
| Mora 2011 [27] | + | + | + | + | -- | + | - | + | + | |
| Non-fatal occupational injuries | ||||||||||
| Cunningham 2012 [28] | - | + | ++ | + | ++ | - | ++ | - | - | + |
| Calys-Tagoe 2017 [29] | - | + | - | ++ | - | ++ | + | - | + | |
| Santana 2003 [30] | + | + | + | ++ | + | + | + | - | ++ | + |
| Depression | ||||||||||
| Abbas 2013 [31] | + | + | ++ | ++ | ++ | ++ | + | ++ | + | |
| Da Silva 2006 a [32] | - | + | - | + | + | ++ | + | ++ | + | + |
| Giatti 2008 * [22] | + | + | + | + | + | + | + | + | ++ | + |
| Musculoskeletal disorders | ||||||||||
| Da Silva 2006 b [33] | - | + | - | + | ++ | + | + | + | + | + |
3.4. Findings
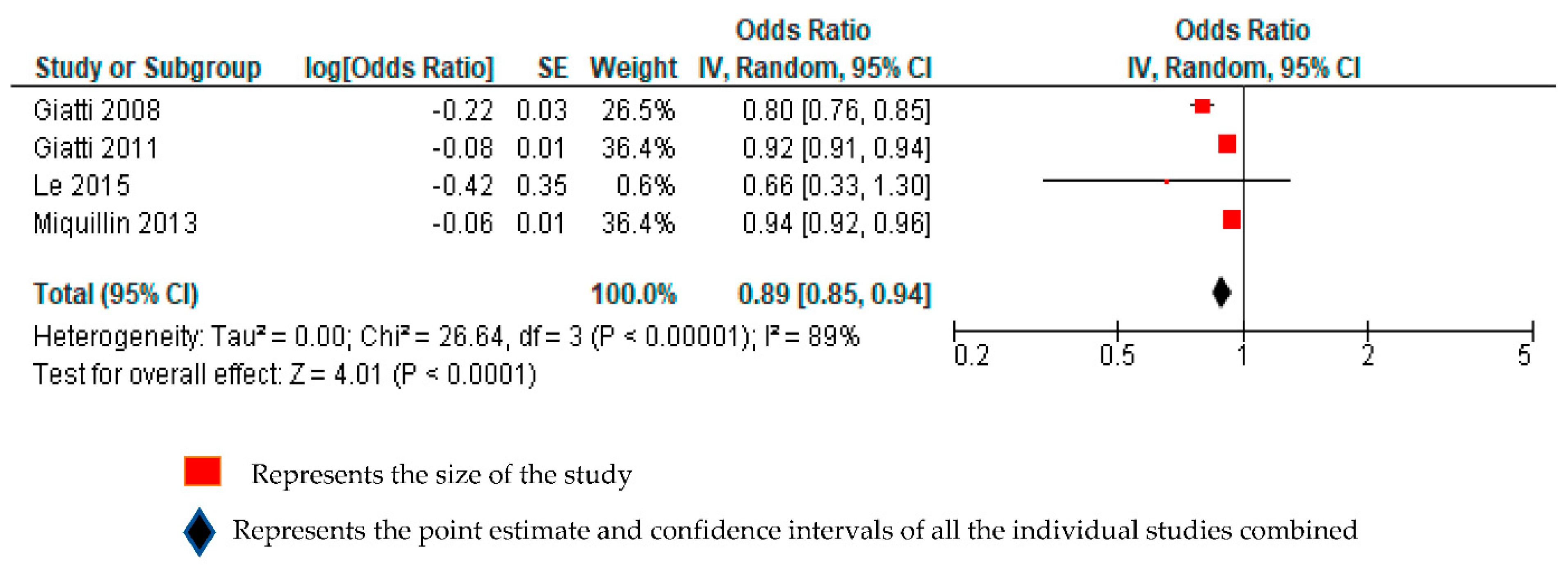
3.4.1. Any Health Services Use
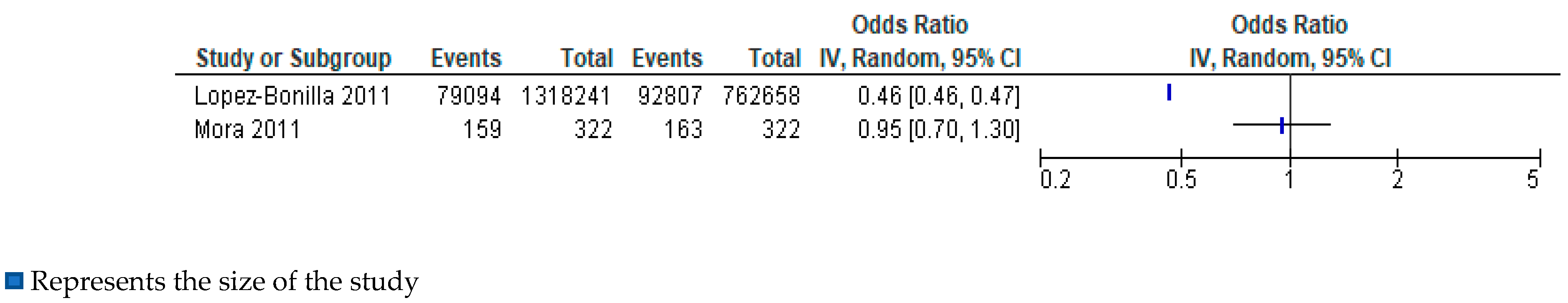
3.4.2. Fatal Occupational Injuries
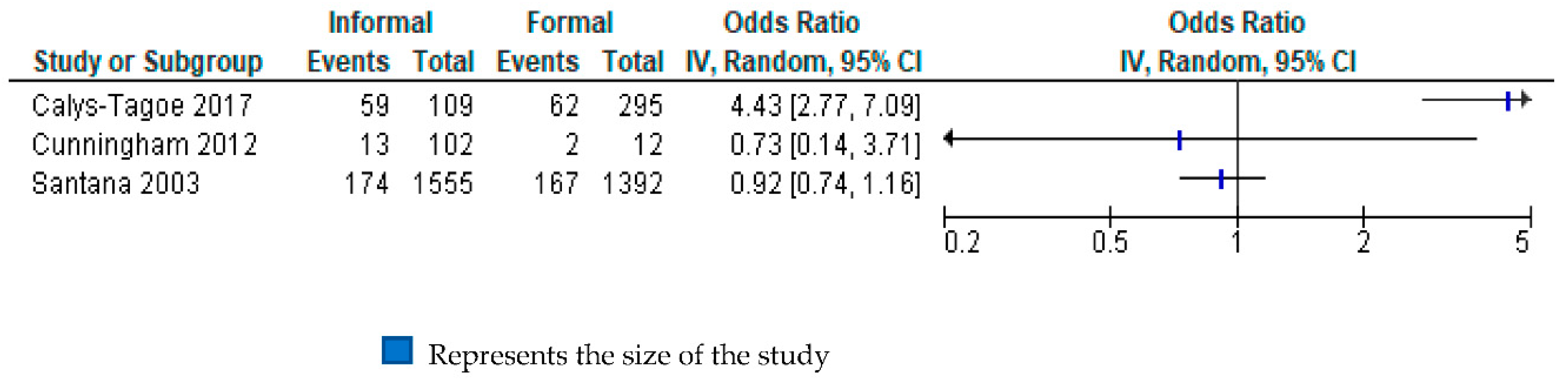
3.4.3. Non-Fatal Occupational Injuries
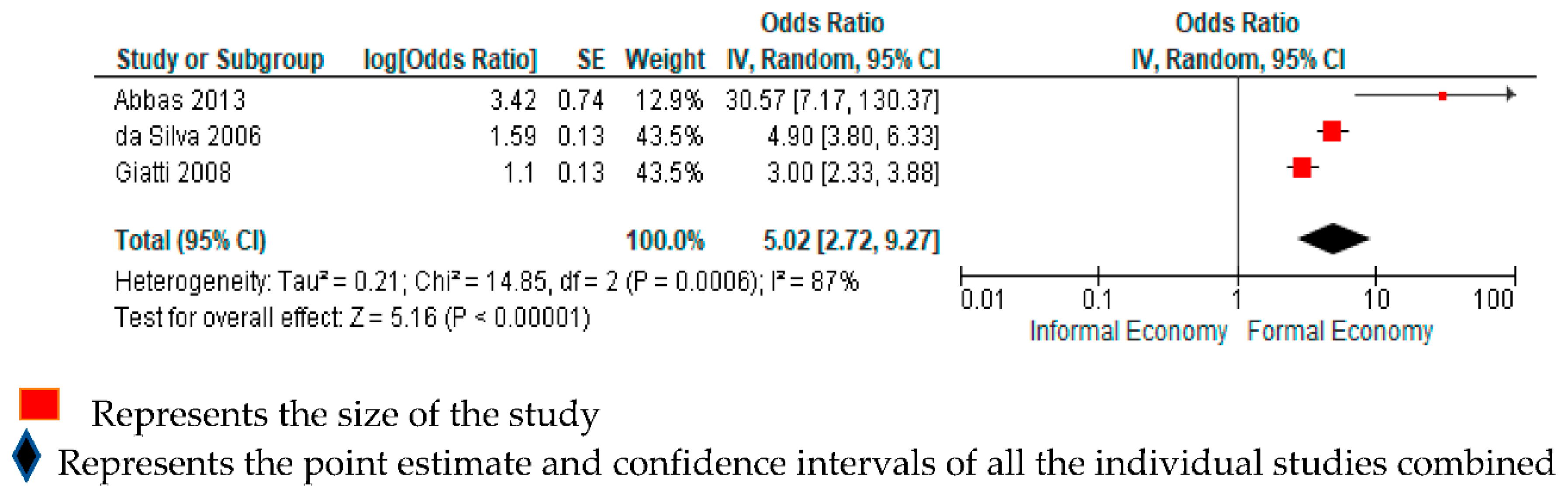
3.4.4. Depression
3.4.5. Musculoskeletal Disorders
4. Discussion
4.1. Summarised Findings
4.2. Comparison with Other Evidence
4.3. Limitations and Research Considerations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- International Labour Organization. Women and Men in the Informal Economy: A Statistical Picture, 3rd ed.; International Labour Organization: Geneva, Switzerland, 2018. [Google Scholar]
- International Labour Organization. Informal Economy. Available online: https://www.ilo.org/ilostat-files/Documents/description_IFL_EN.pdf (accessed on 30 March 2020).
- Naidoo, R.N.; Kessy, F.M.; Mlingi, L.; Petersson, N.; Mirembo, J. Occupational health and safety in the informal sector in southern Africa- the WAHSA project in Tanzania and Mozambique. Occup. Health S. Afr. 2009, 15, 46–50. [Google Scholar]
- Commission on the Social Determinants of Health. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Alfers, L.; Rogan, M. Health risks and informal employment in South Africa: Does formality protect health? Int. J. Occup. Environ. Health 2015, 21, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Akazili, J.; Chatio, S.; Ataguba, J.E.; Agorinya, I.; Kanmiki, E.W.; Sankoh, O.; Oduro, A. Informal workers’ access to health care services: Findings from a qualitative study in the Kassena- Nankana districts of Northern Ghana. BMC Int. Health Hum. Rights 2018, 18, 20. [Google Scholar] [CrossRef] [PubMed]
- Batool, Z.; Akram, M.; Anjum, F.; Faiz, S.; Ibrahim, M. Occupational hazards and health status of trash picker children in Faisalabad city, Punjab, Pakistan. Mediterr. J. Soc. Sci. 2015, 6, 590. [Google Scholar] [CrossRef][Green Version]
- Harris, B.; Goudge, J.; Ataguba, J.E.; McIntyre, D.; Nxumalo, N.; Jikwana, S.; Chersich, M. Inequities in access to health care in South Africa. J. Public Health Policy 2011, 32, 102–123. [Google Scholar] [CrossRef] [PubMed]
- Kistan, J.; Ntlebi, V.; Made, F.; Kootbodien, T.; Wilson, K.; Tlotleng, N.; Kgalamono, S.; Mathee, A.; Naicker, N. Health care access of informal waste recyclers in Johannesburg, South Africa. PLoS ONE 2020, 15, e0235173. [Google Scholar] [CrossRef] [PubMed]
- Chattopadhyay, O. Safety and Health of Urban Informal Sector Workers. Indian J. Community Med. 2005, 30, 46–48. [Google Scholar]
- Santana, V.S.; Loomis, D. Informal jobs and non-fatal occupational injuries. Ann. Occup. Hyg. 2004, 48, 147–157. [Google Scholar]
- Silpasuwan, P.; Prayomyong, S.; Sujitrat, D.; Suwan-Ampai, P. Cotton dust exposure and resulting respiratory disorders among home-based garment workers. Workplace Health Saf. 2016, 64, 95–102. [Google Scholar] [CrossRef]
- Santana, V.S.; Loomis, D.; Newman, B.; Harlow, S.D. Informal jobs: Another Occupational Hazard for Women’s Mental Health? Int. J. Epidemiol. 1997, 26, 1236–1242. [Google Scholar] [CrossRef] [PubMed]
- Robinson, T.; Whittaker, J.; Acharya, A.; Singh, D.; Smith, M. Prevalence of noise-induced hearing loss among woodworkers in Nepal: A pilot study. Int. J. Occup. Environ. Health 2015, 21, 14–22. [Google Scholar] [CrossRef] [PubMed]
- PRISMA. Transparent Reporting of Systematic Reviews and Meta-Analyses. Available online: http://www.prisma-statement.org/ (accessed on 18 March 2020).
- Morgan, R.L.; Whaley, P.; Thayer, K.A.; Schünemann, H.J. Identifying the PECO: A framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ. Int. 2018, 121, 1027–1031. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6908441/ (accessed on 30 March 2020). [CrossRef]
- Hussmanns, R. Defining and Measuring Informal Employment; International Labour Office: Geneva, Switzerland, 2003; Available online: https://www.ilo.org/public/english/bureau/stat/download/papers/meas.pdf (accessed on 15 December 2019).
- World Health Organization. Handbook on Health Inequality Monitoring with a Special Focus on Low- and Middle-Income Countries; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Pega, F.; Norris, S.L.; Backes, C.; Bero, L.A.; Descatha, A.; Gagliardi, D.; Godderis, L.; Loney, T.; Modenese, A.; Morgan, R.L.; et al. RoB-SPEO: A tool for assessing risk of bias in studies estimating the prevalence of exposure to occupational risk factors from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2020, 135, e105039. [Google Scholar] [CrossRef] [PubMed]
- Hulshof, C.T.J.; Pega, F.; Neupane, S.; van der Molen, H.F.; Colosio, C.; Daams, J.G.; Descatha, A.K.c.P.; Kuijer, P.P.F.M.; Mandic-Rajcevic, S.; Masci, F.; et al. The prevalence of occupational exposure to ergonomic risk factors: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021, 146, e106157. [Google Scholar] [CrossRef] [PubMed]
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. (Eds.) GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. Updated October 2013. The GRADE Working Group. 2013. Available online: https://gdt.gradepro.org/app/handbook/handbook.html (accessed on 5 August 2020).
- Miquilin, I.D.O.C.; Marín-Leon, L.; Monteiro, M.I.; Filho, H.R.C. Inequalities in health services access and use among formal, informal, and unemployed workers, based on data from the Brazilian National Household Sample Survey, 2008. Cad. Saúde Pública Rio De Jan. 2013, 29, 1392–1406. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, R.N.; Simpson, C.D.; Keifer, M.C. Hazards faced by informal recyclers in the squatter communities of Aunción, Paraguay. Int. J. Occup. Environ. Health 2012, 18, 181187. [Google Scholar] [CrossRef] [PubMed]
- Mora, A.M.; Mora-Mora, M.G.; Partanen, T.; Wesseling, C. Registration of fatal occupational injuries in Costa Rica, 2005–2006. Int. J. Occup. Environ. Health 2011, 17, 243–250. [Google Scholar] [CrossRef]
- López-Bonilla, I.M.; Flores-Urbina, L.; Partanen, T.; Wesseling, C. Fatal occupational injuries in Nicaragua, 2005. Int. J. Occup. Environ. Health 2011, 17, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Giatti, L.; Barreto, S.M. Labour market status and use of healthcare services in Brazil. Ciĕncia Saúde Coletiva 2011, 16, 3817–3827. [Google Scholar] [CrossRef]
- Giatti, L.; Barreto, S.M.; César, C.C. Informal work, unemployment and health in Brazilian metropolitan areas, 1998 and 2003. Cad. Saúde Pública Rio De Jan. 2008, 24, 2396–2406. [Google Scholar] [CrossRef]
- Da Silva, M.C.; Fassa, A.C.; Kriebel, D. Minor psychiatric disorders among Brazillian ragpickers: A cross-sectional study. Environ. Health A Glob. Access Sci. Source 2006, 5, 17. [Google Scholar]
- Da Silva, M.C.; Fassa, A.G.; Kriebel, D. Musculosketal pain in ragpickers in a southern city in Brazil. Am. J. Ind. Med. 2006, 49, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Santana, V.; Mata, A.P.; Carvalho, C.; Luz, G. Non-fatal occupational injuries: Gender and job contract differences. Cad. Saúde Pública Rio De Jan. 2003, 19, 481–493. [Google Scholar] [CrossRef] [PubMed]
- Calys-Tagoe, B.N.L.; Clarke, E.; Robins, T.; Basu, N. A comparison of licensed and un-licensed artisanal and small-scale gold miners (ASGM) in terms of socio-demographics, work profiles, and injury rates. BMC Public Health 2017, 17, 682. [Google Scholar] [CrossRef] [PubMed]
- Abbas, R.A.; Hmmam, R.A.M.; El-Gohary, S.S.; Sabik, L.M.E.; Hunter, M.S. Screening for common mental disorders and substance abuse among temporary hired cleaners in Egyptian governmental hospitals, Zagazig City, Sharqia Governorate. Int. J. Occup. Environ. Med. 2013, 4, 13–24. [Google Scholar] [PubMed]
- Le, A.T.K.; Vu, L.H.; Schelling, E. Utilization of health care services among internal migrants in Hanoi and its correlation with health insurance: A cross-sectional study. Tap Chi Y Te Cong Cong 2015, 3, 44–56. [Google Scholar] [PubMed]
- Abaerei, A.A.; Ncayiyana, J.; Levin, J. Health-care utilization and associated factors in Gauteng Province, South Africa. Glob. Health Action 2017, 10, 1305765. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Dupre, M.E.; Qui, L.; Zhou, W.; Zhoa, Y.; Gu, D. Age and sex differences in the association between access to medical care and health outcomes among older Chinese. BMC Health Serv. Res. 2018, 18, 1004. [Google Scholar] [CrossRef] [PubMed]
- Hard, D.L.; Myers, J.R.; Gerberich, S.G. Traumatic Injuries in Agriculture. NASD: Human Health Effects of Agriculture: Phyisical Diseases and Illnesses 2001. Available online: https://nasdonline.org/static_content/documents/1828/d001773.pdf (accessed on 21 July 2020).
- Cardenas, V.M.; Cen, R.; Clemens, M.M.; Conner, J.L.; Victory, J.L.; Stallones, L.; Delongchamp, R.R. Morbidity and mortality from farm tractor and other agricultural machinery-related injuries in arkansas. J. Agric. Saf. Health 2018, 24, 213–225. [Google Scholar] [CrossRef]
- Nakua, E.K.; Owusu-Dabo, E.; Newton, S.; Koranteng, A.; Otupiri, E.; Donkor, P.; Mock, C. Injury rate and risk factors among small-scale gold miners in Ghana. BMC Public Health 2018, 19, 1368. [Google Scholar] [CrossRef] [PubMed]
- Jennings, N. Addressing labour and social issues in small-scale mining. In The Socio-Economic Impacts of Artisanal and Small-Scale Mining in Developing Countries; August Aimé Balkema: Rotterdam, The Netherlands, 2003; pp. 151–160. [Google Scholar]
- International Labor Organization. Social and Labour Issues in Small-Scale Mines. Report for Discussion at the Tripartite Meeting on Social and Labour Issues in Small-Scale Mines; International Labor Organization: Geneva, Switzerland, 1999. [Google Scholar]
- Ludermir, A.B.; Lewis, G. Informal work and common mental disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2003, 38, 485–489. [Google Scholar] [CrossRef]
- Llosa, J.A.; Menéndez-Espina, S.; Agulló-Tomás, E.; Rodríguez-Suárez, J. Job insecurity and mental health: A meta-analytical review of the consequences of precarious work in clinical disorders. An. De Psicol. 2018, 34, 211–223. [Google Scholar]
- Leung, M.W.; Yen, I.H.; Meredith Minkler, M. Community-based participatory research: A promising approach for increasing epidemiology’s relevance in the 21st century. Int. J. Epidemiol. 2004, 33, 499–506. [Google Scholar] [CrossRef] [PubMed]

| No | Outcome in This Review | Relevant Sustainable Development Goals Indicator |
|---|---|---|
| 1 | Has used any health service | 3.8.1 Coverage of essential health services (defined as the average coverage of essential services based on tracer interventions that include reproductive, maternal, newborn and child health, infectious diseases, non-communicable diseases and service capacity and access, among the general and the most disadvantaged population) |
| 2 | Has used any occupational safety and health service | |
| 3 | Has died from an occupational injury | 8.8.1 Frequency rates of fatal and non-fatal occupational injuries, by sex and migrant status |
| 4 | Has had any non-fatal occupational injury | |
| 5 | Has human immunodeficiency virus infection | 3.3.1 Number of new HIV infections per 1000 uninfected population, by sex, age and key populations |
| 6 | Has tuberculosis | 3.3.2 Tuberculosis incidence per 1000 population |
| 7 | Has depression | 3.4.2 Suicide mortality rate |
| 8 | Has any musculoskeletal disorder | - |
| 9 | Has noise induced hearing loss (NIHL) | - |
| 10 | Has respiratory infections | 3.4.1 Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease |
| No | First Author | Year of Publication | Country | Study Design | Year of Data Collection | Outcome of Interest | Population | Sex | Occupation | Total Workers in Informal Economy (IE) | Number of Cases in IE | Number of Non-Cases in IE | Total Workers in Formal Economy (FE) | Number of Cases in FE | Number of Non-Cases in FE | Point Estimate (SE) [Ref FE Workers] | 95% CI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Giatti [22] | 2008 | Brazil | Cross sectional | 2003 | Health services use | 32,887 | Male | Multiple | 8255 | 3599 * | 4656 * | 16,673 | 9554 * | 7119 * | OR 0.60 (0.03) | 0.56–0.64 |
| 2 | Giatti [23] | 2011 | Brazil | Cross sectional | 2008 | Health services use | 31,331 | Male | Multiple | 10,185 | 5052 | 5133 | 21,146 | 13,089 | 8057 | OR 0.83 (0.05) | 0.81–0.85 |
| 3 | Le [24] | 2015 | Vietnam | Cross sectional | x | Health services use | 1800 | Both | Multiple | 210 | 120 | 90 | 340 | 213 | 127 | OR 0.38 (0.35) | 0.19–0.74 |
| 4 | Miquillan [25] | 2013 | Brazil | Cross sectional | 2008 | Health services use | 152,233 | Both | Multiple | 62,612 | 54,347 | 8265 | 76,246 | 65,267 | 10,979 | OR 0.86 (0.01) | 0.84–0.89 |
| *5 | Lopez- Bonilla [26] | 2011 | Nicaragua | Cross sectional | 2005 | Fatal occupational injuries | 2,080,899 | Both | Multiple | 1,318,241 | 79,094 | 1,239,147 | 762,658 | 92,807 | 669,851 | OR 0.49 | |
| *6 | Mora [27] | 2011 | Costa Rica | Cross sectional | 2005/2006 | Fatal occupational injuries | x | Both | Multiple | x | 159 | x | x | 163 | x | OR 1.05 | |
| *7 | Cunningham [28] | 2012 | Paraguay | Cross sectional | 2009 | Non-fatal occupational injuries | 114 | Both | Waste recyclers | 102 | 13 | 89 | 12 | 2 | 10 | OR 0.76 | |
| 8 | Calys-Tagoe [29] | 2017 | Ghana | Cross sectional | 2014 | Non-fatal occupational injuries | 404 | Both | Small Scale Miners | 109 | 59 | 50 | 295 | 62 | 233 | OR 0.64 | 0.32–1.18 |
| 9 | Santana [30] | 2003 | Brazil | Cross sectional | 2000 | Non-fatal occupational injuries | 2947 | Both | Multiple | 1555 | 174 | 1381 | 1392 | 167 | 1225 | OR 0.92 | 0.74–1.16 |
| 10 | Abbas [31] | 2013 | Egypt | Cross sectional | 2012 | Depression | 451 | Both | Cleaners | 242 | 143 | 99 | 209 | 62 | 147 | OR 3.4 | 2.27–5.17 |
| 11 | Da Silva [32] | 2006 a | Brazil | Cross sectional | 2004 | Depression | 881 | Both | Waste recyclers | 441 | 197 | 244 | 440 | 148 | 292 | OR 1.4 | 1.2–1.7 |
| 1 | Giatti [22] | 2008 | Brazil | Cross sectional | 2003 | Depression | 32,887 | Male | Multiple | 8255 | x | x | 16,673 | x | x | OR 1.1 | 0.87–1.39 |
| 12 | Da Silva [33] | 2006 b | Brazil | Cross sectional | 2004 | Musculoskeletal disorders | 254 | Both | Waste recyclers | 441 | 61 | 380 | 44 | 25 | 415 | PR LBP 1.1 PR ULP 1.1 PR LLP 0.9 | 0.9–1.1 1.0–1.3 0.8–1.1 |
| Population: Informal Economy Workers Setting: Any Country, Occupation, Industrial Sector and Workplace Comparator: Formal Economy Workers in the Same Country | ||||||
|---|---|---|---|---|---|---|
| Outcomes | Anticipated Absolute Risk * (95% CI) | Relative Difference (95% CI) | No of Participants (No of Studies) | Quality of the Evidence (GRADE) | Comments | |
| Risk among Formal Economy Workers | Risk among Informal Economy Workers | |||||
| Has used any health services | 770 per 1000 | 749 per 1000 (740 to 759) | OR 0.89 (0.85 to 0.94) | 195667 (4 studies) | ⊕⊕⊝⊝ Low—a,b,c | Informal economy workers may be less likely to have used any health service, compared with formal economy workers. |
| Has used any occupational safety and health services | - | - | - | - | - | No evidence available on this outcome. |
| Has died from an occupational injury | - | - | - | 15650750 (2 studies) |  Very low—a,b,d,e | We are very uncertain about the estimate for this outcome. |
| Has had any non-fatal occupational injury | - | - | - | 3465 (2 studies) |  Very Low—a,b,d,f,g | We are very uncertain about the estimate for this outcome. |
| Has depression | 20 per 1000 | 92 per 1000 (52 to 158) | OR 5.02 (2.72 to 9.27) | 26260 (3 studies) | ⊕⊕⊝⊝ Low—b,g | Informal economy workers may be more likely to have depression, compared with formal economy workers. |
| Has any musculoskeletal disorder | - | - | - | 881 (1 study) |  Very Low—b,g | We are very uncertain about the estimate for this outcome. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naicker, N.; Pega, F.; Rees, D.; Kgalamono, S.; Singh, T. Health Services Use and Health Outcomes among Informal Economy Workers Compared with Formal Economy Workers: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 3189. https://doi.org/10.3390/ijerph18063189
Naicker N, Pega F, Rees D, Kgalamono S, Singh T. Health Services Use and Health Outcomes among Informal Economy Workers Compared with Formal Economy Workers: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(6):3189. https://doi.org/10.3390/ijerph18063189
Chicago/Turabian StyleNaicker, Nisha, Frank Pega, David Rees, Spo Kgalamono, and Tanusha Singh. 2021. "Health Services Use and Health Outcomes among Informal Economy Workers Compared with Formal Economy Workers: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 6: 3189. https://doi.org/10.3390/ijerph18063189
APA StyleNaicker, N., Pega, F., Rees, D., Kgalamono, S., & Singh, T. (2021). Health Services Use and Health Outcomes among Informal Economy Workers Compared with Formal Economy Workers: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(6), 3189. https://doi.org/10.3390/ijerph18063189






