Pragmatic Quasi-Experimental Controlled Trial Evaluating the Outcomes of Blended CBT Compared to Face-to-Face CBT and Treatment as Usual for Adolescents with Depressive Disorders
Abstract
1. Background
2. Methods
2.1. Ethics
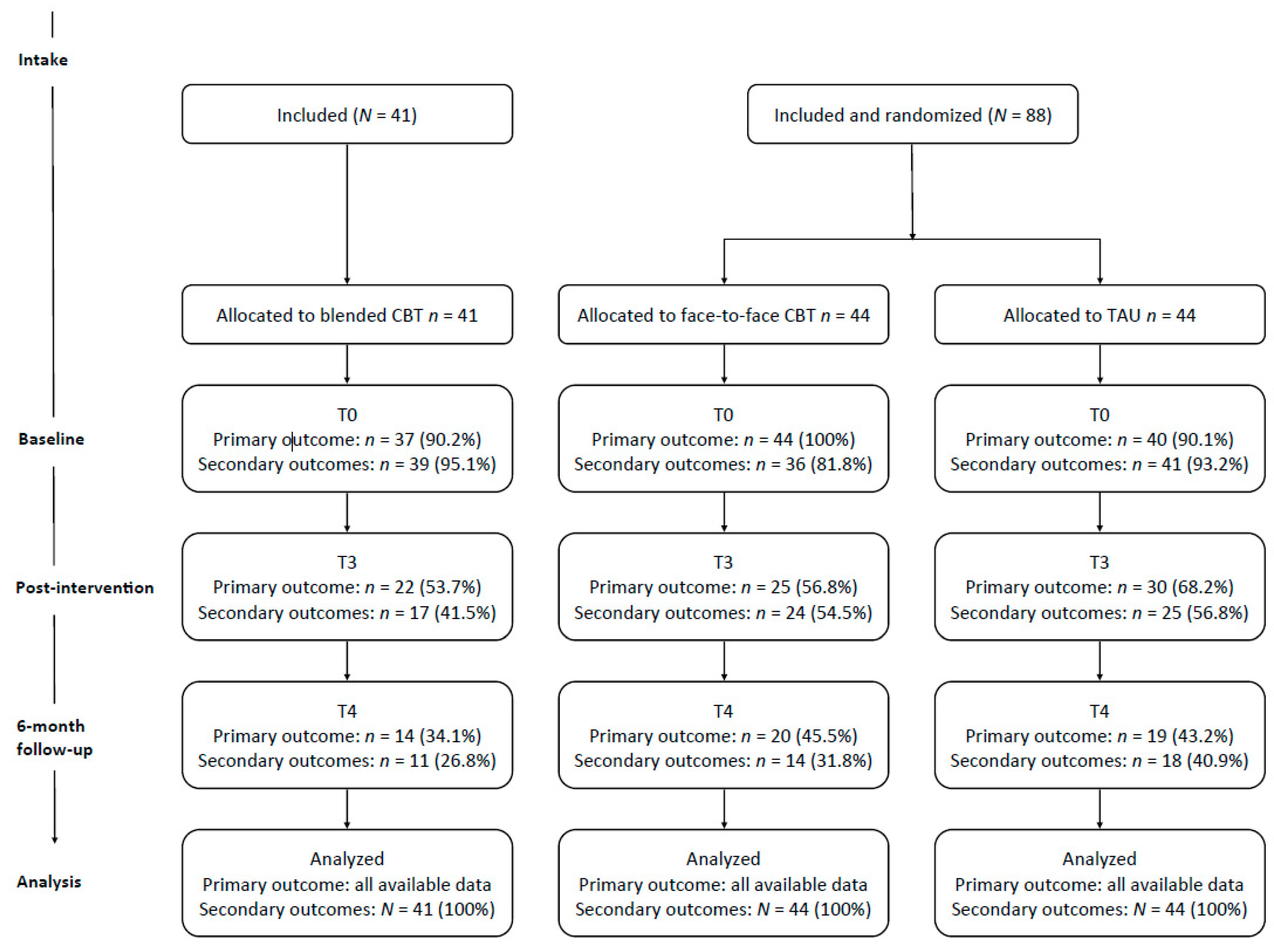
2.2. Design and Procedure
2.3. Sample Size
2.4. Participants
2.5. Treatment Allocation
2.6. Interventions
2.7. Therapists
2.8. Measures
2.8.1. Primary Outcome
2.8.2. Secondary Outcomes
2.9. Missing Data
2.10. Statistical Analysis
3. Results
3.1. Demographics, Clinical Diagnoses and Clinical Characteristics at Baseline
3.2. Drop-Out
3.3. Adverse Events
3.4. Treatment Dosage
3.4.1. Primary Outcome
Remission
3.4.2. Secondary Outcomes
Depressive Symptoms
Change in Depressive Symptoms over Time
Reliable Change in Depressive Symptoms
Other Outcomes
Sensitivity Analyses
4. Discussion
4.1. Strengths and Limitations
4.2. Clinical Implications
4.3. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; WHO Document Production Services: Geneva, Switzerland, 2017. [Google Scholar]
- Ormel, J.; Raven, D.; Van Oort, F.; Hartman, C.A.; Reijneveld, S.A.; Veenstra, R.; Vollebergh, W.A.M.; Buitelaar, J.; Verhulst, F.C.; Oldehinkel, A.J. Mental health in Dutch adolescents: A TRAILS report on prevalence, severity, age of onset, continuity and co-morbidity of DSM disorders. Psychol. Med. 2015, 45, 345–360. [Google Scholar] [CrossRef] [PubMed]
- Birmaher, B.; Brent, D.A.; AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 1503–1526. [Google Scholar] [CrossRef]
- Ryan, N.D. Treatment of depression in children and adolescents. Lancet 2005, 366, 933–940. [Google Scholar] [CrossRef]
- Portzky, G.; Van Heeringen, C. Suïcide bij jongeren. Psychol. Gezondh. 2009, 37, 75–89. [Google Scholar] [CrossRef]
- Jaycox, L.H.; Stein, B.D.; Paddock, S.; Miles, J.N.V.; Chandra, A.; Meredith, L.S.; Tanielian, T.; Hickey, S.; Burnam, M.A. Impact of teen depression on academic, social, and physical functioning. Pediatrics 2009, 124, e596–e605. [Google Scholar] [CrossRef]
- Verboom, C.E.; Sijtsema, J.J.; Verhulst, F.C.; Penninx, B.W.J.H.; Ormel, J. Longitudinal associations between depressive problems, academic performance, and social functioning in adolescent boys and girls. Dev. Psychol. 2014, 50, 247. [Google Scholar] [CrossRef]
- Wickrama, K.A.S.; Conger, R.D.; Lorenz, F.O.; Jung, T. Family antecedents and consequences of trajectories of depressive symptoms from adolescence to young adulthood: A life course investigation. J. Health Soc. Behav. 2008, 49, 468–483. [Google Scholar] [CrossRef]
- Seeley, J.R.; Stice, E.; Rohde, P. Screening for depression prevention: Identifying adolescent girls at high risk for future depression. J. Abnorm. Psychol. 2009, 118, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Ellis, R.E.R.; Seal, M.L.; Simmons, J.G.; Whittle, S.; Schwartz, O.S.; Byrne, M.L.; Allen, N.B. Longitudinal trajectories of depression symptoms in adolescence: Psychosocial risk factors and outcomes. Child Psychiatry Hum. Dev. 2017, 48, 554–571. [Google Scholar] [CrossRef]
- Weisz, J.R.; Kuppens, S.; Eckshtain, D.; Ugueto, A.M.; Hawley, K.M.; Jensen-Doss, A. Performance of evidence-based youth psychotherapies compared with usual clinical care: A multilevel meta-analysis. JAMA Psychiat 2013, 70, 750–761. [Google Scholar] [CrossRef]
- Weisz, J.R.; McCarty, C.A.; Valeri, S.M. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychol. Bull. 2006, 132, 132. [Google Scholar] [CrossRef]
- Cuijpers, P.; Karyotaki, E.; Eckshtain, D.; Ng, M.Y.; Corteselli, K.A.; Noma, H.; Quero, S.; Weisz, J.R. Psychotherapy for depression across different age groups: A systematic review and meta-analysis. JAMA Psychiat 2020, 77, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Klein, J.B.; Jacobs, R.H.; Reinecke, M.A. Cognitive-behavioral therapy for adolescent depression: A meta-analytic investigation of changes in effect-size estimates. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 1403–1413. [Google Scholar] [CrossRef] [PubMed]
- American Psychological Association; Guideline Development Panel for the Treatment of Depressive Disorders. Clinical Practice Guideline for the Treatment of Depression Across Three Age Cohorts; American Psychological Association: Washington, DC, USA, 2019. [Google Scholar]
- Landelijke Stuurgroep Multidisciplinaire Richtlijnontwikkeling in de GGZ. Guidelines for Youth Depression [Richtlijn Voor Depressie Bij Jeugd, Addendum]; Trimbos Institute: Utrecht, The Netherlands, 2009. [Google Scholar]
- Watanabe, N.; Hunot, V.; Omori, I.M.; Churchill, R.; Furukawa, T.A. Psychotherapy for depression among children and adolescents: A systematic review. Acta Psychiatr. Scand. 2007, 116, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Hetrick, S.E.; Cuijpers, P.; Qin, B.; Barth, J.; Whittington, C.J.; Cohen, D.; Del Giovane, C.; Liu, Y.; Michael, K.D. Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: A systematic review and network meta-analysis. World Psychiatry 2015, 14, 207–222. [Google Scholar] [CrossRef]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 2010, 10, 113. [Google Scholar] [CrossRef]
- Ebert, D.D.; Zarski, A.-C.; Christensen, H.; Stikkelbroek, Y.; Cuijpers, P.; Berking, M.; Riper, H. Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: A meta-analysis of randomized controlled outcome trials. PLoS ONE 2015, 10, e0119895. [Google Scholar] [CrossRef] [PubMed]
- Titov, N.; Dear, B.F.; Staples, L.G.; Bennett-Levy, J.; Klein, B.; Rapee, R.M.; Shann, C.; Richards, D.; Andersson, G.; Ritterband, L. MindSpot clinic: An accessible, efficient, and effective online treatment service for anxiety and depression. Psychiatr. Serv. 2015, 66, 1043–1050. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G.; Titov, N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry 2014, 13, 4–11. [Google Scholar] [CrossRef]
- Emmelkamp, P.M.G.; David, D.; Beckers, T.; Muris, P.; Cuijpers, P.; Lutz, W.; Andersson, G.; Araya, R.; Banos Rivera, R.M.; Barkham, M. Advancing psychotherapy and evidence-based psychological interventions. Int. J. Methods Psychiatr. Res. 2014, 23, 58–91. [Google Scholar] [CrossRef]
- Wozney, L.; Huguet, A.; Bennett, K.; Radomski, A.D.; Hartling, L.; Dyson, M.; McGrath, P.J.; Newton, A.S. How do eHealth programs for adolescents with depression work? A realist review of persuasive system design components in internet-based psychological therapies. J. Med. Internet Res. 2017, 19, e266. [Google Scholar] [CrossRef]
- Erbe, D.; Eichert, H.C.; Riper, H.; Ebert, D.D. Blending face-to-face and internet-based interventions for the treatment of mental disorders in adults: Systematic review. J. Med. Internet Res. 2017, 19, e306. [Google Scholar] [CrossRef]
- Van der Vaart, R.; Witting, M.; Riper, H.; Kooistra, L.; Bohlmeijer, E.T.; van Gemert-Pijnen, L.J. Blending online therapy into regular face-to-face therapy for depression: Content, ratio and preconditions according to patients and therapists using a Delphi study. BMC Psychiatry 2014, 14, 355. [Google Scholar] [CrossRef]
- Kooistra, L.C.; Wiersma, J.E.; Ruwaard, J.; van Oppen, P.; Smit, F.; Lokkerbol, J.; Cuijpers, P.; Riper, H. Blended vs. face-to-face cognitive behavioural treatment for major depression in specialized mental health care: Study protocol of a randomized controlled cost-effectiveness trial. BMC Psychiatry 2014, 14, 290. [Google Scholar] [CrossRef] [PubMed]
- Mathiasen, K.; Andersen, T.E.; Riper, H.; Kleiboer, A.A.M.; Roessler, K.K. Blended CBT versus face-to-face CBT: A randomised non-inferiority trial. BMC Psychiatry 2016, 16, 432. [Google Scholar] [CrossRef]
- Kenter, R.M.F.; Van de Ven, P.M.; Cuijpers, P.; Koole, G.; Niamat, S.; Gerrits, R.S.; Willems, M.; Van Straten, A. Costs and effects of Internet cognitive behavioral treatment blended with face-to-face treatment: Results from a naturalistic study. Internet Interv. 2015, 2, 77–83. [Google Scholar] [CrossRef]
- Cerga-Pashoja, A.; Doukani, A.; Gega, L.; Walke, J.; Araya, R. Added value or added burden? A qualitative investigation of blending internet self-help with face-to-face cognitive behaviour therapy for depression. Psychother. Res. 2020, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Sethi, S. Treating youth depression and anxiety: A randomised controlled trial examining the efficacy of computerised versus face-to-face cognitive behaviour therapy. Aust. Psychol. 2013, 48, 249–257. [Google Scholar] [CrossRef]
- Sethi, S.; Campbell, A.J.; Ellis, L.A. The use of computerized self-help packages to treat adolescent depression and anxiety. J. Technol. Hum. Serv. 2010, 28, 144–160. [Google Scholar] [CrossRef]
- Kobak, K.A.; Mundt, J.C.; Kennard, B. Integrating technology into cognitive behavior therapy for adolescent depression: A pilot study. Ann. Gen. Psychiatry 2015, 14, 37. [Google Scholar] [CrossRef]
- Topooco, N.; Berg, M.; Johansson, S.; Liljethörn, L.; Radvogin, E.; Vlaescu, G.; Nordgren, L.B.; Zetterqvist, M.; Andersson, G. Chat- and internet-based cognitive-behavioural therapy in treatment of adolescent depression: Randomised controlled trial. BJPsych Open 2018, 4, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Topooco, N.; Byléhn, S.; Dahlström Nysäter, E.; Holmlund, J.; Lindegaard, J.; Johansson, S.; Åberg, L.; Bergman Nordgren, L.; Zetterqvist, M.; Andersson, G. Evaluating the Efficacy of Internet-Delivered Cognitive Behavioral Therapy Blended With Synchronous Chat Sessions to Treat Adolescent Depression: Randomized Controlled Trial. J. Med. Internet Res. 2019, 21, e13393. [Google Scholar] [CrossRef]
- Rasing, S.P.A. Blended Treatment for Depressive Disorders in Youth: A Narrative Review. Int. J. Cogn. Ther. 2020, 1–12. [Google Scholar] [CrossRef]
- Rasing, S.P.A.; Stikkelbroek, Y.A.J.; Riper, H.; Dekovic, M.; Nauta, M.H.; Dirksen, C.D.; Creemers, D.H.M.; Bodden, D.H.M. Effectiveness and Cost-Effectiveness of Blended Cognitive Behavioral Therapy in Clinically Depressed Adolescents: Protocol for a Pragmatic Quasi-Experimental Controlled Trial. JMIR Res. Protocols 2019, 8, e13434. [Google Scholar] [CrossRef]
- Stikkelbroek, Y.A.J.; Bodden, D.H.M.; Deković, M.; van Baar, A.L. Effectiveness and cost effectiveness of cognitive behavioral therapy (CBT) in clinically depressed adolescents: Individual CBT versus treatment as usual (TAU). BMC Psychiatry 2013, 13, 314. [Google Scholar] [CrossRef]
- Stikkelbroek, Y.; Vink, G.; Nauta, M.H.; Bottelier, M.A.; Vet, L.J.J.; Lont, C.M.; Van Baar, A.L.; Bodden, D.H.M. Effectiveness and moderators of individual cognitive behavioral therapy versus treatment as usual in clinically depressed adolescents: A randomized controlled trial. Sci. Rep. 2020, 10, 1–13. [Google Scholar]
- Schulz, K.F.; Altman, D.G.; Moher, D.; Consort Group. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. Trials 2010, 11, 32. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2012, 10, 28–55. [Google Scholar] [CrossRef]
- Chan, A.W.; Tetzlaff, J.M.; Altman, D.G.; Laupacis, A.; Gøtzsche, P.C.; Krleža-Jerić, K.; Hróbjartsson, A.; Mann, H.; Dickersin, K.; Berlin, J.A. SPIRIT 2013 statement: Defining standard protocol items for clinical trials. Ann. Intern. Med. 2013, 158, 200–207. [Google Scholar] [CrossRef]
- Andrews, G.; Cuijpers, P.; Craske, M.G.; McEvoy, P.; Titov, N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: A meta-analysis. PLoS ONE 2010, 5, e13196. [Google Scholar] [CrossRef]
- Stikkelbroek, Y.A.J.; Bouman, H.; Cuijpers, P. De Doepressiecursus; Doepressie.nl: Dordrecht, The Netherlands, 2005. [Google Scholar]
- Clarke, G.N.; Lewinsohn, P.M.; Hops, H. Adolescent Coping with Depression Course; Castalia Publishing: Eugene, OR, USA, 1990. [Google Scholar]
- Stikkelbroek, Y.A.J.; Van Dijk, J. D(o)epressie Blended; Jouw Omgeving: Utrecht, The Netherlands, 2013. [Google Scholar]
- Kaufman, J.; Birmaher, B.; Brent, D.A.; Rao, U.M.A.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef]
- Reichart, C.G.; Wals, M.; Hillegers, M. Vertaling K-Sads; HC Rümke Groep: Utrecht, The Netherlands, 2000. [Google Scholar]
- Bodden, D.; Stikkelbroek, Y.; Braet, C. The Child Depression Inventory 2 (CDI-2); Utrecht University Press: Utrecht, The Netherlands, 2016. [Google Scholar]
- Kovacs, M. The Children’s Depression Inventory 2: Manual; Multi-Health Systems, Inc.: North Tonawanda, NY, USA, 2011. [Google Scholar]
- Reynolds, W.M. SIQ, Suicidal Ideation Questionnaire: Professional Manual; Psychological Assessment Resources: Odessa, FL, USA, 1988. [Google Scholar]
- Posner, K.; Brown, G.K.; Stanley, B.; Brent, D.A.; Yershova, K.V.; Oquendo, M.A.; Currier, G.W.; Melvin, G.A.; Greenhill, L.; Shen, S. The Columbia–Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am. J. Psychiatry 2011, 168, 1266–1277. [Google Scholar] [CrossRef]
- Achenbach, T.M. Manual for the Child Behavior Checklist/4-18, YSR, and TRF Profiles; University of Vermont Department of Psychiatry: Burlington, VT, USA, 1991. [Google Scholar]
- Verhulst, F.; Ende, J.; Van der Koot, H. Handleiding Voor de CBCL/4–18; Erasmus University Rotterdam: Rotterdam, The Netherlands, 1996. [Google Scholar]
- Guy, W. ECDEU Assessment Manual for Psychopharmacology; US Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research BranchDivision of Extramural Research Programs: Rockville, MD, USA, 1976. [Google Scholar]
- Shaffer, D.; Gould, M.S.; Brasic, J.; Ambrosini, P.; Fisher, P.; Bird, H.; Aluwahlia, S. A children’s global assessment scale (CGAS). Arch. Gen. Psychiatry 1983, 40, 1228–1231. [Google Scholar] [CrossRef]
- Bunte, T.; Schoemaker, K.; Matthys, W. Children’s Global Assessment Scale (CGAS), Dutch Translation; Utrecht University Press: Utrecht, The Netherlands, 2011. [Google Scholar]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; Wiley: New York, NY, USA, 1987. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing. Available online: https://www.R-project.org (accessed on 16 September 2020).
- Van Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2011, 45, 1–68. [Google Scholar] [CrossRef]
- Bates, D.M.; Maechler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Twisk, J.; Bosman, L.; Hoekstra, T.; Rijnhart, J.; Welten, M.; Heymans, M. Different ways to estimate treatment effects in randomised controlled trials. Contemp. Clin. Trials Commun. 2018, 10, 80–85. [Google Scholar]
- Brown, H.; Prescott, R. Applied Mixed Models in Medicine; John Wiley & Sons: West Sussex, UK, 2014. [Google Scholar]
- Jacobson, N.S.; Truax, P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991, 59, 12–19. [Google Scholar] [CrossRef] [PubMed]
- De Haan, A.M.; Boon, A.E.; De Jong, J.T.V.M.; Hoeve, M.; Vermeiren, R.R.J.M. A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin. Psychol. Rev. 2013, 33, 698–711. [Google Scholar] [CrossRef] [PubMed]
- Schuster, R.; Pokorny, R.; Berger, T.; Topooco, N.; Laireiter, A.R. Advantages and disadvantages of online and blended therapy: Attitudes towards both interventions amongst licensed psychotherapists in Austria. J. Med. Internet Res. 2018, 20, e11007. [Google Scholar] [CrossRef]
- Wampold, B.E. How important are the common factors in psychotherapy? An update. World Psychiatry 2015, 14, 270–277. [Google Scholar] [CrossRef]
- Vernmark, K.; Hesser, H.; Topooco, N.; Berger, T.; Riper, H.; Luuk, L.; Backlund, L.; Carlbring, P.; Andersson, G. Working alliance as a predictor of change in depression during blended cognitive behaviour therapy. Cogn. Behav. Ther. 2019, 48, 285–299. [Google Scholar] [CrossRef] [PubMed]
- Cuijpers, P. Four decades of outcome research on psychotherapies for adult depression: An overview of a series of meta-analyses. Can. Psychol./Psychol. Can. 2017, 58, 7. [Google Scholar] [CrossRef]
- Weisz, J.R.; Krumholz, L.S.; Santucci, L.; Thomassin, K.; Ng, M.Y. Shrinking the gap between research and practice: Tailoring and testing youth psychotherapies in clinical care contexts. Annu. Rev. Clin. Psychol. 2015, 11, 139–163. [Google Scholar] [CrossRef] [PubMed]
- Bonevski, B.; Randell, M.; Paul, C.; Chapman, K.; Twyman, L.; Bryant, J.; Brozek, I.; Hughes, C. Reaching the hard-to-reach: A systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med. Res. Methodol. 2014, 14, 42. [Google Scholar] [CrossRef]
| Blended Cognitive Behavioral Therapy (CBT) (n = 37) | Face-to-Face CBT (n = 44) | Treatment as usual (TAU) (n = 40) | Blended CBT vs. Face-to-Face CBT | Blended CBT vs. TAU | |||
|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | χ2 | p | χ2 | p | |
| Depressive disorder (MDD or Dysthymic disorder) | 37 (100%) | 44 (100%) | 40 (100%) | * | * | ||
| Bipolar disorder | 0 | 0 | 0 | * | * | ||
| Psychotic disorder | 0 | 2 (4.5%) | 0 | 1.72 | 0.19 | * | |
| Panic disorder | 1 (2.7%) | 4 (9.1%) | 1 (2.5%) | 1.42 | 0.23 | 0.003 | 0.96 |
| Social phobia | 1 (2.7%) | 13 (29.5%) | 8 (20.0%) | 10.13 | 0.001 | 5.57 | 0.02 |
| Specific phobia | 1 (2.7%) | 4 (9.1%) | 3 (7.5%) | 1.42 | 0.23 | 0.90 | 0.34 |
| Separation anxiety | 1 (2.7%) | 2 (4.5%) | 2 (5.0%) | 1.91 | 0.66 | 0.27 | 0.60 |
| Generalized Anxiety Disorder | 12 (32.4%) | 14 (31.8%) | 9 (22.5%) | 0.003 | 0.95 | 0.96 | 0.33 |
| Post-Traumatic Stress Disorder (PTSD) | 1 (2.7%) | 3 (6.8%) | 3 (7.5%) | 0.73 | 0.39 | 0.90 | 0.34 |
| Acute Stress Disorder | 0 | 0 | 1 (2.5%) | * | 0.94 | 0.33 | |
| Obsessive Compulsive Disorder (OCD) | 0 | 0 | 0 | * | * | ||
| Anorexia Nervosa | 0 | 1 (2.3%) | 0 | 0.85 | 0.36 | * | |
| Bulimia Nervosa | 0 | 1 (2.3%) | 0 | 0.85 | 0.36 | * | |
| Attention Deficit and Hyperactivity Disorder (ADHD) | 5 (13.5%) | 6 (13.6%) | 5 (12.5%) | 0 | 0.99 | 0.02 | 0.90 |
| Conduct Disorder | 0 | 0 | 0 | * | * | ||
| Oppositional Defiant Disorder (ODD) | 0 | 1 (2.3%) | 1 (2.5%) | 0.85 | 0.36 | 0.94 | 0.33 |
| Tic disorder | 1 (2.7%) | 0 | 0 | 1.20 | 0.27 | 1.10 | 0.30 |
| Blended CBT | Face-to-Face CBT | TAU | Blended CBT vs. Face-to-Face CBT | Blended CBT vs. TAU | |||||
|---|---|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | U | p | d (95% CI) | U | p | d (95% CI) | |
| Depressive symptoms T0 | 25.94 (6.07) | 26.58 (9.45) | 24.73 (7.46) | 746.5 | 0.64 | −0.08 (−0.51, 0.35) | 707.0 | 0.37 | 0.18 (−0.25, 0.60) |
| Depressive symptoms T3 | 18.83 (10.85) | 16.43 (13.79) | 19.03 (11.88) | 141.0 | 0.10 | 0.19 (−0.23, 0.62) | 187.0 | 0.52 | −0.02 (−0.44, 0.41) |
| Depressive symptoms T4 | 14.36 (13.46) | 14.19 (16.63) | 12.61 (13.06) | 60.5 | 0.38 | 0.01 (−0.41, 0.44) | 95.5 | 0.89 | 0.13 (−0.29, 0.56) |
| Suicide risk T0 | 3.53 (3.21) | 4.55 (4.13) | 3.66 (3.40) | 702.0 | 0.40 | −0.27 (−0.70, 0.15) | 672.5 | 0.94 | −0.04 (−0.46, 0.39) |
| Suicide risk T3 | 2.93 (4.11) | 2.52 (4.06) | 3.01 (4.52) | 136.5 | 0.15 | 0.10 (−0.33, 0.53) | 178.5 | 0.57 | −0.02 (−0.45, 0.41) |
| Suicide risk T4 | 1.50 (4.23) | 1.73 (4.24) | 0.90 (2.67) | 71.0 | 0.74 | −0.05 (−0.48, 0.37) | 66.5 | 0.22 | 0.17 (−0.25, 0.60) |
| Internalizing symptoms T0 | 28.20 (9.03) | 29.31 (9.08) | 28.60 (9.13) | 731.0 | 0.48 | −0.12 (−0.55, 0.30) | 800.5 | 0.82 | −0.04 (−0.47, 0.38) |
| Internalizing symptoms T3 | 22.32 (13.51) | 20.41 (14.98) | 22.05 (15.15) | 161.0 | 0.40 | 0.13 (−0.29, 0.56) | 188.5 | 0.77 | 0.02 (−0.41, 0.44) |
| Internalizing symptoms T4 | 17.86 (19.01) | 16.03 (14.95) | 17.60 (15.38) | 66.0 | 0.56 | 0.11 (−0.32, 0.53) | 118.0 | 0.58 | 0.02 (−0.41, 0.44) |
| Externalizing symptoms T0 | 11.01 (7.17) | 13.43 (9.85) | 12.63 (8.09) | 784.0 | 0.19 | −0.28 (−0.71, 0.15) | 876.0 | 0.33 | −0.21 (−0.64, 0.21) |
| Externalizing symptoms T3 | 9.87 (12.50) | 11.55 (10.33) | 10.55 (11.34) | 247.0 | 0.13 | −0.15 (−0.57, 0.28) | 251.5 | 0.17 | −0.06 (−0.48, 0.37) |
| Externalizing symptoms T4 | 7.38 (10.21) | 7.89 (8.56) | 8.18 (9.69) | 101.0 | 0.20 | −0.05 (−0.48, 0.37) | 135.5 | 0.19 | −0.08 (−0.51, 0.35) |
| Severity of depression T0 | 4.16 (1.02) | 4.16 (1.01) | 3.93 (1.36) | 663.0 | 0.34 | 0.00 (−0.43, 0.42) | 686.5 | 0.56 | 0.19 (−0.24, 0.62) |
| Severity of depression T3 | 2.72 (1.85) | 2.53 (1.87) | 2.38 (1.53) | 310.0 | 0.66 | 0.10 (−0.33, 0.53) | 286.0 | 0.15 | 0.20 (−0.23, 0.63) |
| Global functioning T0 | 50.88 (7.32) | 49.67 (10.03) | 49.24 (10.08) | 740.0 | 1.00 | 0.14 (−0.29, 0.56) | 613.0 | 0.35 | 0.19 (−0.24, 0.61) |
| Global functioning T3 | 60.85 (18.52) | 62.51 (17.82) | 64.15 (14.23) | 337.0 | 0.74 | −0.09 (−0.52, 0.33) | 381.0 | 0.47 | −0.20 (−0.63, 0.23) |
| Blended CBT vs. Face-to-Face CBT | Blended CBT vs. TAU | |||||
|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | |
| Suicide risk T3 | 0.68 | 0.66 | 0.30 | −0.01 | 0.66 | 0.97 |
| Suicide risk T4 | 0.05 | 0.65 | 0.94 | 0.69 | 0.66 | 0.29 |
| Internalizing symptoms T3 | 2.07 | 2.26 | 0.36 | 0.44 | 2.27 | 0.85 |
| Internalizing symptoms T4 | 1.98 | 2.24 | 0.38 | 0.39 | 2.27 | 0.86 |
| Externalizing symptoms T3 | −0.94 | 1.57 | 0.55 | −0.21 | 1.56 | 0.89 |
| Externalizing symptoms T4 | 0.26 | 1.56 | 0.87 | −0.35 | 1.57 | 0.82 |
| Severity of depression T3 | 0.19 | 0.29 | 0.52 | 0.32 | 0.30 | 0.28 |
| Global functioning T3 | −1.91 | 2.60 | 0.46 | −3.69 | 2.58 | 0.15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rasing, S.P.A.; Stikkelbroek, Y.A.J.; den Hollander, W.; Riper, H.; Deković, M.; Nauta, M.H.; Creemers, D.H.M.; Immink, M.C.P.; Spuij, M.; Bodden, D.H.M. Pragmatic Quasi-Experimental Controlled Trial Evaluating the Outcomes of Blended CBT Compared to Face-to-Face CBT and Treatment as Usual for Adolescents with Depressive Disorders. Int. J. Environ. Res. Public Health 2021, 18, 3102. https://doi.org/10.3390/ijerph18063102
Rasing SPA, Stikkelbroek YAJ, den Hollander W, Riper H, Deković M, Nauta MH, Creemers DHM, Immink MCP, Spuij M, Bodden DHM. Pragmatic Quasi-Experimental Controlled Trial Evaluating the Outcomes of Blended CBT Compared to Face-to-Face CBT and Treatment as Usual for Adolescents with Depressive Disorders. International Journal of Environmental Research and Public Health. 2021; 18(6):3102. https://doi.org/10.3390/ijerph18063102
Chicago/Turabian StyleRasing, Sanne P.A., Yvonne A.J. Stikkelbroek, Wouter den Hollander, Heleen Riper, Maja Deković, Maaike H. Nauta, Daan H.M. Creemers, Marianne C.P. Immink, Mariken Spuij, and Denise H.M. Bodden. 2021. "Pragmatic Quasi-Experimental Controlled Trial Evaluating the Outcomes of Blended CBT Compared to Face-to-Face CBT and Treatment as Usual for Adolescents with Depressive Disorders" International Journal of Environmental Research and Public Health 18, no. 6: 3102. https://doi.org/10.3390/ijerph18063102
APA StyleRasing, S. P. A., Stikkelbroek, Y. A. J., den Hollander, W., Riper, H., Deković, M., Nauta, M. H., Creemers, D. H. M., Immink, M. C. P., Spuij, M., & Bodden, D. H. M. (2021). Pragmatic Quasi-Experimental Controlled Trial Evaluating the Outcomes of Blended CBT Compared to Face-to-Face CBT and Treatment as Usual for Adolescents with Depressive Disorders. International Journal of Environmental Research and Public Health, 18(6), 3102. https://doi.org/10.3390/ijerph18063102






