Association of Acculturation Status with Longitudinal Changes in Health-Related Quality of Life—Results from a Cohort Study of Adults with Turkish Origin in Germany
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample and Design
2.2. Measures
2.2.1. Health-Related Quality of Life
2.2.2. Acculturation
2.2.3. Sociodemographic Covariates
2.3. Statistical Analyses
3. Results
3.1. Characteristics of the Study Sample
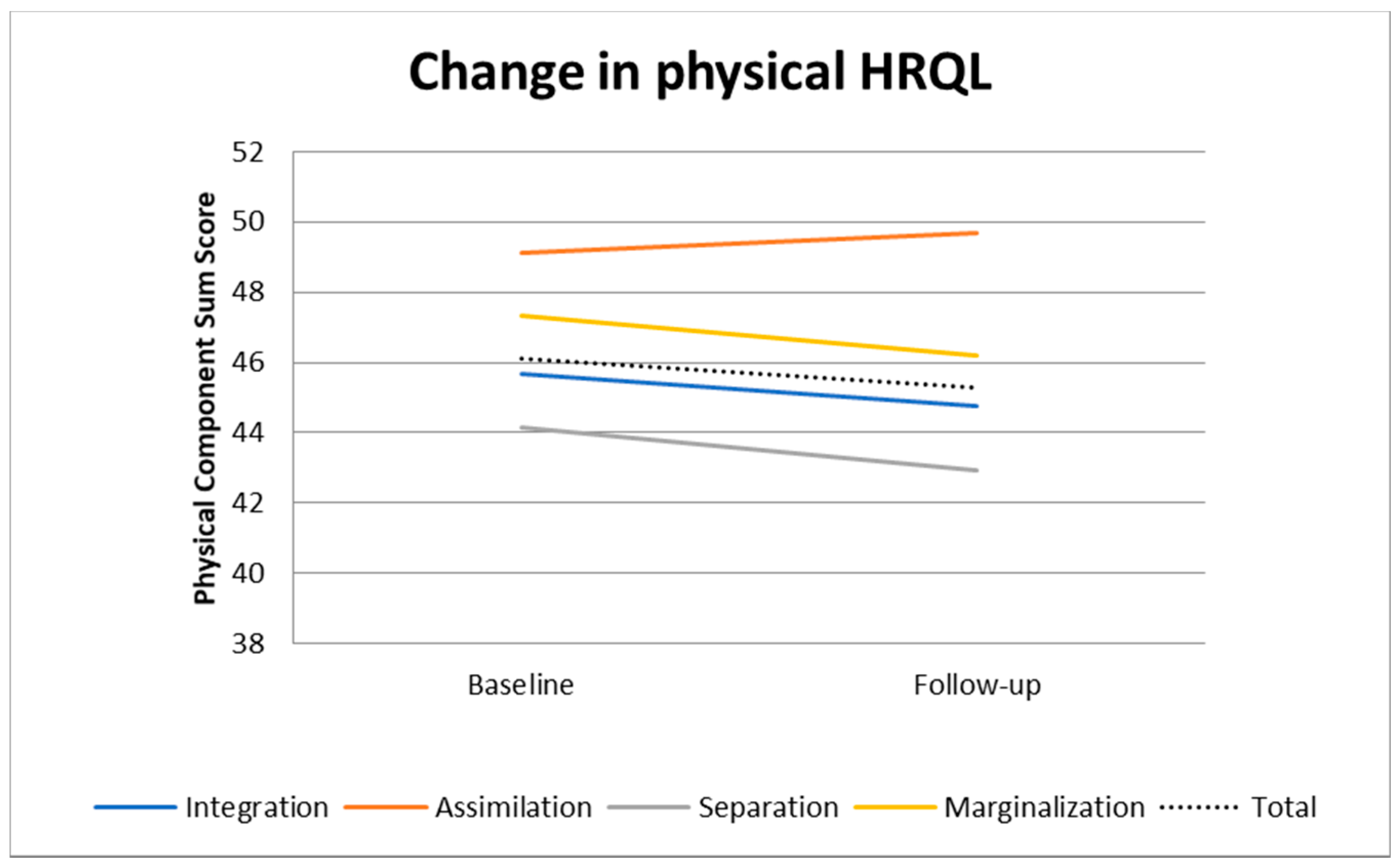
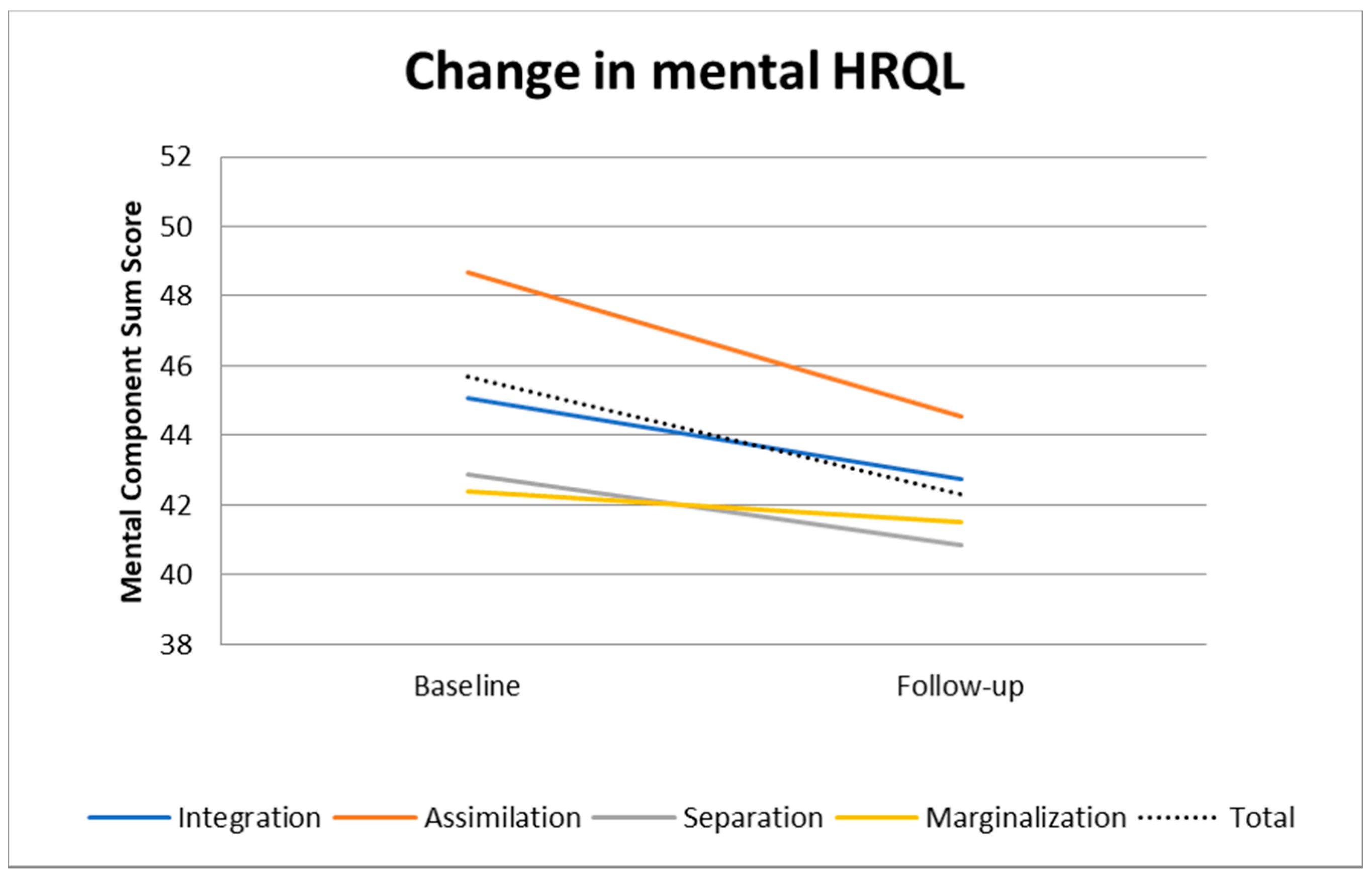
3.2. Changes in HRQL
3.3. Association of Acculturation with HRQL
3.3.1. Cross-Sectional Analysis
3.3.2. Longitudinal Analysis
4. Discussion
4.1. Main Study Findings and Comparison with Other Studies
4.2. Strengths and Limitations
4.3. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Report on the Health of Refugees and Migrants in the WHO European Region; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Ujcic-Voortman, J.K.; Baan, C.A.; Seidell, J.C.; Verhoeff, A.P. Obesity and cardiovascular disease risk among Turkish and Moroccan migrant groups in Europe: A systematic review. Obes. Rev. 2012, 13, 2–16. [Google Scholar] [CrossRef] [PubMed]
- Reeske, A.; Spallek, J.; Razum, O. Changes in smoking prevalence among first- and second-generation Turkish migrants in Germany - an analysis of the 2005 Microcensus. Int. J. Equity Health 2009, 8, 26. [Google Scholar] [CrossRef]
- Hjörleifsdottir-Steiner, K.; Satman, I.; Sundquist, J.; Kaya, A.; Wändell, P. Diabetes and impaired glucose tolerance among Turkish immigrants in Sweden. Diabetes Res. Clin. Pract. 2011, 92, 118–123. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Beutel, M.E.; Jünger, C.; Klein, E.M.; Wild, P.; Lackner, K.J.; Blettner, M.; Banerjee, M.; Michal, M.; Wiltink, J.; Brähler, E. Depression, anxiety and suicidal ideation among 1st and 2nd generation migrants-results from the Gutenberg health study. BMC Psychiatry 2016, 16, 1–10. [Google Scholar] [CrossRef]
- Levecque, K.; Lodewyckx, I.; Vranken, J. Depression and generalised anxiety in the general population in Belgium: A comparison between native and immigrant groups. J. Affect. Disord. 2007, 97, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Ünlü Ince, B.; Fassaert, T.; de Wit, M.A.S.; Cuijpers, P.; Smit, J.; Ruwaard, J.; Riper, H. The relationship between acculturation strategies and depressive and anxiety disorders in Turkish migrants in the Netherlands. BMC Psychiatry 2014, 14, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Morawa, E.; Erim, Y. Acculturation and depressive symptoms among Turkish immigrants in Germany. Int. J. Environ. Res. Public Health 2014, 11, 9503–9521. [Google Scholar] [CrossRef]
- International Organization for Migration. World Migration Report 2020; International Organization for Migration: Grand-Saconnex, Switzerland, 2020. [Google Scholar]
- Solé-Auró, A.; Crimmins, E.M. Health of immigrants in European countries. Int. Migr. Rev. 2008, 42, 861–876. [Google Scholar] [CrossRef]
- Walter, U.; Bisson, S.; Gerken, U.; Machleidt, W.; Krauth, C. Gesundheits- und Präventionsverhalten von Personen mit und ohne Migrationshintergrund. Gesundheitswesen Suppl. 2015, 77, S85–S86. [Google Scholar] [CrossRef]
- Gazard, B.; Frissa, S.; Nellums, L.; Hotopf, M.; Hatch, S.L. Challenges in researching migration status, health and health service use: An intersectional analysis of a South London community. Ethn. Health 2015, 20, 564–593. [Google Scholar] [CrossRef]
- Kristiansen, M.; Razum, O.; Tezcan-Güntekin, H.; Krasnik, A. Aging and health among migrants in a European perspective. Public Health Rev. 2016, 37, 1–14. [Google Scholar] [CrossRef]
- Sand, G.; Gruber, S. Differences in Subjective Well-being Between Older Migrants and Natives in Europe. J. Immigr. Minor. Health 2018, 20, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Salgado, H.; Castañeda, S.F.; Talavera, G.A.; Lindsay, S.P. The role of social support and acculturative stress in health-related quality of life among day laborers in Northern San Diego. J. Immigr. Minor. Health 2012, 14, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Toselli, S.; Gualdi-Russo, E.; Marzouk, D.; Sundquist, J.; Sundquist, K. Psychosocial health among immigrants in central and southern Europe. Eur. J. Public Health 2014, 24, 26–30. [Google Scholar] [CrossRef]
- Pantzer, K.; Rajmil, L.; Tebé, C.; Codina, F.; Serra-Sutton, V.; Ferrer, M.; Ravens-Sieberer, U.; Simeoni, M.C.; Alonso, J. Health related quality of life in immigrants and native school aged adolescents in Spain. J. Epidemiol. Community Health 2006, 60, 694–698. [Google Scholar] [CrossRef] [PubMed]
- Brand, T.; Samkange-Zeeb, F.; Ellert, U.; Keil, T.; Krist, L.; Dragano, N.; Jöckel, K.-H.; Razum, O.; Reiss, K.; Greiser, K.H.; et al. Acculturation and health-related quality of life: Results from the German National Cohort migrant feasibility study. Int. J. Public Health 2017, 62, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, P.T. Psychological problems of Turkish migrants in West Germany. Am. J. Psychother. 1981, 35, 187–194. [Google Scholar] [CrossRef]
- Aichberger, M.C.; Bromand, Z.; Heredia Montesinos, A.; Temur-Erman, S.; Mundt, A.; Heinz, A.; Rapp, M.A.; Schouler-Ocak, M. Socio-economic status and emotional distress of female Turkish immigrants and native German women living in Berlin. Eur. Psychiatry 2012, 27, S10–S16. [Google Scholar] [CrossRef]
- Yoon, E.; Chang, C.T.; Kim, S.; Clawson, A.; Cleary, S.E.; Hansen, M.; Bruner, J.P.; Chan, T.K.; Gomes, A.M. A meta-analysis of acculturation/enculturation and mental health. J. Couns. Psychol. 2013, 60, 15–30. [Google Scholar] [CrossRef]
- Yoon, E.; Hacker, J.; Hewitt, A.; Abrams, M.; Cleary, S. Social connectedness, discrimination, and social status as mediators of acculturation/enculturation and well-being. J. Couns. Psychol. 2012, 59, 86–96. [Google Scholar] [CrossRef]
- Verhagen, I.; Ros, W.J.G.; Steunenberg, B.; de Wit, N.J. Ethnicity does not account for differences in the health-related quality of life of Turkish, Moroccan, and Moluccan elderly in the Netherlands. Health Qual. Life Outcomes 2014, 12, 1–8. [Google Scholar] [CrossRef]
- Cho, S.; Lee, H.; Oh, E.G.; Kim, G.S.; Kim, Y.C.; Park, C. gi Health-related quality of life among migrant workers: The impact of health-promoting behaviors. Nurs. Health Sci. 2020, 22, 318–327. [Google Scholar] [CrossRef]
- Schumann, M.; Bug, M.; Kajikhina, K.; Koschollek, C.; Bartig, S.; Lampert, T.; Santos-Hövener, C. SSM-Population Health The concept of acculturation in epidemiological research among migrant populations: A systematic review. SSM Popul. Health 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Rudmin, F.W. Critical History of the Acculturation Psychology of Assimilation, Separation, Integration, and Marginalization. Rev. Gen. Psychol. 2003, 7, 3–37. [Google Scholar] [CrossRef]
- Gordon, M.M. Assimilation in Americal Life; 1964; ISBN 9788578110796. Available online: https://research.vu.nl/en/publications/the-professional-teacher-educator-roles-behaviour-and-professiona (accessed on 31 December 2014).
- Berry, J.W. Immigration, Acculturation, and Adaptation. Appl. Psychol. 1997, 46, 5–34. [Google Scholar] [CrossRef]
- Berry, J.W. Acculturation: A Personal Journey across Cultures; Cambridge University Press: Cambridge, UK, 2019; ISBN 9781108589666. [Google Scholar]
- Goh, Y.S.; Lopez, V. Acculturation, quality of life and work environment of international nurses in a multi-cultural society: A cross-sectional, correlational study. Appl. Nurs. Res. 2016, 30, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Berry, J.W.; Sabatier, C. Acculturation, discrimination, and adaptation among second generation immigrant youth in Montreal and Paris. Int. J. Intercult. Relations 2010, 34, 191–207. [Google Scholar] [CrossRef]
- Behrens, K.; Del Pozo, M.A.; Großhennig, A.; Sieberer, M.; Graef-Calliess, I.T. How much orientation towards the host culture is healthy? Acculturation style as risk enhancement for depressive symptoms in immigrants. Int. J. Soc. Psychiatry 2015, 61, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Borraccino, A.; Charrier, L.; Berchialla, P.; Lazzeri, G.; Vieno, A.; Dalmasso, P.; Lemma, P. Perceived well-being in adolescent immigrants: It matters where they come from. Int. J. Public Health 2018, 63, 1037–1045. [Google Scholar] [CrossRef]
- Prapas, C.; Mavreas, V. The Relationship Between Quality of Life, Psychological Wellbeing, Satisfaction with Life and Acculturation of Immigrants in Greece. Cult. Med. Psychiatry 2019, 43, 77–92. [Google Scholar] [CrossRef]
- Urzúa, A.; Ferrer, R.; Canales Gaete, V.; Núñez Aragón, D.; Ravanal Labraña, I.; Tabilo Poblete, B. The influence of acculturation strategies in quality of life by immigrants in Northern Chile. Qual. Life Res. 2017, 26, 717–726. [Google Scholar] [CrossRef]
- Nap, A.; Van Loon, A.; Peen, J.; Van Schaik, D.J.F.; Beekman, A.T.F.; Dekker, J.J.M. The influence of acculturation on mental health and specialized mental healthcare for non-western migrants. Int. J. Soc. Psychiatry 2015, 61, 530–538. [Google Scholar] [CrossRef]
- Nesterko, Y.; Turrión, C.M.; Friedrich, M.; Glaesmer, H. Trajectories of health-related quality of life in immigrants and non-immigrants in Germany: A population-based longitudinal study. Int. J. Public Health 2019, 64, 49–58. [Google Scholar] [CrossRef]
- Statistisches Bundesamt (Destatis). Bevölkerung und Erwerbstätigkeit: Bevölkerung mit Migrationshintergrund–Ergebnisse des Mikrozensus 2019; Statistisches Bundesamt (Destatis): Wiesbaden, Germany, 2020. [Google Scholar]
- Reiss, K.; Dragano, N.; Ellert, U.; Fricke, J.; Greiser, K.H.; Keil, T.; Krist, L.; Moebus, S.; Pundt, N.; Schlaud, M.; et al. Comparing sampling strategies to recruit migrants for an epidemiological study. Results from a German feasibility study. Eur. J. Public Health 2014, 24, 721–726. [Google Scholar] [CrossRef]
- Krist, L.; Dornquast, C.; Reinhold, T.; Solak, S.; Durak, M.; Keil, T. Strategies to enhance follow-up response in a cohort study with Berliners of Turkish descent. Eur. J. Public Health 2019, 29, 400–401. [Google Scholar] [CrossRef]
- Ware, J.; Kosinski, M.; Dewey, J.; Gandek, B. How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8TM Health Survey.–ScienceOpen; QualyMetric: Lincoln, RI, USA, 2001. [Google Scholar]
- Ware, J.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Maruish, M.E. (Ed.) User’s Manual for the SF-12v2 Health Survey, 3rd ed.; ScienceOpen: Berlin, Germany, 2012; ISBN 1891810294. [Google Scholar]
- Ellert, U.; Lampert, T.; Ravens-Sieberer, U. Messung der gesundheitsbezogenen Lebensqualität mit dem SF-8. Eine Normstichprobe für Deutschland. Bundesgesundheitsblatt-Gesundheitsforsch.-Gesundheitsschutz 2005, 48, 1330–1337. [Google Scholar] [CrossRef] [PubMed]
- Lang, L.; Zhang, L.; Zhang, P.; Li, Q.; Bian, J.; Guo, Y. Evaluating the reliability and validity of SF-8 with a large representative sample of urban Chinese. Health Qual. Life Outcomes 2018, 16, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Schofield, M.J.; Mishra, G. Validity of the SF-12 compared with the SF-36 Health Survey in pilot studies of the Australian Longitudinal Study on Women’s Health. J. Health Psychol. 1998, 3, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Gandek, B.; Ware, J.E.; Aaronson, N.K.; Apolone, G.; Bjorner, J.B.; Brazier, J.E.; Bullinger, M.; Kaasa, S.; Leplege, A.; Prieto, L.; et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: Results from the IQOLA Project. J. Clin. Epidemiol. 1998, 51, 1171–1178. [Google Scholar] [CrossRef]
- Bongard, S.; Pogge, S.F.; Arslaner, H.; Rohrmann, S.; Hodapp, V. Acculturation and cardiovascular reactivity of second-generation Turkish migrants in Germany. J. Psychosom. Res. 2002, 53, 795–803. [Google Scholar] [CrossRef]
- Bongard, S.; Etzler, S.F.E. FRACC: Frankfurt Acculturation Scale; Hogrefe: Göttingen, Germany, 2020. [Google Scholar]
- Aksit, N. Educational reform in Turkey. Int. J. Educ. Dev. 2007, 27, 129–137. [Google Scholar] [CrossRef]
- Twisk, J.W.R. Applied Longitudinal Data Analysis for Epidemiology: A Practical Guide, 2nd ed.; Cambridge University Press: Camebridge, UK, 2013. [Google Scholar]
- Donders, A.R.T.; van der Heijden, G.J.M.G.; Stijnen, T.; Moons, K.G.M. Review: A gentle introduction to imputation of missing values. J. Clin. Epidemiol. 2006, 59, 1087–1091. [Google Scholar] [CrossRef] [PubMed]
- de la Cruz, F.A.; Padilia, G.V.; Butts, E. Validating a Short Acculturation Scale For Filipino-Americans. Search Res. 1998, 10, 453–460. [Google Scholar]
- Adedeji, A.; Bullinger, M. Subjective integration and quality of life of Sub-Saharan African migrants in Germany. Public Health 2019, 174, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Antidiskriminierungsstelle des Bundes. Diskriminierungserfahrungen von Migrant_innen; Antidiskriminierungsstelle des Bundes: Berlin, Germany, 2012. [Google Scholar]
- Antidiskriminierungsstelle des Bundes. Akzeptanz Religiöser und Weltanschaulicher Vielfalt in Deutschland Ergebnisse einer Repräsentativen Umfrage; Antidiskriminierungsstelle des Bundes: Berlin, Germany, 2016. [Google Scholar]
- Decker, O.; Kiess, J.; Brähler, E. Die Enthemmte Mitte. Autoritäre und Rechtsextreme Einstellung in Deutschland; Psychosozial-Verlag: Gießen, Germany, 2016; ISBN 9783837926309. [Google Scholar]
- Brand, T.; Samkange-Zeeb, F.; Dragano, N.; Keil, T.; Krist, L.; Yesil-Jürgens, R.; Schlaud, M.; Jöckel, K.H.; Razum, O.; Reiss, K.; et al. Participation of Turkish Migrants in an Epidemiological Study: Does the Recruitment Strategy Affect the Sample Characteristics? J. Immigr. Minor. Health 2019, 21, 811–819. [Google Scholar] [CrossRef] [PubMed]
- Murray, K.E.; Klonoff, E.A.; Garcini, L.M.; Ullman, J.B.; Wall, T.L.; Myers, M.G. Assessing Acculturation Over Time: A Four-year Prospective Study of Asian American Young Adults. Asian Am. J. Psychol 2014, 5, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.M.; Wang, E.; Szalacha, L.A.; Sorokin, O. Longitudinal Changes in Acculturation for Immigrant Women from the Former Soviet Union. J Cross Cult Psychol. 2009, 40, 400–415. [Google Scholar] [CrossRef]
- Salman, R. Gesundheit mit Migranten für Migranten - Die MiMi Präventionstechnologie als interkulturelles Health-Literacy-Programm. Public Health Forum 2015, 23, 109–112. [Google Scholar] [CrossRef]
| N | Men (n = 118) | Women (n = 211) | Total (n = 330) § |
|---|---|---|---|
| Baseline variables | |||
| Age groups (%) | |||
| 20–29 | 9.3 | 19.0 | 15.5 |
| 30–39 | 20.3 | 26.1 | 24.0 |
| 40–49 | 39.0 | 28.0 | 31.9 |
| 50–59 | 19.5 | 14.7 | 16.4 |
| 60–69 | 11.9 | 12.3 | 12.2 |
| Country of birth (%) | |||
| Turkey | 79.7 | 70.6 | 73.9 |
| Germany | 13.6 | 24.6 | 20.7 |
| Missing | 6.8 | 4.7 | 5.5 |
| Educational level (%) | |||
| Low | 30.0 | 17.0 | 37.4 |
| Medium | 29.7 | 35.6 | 26.5 |
| High | 31.2 | 42.4 | 25.1 |
| Missing | 9.1 | 5.1 | 10.9 |
| Monthly net income (%) | |||
| <1000 Euro | 16.1 | 22.8 | 20.4 |
| 1000–<2500 Euro | 44.9 | 41.2 | 42.6 |
| 2500 Euro or more | 29.7 | 20.9 | 24.0 |
| Missing | 9.3 | 15.2 | 13.1 |
| Acculturation status (%) | |||
| Integration | 20.3 | 11.9 | 14.9 |
| Assimilation | 33.1 | 21.3 | 25.5 |
| Separation | 17.8 | 23.7 | 21.6 |
| Marginalization | 11.0 | 10.4 | 10.6 |
| Missing | 17.8 | 32.7 | 27.4 |
| PCS (mean, SD) | 47.6 (9.1) | 45.2 (10.2) | 46.1 (9.8) |
| MCS (mean, SD) | 49.0 (10.4) | 43.7 (11.0) | 45.7 (11.0) |
| Follow-up variables | |||
| PCS (mean, SD) | 48.4 (9.3) | 43.6 (10.5) | 45.3 (10.3) |
| MCS (mean, SD) | 45.8 (9.8) | 40.5 (10.5) | 42.3 (10.6) |
| PCS Baseline | PCS Follow-Up | MCS Baseline | MCS Follow-Up | |
|---|---|---|---|---|
| N | 287 | 289 | 287 | 289 |
| Acculturation status (Ref. Assimilation) | ||||
| Integration | −1.86 | −3.95 * | −2.96 | −1.87 |
| [−5.69, 1.98] | [−7.37, −0.54] | [−6.59, 0.66] | [−5.89, 2.16] | |
| Separation | −3.44 | −3.40 * | −4.45 * | −2.87 |
| [−7.50, 0.61] | [−6.85, −0.04] | [−8.57, −0.34] | [−638, 0.63] | |
| Marginalization | −0.88 | −1.92 | −2.90 | −1.81 |
| [−4.65, 2.87] | [−5.27, 1.43] | [−7.98, 2.17] | [−6.62, 2.98] | |
| Sex (Ref. Men) | ||||
| Women | −1.60 | −3.89 ** | −4.08 ** | −3.51 ** |
| [−4.10, 0.89] | [−6.20, −1.57] | [−6.87, −1.30] | [−6.05, −0.97] | |
| Monthly net income (Ref. <1000€) | ||||
| 1000–<2500€ | 2.01 | 2.52 | 3.84 * | 2.29 |
| [−1.10, 5.12] | [−0.42, 5.47] | [0.33, 7.36] | [0.03, 6.25] | |
| ≥2500€ | 4.65 ** | 6.31 *** | 7.16 *** | 6.97 *** |
| [1.19, 8.12] | [3.01, 9.61] | [3.21, 11.1] | [3.30, 10.64] | |
| Educational level (Ref. Low) | ||||
| Medium | 0.06 | 1.30 | −0.56 | 1.17 |
| [−2.89, 3.00] | [−1.47, 4.07] | [−3.84, 2.72] | [−1.93, 4.27] | |
| High | 2.52 | 1.97 | 0.74 | 2.51 |
| [−0.48, 5.48] | [−0.85, 4.78] | [−2.62, 4.11] | [−0.62, 5.65] |
| PCS | MCS | |||
|---|---|---|---|---|
| N | 585 | 585 | ||
| Coef. | [95% CI] | Coef. | [95% CI] | |
| Change over time | 0.24 | [−1.94, 2.41] | −3.86 ** | [−6.21, −1.51] |
| Acculturation status (Ref. Assimilation) | ||||
| Integration | −1.91 | [−5.65, 1.82] | −3.13 | [−6.63, 0.35] |
| Separation | −3.02 | [−6.87, 0.83] | −4.04 * | [−8.00, −0.08] |
| Marginalization | −1.03 | [−4.71, 2.63] | −2.37 | [−7.27, 2.51] |
| Time by acculturation (Ref. Time#Assimilation) | ||||
| Time#Integration | −2.04 | [−6.68, 2.61] | 1.44 | [−3.24, 6.13] |
| Time#Separation | −0.86 | [−4.16, 2.45] | 1.06 | [−2.41, 4.53] |
| Time#Marginalization | −0.93 | [−5.06, 3.19] | 0.27 | [−4.11, 4.65] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krist, L.; Dornquast, C.; Reinhold, T.; Becher, H.; Jöckel, K.-H.; Schmidt, B.; Schramm, S.; Icke, K.; Danquah, I.; Willich, S.N.; et al. Association of Acculturation Status with Longitudinal Changes in Health-Related Quality of Life—Results from a Cohort Study of Adults with Turkish Origin in Germany. Int. J. Environ. Res. Public Health 2021, 18, 2827. https://doi.org/10.3390/ijerph18062827
Krist L, Dornquast C, Reinhold T, Becher H, Jöckel K-H, Schmidt B, Schramm S, Icke K, Danquah I, Willich SN, et al. Association of Acculturation Status with Longitudinal Changes in Health-Related Quality of Life—Results from a Cohort Study of Adults with Turkish Origin in Germany. International Journal of Environmental Research and Public Health. 2021; 18(6):2827. https://doi.org/10.3390/ijerph18062827
Chicago/Turabian StyleKrist, Lilian, Christina Dornquast, Thomas Reinhold, Heiko Becher, Karl-Heinz Jöckel, Börge Schmidt, Sara Schramm, Katja Icke, Ina Danquah, Stefan N. Willich, and et al. 2021. "Association of Acculturation Status with Longitudinal Changes in Health-Related Quality of Life—Results from a Cohort Study of Adults with Turkish Origin in Germany" International Journal of Environmental Research and Public Health 18, no. 6: 2827. https://doi.org/10.3390/ijerph18062827
APA StyleKrist, L., Dornquast, C., Reinhold, T., Becher, H., Jöckel, K.-H., Schmidt, B., Schramm, S., Icke, K., Danquah, I., Willich, S. N., Keil, T., & Brand, T. (2021). Association of Acculturation Status with Longitudinal Changes in Health-Related Quality of Life—Results from a Cohort Study of Adults with Turkish Origin in Germany. International Journal of Environmental Research and Public Health, 18(6), 2827. https://doi.org/10.3390/ijerph18062827









