Religious Affiliations Influence Health-Related and General Decision Making: A Brazilian Nationwide Survey
Abstract
1. Introduction
2. Materials and Methods
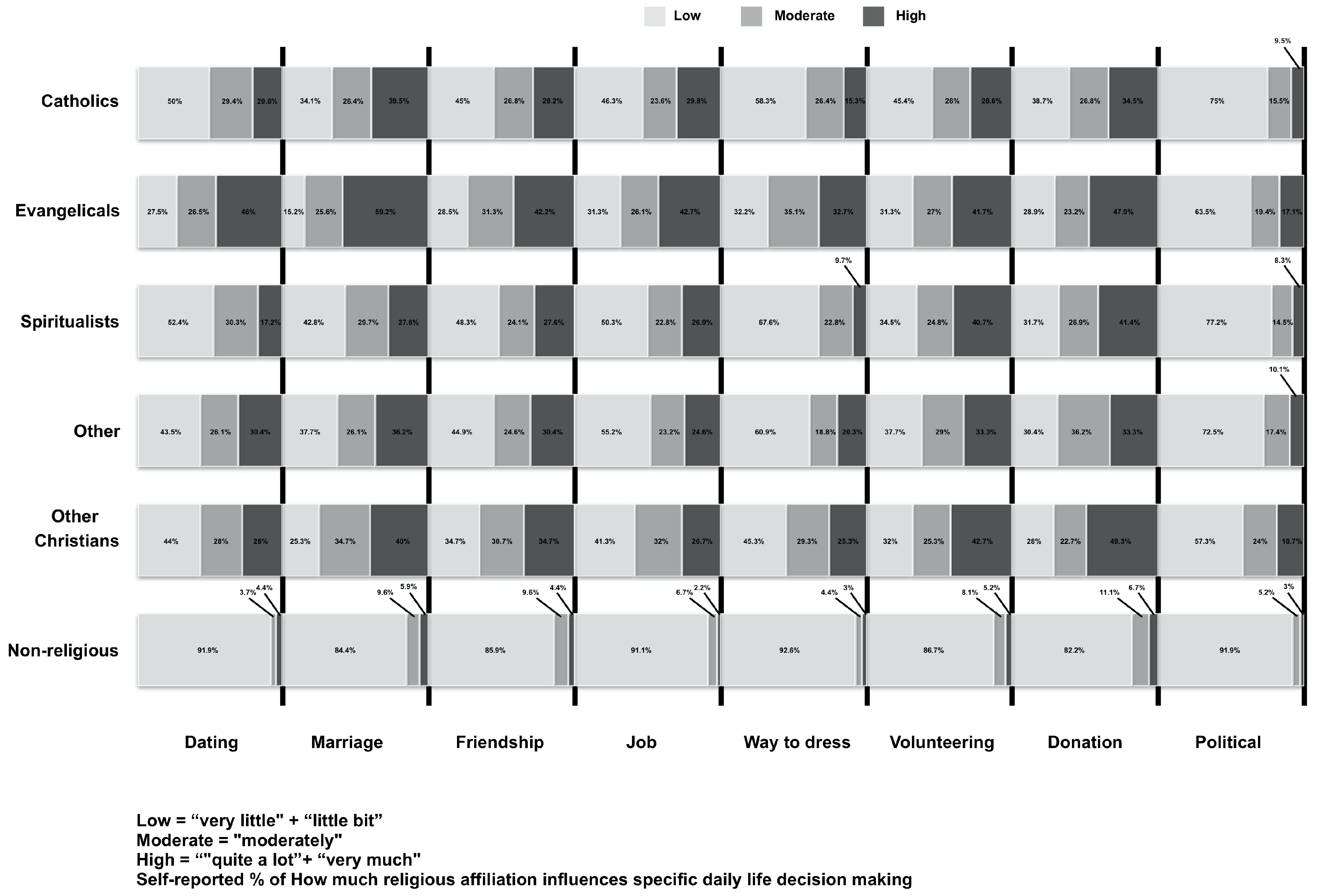
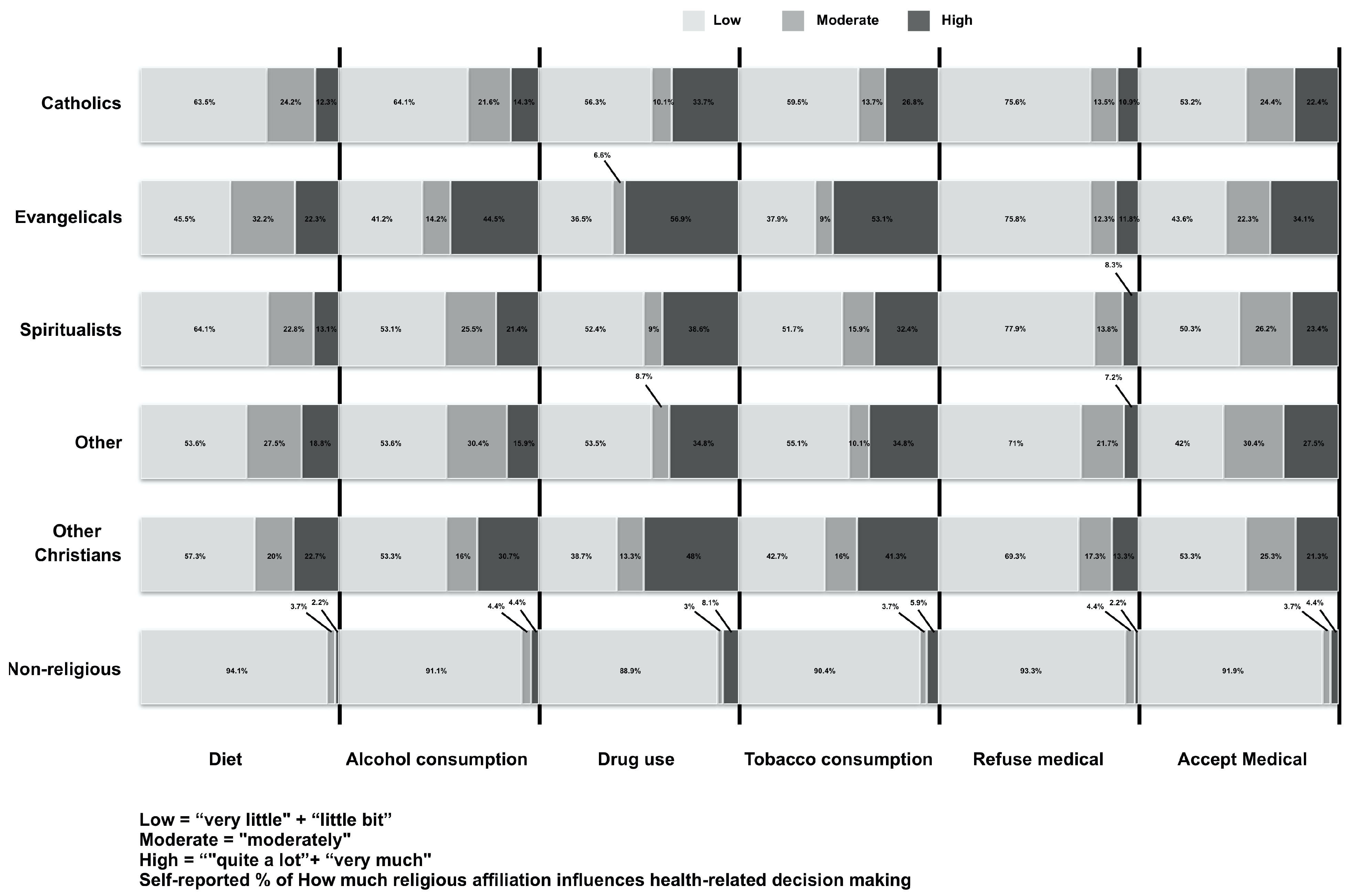
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moreira-Almeida, A.; Neto, F.L.; Koenig, H.G. Religiousness and mental health: A review. Rev. Bras. Psiquiatr. 2006, 36, 176–182. [Google Scholar] [CrossRef]
- Lucchetti, G.; Lucchetti, A.L. Spirituality, religion, and health: Over the last 15 years of field research (1999–2013). Int. J. Psychiatry Med. 2014, 48, 199–215. [Google Scholar] [CrossRef]
- Koenig, H.G. Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry 2012, 2012, 278730. [Google Scholar] [CrossRef] [PubMed]
- Goncalves, J.P.B.; Lucchetti, G.; Menezes, P.R.; Vallada, H. Complementary religious and spiritual interventions in physical health and quality of life: A systematic review of randomized controlled clinical trials. PLoS ONE 2017, 12, e0186539. [Google Scholar] [CrossRef]
- Lucchetti, G.; Lucchetti, A.L.; Puchalski, C.M. Spirituality in medical education: Global reality? J. Relig. Health 2012, 51, 3–19. [Google Scholar] [CrossRef]
- Vieten, C.; Scammell, S.; Pilato, R.; Ammondson, I.; Pargament, K.I.; Lukoff, D. Spiritual and religious competencies for psychologists. Psychol. Relig. Spirit. 2013, 5, 129–144. [Google Scholar] [CrossRef]
- Moreira-Almeida, A.; Koenig, H.G.; Lucchetti, G. Clinical implications of spirituality to mental health: Review of evidence and practical guidelines. Rev. Bras. Psiquiatr. 2014, 36, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Borras, L.; Mohr, S.; Brt, P.Y.; Gillieron, C.; Eytan, A.; Huguelet, P. Religious beliefs in schizophrenia: Their relevance for adherence to treatment. Schizophr. Bull. 2007, 33, 1238–1246. [Google Scholar] [CrossRef] [PubMed]
- Grossoehme, D.H.; Ragsdale, J.R.; Cotton, S.; Meyers, M.A.; Clancy, J.P.; Seid, M.; Joseph, P.M. Using spirituality after an adult CF diagnosis: Cognitive reframing and adherence motivation. J. Health Care Chaplain. 2012, 18, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Koenig, H.G. Spirituality and Health Research: Methods, Measurements, Statistics, and Resources; Templeton Press: Conshohocken, PA, USA, 2012. [Google Scholar]
- Kogan, S.M.; Luo, Z.; Murry, V.M.; Brody, G.H. Risk and protective factors for substance use among African American high school dropouts. Psychol. Addict. Behav. 2005, 19, 382–391. [Google Scholar] [CrossRef]
- Hussain, M.; Walker, C.; Moon, G. Smoking and Religion: Untangling Associations Using English Survey Data. J. Relig. Health 2019, 58, 2263–2276. [Google Scholar] [CrossRef]
- Garcia, G.; Ellison, C.G.; Sunil, T.S.; Hill, T.D. Religion and selected health behaviors among Latinos in Texas. J. Relig. Health 2013, 52, 18–31. [Google Scholar] [CrossRef]
- Peres, M.F.P.; de Oliveira, A.B.; Leão, F.C.; Filho, H.P.V.; Moreira-Almeida, A.; Lucchetti, G. Religious landscape in Brazil: Comparing different representative nationwide approaches to obtain sensitive information in healthcare research. SSM Popul. Health 2018, 6, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.K.; Yu, E.S.; Chen, E.H.; Kim, J.; Brintnall, R.; Vance, S. Smoking behavior, knowledge, and beliefs among Korean Americans. Cancer Pract. 2000, 8, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Craig, B.A.; Morton, D.P.; Kent, L.M.; Gane, A.B.; Butler, T.L.; Rankin, P.M.; Price, K.R. Religious Affiliation Influences on the Health Status and Behaviours of Students Attending Seventh-Day Adventist Schools in Australia. J. Relig. Health 2017, 57, 994–1009. [Google Scholar] [CrossRef]
- VanderWeele, T.J. Religion and health in Europe: Cultures, countries, context. Eur. J. Epidemiol. 2017, 32, 857–861. [Google Scholar] [CrossRef] [PubMed]
- Connor, K.M.; Davidson, J.R.; Lee, L.C. Spirituality, resilience, and anger in survivors of violent trauma: A community survey. J. Trauma Stress. 2003, 16, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Peres, M.F.P.; Kamei, H.H.; Tobo, P.R.; Lucchetti, G. Mechanisms Behind Religiosity and Spirituality’s Effect on Mental Health, Quality of Life and Well-Being. J. Relig. Health 2018, 57, 1842–1855. [Google Scholar] [CrossRef] [PubMed]
- McSherry, W.; Jamieson, S. The qualitative findings from an online survey investigating nurses’ perceptions of spirituality and spiritual care. J. Clin. Nurs. 2013, 22, 3170–3182. [Google Scholar] [CrossRef] [PubMed]
- Selman, L.; Young, T.; Vermandere, M.; Stirling, I.; Leget, C. Research priorities in spiritual care: An international survey of palliative care researchers and clinicians. J. Pain Symptom Manag. 2014, 48, 518–531. [Google Scholar] [CrossRef]
- Brandon, D.M.; Long, J.H.; Loraas, T.M.; Mueller-Phillips, J.; Vansant, B. Online Instrument Delivery and Participant Recruitment Services: Emerging Opportunities for Behavioral Accounting Research. Behav. Res. Account. 2013, 26, 1–23. [Google Scholar] [CrossRef]
- Lucchetti, G.; de Almeida, L.G.; Lucchetti, A.L. Religiousness, mental health, and quality of life in Brazilian dialysis patients. Hemodial Int. 2012, 16, 89–94. [Google Scholar] [CrossRef]
- Vitorino, L.M.; Lucchetti, G.; Leao, F.C.; Vallada, H.; Peres, M.F.P. The association between spirituality and religiousness and mental health. Sci. Rep. 2018, 8, 17233. [Google Scholar] [CrossRef]
- Richards, P.S.; Berrett, M.E.; Hardman, R.K.; Eggett, D.L. Comparative efficacy of spirituality, cognitive, and emotional support groups for treating eating disorder inpatients. Eat Disord. 2006, 14, 401–415. [Google Scholar] [CrossRef]
- Smith, F.T.; Hardman, R.K.; Richards, P.S.; Fischer, L. Intrinsic religiousness and spiritual well-being as predictors of treatment outcome among women with eating disorders. Eat Disord. 2003, 11, 15–26. [Google Scholar] [CrossRef]
- Lucchetti, G.; Koenig, H.G.; Pinsky, I.; Laranjeira, R.; Vallada, H. Religious beliefs and alcohol control policies: A Brazilian nationwide study. Rev. Bras. Psiquiatr. 2014, 36, 4–10. [Google Scholar] [CrossRef]
- Witkiewitz, K.; McCallion, E.; Kirouac, M. Religious Affiliation and Spiritual Practices: An Examination of the Role of Spirituality in Alcohol Use and Alcohol Use Disorder. Alcohol. Res. Curr. Rev. 2016, 38, 55–58. [Google Scholar]
- Degenhardt, L.; Chiu, W.T.; Sampson, N.; Kessler, R.C.; Anthony, J.C. Epidemiological patterns of extra-medical drug use in the United States: Evidence from the National Comorbidity Survey Replication, 2001–2003. Drug Alcohol. Depend. 2007, 90, 210–223. [Google Scholar] [CrossRef][Green Version]
- Sajjadi, H.; Ghaedamini Harouni, G.; Sharifian, S.M. Personal, familial and environmental determinants of drug abuse: A causal-comparative study. Glob. J. Health Sci. 2015, 7, 367–374. [Google Scholar] [CrossRef][Green Version]
- Drabble, L.; Trocki, K.F.; Klinger, J.L. Religiosity as a protective factor for hazardous drinking and drug use among sexual minority and heterosexual women: Findings from the National Alcohol Survey. Drug Alcohol. Depend. 2016, 161, 127–134. [Google Scholar] [CrossRef]
- Garrusi, B.; Nakhaee, N. Religion and Smoking: A Review of Recent Literature. Int. J. Psychiatry Med. 2012, 43, 279–292. [Google Scholar] [CrossRef] [PubMed]
- Benjamins, M.R. Religious influences on trust in physicians and the health care system. Int. J. Psychiatry Med. 2006, 36, 69–83. [Google Scholar] [CrossRef]
- Summerskill, W.; Horton, R. Faith-based delivery of science-based care. Lancet 2015, 386, 1709–1710. [Google Scholar] [CrossRef]
- Lucchetti, G.; Bassi, R.M.; Lucchetti, A.L. Taking spiritual history in clinical practice: A systematic review of instruments. Explore 2013, 9, 159–170. [Google Scholar] [CrossRef]
| Categories | Catholics | Evangelicals | Spiritualists | Other | Other Christians | Non-Religious | |
|---|---|---|---|---|---|---|---|
| Variables | Total (n = 496) n(%) | Total (n = 411) n(%) | Total (n = 145) n(%) | Total (n = 69) n(%) | Total (n = 75) n(%) | Total (n = 135) n(%) | |
| Gender | Female | 235 (47.4) | 122 (57.8) | 94 (64.8) | 36 (56.2) | 45 (60) | 63 (43.7) |
| Male | 261 (52.6) | 89 (42.2) | 51 (35.2) | 33 (47.8) | 30 (40.0) | 72 (53.3) | |
| Age Range (years) | 18–25 | 116 (23.4) | 48 (22.7) | 28 (19.3) | 10 (14.5) | 24 (32.0) | 30 (22.2) |
| 26–35 | 93 (18.8) | 48 (22.7) | 31 (21.4) | 14 (20.3) | 18 (24.0) | 27 (20.0) | |
| 36–45 | 103 (20.8) | 46 (21.8) | 37 (25.5) | 16 (23.2) | 8 (10.7) | 24 (17.8) | |
| 46–55 | 80 (16.2) | 22 (10.4) | 23 (15.9) | 18 (26.1) | 12 (16.0) | 22 (16.3) | |
| 56–65 | 72 (14.5) | 34 (16.1) | 14 (9.7) | 7 (10.1) | 9 (12.0) | 18 (13.3) | |
| >65 | 31 (6.3) | 13 (6.2) | 12 (8.3) | 4 (5.8) | 4 (5.3) | 14 (10.4) | |
| Educational Level | Incomplete high school | 18 (3.6) | 16 (7.6) | 5 (3.4) | 9 (13) | 2 (2.7) | 7 (5.2) |
| Completed high school | 192 (38.7) | 105 (49.8) | 41 (28.3) | 33 (47.8) | 29 (38.7) | 52 (38.5) | |
| Completed university | 193 (38.9) | 61 (28.9) | 60 (41.4) | 19 (27.5) | 30 (40.0) | 62 (45.9) | |
| Postgraduated | 93 (18.8) | 29 (13.7) | 39 (26.9) | 8 (11.6) | 14 (18.7) | 14 (10.4) | |
| Marital Status | Single | 149 (30.0) | 56 (26.5) | 43 (29.7) | 24 (34.8) | 29 (38.7) | 74 (54.8) |
| Judicially separated | 12 (2.4) | 6 (2.8) | 3 (2.1) | 0 (0) | 0 (0) | 4 (3.0) | |
| Divorced | 28 (5.6) | 7 (3.3) | 6 (4.1) | 6 (8.7) | 3 (4.0) | 7 (5.2) | |
| Married | 300 (60.5) | 138 (65.4) | 88 (60.7) | 38 (55.1) | 43 (57.3) | 48 (35.6) | |
| Widowed | 7 (1.4) | 4 (1.9) | 5 (3.4) | 1 (1.4) | 0 (0) | 2 (1.5) | |
| Monthly income range (USD) * | >4114 | 46 (10.6) | 14 (8.1) | 12 (10.2) | 5 (9.3) | 5 (7.7) | 8 (6.8) |
| 2058–4114 | 132 (30.5) | 36 (20.8) | 36 (30.5) | 10 (18.5) | 14 (21.5) | 31 (26.5) | |
| 823–2057 | 158 (36.5) | 61 (35.3) | 48 (40.7) | 18 (33.3) | 28 (43.1) | 50 (42.7) | |
| 411–822 | 71 (16.4) | 40 (23.1) | 16 (13.6) | 17 (31.5) | 10 (15.4) | 20 (17.1) | |
| <411 | 26 (6.0) | 22 (12.7) | 6 (5.1) | 4 (7.4) | 8 (12.3) | 8 (6.8) | |
| Race/Color | White | 325 (65.5) | 107 (50.7) | 95 (65.5) | 38 (55.1) | 34 (45.3) | 94 (69.6) |
| Black | 19 (3.8) | 15 (7.1) | 9 (6.2) | 4 (5.8) | 3 (4.0) | 11 (8.1) | |
| Asian | 12 (2.4) | 6 (2.8) | 2 (1.4) | 3 (4.3) | 2 (2.7) | 4 (3.0) | |
| Pardo (mixed) | 138 (27.8) | 81 (38.4) | 38 (26.2) | 22 (31.9) | 36 (48) | 25 (18.5) | |
| Indigenous | 2 (0.4) | 2 (0.9) | 1 (0.7) | 2 (2.9) | 0 (0) | 1 (0.7) | |
| Region | Northeast | 144 (29) | 51 (24.2) | 44 (30.3) | 18 (26.1) | 18 (24) | 33 (24.4) |
| South | 66 (13.3) | 34 (16.1) | 23 (15.9) | 11 (15.9) | 9 (12) | 18 (13.3) | |
| Midwest | 37 (7.5) | 13 (6.2) | 10 (6.9) | 4 (5.8) | 9 (12) | 16 (11.9) | |
| Southeast | 213 (42.9) | 93 (44.1) | 62 (42.8) | 27 (39.1) | 35 (46.7) | 60 (44.4) | |
| North | 36 (7.3) | 20 (9.5) | 6 (4.1) | 9 (13) | 4 (5.3) | 8 (5.9) |
| Catholics | Evangelicals | Spiritualists | Other | Other Christians | Non Religious | |
|---|---|---|---|---|---|---|
| Dating | 0.50 * | 0.41 * | 0.36 * | 0.55 * | 0.49 * | 0.34 * |
| Marriage | 0.51 * | 0.44 * | 0.39 * | 0.46 * | 0.53 * | 0.37 * |
| Friendship | 0.59 * | 0.41 * | 0.37 * | 0.48 * | 0.43 * | 0.50 * |
| Job | 0.62 * | 0.34 * | 0.41 * | 0.42 * | 0.48 * | 0.55 * |
| Dress | 0.50 * | 0.40 * | 0.26 * | 0.44 * | 0.46 * | 0.60 * |
| Volunteers | 0.57 * | 0.34 * | 0.43 * | 0.61 * | 0.64 * | 0.52 * |
| Donation | 0.62 * | 0.37 * | 0.43 * | 0.56 * | 0.56 * | 0.52 * |
| Politics | 0.35 * | 0.22 * | 0.29 * | 0.20 * | 0.44 * | 0.30 * |
| Diet | 0.47 * | 0.32 * | 0.32 * | 0.49 * | 0.32 * | 0.53 * |
| Alcohol | 0.39 * | 0.34 * | 0.43 * | 0.52 * | 0.34 * | 0.44 * |
| Drug use | 0.38 * | 0.29 * | 0.40 * | 0.37 * | 0.45 * | 0.33 * |
| Tobacco | 0.36 * | 0.36 * | 0.49 * | 0.43 * | 0.50 * | 0.33 * |
| Refuse Medical | 0.30 * | 0.19 * | 0.29 * | 0.27 ** | 0.33 * | 0.54 * |
| Acept Medical | 0.61 * | 0.31 * | 0.50 * | 0.59 * | 0.46 * | 0.50 * |
 ; Medium,
; Medium,  ; Weak,
; Weak,  ; Very week,
; Very week,  .
.Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borges, M.; Lucchetti, G.; Leão, F.C.; Vallada, H.; Peres, M.F.P. Religious Affiliations Influence Health-Related and General Decision Making: A Brazilian Nationwide Survey. Int. J. Environ. Res. Public Health 2021, 18, 2873. https://doi.org/10.3390/ijerph18062873
Borges M, Lucchetti G, Leão FC, Vallada H, Peres MFP. Religious Affiliations Influence Health-Related and General Decision Making: A Brazilian Nationwide Survey. International Journal of Environmental Research and Public Health. 2021; 18(6):2873. https://doi.org/10.3390/ijerph18062873
Chicago/Turabian StyleBorges, Marcelo, Giancarlo Lucchetti, Frederico C. Leão, Homero Vallada, and Mario F. P. Peres. 2021. "Religious Affiliations Influence Health-Related and General Decision Making: A Brazilian Nationwide Survey" International Journal of Environmental Research and Public Health 18, no. 6: 2873. https://doi.org/10.3390/ijerph18062873
APA StyleBorges, M., Lucchetti, G., Leão, F. C., Vallada, H., & Peres, M. F. P. (2021). Religious Affiliations Influence Health-Related and General Decision Making: A Brazilian Nationwide Survey. International Journal of Environmental Research and Public Health, 18(6), 2873. https://doi.org/10.3390/ijerph18062873






