Patients’ Perspectives about Lifestyle Behaviors and Health in the Context of Family Medicine: A Cross-Sectional Study in Portugal
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Definition of the Variables of Lifestyle
2.3.1. Diet
2.3.2. Physical Activity
2.3.3. Alcohol Consumption
2.3.4. Tobacco Use
2.3.5. Illicit Drugs
2.3.6. Sleep Habits
2.3.7. Screen Activities
2.3.8. Stress
2.3.9. Being Sedentary
2.4. Statistical Analysis
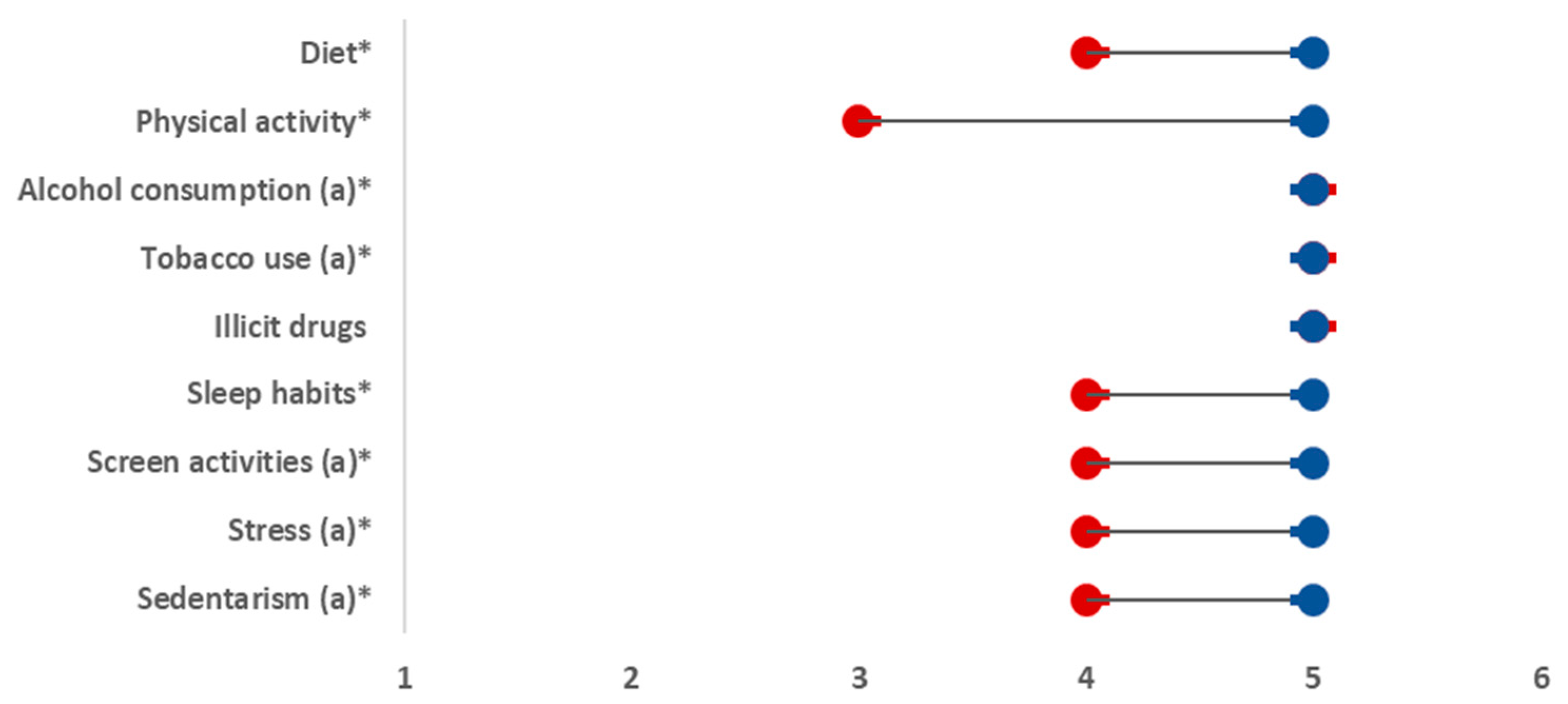
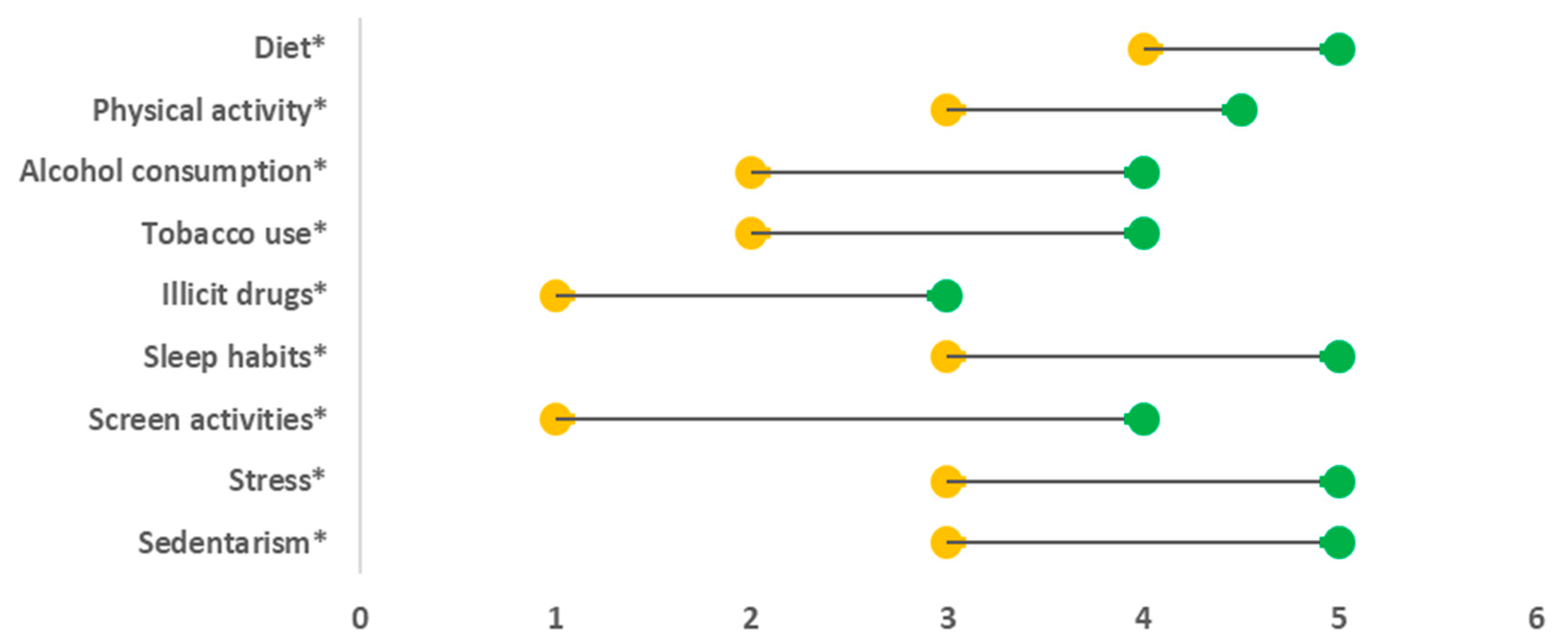
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Leading Causes of Death in Europe: Fact Sheet. 2012. Available online: http://www.euro.who.int/__data/assets/pdf_file/0004/185215/Leading-causes-of-death-in-Europe-Fact-Sheet.pdf (accessed on 17 July 2020).
- World Health Organization. Noncommunicable Diseases. Fact sheet. 2017. Available online: http://www.who.int/mediacentre/factsheets/fs355/en/ (accessed on 17 July 2020).
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases: 2013–2020. 2013. Available online: http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf (accessed on 25 February 2020).
- Lianov, L. Physician Competencies for Prescribing Lifestyle Medicine. JAMA 2010, 304, 202. [Google Scholar] [CrossRef]
- Kushner, R.F.; Mechanick, J.I. Lifestyle Medicine—An Emerging New Discipline. US Endocrinol. 2015, 11, 36. Available online: http://www.touchendocrinology.com/articles/lifestyle-medicine-emerging-new-discipline (accessed on 17 July 2020).
- World Health Organization. First Global Ministerial Conference on Healthy Lifestyles and Noncommunicable Disease Control 2011. Available online: http://www.un.org/en/ga/president/65/issues/moscow_declaration_en.pdf (accessed on 17 July 2020).
- Egger, G.J.; Binns, A.F.; Rossner, S.R. The emergence of ‘lifestyle medicine’ as a structured approach for management of chronic disease. Med. J. Aust. 2009, 190, 143–145. [Google Scholar] [CrossRef]
- WONCA EUROPE Edition. The European Definition of General Practice/Family Medicine; WHO Europe Office: Barcelona, Spain, 2011. [Google Scholar]
- Nahrendorf, M.; Swirski, F.K. Lifestyle Effects on Hematopoiesis and Atherosclerosis. Circ. Res. 2015, 116, 884–894. [Google Scholar] [CrossRef]
- Egger, G. Defining a Structure and Methodology for the Practice of Lifestyle Medicine. Am. J. Lifestyle Med. 2018, 12, 396–403. [Google Scholar] [CrossRef]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M. Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [PubMed]
- Hambrecht, R.; Walther, C.; Möbius-Winkler, S.; Gielen, S.; Linke, A.; Conradi, K.; Erbs, S.; Kluge, R.; Kendziorra, K.; Sabri, O.; et al. Percutaneous Coronary Angioplasty Compared with Exercise Training in Patients With Stable Coronary Artery Disease: A Randomized Trial. Circulation 2004, 109, 1371–1378. [Google Scholar] [CrossRef]
- Jenkins, D.J.A.; Jones, P.J.H.; Lamarche, B.; Kendall, C.W.C.; Faulkner, D.; Cermakova, L.; Gigleux, I.; Ramprasath, V.; De Souza, R.; Ireland, C.; et al. Effect of a Dietary Portfolio of Cholesterol-Lowering Foods Given at 2 Levels of Intensity of Dietary Advice on Serum Lipids in Hyperlipidemia: A Randomized Controlled Trial. JAMA 2011, 306, 831–839. Available online: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2011.1202 (accessed on 10 May 2020). [CrossRef] [PubMed]
- Lawrence, M.; Kerr, S.; McVey, C.; Godwin, J. The Effectiveness of Secondary Prevention Lifestyle Interventions Designed to Change Lifestyle Behavior following Stroke: Summary of a Systematic Review. Int. J. Stroke 2012, 7, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Razavi, M.; Fournier, S.; Shepard, D.S.; Ritter, G.; Strickler, G.K.; Stason, W.B. Effects of Lifestyle Modification Programs on Cardiac Risk Factors. PLoS ONE 2014, 9, e114772. [Google Scholar] [CrossRef] [PubMed]
- Demark-Wahnefried, W.; Rock, C.L.; Patrick, K.; Byers, T. Lifestyle interventions to reduce cancer risk and improve outcomes. Am. Fam. Physician 2008, 77, 1573–1578. [Google Scholar]
- LoConte, N.K.; Gershenwald, J.E.; Thomson, C.A.; Crane, T.E.; Harmon, G.E.; Rechis, R. Lifestyle Modifications and Policy Implications for Primary and Secondary Cancer Prevention: Diet, Exercise, Sun Safety, and Alcohol Reduction. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 88–100. [Google Scholar] [CrossRef]
- Ambrosino, N.; Bertella, E. Lifestyle interventions in prevention and comprehensive management of COPD. Breathe 2018, 14, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Colditz, G.A.; Philpott, S.E.; Hankinson, S.E. The Impact of the Nurses’ Health Study on Population Health: Prevention, Translation, and Control. Am. J. Public Health 2016, 106, 1540–1545. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Bergmann, M.M.; Kröger, J.; Schienkiewitz, A.; Weikert, C.; Boeing, H. Healthy Living Is the Best Revenge: Findings from the European Prospective Investigation Into Cancer and Nutrition–Potsdam Study. Arch. Intern. Med. 2009, 169, 1355. [Google Scholar] [PubMed]
- Larsson, S.C.; Tektonidis, T.G.; Gigante, B.; Åkesson, A.; Wolk, A. Healthy Lifestyle and Risk of Heart Failure: Results from 2 Prospective Cohort Studies. Circ. Heart Fail. 2016, 9. [Google Scholar] [CrossRef] [PubMed]
- Åkesson, A.; Larsson, S.C.; Discacciati, A.; Wolk, A. Low-Risk Diet and Lifestyle Habits in the Primary Prevention of Myocardial Infarction in Men. J. Am. Coll. Cardiol. 2014, 64, 1299–1306. [Google Scholar] [CrossRef] [PubMed]
- van Dammen, L.; Wekker, V.; de Rooij, S.R.; Groen, H.; Hoek, A.; Roseboom, T.J. A systematic review and meta-analysis of lifestyle interventions in women of reproductive age with overweight or obesity: The effects on symptoms of depression and anxiety: Lifestyle interventions and symptoms of depression and anxiety. Obes. Rev. 2018, 19, 1679–1687. [Google Scholar] [CrossRef]
- Glechner, A.; Keuchel, L.; Affengruber, L.; Titscher, V.; Sommer, I.; Matyas, N.; Wagner, G.; Kien, C.; Klerings, I.; Gartlehner, G. Effects of lifestyle changes on adults with prediabetes: A systematic review and meta-analysis. Prim. Care Diabetes 2018, 12, 393–408. [Google Scholar] [CrossRef]
- Pattyn, N.; Cornelissen, V.A.; Eshghi, S.R.T.; Vanhees, L. The Effect of Exercise on the Cardiovascular Risk Factors Constituting the Metabolic Syndrome: A Meta-Analysis of Controlled Trials. Sports Med. 2013, 43, 121–133. [Google Scholar] [CrossRef]
- Yamaoka, K.; Tango, T. Effects of lifestyle modification on metabolic syndrome: A systematic review and meta-analysis. BMC Med. 2012, 10, 138. Available online: http://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-10-138 (accessed on 17 July 2020). [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.F.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M. The 2017 American College of Cardiology/American Heart Association Clinical Practice Guideline for High Blood Pressure in Adults. AMA Cardiol. 2018, 3, 352. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. 5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes—2020. Diabetes Care 2019, 43 (Suppl. 1), S48–S65. [Google Scholar]
- Singh, D.; Agusti, A.; Anzueto, A.; Barnes, P.J.; Bourbeau, J.; Celli, B.R.; Criner, G.J.; Frith, P.; Halpin, D.M.G.; Han, M.; et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: The GOLD science committee report 2019. Eur. Respir. J. 2019, 53, 1900164. [Google Scholar] [CrossRef] [PubMed]
- Eckel, R.H.; Jakicic, J.M.; Ard, J.D.; de Jesus, J.M.; Miller, N.H.; Hubbard, V.S.; Lee, I.-M.; Lichtenstein, A.H.; Loria, C.M.; Millen, B.E.; et al. 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 129 (Suppl. 2), S76–S99. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Afshin, A.; Benowitz, N.L.; Bittner, V.; Daniels, S.R.; Franch, H.A.; Jacobs, D.R., Jr.; Kraus, W.E.; Kris-Etherton, P.M.; Krummel, D.A.; et al. Population Approaches to Improve Diet, Physical Activity, and Smoking Habits: A Scientific Statement from the American Heart Association. Circulation 2012, 126, 1514–1563. [Google Scholar] [CrossRef]
- Cook, R.; Lamont, T.; Martin, R. Lifestyle changes may be more important than drugs for mild hypertension. BMJ 2019, 364, l571. [Google Scholar] [CrossRef]
- Horodyska, K.; Luszczynska, A.; van den Berg, M.; Hendriksen, M.; Roos, G.; De Bourdeaudhuij, I.; Brug, J. Good practice characteristics of diet and physical activity interventions and policies: An umbrella review. BMC Public Health 2015, 15, 19. [Google Scholar] [CrossRef]
- Morton, D.; Mitchell, B.; Kent, L.; Egger, G.; Hurlow, T. Lifestyle as medicine—Past precepts for present problems. Aust. Fam. Physician 2016, 45, 248–249. [Google Scholar]
- Sá, L.; Ribeiro, O.; Azevedo, L.F.; Couto, L.; Costa-Pereira, A.; Hespanhol, A.; Santos, P.; Martins, C. Patients’ estimations of the importance of preventive health services: A nationwide, population-based cross-sectional study in Portugal. BMJ Open 2016, 6, e011755. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Estatística. Resultados Definitivos Portugal. Lisboa. 2012. Available online: https://censos.ine.pt/xportal/xmain?xpid=CENSOS&xpgid=ine_censos_publicacao_det&contexto=pu&PUBLICACOESpub_boui=73212469&PUBLICACOESmodo=2&selTab=tab1&pcensos=61969554 (accessed on 28 May 2020).
- Gilbert, G.N. Researching Social Life, 2nd ed.; SAGE Publications: Szende Oaks, CA, USA, 2001. [Google Scholar]
- Gil, A.P.; Barreto, M.; Gaio, V.; Namorado, S.; Kislaya, I.; Lyshol, H.; Nunes, B.; Dias, C.M. Portuguese National Health Examination Survey: Questionnaire Development. Available online: https://www.researchgate.net/publication/283224075_Portuguese_National_Health_Examination_Survey_questionnaire_development (accessed on 9 February 2021).
- Nunes, B.; Barreto, M.; Gil, A.P.; Kislaya, I.; Namorado, S.; Antunes, L.; Gaio, V.; Santos, A.J.; Rodrigues, A.P.; Santos, J.; et al. The first Portuguese National Health Examination Survey (2015): Design, planning and implementation. J. Public Health 2019, 41, 511–517. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Healthy Diet. Fact Sheet. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 17 July 2020).
- Dernini, S.; Berry, E.M. Mediterranean Diet: From a Healthy Diet to a Sustainable Dietary Pattern. Front. Nutr. 2015, 2. Available online: http://www.frontiersin.org/Nutrition_and_Environmental_Sustainability/10.3389/fnut.2015.00015/abstract (accessed on 13 March 2020). [CrossRef]
- Monteagudo, C.; Mariscal-Arcas, M.; Rivas, A.; Lorenzo-Tovar, M.L.; Tur, J.A.; Olea-Serrano, F. Proposal of a Mediterranean Diet Serving Score. PLoS ONE 2015, 10, e0128594. [Google Scholar] [CrossRef]
- World Health Organization. Physical Activity Strategy for the WHO European Region 2016–2025; WHO Regional Office for Europe: Copenhagen, Denmark, 2016. [Google Scholar]
- Broholm, K.; Galluzzo, L.; Gandin, C.; Ghirini, S.; Ghiselli, A.; Jones, L.; Martire, S.; Mongan, D.; Montonen, M.; Mäkelä, P.; et al. Good practice principles for low risk drinking guidelines. In RARHA—Reducing Alcohol Related Harms; National Institute for Health and Welfare (THL): Helsinki, Finland, 2016. [Google Scholar]
- Bjartveit, K. Health consequences of smoking 1-4 cigarettes per day. Tob. Control 2005, 14, 315–320. [Google Scholar] [CrossRef]
- European Monitoring Centre for Drugs and Drug Addiction. Drug-Related Deaths and Mortality in Europe: Update from the EMCDDA Expert Network: July 2019. 2019. Available online: http://publications.europa.eu/publication/manifestation_identifier/PUB_TD0319444ENN (accessed on 16 May 2020).
- World Health Organization Regional Office for Europe, European Centre for Environment and Health, Bonn Office. WHO Technical Meeting on Sleep and Health; WHO Regional Office for Europe: Copenhagen, Denmark, 2004. [Google Scholar]
- Koyanagi, A.; Garin, N.; Olaya, B.; Ayuso-Mateos, J.L.; Chatterji, S.; Leonardi, M.; Koskinen, S.; Tobiasz-Adamczyk, B.; Haro, J.M. Chronic Conditions and Sleep Problems among Adults Aged 50 years or over in Nine Countries: A Multi-Country Study. PLoS ONE 2014, 9, e114742. [Google Scholar] [CrossRef]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; E Powell, K.; Bauman, A.; Lee, I.-M. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef]
- Wu, L.; Sun, S.; He, Y.; Jiang, B. The effect of interventions targeting screen time reduction: A systematic review and meta-analysis. Medicine (Baltimore) 2016, 95, e4029. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; on behalf of SBRN Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [PubMed]
- Gee, M.E.; Bienek, A.; Campbell, N.R.; Bancej, C.M.; Robitaille, C.; Kaczorowski, J.; Joffres, M.; Dai, S.; Gwadry-Sridar, F.; Nolan, R.P. Prevalence of, and Barriers to, Preventive Lifestyle Behaviors in Hypertension (from a National Survey of Canadians With Hypertension). Am. J. Cardiol. 2012, 109, 570–575. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Peral, P.; Conejo-Cerón, S.; Fernández, A.; Berenguera, A.; Martínez-Andrés, M.; Pons-Vigués, M.; Motrico, E.; Rodríguez-Martín, B.; Bellón, J.A.; Rubio-Valera, M. Primary Care Patients’ Perspectives of Barriers and Enablers of Primary Prevention and Health Promotion—A Meta-Ethnographic Synthesis. PLoS ONE 2015, 10, e0125004. [Google Scholar] [CrossRef] [PubMed]
- Wermeling, M.; Thiele-Manjali, U.; Koschack, J.; Lucius-Hoene, G.; Himmel, W. Type 2 diabetes patients’ perspectives on lifestyle counselling and weight management in general practice: A qualitative study. BMC Fam. Pract. 2014, 15, 97. [Google Scholar] [CrossRef]
- Walseth, L.T.; Abildsnes, E.; Schei, E. Patients’ experiences with lifestyle counselling in general practice: A qualitative study. Scand. J. Prim. Heal. Care 2011, 29, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, S.; Weber, D. Reporting biases in self-assessed physical and cognitive health status of older Europeans. PLoS ONE 2019, 14, e0223526. [Google Scholar] [CrossRef]
- Smith, A.W.; Borowski, L.A.; Liu, B.; Galuska, D.A.; Signore, C.; Klabunde, C.; Huang, T.T.-K.; Krebs-Smith, S.M.; Frank, E.; Pronk, N.; et al. U.S. Primary Care Physicians’ Diet-, Physical Activity-, and Weight-Related Care of Adult Patients. Am. J. Prev. Med. 2011, 41, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Foster, G.D.; Wadden, T.A.; Makris, A.P.; Davidson, D.; Sanderson, R.S.; Allison, D.B.; Kessler, A. Primary Care Physicians’ Attitudes about Obesity and Its Treatment. Obes. Res. 2003, 11, 1168–1177. [Google Scholar] [CrossRef]
- BBrotons, C.; Bulc, M.; Sammut, M.R.; Sheehan, M.; Martins, C.M.D.S.; Björkelund, C.; Drenthen, A.J.M.; Duhot, D.; Görpelioglui, S.; Jurgova, E.; et al. Attitudes toward preventive services and lifestyle: The views of primary care patients in Europe. The EUROPREVIEW patient study. Fam. Pract. 2012, 29 (Suppl. 1), i168–i176. [Google Scholar] [CrossRef] [PubMed]
- Brotons, C.; Björkelund, C.; Bulc, M.; Ciurana, R.; Godycki-Cwirko, M.; Jurgova, E.; Kloppe, P.; Lionis, C.; Mierzecki, A.; Piñeiro, R.; et al. Prevention and health promotion in clinical practice: The views of general practitioners in Europe. Prev. Med. 2005, 40, 595–601. [Google Scholar] [CrossRef]
- Brug, J.; van der Ploeg, H.P.; Loyen, A.; Ahrens, W.; Allais, O.; Andersen, L.F.; Cardon, G.; Capranica, L.; Chastin, S.; De Bourdeaudhuij, I.; et al. Determinants of diet and physical activity (DEDIPAC): A summary of findings. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 150. [Google Scholar] [CrossRef]
- Sagner, M.; Katz, D.; Egger, G.; Lianov, L.; Schulz, K.-H.; Braman, M.; Behbod, B.; Phillips, E.; Dysinger, W.; Ornish, D. Lifestyle medicine potential for reversing a world of chronic disease epidemics: From cell to community. Int. J. Clin. Prac. 2014, 68, 1289–1292. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Valera, M.; Pons-Vigués, M.; Martínez-Andrés, M.; Moreno-Peral, P.; Berenguera, A.; Fernández, A. Barriers and Facilitators for the Implementation of Primary Prevention and Health Promotion Activities in Primary Care: A Synthesis through Meta-Ethnography. PLoS ONE 2014, 9, e89554. [Google Scholar] [CrossRef] [PubMed]
- Condello, G.; Ling, F.C.M.; Bianco, A.; Chastin, S.; Cardon, G.; Ciarapica, D.; Conte, D.; Cortis, C.; De Craemer, M.; Di Blasio, A.; et al. Using concept mapping in the development of the EU-PAD framework (EUropean-Physical Activity Determinants across the life course): A DEDIPAC-study. BMC Public Health 2016, 16, 1145. [Google Scholar] [CrossRef] [PubMed]
- Gebremariam, A.; Yalew, A.W.; Hirpa, S.; Wondimagegnehu, A.; Kaba, M.; Assefa, M.; Mitiku, I.; Kantelhardt, E.J.; Jemal, A.; Addissie, A.; et al. Application of the rapid ethical assessment approach to enhance the ethical conduct of longitudinal population based female cancer research in an urban setting in Ethiopia. BMC Med. Ethics. 2018, 19, 87. [Google Scholar] [CrossRef]
- Chastin, S.F.M.; De Craemer, M.; Lien, N.; Bernaards, C.; Buck, C.; Oppert, J.-M.; Nazare, J.-A.; Lakerveld, J.; O’Donoghue, G.; Holdsworth, M.; et al. The SOS-framework (Systems of Sedentary behaviours): An international transdisciplinary consensus framework for the study of determinants, research priorities and policy on sedentary behaviour across the life course: A DEDIPAC-study. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 83. [Google Scholar] [CrossRef] [PubMed]
| n = 900 | |
|---|---|
| Nationality, n (%) | |
| Portuguese | 859 (95.4) |
| Other nationality | 41 (4.6) |
| Age (years), , Med, min-max | 51.8 ± 18.1, 51, 20–99 |
| Age groups (years), n (%) | |
| [20; 24] | 58 (6.4) |
| [25; 29] | 59 (6.6) |
| [30; 34] | 63 (7.0) |
| [35; 39] | 76 (8.4) |
| [40; 44] | 89 (9.9) |
| [45; 49] | 83 (9.2) |
| [50; 54] | 81 (9.0) |
| [55; 59] | 78 (8.7) |
| [60; 64] | 72 (8.0) |
| [65; 69] | 67 (7.4) |
| [70; 74] | 57 (6.3) |
| ≥75 | 117 (13.0) |
| Gender, n (%) | |
| Female | 483 (53.7) |
| Male | 417 (46.3) |
| Marital status, n (%) | |
| Single | 187 (20.8) |
| Married | 506 (56.2) |
| Married but legally separated | 16 (1.8) |
| Divorced | 85 (9.4) |
| Widowed | 106 (11.8) |
| Highest level of education completed, n (%) | |
| None | 24 (2.7) |
| Primary, first cycle | 204 (22.7) |
| Primary, second cycle | 76 (8.4) |
| Primary, third cycle | 183 (20.3) |
| Secondary education | 298 (33.1) |
| Higher education, bachelor | 12 (1.3) |
| Higher education, graduation | 78 (8.7) |
| Higher education, postgraduate studies | 8 (0.9) |
| Higher education, masters | 14 (1.6) |
| Higher education, PhD | 3 (0.3) |
| Main occupation, n (%) | |
| Works on its own | 146 (16.2) |
| Employed by others | 424 (47.1) |
| Student | 23 (2.6) |
| Doing military service | 0 (0) |
| Homemaker | 11 (1.2) |
| Retired | 238 (26.4) |
| Unemployed | 58 (6.4) |
| Professional sector (n = 570), n (%) | |
| Primary sector | 3 (0.5) |
| Secondary sector | 80 (14.0) |
| Tertiary sector | 486 (85.3) |
| Health care beneficiary (multi response), n (%) | |
| SNS (National Health Service) | 842 (93.6) |
| Private Health Insurance | 128 (14.2) |
| Semi-private Health Service Assistance | 74 (8.3) |
| Geographic distribution (NUTS II), n (%) | |
| North | 330 (36.7) |
| Center | 209 (23.2) |
| Metropolitan area of Lisbon | 254 (28.2) |
| Alentejo | 67 (7.4) |
| Algarve | 40 (4.4) |
| Health General Status, n (%) | |
| Very good | 83 (9.2) |
| Good | 413 (45.9) |
| Reasonable | 325 (36.1) |
| Poor | 71 (7.9) |
| Very poor | 8 (0.9) |
| Health problems last 12 months, n (%) | |
| None | 356 (39.6) |
| Osteoarticular/muscular pain | 349 (38.8) |
| Hypertension | 178 (19.8) |
| Anxiety | 153 (17.0) |
| Hypercholesterolemia | 145 (16.1) |
| Overweight | 140 (15.6) |
| Diabetes | 99 (11.0) |
| Heart problems | 72 (8.0) |
| Depression | 58 (6.4) |
| Gastritis or peptic ulcer disease | 49 (5.4) |
| Asthma and/or COPD | 40 (4.4) |
| Stroke | 16 (1.8) |
| Obesity | 19 (2.1) |
| Cancer | 12 (1.3) |
| Number of health problems last 12 months, n (%) | |
| 1 | 189 (21.0) |
| 2 | 141 (39.7) |
| 3 | 105 (29.6) |
| 4 | 45 (12.7) |
| ≥ 5 | 64 (18.0) |
| 1 Strongly Disagree n (%) | 2 Partially Disagree n (%) | 3 Indifferent n (%) | 4 Partially Agree n (%) | 5 Strongly Agree n (%) | Med [95% CI] | |
|---|---|---|---|---|---|---|
| Diet | ||||||
| A healthy diet can prevent and help control some diseases. | 0 (0.0) | 1 (0.1) | 8 (0.9) | 108 (12.0) | 783 (87.0) | 5 [5; 5] |
| My diet is healthy. | 13 (1.4) | 46 (5.1) | 159 (17.7) | 373 (41.4) | 309 (34.3) | 4 [4; 4] |
| It is important that my family doctor asks/advises me about my diet. | 57 (6.3) | 18 (2.0) | 84 (9.3) | 233 (25.9) | 508 (56.4) | 5 [5; 5] |
| Usually, my family doctor asks/advises me about healthy diet. | 258 (28.7) | 93 (10.3) | 73 (8.1) | 171 (19.0) | 305 (33.9) | 4 [3; 4] |
| Physical activity | ||||||
| Regular physical activity can prevent and help control some diseases. | 2 (0.2) | 3 (0.3) | 5 (0.6) | 104 (11.6) | 786 (87.3) | 5 [5; 5] |
| My physical activity is regular. | 271 (30.1) | 168 (18.7) | 94 (10.4) | 149 (16.6) | 218 (24.2) | 3 [2; 3] |
| It is important that my family doctor asks/advises me about my physical activity. | 91 (10.1) | 21 (2.3) | 131 (14.6) | 207 (23.0) | 450 (50.0) | 4.5 [4; 5] |
| Usually, my family doctor asks/advises me about physical activity. | 306 (34.0) | 81 (9.0) | 98 (10.9) | 149 (16.6) | 266 (29.6) | 3 [3; 3] |
| Alcohol consumption | ||||||
| Excessive alcohol consumption can cause and aggravate some diseases. | 1 (0.1) | 0 (0) | 3 (0.3) | 66 (7.3) | 830 (92.2) | 5 [5; 5] |
| My alcohol consumption is excessive. | 745 (82.8) | 85 (9.4) | 53 (5.9) | 15 (1.7) | 2 (0.2) | 1 [1; 1] |
| It is important that my family doctor asks/advises me about my alcohol consumption. | 132 (14.7) | 36 (4.0) | 154 (17.1) | 167 (18.6) | 411 (45.7) | 4 [4; 4] |
| Usually, my family doctor asks/advises me about alcohol consumption. | 402 (44.7) | 85 (9.4) | 97 (10.8) | 114 (12.7) | 202 (22.4) | 2 [2; 2] |
| Tobacco use | ||||||
| Smoking can cause and aggravate some diseases. | 1 (0.1) | 0 (0) | 1 (0.1) | 53 (5.9) | 845 (93.9) | 5 [5; 5] |
| I am an active smoker. | 653 (72.6) | 27 (3.0) | 9 (1.0) | 54 (6.0) | 157 (17.4) | 1 [1; 1] |
| It is important that my family doctor asks/advises me about smoking. | 144 (16.0) | 27 (3.0) | 139 (15.4) | 170 (18.9) | 420 (46.7) | 4 [4; 4] |
| Usually, my family doctor asks/advises me about smoking. | 396 (44.0) | 69 (7.7) | 100 (11.1) | 105 (11.7) | 230 (25.6) | 2 [2; 3] |
| Illicit drugs | ||||||
| Illicit drugs can cause and aggravate some diseases. | 2 (0.2) | 0 (0) | 7 (0.8) | 38 (4.2) | 853 (94.8) | 5 [5; 5] |
| I do not use illicit drugs. | 6 (0.7) | 4 (0.4) | 2 (0.2) | 18 (2.0) | 870 (96.7) | 5 [5; 5] |
| It is important that my family doctor asks/advises me about illicit drugs. | 265 (29.4) | 41 (4.6) | 150 (16.7) | 116 (12.9) | 328 (36.4) | 3 [3; 4] |
| Usually, my family doctor asks/advises me about illicit drugs. | 603 (67.0) | 55 (6.1) | 106 (11.8) | 42 (4.7) | 94 (10.4) | 1 [1; 1] |
| Sleep habits | ||||||
| Good quality sleep can prevent and help control some diseases. | 1 (0.1) | 1 (0.1) | 2 (0.2) | 75 (8.3) | 821 (91.2) | 5 [5; 5] |
| I have a good quality of sleep. | 99 (11.0) | 106 (11.8) | 131 (14.6) | 220 (24.4) | 344 (38.2) | 4 [4; 4] |
| It is important that my family doctor asks/advises me about sleep habits. | 53 (5.9) | 23 (2.6) | 106 (11.8) | 210 (23.3) | 508 (56.4) | 5 [5; 5] |
| Usually, my family doctor asks/advises me about sleep habits. | 263 (29.2) | 106 (11.8) | 84 (9.3) | 156 (17.3) | 291 (32.3) | 3 [3; 4] |
| Screen activities | ||||||
| Excessive screen activities can cause and aggravate some diseases. | 0 (0) | 5 (0.6) | 40 (4.4) | 139 (15.4) | 716 (79.6) | 5 [5; 5] |
| I have excessive screen activities. | 388 (43.1) | 159 (17.7) | 136 (15.1) | 132 (14.7) | 85 (9.4) | 2 [2; 2] |
| It is important that my family doctor asks/advises me about screen activities. | 187 (20.8) | 63 (7.0) | 192 (21.3) | 142 (15.8) | 316 (35.1) | 4 [3; 4] |
| Usually, my family doctor asks/advises me about screen activities. | 518 (57.6) | 93 (10.3) | 95 (10.6) | 67 (7.4) | 127 (14.1) | 1 [1; 1] |
| Stress | ||||||
| A high level of stress can cause and aggravate some diseases. | 0 (0) | 0 (0) | 11 (1.2) | 68 (7.6) | 821 (91.2) | 5 [5; 5] |
| I have a high level of stress. | 340 (37.8) | 166 (18.4) | 151 (16.8) | 162 (18.0) | 81 (9.0) | 2 [2; 2] |
| It is important that my family doctor asks/advises me about my level of stress. | 68 (7.6) | 30 (3.3) | 117 (13.0) | 219 (24.3) | 466 (51.8) | 5 [4; 5] |
| Usually, my family doctor asks/advises me about managing stress. | 309 (34.3) | 90 (10.0) | 92 (10.2) | 161 (17.9) | 248 (27.6) | 3 [3; 3] |
| Sedentarism | ||||||
| Sedentarism can cause and aggravate some diseases. | 0 (0) | 0 (0) | 6 (0.7) | 85 (9.4) | 809 (89.9) | 5 [5; 5] |
| I am sedentary. | 423 (47.0) | 171 (19.0) | 111 (12.3) | 136 (15.1) | 59 (6.6) | 2 [1; 2] |
| It is important that my family doctor asks/advises me about sedentarism. | 68 (7.6) | 30 (3.3) | 119 (13.2) | 221 (24.6) | 462 (51.3) | 5 [4; 5] |
| Usually, my family doctor asks/advises me about sedentarism. | 312 (34.7) | 90 (10.0) | 96 (10.7) | 161 (17.9) | 241 (26.8) | 3 [3; 3] |
| Diet, n (%) | |
|---|---|
| Healthy diet | 126 (14.0) |
| Additional information on the topic: | |
| Body mass index (n = 891), n (%) | |
| Underweight | 13 (1.4) |
| Normal | 401 (44.6) |
| Overweight | 358 (40.2) |
| Obesity | 119 (13.4) |
| Physical activity, n (%) | |
| Regular physical activity | 260 (28.9) |
| Alcohol consumption, n (%) | |
| Moderate alcohol consumption | 649 (72.1) |
| Tobacco use, n (%) | |
| Non-smokers | 669 (74.3) |
| Illicit drugs, n (%) | |
| Do not consume illicit drugs | 888 (98.7) |
| Sleep habits, n (%) | |
| Good quality sleep | 493 (54.8) |
| Screen activities, n (%) | |
| Moderate screen activities | 586 (64.6) |
| Stress, n (%) | |
| Moderate stress level | 584 (64.9) |
| Sedentarism, n (%) | |
| No sedentarism | 455 (50.6) |
| Dimension 1 | Dimension 2 | Dimension 3 | Dimension 4 | ||
|---|---|---|---|---|---|
| Diet | Gender | 0.159 a | 0.376 a | 0.233 a | 0.269 a |
| Female | 5 [5; 5] | 4 [4; 5] | 5 [4; 5] | 4 [1; 5] | |
| Male | 5 [5; 5] | 4 [3.5; 5] | 5 [4; 5] | 4 [1; 5] | |
| Age | −0.011; 0.731 b | 0.060; 0.073 b | 0.074; 0.026 b,* | 0.158; <0.001 b,* | |
| Marital status | 0.454 a | 0.086 a | 0.290 a | 0.030 a,* | |
| Married | 5 [5; 5] | 4 [4; 5] | 5 [4; 5] | 4 [1; 5] | |
| Others | 5 [5; 5] | 4 [3; 5] | 5 [4; 5] | 3 [1; 5] | |
| Education level | 0.059 a | 0.626 a | 0.664 a | 0.318 a | |
| High school or less | 5 [5; 5] | 4 [4; 5] | 5 [4; 5] | 4 [1; 5] | |
| Universitary education | 5 [5; 5] | 4 [3; 5] | 5 [4; 5] | 4 [1; 5] | |
| Health general status | 0.984 c | 0.025 c,* | 0.020 c,* | 0.091 c | |
| Very Good | 5 [5; 5] | 4 [4; 5] | 4 [4; 5] | 2 [1; 4] | |
| Good | 5 [5; 5] | 4 [4; 5] | 5 [4; 5] | 4 [1; 5] | |
| Reasonable | 5 [5; 5] | 4 [4; 5] | 5 [4; 5] | 4 [1; 5] | |
| Poor | 5 [5; 5] | 4 [3; 4] | 4 [3; 5] | 4 [1; 5] | |
| Very poor | 5 [5; 5] | 4 [2.5; 4] | 5 [4; 5] | 4 [1; 4] | |
| NHPL 12 months | 0.054; 0.104 b | −0.211; <0.001 b,* | −0.024; 0.466 b | 0.011; 0.734 b | |
| Physical activity | Gender | 0.984 a | 0.123 a | 0.031 a,* | 0.216 a |
| Female | 5 [5; 5] | 2 [1; 4] | 5 [4; 5] | 3 [1; 5] | |
| Male | 5 [5; 5] | 3 [1; 4] | 4 [3; 5] | 3 [1; 5] | |
| Age | −0.105; 0.022 b,* | −0.292; <0.001 b,* | −0.066; 0.150 b | 0.039; 0.393 b | |
| Marital status | 0.868 a | 0.036 a,* | 0.458 a | 0.138 a | |
| Married | 5 [5; 5] | 2 [1; 4] | 4.5 [4; 5] | 3.5 [1; 5] | |
| Others | 5 [5; 5] | 3 [1; 5] | 4.5 [3; 5] | 3 [1; 5] | |
| Education level | 0.418 a | <0.001 a,* | 0.065 a | 0.547 a | |
| High school or less | 5 [5; 5] | 2 [1; 4] | 4 [3; 5] | 3 [1; 5] | |
| Universitary education | 5 [5; 5] | 4 [2; 5] | 5 [3; 5] | 3 [1; 5] | |
| Health general status | 0.269 c | <0.001 c,* | 0.017 c,* | 0.046 c,* | |
| Very Good | 5 [5; 5] | 4 [2; 5] | 4 [3; 5] | 2 [1; 4] | |
| Good | 5 [5; 5] | 3 [2; 5] | 5 [3; 5] | 3 [1; 5] | |
| Reasonable | 5 [5; 5] | 2 [1; 4] | 5 [4; 5] | 4 [1; 5] | |
| Poor | 5 [5; 5] | 2 [1; 3] | 4 [3; 5] | 3 [1; 4] | |
| Very poor | 5 [4.25; 5] | 1 [1; 1.75] | 4.5 [3.25; 5] | 1.5 [1; 4] | |
| NHPL 12 months | 0.027; 0.554 b | −0.301; <0.001 b,* | −0.116; 0.010 b,* | −0.043; 0.342 b | |
| Alcohol consumption | Gender | 0.510 a | <0.001 a,* | 0.103 a | 0.003 a,* |
| Female | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 2 [1; 4] | |
| Male | 5 [5; 5] | 5 [4; 5] | 4 [3; 5] | 3 [1; 5] | |
| Age | 0.010; 0.757 b | 0.115; 0.001 b,* | −0.048; 0.148 b | 0.039; 0.239 b | |
| Marital status | 0.173 a | 0.744 a | 0.218 a | 0.022 a,* | |
| Married | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 2 [1; 4] | |
| Others | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 2 [1; 4] | |
| Education level | 0.437 a | 0.357 a | 0.205 a | 0.084 a | |
| High school or less | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 2 [1; 4] | |
| Universitary education | 5 [5; 5] | 5 [5; 5] | 5 [3; 5] | 1 [1; 4] | |
| Health general status | 0.874 c | 0.092 c | 0.005 c,* | 0.016 c,* | |
| Very Good | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 1 [1; 4] | |
| Good | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 2 [1; 4] | |
| Reasonable | 5 [5; 5] | 5 [5; 5] | 5 [3; 5] | 2 [1; 4] | |
| Poor | 5 [5; 5] | 5 [5; 5] | 3 [1; 5] | 1 [1; 3] | |
| Very poor | 5 [5; 5] | 5 [5; 5] | 5 [3; 5] | 1 [1; 2.75] | |
| NHPL 12 months | 0.073; 0.029 b,* | 0.109; 0.001 b,* | −0.175; <0.001 b,* | −0.142; <0.001 b,* | |
| Tobacco use | Gender | 0.327 a | <0.001 a,* | 0.170 a | 0.001 a,* |
| Female | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 2 [1; 4] | |
| Male | 5 [5; 5] | 5 [2; 5] | 4 [3; 5] | 3 [1; 5] | |
| Age | 0.012; 0.721 b | 0.226; <0.001 b,* | −0.151; <0.001 b,* | −0.118; <0.001 b,* | |
| Marital status | 0.264 a | 0.003 a,* | 0.046 a,* | 0.199 a | |
| Married | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 2 [1; 5] | |
| Others | 5 [5; 5] | 5 [2; 5] | 4 [3; 5] | 2 [1; 4] | |
| Education level | 0.210 a | 0.095 a | 0.329 a | 0.372 a | |
| High school or less | 5 [5; 5] | 5 [3; 5] | 4 [3; 5] | 2 [1; 5] | |
| Universitary education | 5 [5; 5] | 5 [5; 5] | 5 [3; 5] | 1 [1; 5] | |
| Health general status | 0.354 c | <0.001 c,* | 0.004 c,* | 0.014 c,* | |
| Very Good | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 1 [1; 4] | |
| Good | 5 [5; 5] | 5 [2; 5] | 4 [3; 5] | 3 [1; 5] | |
| Reasonable | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 2 [1; 4] | |
| Poor | 5 [5; 5] | 5 [5; 5] | 3 [1; 5] | 1 [1; 3] | |
| Very poor | 5 [5; 5] | 5 [5; 5] | 4.5 [1.5; 5] | 1 [1; 2.5] | |
| NHPL 12 months | 0.103; 0.002 b,* | 0.090; 0.007 b,* | −0.237; <0.001 b,* | −0.203; <0.001 b,* | |
| Ilicit drugs | Gender | 0.188 a | 0.002 a,* | 0.895 a | 0.297 a |
| Female | 5 [5; 5] | 5 [5; 5] | 3 [1; 5] | 1 [1; 3] | |
| Male | 5 [5; 5] | 5 [5; 5] | 3 [1; 5] | 1 [1; 3] | |
| Age | 0.002; 0.955 b | 0.042; 0.206 b | −0.162; <0.001 b,* | −0.099; 0.003 b,* | |
| Marital status | 0.278 a | 0.065 a | 0.591 a | 0.602 a | |
| Married | 5 [5; 5] | 5 [5; 5] | 3 [1; 5] | 1 [1; 3] | |
| Others | 5 [5; 5] | 5 [5; 5] | 3 [1; 5] | 1 [1; 3] | |
| Education level | 0.998 a | 0.650 a | 0.045 a,* | 0.947 a | |
| High school or less | 5 [5; 5] | 5 [5; 5] | 3 [1; 5] | 1 [1; 3] | |
| Universitary education | 5 [5; 5] | 5 [5; 5] | 4 [2; 5] | 1 [1; 3] | |
| Health general status | 0.070 c | 0.716 c | 0.072 c | 0.349 c | |
| Very Good | 5 [5; 5] | 5 [5; 5] | 4 [3; 5] | 1 [1; 3] | |
| Good | 5 [5; 5] | 5 [5; 5] | 3 [1; 5] | 1 [1; 3] | |
| Reasonable | 5 [5; 5] | 5 [5; 5] | 4 [1; 5] | 1 [1; 3] | |
| Poor | 5 [5; 5] | 5 [5; 5] | 3 [1; 4] | 1 [1; 2] | |
| Very poor | 5 [5; 5] | 5 [5; 5] | 2.5 [1; 5] | 1 [1; 1] | |
| NHPL 12 months | 0.090; 0.007 b,* | 0.068; 0.041 b,* | −0.095; 0.004 b,* | −0.202; <0.001 b,* | |
| Sleep habits | Gender | 0.423 a | 0.005 a,* | 0.006 a,* | 0.036 a,* |
| Female | 5 [5; 5] | 4 [2; 5] | 5 [4; 5] | 4 [1; 5] | |
| Male | 5 [5; 5] | 4 [3; 5] | 5 [4; 5] | 3 [1; 5] | |
| Age | −0.031; 0.346 b | −0.168; <0.001 b,* | 0.136; <0.001 b,* | 0.215; <0.001 b,* | |
| Marital status | 0.417 a | 0.280 a | 0.895 a | 0.644 a | |
| Married | 5 [5; 5] | 4 [3; 5] | 5 [4; 5] | 3.5 [1; 5] | |
| Others | 5 [5; 5] | 4 [2.75; 5] | 5 [4; 5] | 3 [1; 5] | |
| Education level | 0.989 a | 0.005 a,* | 0.567 a | 0.019 a,* | |
| High school or less | 5 [5; 5] | 4 [3; 5] | 5 [4; 5] | 4 [1; 5] | |
| Universitary education | 5 [5; 5] | 5 [3; 5] | 5 [3; 5] | 3 [1; 4] | |
| Health general status | 0.948 c | <0.001 c,* | <0.001 c,* | <0.001 c,* | |
| Very Good | 5 [5; 5] | 5 [4; 5] | 4 [3; 5] | 2 [1; 4] | |
| Good | 5 [5; 5] | 4 [3; 5] | 5 [4; 5] | 3 [1; 5] | |
| Reasonable | 5 [5; 5] | 4 [2; 5] | 5 [4; 5] | 4 [2; 5] | |
| Poor | 5 [5; 5] | 3 [2; 4] | 4 [3; 5] | 4 [1; 5] | |
| Very poor | 5 [5; 5] | 1.5 [1; 3.75] | 5 [4.25; 5] | 3 [1; 4.75] | |
| NHPL 12 months | 0.008; 0.817 b | −0.420; <0.001 b,* | 0.017; 0.602 b | 0.026; 0.433 b | |
| Screen activities | Gender | 0.030 a,* | 0.663 a | 0.756 a | 0.632 a |
| Female | 5 [5; 5] | 4 [3; 5] | 4 [2; 5] | 1 [1; 3] | |
| Male | 5 [5; 5] | 4 [3; 5] | 4 [2; 5] | 1 [1; 3] | |
| Age | −0.033; 0.320 b | 0.220; <0.001 b,* | −0.066; 0.047 b,* | −0.003; 0.924 b | |
| Marital status | 0.109 a | 0.123 a | 0.012 a,* | 0.044 a,* | |
| Married | 5 [5; 5] | 4 [3; 5] | 4 [2; 5] | 1 [1; 3] | |
| Others | 5 [5; 5] | 4 [2; 5] | 3 [2; 5] | 1 [1; 3] | |
| Education level | 0.341 a | <0.001 a,* | 0.662 a | 0.056 a | |
| High school or less | 5 [5; 5] | 4 [3; 5] | 4 [2; 5] | 1 [1; 3] | |
| Universitary education | 5 [5; 5] | 3 [2; 5] | 4 [2; 5] | 1 [1; 2] | |
| Health general status | 0.040 c,* | 0.064 c | <0.001 c,* | 0.006 c,* | |
| Very Good | 5 [4; 5] | 4 [2; 5] | 3 [1; 4] | 1 [1; 2] | |
| Good | 5 [5; 5] | 4 [2; 5] | 4 [2.5; 5] | 1 [1; 3] | |
| Reasonable | 5 [5; 5] | 4 [3; 5] | 4 [2; 5] | 1 [1; 3] | |
| Poor | 5 [4; 5] | 4 [3; 5] | 3 [1; 4] | 1 [1; 3] | |
| Very poor | 5 [5; 5] | 5 [2.5; 5] | 4 [2; 5] | 1 [1; 1.75] | |
| NHPL 12 months | −0.024; 0.467 b | 0.009; 0.788 b | −0.182; <0.001 b,* | −0.192; <0.001 b,* | |
| Stress | Gender | 0.723 a | 0.024 a,* | 0.417 a | 0.142 a |
| Female | 5 [5; 5] | 4 [2; 5] | 5 [4; 5] | 3 [1; 5] | |
| Male | 5 [5; 5] | 4 [3; 5] | 5 [3; 5] | 3 [1; 5] | |
| Age | −0.028; 0.408 b | 0.139; <0.001 b,* | 0.035; 0.288 b | 0.080; 0.016 b,* | |
| Marital status | 0.555 a | 0.399 a | 0.091 a | 0.088 a | |
| Married | 5 [5; 5] | 4 [2; 5] | 5 [4; 5] | 3 [1; 5] | |
| Others | 5 [5; 5] | 4 [2; 5] | 4 [3; 5] | 3 [1; 5] | |
| Education level | 0.939 a | 0.003 a,* | 0.634 a | 0.090 a | |
| High school or less | 5 [5; 5] | 4 [2; 5] | 5 [4; 5] | 3 [1; 5] | |
| Universitary education | 5 [5; 5] | 3 [2; 5] | 5 [3; 5] | 2 [1; 4] | |
| Health general status | 0.721 c | 0.086 c | 0.035 c,* | 0.030 c,* | |
| Very Good | 5 [5; 5] | 4 [3; 5] | 4 [3; 5] | 2 [1; 4] | |
| Good | 5 [5; 5] | 4 [2; 5] | 5 [4; 5] | 3 [1; 5] | |
| Reasonable | 5 [5; 5] | 4 [2; 5] | 5 [4; 5] | 3 [1; 5] | |
| Poor | 5 [5; 5] | 3 [2; 5] | 4 [4; 5] | 4 [1; 5] | |
| Very poor | 5 [5; 5] | 3 [2; 3.75] | 5 [4.25; 5] | 4 [1; 4] | |
| NHPL 12 months | 0.045; 0.181 b | −0.173; <0.001 b,* | −0.042; 0.214 b | −0.043; 0.196 b | |
| Sedentarism | Gender | 0.699 a | 0.289 a | 0.162 a | 0.962 a |
| Female | 5 [5; 5] | 4 [3; 5] | 5 [4; 5] | 3 [1; 5] | |
| Male | 5 [5; 5] | 4 [3; 5] | 4 [3; 5] | 3 [1; 5] | |
| Age | −0.030; 0.371 b | −0.267; <0.001 b,* | 0.056; 0.095 b | 0.151; <0.001 b,* | |
| Marital status | 0.250 a | 0.065 a | 0.093 a | 0.749 a | |
| Married | 5 [5; 5] | 4 [3; 5] | 5 [4; 5] | 3 [1; 5] | |
| Others | 5 [5; 5] | 4 [3; 5] | 4 [3; 5] | 3 [1; 5] | |
| Education level | 0.817 a | 0.664 a | 0.480 a | 0.331 a | |
| High school or less | 5 [5; 5] | 4 [3; 5] | 5 [4; 5] | 3 [1; 5] | |
| Universitary education | 5 [5; 5] | 4 [3; 5] | 5 [3; 5] | 2 [1; 5] | |
| Health general status | 0.446 c | <0.001 c,* | 0.025 c,* | <0.001 c,* | |
| Very Good | 5 [5; 5] | 5 [4; 5] | 4 [3; 5] | 1 [1; 3] | |
| Good | 5 [5; 5] | 5 [3; 5] | 5 [4; 5] | 3 [1; 5] | |
| Reasonable | 5 [5; 5] | 4 [2; 5] | 5 [4; 5] | 3 [1; 5] | |
| Poor | 5 [5; 5] | 3 [2; 5] | 4 [3; 5] | 4 [1; 4] | |
| Very poor | 5 [5; 5] | 2 [2; 4.75] | 5 [4.25; 5] | 3.5 [1; 4.75] | |
| NHPL 12 months | 0.064; 0.055 b | −0.251; <0.001 b,* | −0.043; 0.202 b | 0.005; 0.870 b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Páscoa, R.; Teixeira, A.; Gregório, M.; Carvalho, R.; Martins, C. Patients’ Perspectives about Lifestyle Behaviors and Health in the Context of Family Medicine: A Cross-Sectional Study in Portugal. Int. J. Environ. Res. Public Health 2021, 18, 2981. https://doi.org/10.3390/ijerph18062981
Páscoa R, Teixeira A, Gregório M, Carvalho R, Martins C. Patients’ Perspectives about Lifestyle Behaviors and Health in the Context of Family Medicine: A Cross-Sectional Study in Portugal. International Journal of Environmental Research and Public Health. 2021; 18(6):2981. https://doi.org/10.3390/ijerph18062981
Chicago/Turabian StylePáscoa, Rosália, Andreia Teixeira, Micaela Gregório, Rosa Carvalho, and Carlos Martins. 2021. "Patients’ Perspectives about Lifestyle Behaviors and Health in the Context of Family Medicine: A Cross-Sectional Study in Portugal" International Journal of Environmental Research and Public Health 18, no. 6: 2981. https://doi.org/10.3390/ijerph18062981
APA StylePáscoa, R., Teixeira, A., Gregório, M., Carvalho, R., & Martins, C. (2021). Patients’ Perspectives about Lifestyle Behaviors and Health in the Context of Family Medicine: A Cross-Sectional Study in Portugal. International Journal of Environmental Research and Public Health, 18(6), 2981. https://doi.org/10.3390/ijerph18062981









