Housing Risk Factors Associated with Respiratory Disease: A Systematic Review
Abstract
:1. Introduction
2. Related Works
3. Aim and Research Questions
- What are the housing-related risk factors reported in the literature associated with respiratory illnesses and how are they categorised?
- What are the demographic characteristics of occupants who are susceptible to the identified risks?
- What mitigation solutions have been implemented to reduce the effects of housing-related risk factors on occupants’ respiratory health?
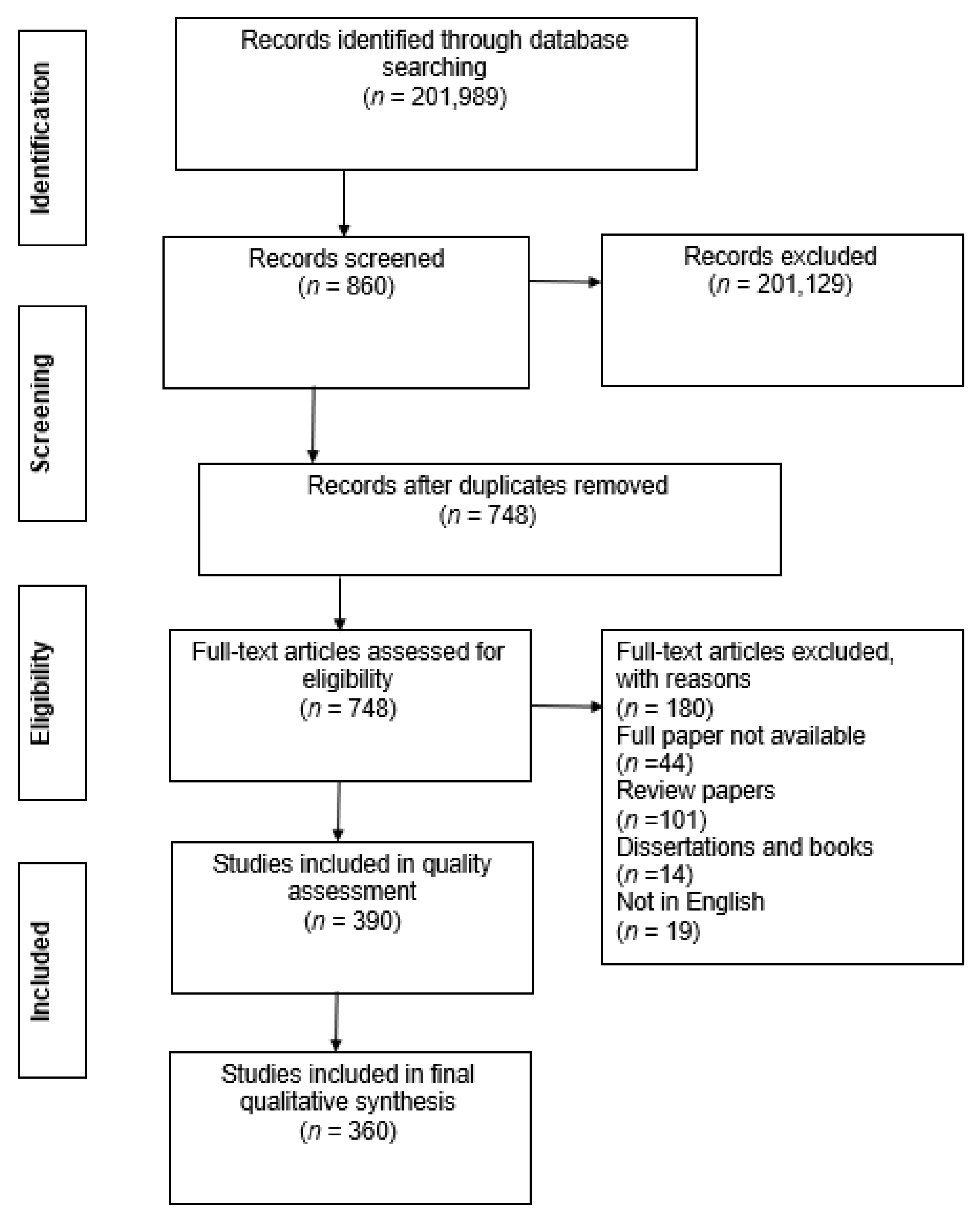
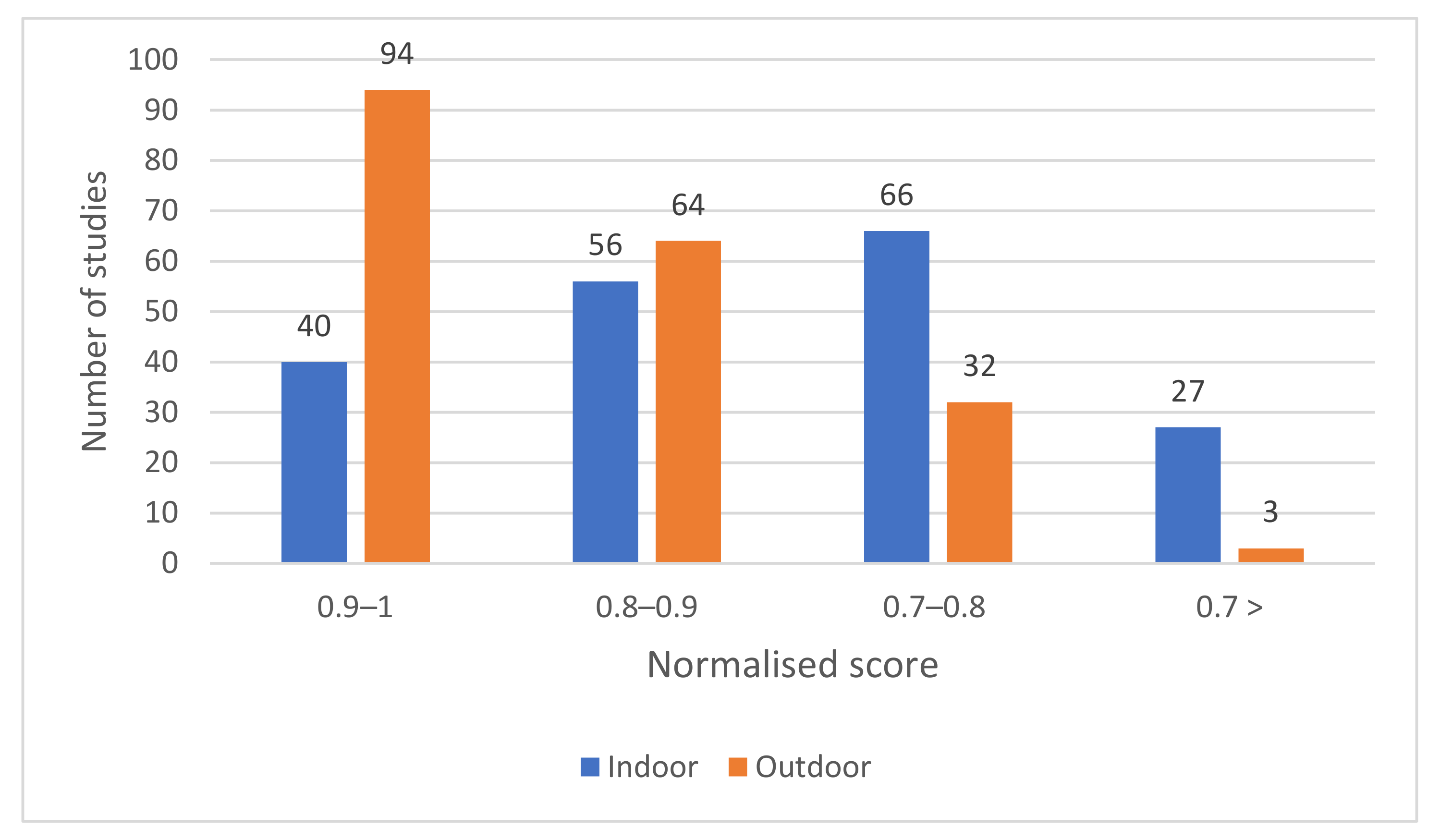
4. Methodology
5. Results
5.1. Publication Sources of the Reviewed Articles
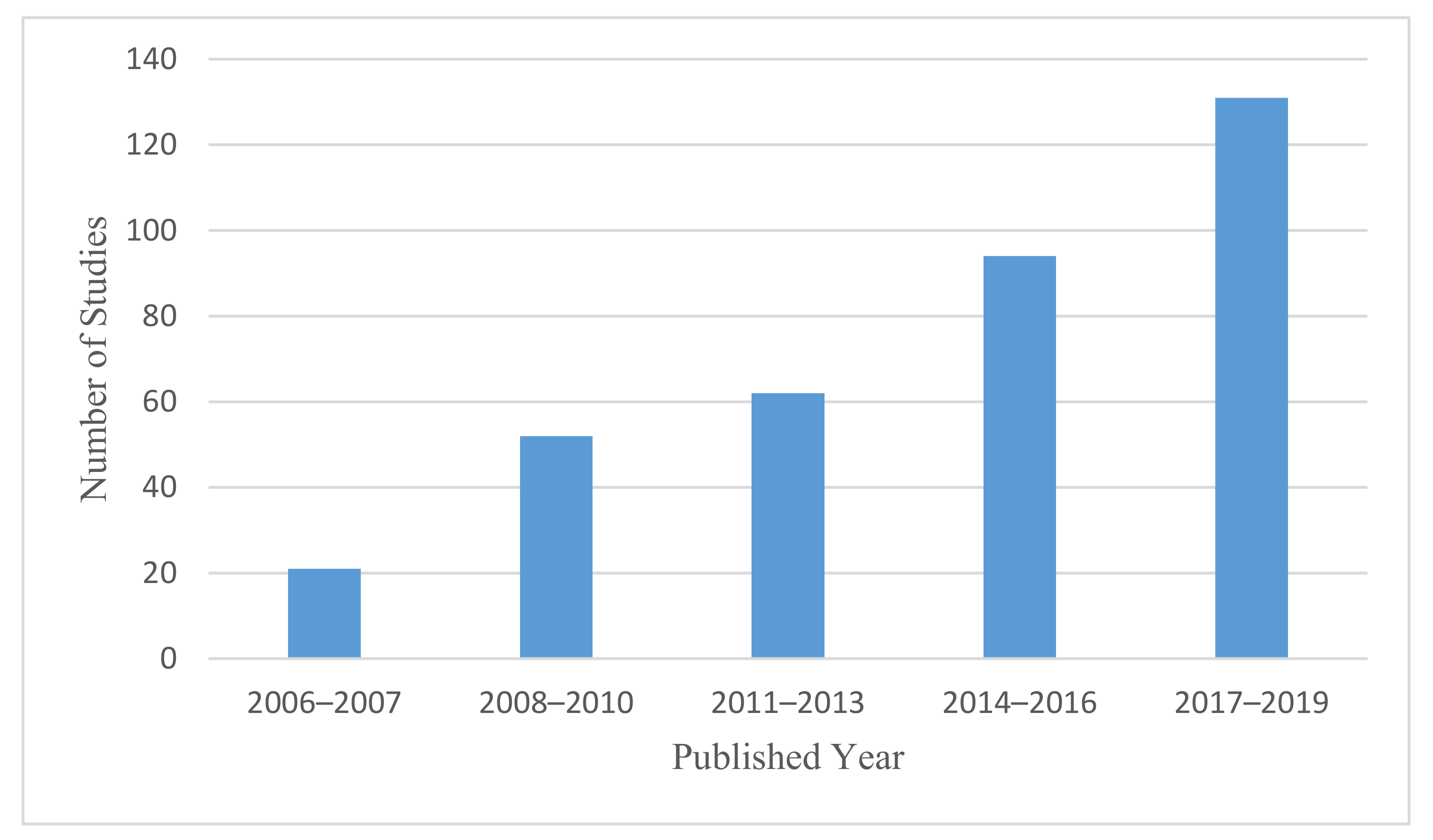
5.2. Chronological Distribution of the Reviewed Articles
5.3. Geographical Distribution of Identified Articles
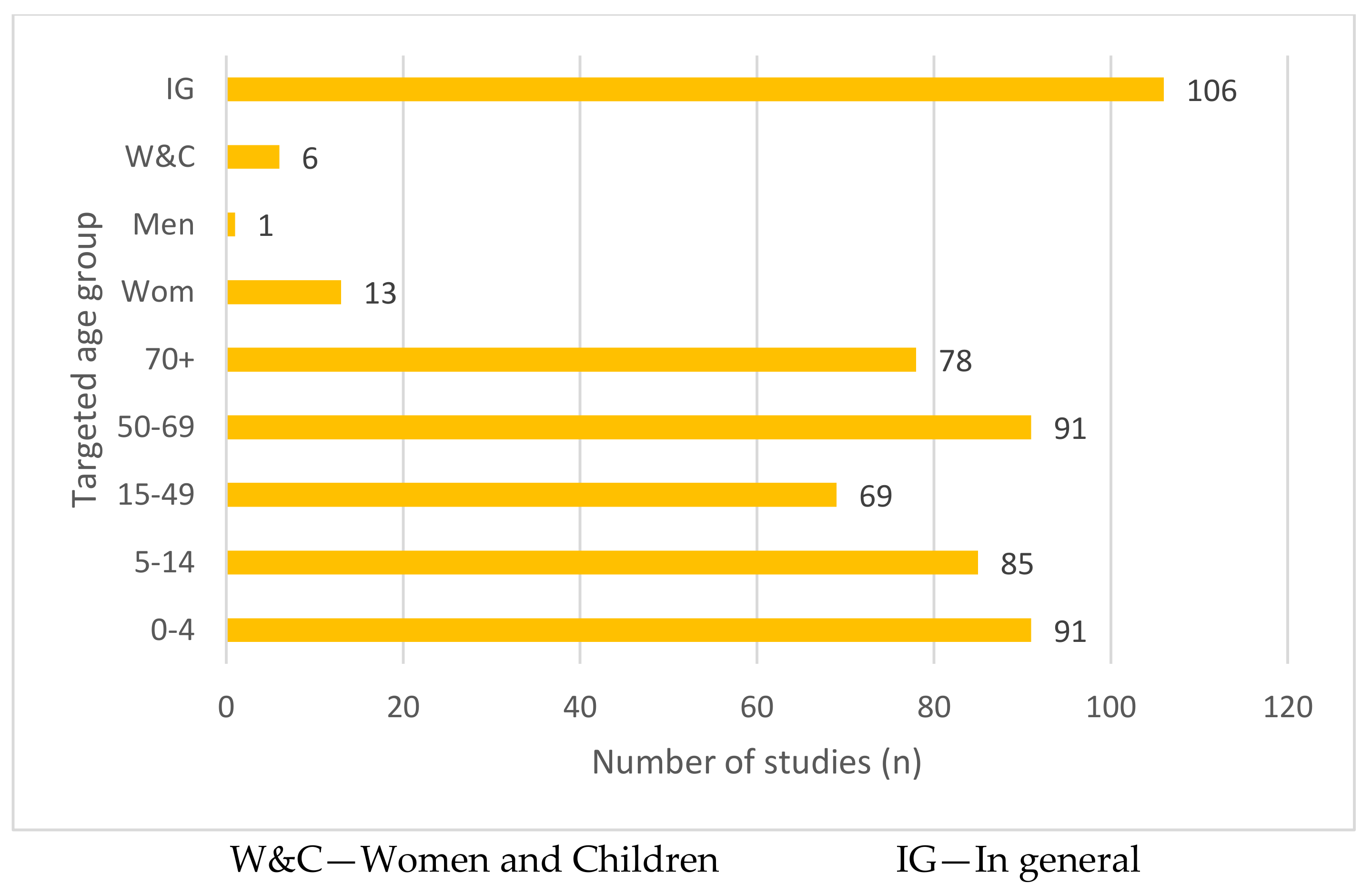
5.4. Demographics of the Population under Investigation
5.5. Housing-Related Factors Associated with Respiratory Illness
| Factor Ranking | Factor | Category | % of Factor Appearance | Respiratory Diseases (RD) | Pollutant/Effect | Selected Sources |
|---|---|---|---|---|---|---|
| 1 | Living close to city areas, main roads, highways or industrial areas | Outdoor environment | 34% | Acute and chronic respiratory diseases (Asthma, COPD, pneumonia, tuberculosis) | PM, CO, NOx, SO2, O3, VOC | Morgenstern et al. [39], Ji and Zhao [40] |
| 2 | Exposure to solid fuel | Indoor air pollution | 17% | Asthma, COPD, pneumonia, ARI, URD (both acute and chronic respiratory infection) | PM2.5, PM10, CO, NO2, SO2 | Da Silva et al. [41], Murray et al. [42], Ranathunga et al. [43] |
| 3 | Meteorological factors | Outdoor environment | 11% | Asthma, pneumonia, RSV | Extreme temperature and humidity, rainfall and high atmospheric pressure related to an increase in the rate of RDs | Han et al. [44], Fernandez-Raga et al. [45], Son et al. [46] |
| 4 | Exposure to ETS | Indoor air pollution | 9% | Asthma, ARI, lung cancer, COPD, URD | PM10, PM2.5, CO, methane | Walker et al. [47], Håberg et al. [48] |
| 5 | Moisture or mould damage | Structural related | 7% | Asthma, pneumonia, URD | Allergens, bacteria | Park et al. [49], Karvonen et al. [50] |
| 6 | Exposure to radon | Indoor air pollution | 4% | Lung cancer | Radioactive gas | Bräuner et al. [51], Dempsey et al. [52] |
| 7 | Exposure to indoor asbestos fibers | Indoor air pollution | 3% | Malignant mesothelioma, lung cancer, lower lung fibrosis | Asbestos fibers | Reid et al. [53], Visonà et al. [54] |
| 8 | Carpet floors and HDM | Non-structural related | 2% | ARI | Dust, PM | Dales et al. [55], Shendell et al. [56] |
| 9 | Presence of pets | Non-structural | 2% | Asthma and wheeze | Allergens | Fernandes et al. [57], Dong et al. [58] |
| 10 | Exposure to wildland fire | Outdoor environment | 2% | Asthma, COPD | PM10, PM2.5 | Liu et al. [59], Shaposhnikov et al. [60] |
| 11 | Exposure to VOCs | Indoor air pollution | 2% | Asthma, pneumonia | VOCs | Cipolla et al. [61], Jiang et al. [62] |
| 12 | Crowding | Non-structural | 1% | ARI | Inadequate ventilation | Taksande and Yeole [5], Murray et al. [63] |
| 13 | Exposure to dust storms | Outdoor environment | 1% | Asthma, ARI | Dust | Trianti et al. [64], Thalib and Al-Taiar [65] |
| 14 | Pollen | Outdoor environment | 1% | Asthma, eczema, allergic rhinitis | Allergens | Linares et al. [66], Li et al. [67] |
| 15 | Use of ozone emitting air cleaners | Indoor air pollution | 1% | Asthma, wheeze, dry cough | Ozone | Liu et al. [68], Nguyen et al. [69] |
| 16 | Daily cleaning activities (ammonia or chlorine-based cleaners) | Non-structural | 0.5% | Asthma | Ammonia | Wang, Su, Hsu, Wang and Wu [4], Medina et al. [70] |
| 17 | Drying clothes inside | Non-structural | 0.5% | ARI, URD | Facilitate the growth of mould spores and HDM | Mengersen et al. [71], Turunen et al. [72] |
| 18 | Living close to mines | Outdoor environment | 0.5% | Asthma, lung cancer | Dust | Herrera et al. [73], Pun et al. [74] |
| 19 | Exposure to Portland cement dust and volcanic ash | Outdoor environment | 0.5% | Lung cancer | Dust | Eom et al. [75], Higuchi et al. [76] |
5.5.1. Outdoor Environment Related Factors
5.5.2. Indoor Air Pollution-Related Factors
5.5.3. Non-Structure-Related Factors
5.5.4. Housing Structure-Related Factors
5.6. Mitigation Solutions Suggested in the Articles
6. Discussion
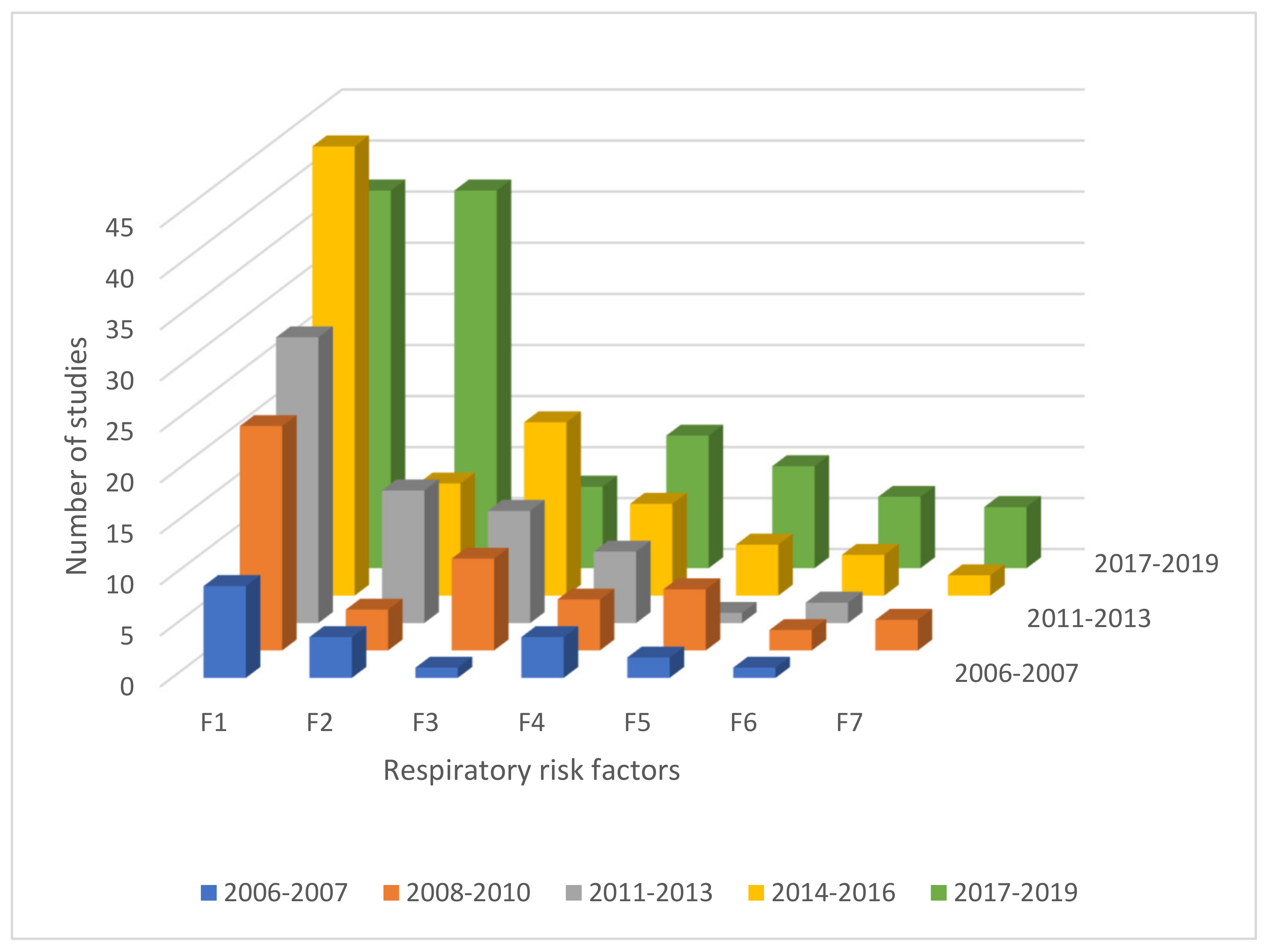
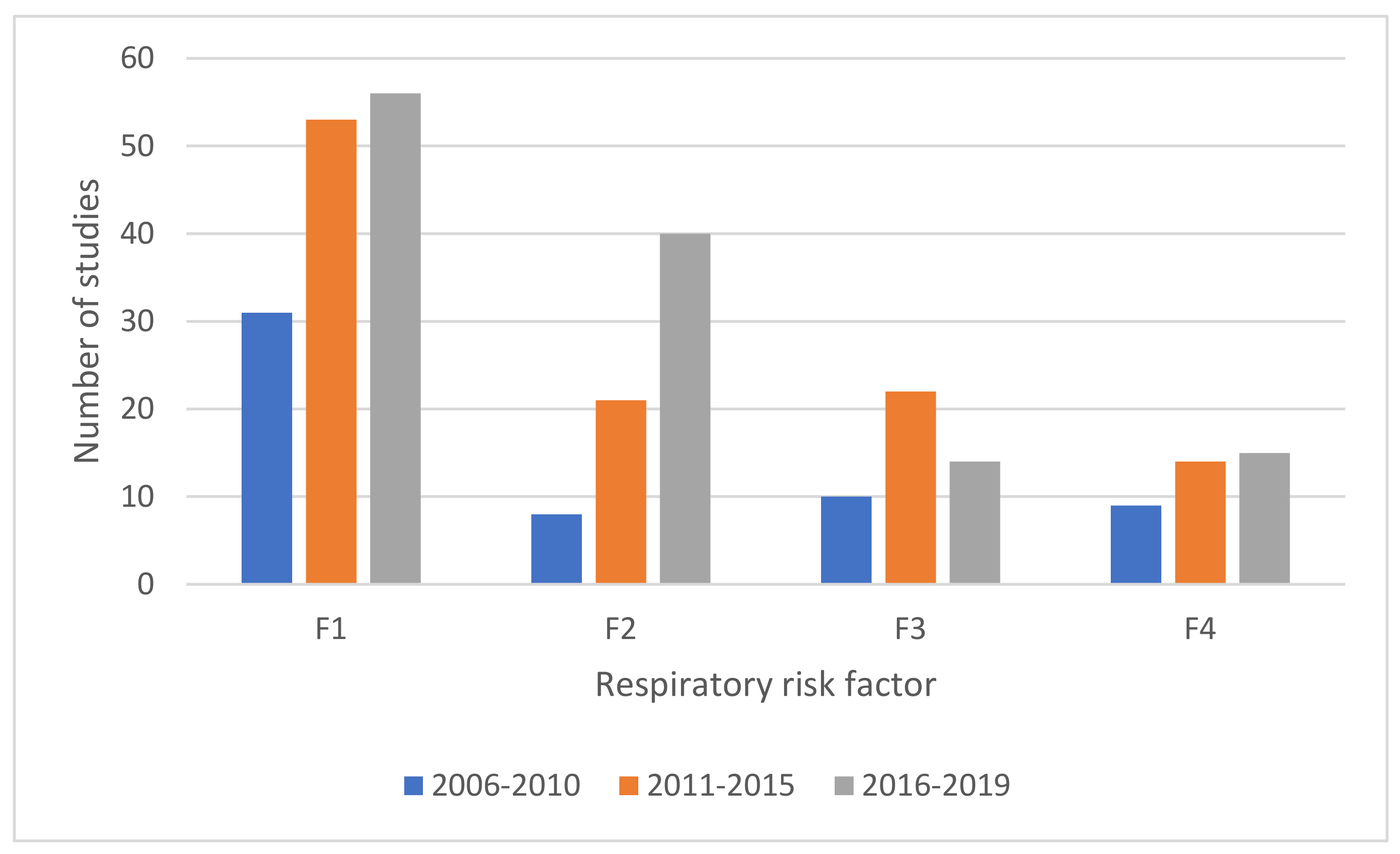
6.1. Respiratory Risk Factors Evolving over Time
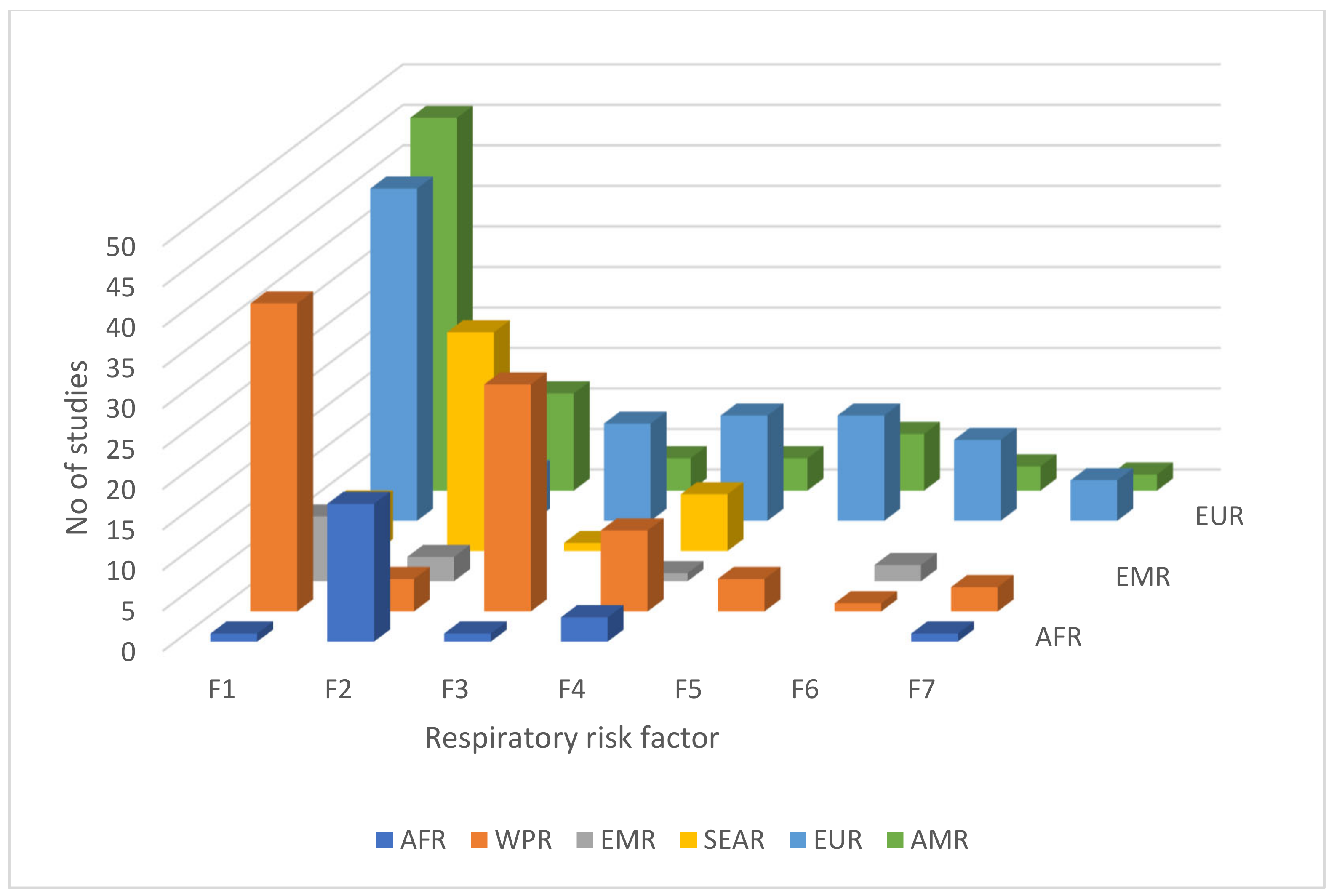
6.2. Distribution of Respiratory Risk Factors across Geographical Regions
6.3. Mitigation Measures Associated with the Risk Factors
6.4. Challenges and Existing Gaps
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| 1. Was the research question or objective in this paper clearly stated? |
| 2. Was the study population clearly specified and defined? |
| 3. Was the participation rate of eligible persons at least 50%? |
| 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? |
| 5. Was a sample size justification, power description, or variance and effect estimates provided? |
| 6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? |
| 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? |
| 8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? |
| 9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
| 10. Was the exposure(s) assessed more than once over time? |
| 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
| 12. Were the outcome assessors blinded to the exposure status of participants? |
| 13. Was loss to follow-up after baseline 20% or less? |
| 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? |
References
- Zanuzdana, A.; Khan, M.; Kraemer, A. Housing satisfaction related to health and importance of services in urban slums: Evidence from Dhaka, Bangladesh. Soc. Indic. Res. 2013, 112, 163–185. [Google Scholar] [CrossRef]
- WHO. Developing Guidance for Health Protection in the Built Environment-Mitigation and Adaptation Responses; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Rauh, V.A.; Landrigan, P.J.; Claudio, L. Housing and health. Ann. N. Y. Acad. Sci. 2008, 1136, 276–288. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.H.; Su, H.H.; Hsu, L.; Wang, C.Y.; Wu, P.H. Correlation between novel potential indoor risk factors and frequency of doctor’s visit for respiratory problem in Taiwan’s tropical environment. Int. J. Occup. Environ. Med. 2018, 9, 10–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taksande, A.M.; Yeole, M. Risk factors of Acute Respiratory Infection (ARI) in under-fives in a rural hospital of Central India. J. Pediatric Neonatal Individ. Med. 2016, 5. [Google Scholar] [CrossRef]
- Jo, E.J.; Lee, W.S.; Jo, H.Y.; Kim, C.H.; Eom, J.S.; Mok, J.H.; Kim, M.H.; Lee, K.; Kim, K.U.; Lee, M.K.; et al. Effects of particulate matter on respiratory disease and the impact of meteorological factors in Busan, Korea. Respir. Med. 2017, 124, 79–87. [Google Scholar] [CrossRef] [Green Version]
- Morley, C.; Grimwood, K.; Maloney, S.; Ware, R.S. Meteorological factors and respiratory syncytial virus seasonality in subtropical Australia. Epidemiol. Infect. 2018, 146, 757–762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krieger, J.; Higgins, D.L. Housing and health: Time again for public health action. Am. J. Public Health 2002, 92, 758–768. [Google Scholar] [CrossRef] [PubMed]
- Macintyre, S.; Ellaway, A.; Hiscock, R.; Kearns, A.; Der, G.; McKay, L. What features of the home and the area might help to explain observed relationships between housing tenure and health? Evidence from the west of Scotland. Health Place 2003, 9, 207–218. [Google Scholar] [CrossRef]
- Weich, S.; Blanchard, M.; Prince, M.; Burton, E.; Erens, B.; Sproston, K. Mental health and the built environment: Cross-sectional survey of individual and contextual risk factors for depression. Br. J. Psychiatry 2002, 180, 428–433. [Google Scholar] [CrossRef]
- United Nations. Growing at a Slower Pace, World Population is Expected to Reach 9.7 Billion in 2050 and Could Peak at Nearly 11 Billion around 2100. Available online: https://www.un.org/development/desa/en/news/population/world-population-prospects-2019.html (accessed on 15 March 2020).
- World Economic Forum. Making Affordable Housing a Reality in Cities; World Economic Forum: Geneva, Switzerland, 2019. [Google Scholar]
- Na, Z. The Aging Housing Stock. Available online: http://eyeonhousing.org/2017/01/the-aging-housing-stock-3/ (accessed on 13 February 2020).
- Nieto, M.; MacAller, R. Why restore habitat? A case study on one small corner of the world: The cultural, regulatory, and public health drivers of habitat restoration in San Diego, California, USA. In Proceedings of the Beijing International Symposium on Land Reclamation and Ecological Restoration, Beijing, China, 16–19 October 2014; pp. 651–656. [Google Scholar]
- Housing New Zealand. Housing New Zealand Annual Report 2016/17; Housing New Zealand: Wellington, New Zealand, 2017. [Google Scholar]
- BRANZ. House Repair Priorities; Building Research Association of New Zealand: Judgeford, New Zealand, 2013. [Google Scholar]
- Jackson, S.; Mathews, K.H.; Pulanić, D.; Falconer, R.; Rudan, I.; Campbell, H.; Nair, H. Risk factors for severe acute lower respiratory infections in children—A systematic review and meta-analysis. Croat. Med. J. 2013, 54, 110–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, T.; Balsells, E.; Wastnedge, E.; Singleton, R.; Rasmussen, Z.A.; Zar, H.J.; Rath, B.A.; Madhi, S.A.; Campbell, S.; Vaccari, L.C. Risk factors for respiratory syncytial virus associated with acute lower respiratory infection in children under five years: Systematic review and meta–analysis. J. Glob. Health 2015, 5. [Google Scholar] [CrossRef] [PubMed]
- Sonego, M.; Pellegrin, M.C.; Becker, G.; Lazzerini, M. Risk factors for mortality from acute lower respiratory infections (ALRI) in children under five years of age in low and middle-income countries: A systematic review and meta-analysis of observational studies. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [Green Version]
- Forum of International Respiratory Societies. The Global Impact of Respiratory Disease, 2nd ed.; European Respiratory Society: Sheffield, UK, 2017. [Google Scholar]
- Kumar, R.; Goel, N.; Gupta, N.; Singh, K.; Nagar, S.; Mittal, J. Indoor air pollution and respiratory illness in children from rural India: A pilot study. Indian J. Chest Dis. Allied Sci. 2014, 56, 79–83. [Google Scholar]
- Uman, L.S. Systematic reviews and meta-analyses. J. Can. Acad. Child Adolesc. Psychiatry 2011, 20, 57–59. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Jørgensen, M.; Shepperd, M. A systematic review of software development cost estimation studies. Ieee Trans. Softw. Eng. 2007, 33, 33–53. [Google Scholar] [CrossRef] [Green Version]
- Klewitz, J.; Hansen, E.G. Sustainability-oriented innovation of SMEs: A systematic review. J. Clean. Prod. 2014, 65, 57–75. [Google Scholar] [CrossRef]
- Lund, C.; Breen, A.; Flisher, A.J.; Kakuma, R.; Corrigall, J.; Joska, J.A.; Swartz, L.; Patel, V. Poverty and common mental disorders in low and middle income countries: A systematic review. Soc. Sci. Med. 2010, 71, 517–528. [Google Scholar] [CrossRef] [Green Version]
- Hay, L.; Duffy, A.H.B.; McTeague, C.; Pidgeon, L.M.; Vuletic, T.; Grealy, M. A systematic review of protocol studies on conceptual design cognition: Design as search and exploration. Des. Sci. 2017, 3. [Google Scholar] [CrossRef] [Green Version]
- King, C.R. The timing of salvage radiotherapy after radical prostatectomy: A systematic review. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 104–111. [Google Scholar] [CrossRef]
- Soldati, A.; Marchioli, C. Physics and modelling of turbulent particle deposition and entrainment: Review of a systematic study. Int. J. Multiph. Flow 2009, 35, 827–839. [Google Scholar] [CrossRef]
- Oates, B.J.; Capper, G. Using systematic reviews and evidence-based software engineering with masters students. In Proceedings of the 13th International Conference on Evaluation and Assessment in Software Engineering (EASE) 13, Durham, UK, 20–21 April 2009; pp. 1–9. [Google Scholar]
- Mallett, R.; Hagen-Zanker, J.; Slater, R.; Duvendack, M. The benefits and challenges of using systematic reviews in international development research. J. Dev. Eff. 2012, 4, 445–455. [Google Scholar] [CrossRef]
- Johansen, M.; Thomsen, S.F. Guidelines for reporting medical research: A critical appraisal. Int. Sch. Res. Not. 2016, 2016, 1346026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ritchie, H.; Roser, M. Causes of Death. Available online: https://ourworldindata.org/causes-of-death (accessed on 28 July 2020).
- Laryea, S.; Ibem, E.O. Patterns of Technological Innovation in the use of e-Procurement in Construction. J. Inf. Technol. Constr. 2014, 19, 104–125. [Google Scholar]
- Babalola, O.; Ibem, E.O.; Ezema, I.C. Implementation of lean practices in the construction industry: A systematic review. Build. Environ. 2019, 148, 34–43. [Google Scholar] [CrossRef]
- National Heart Lung and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 25 May 2019).
- Tan, S.S.-L.; Goonawardene, N. Internet health information seeking and the patient-physician relationship: A systematic review. J. Med. Internet Res. 2017, 19. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Status Report on Noncommunicable Diseases 2014; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Morgenstern, V.; Zutavern, A.; Cyrys, J.; Brockow, I.; Gehring, U.; Koletzko, S.; Bauer, C.P.; Reinhardt, D.; Wichmann, H.E.; Heinrich, J. Respiratory health and individual estimated exposure to traffic-related air pollutants in a cohort of young children. Occup. Environ. Med. 2007, 64, 8–16. [Google Scholar] [CrossRef] [Green Version]
- Ji, W.; Zhao, B. Estimating mortality derived from indoor exposure to particles of outdoor origin. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, L.F.; Saldiva, S.R.; Saldiva, P.H.; Dolhnikoff, M. Impaired lung function in individuals chronically exposed to biomass combustion. Environ. Res. 2012, 112, 111–117. [Google Scholar] [CrossRef]
- Murray, E.L.; Brondi, L.; Kleinbaum, D.; McGowan, J.E.; Van Mels, C.; Brooks, W.A.; Goswami, D.; Ryan, P.B.; Klein, M.; Bridges, C.B. Cooking fuel type, household ventilation, and the risk of acute lower respiratory illness in urban Bangladeshi children: A longitudinal study. Indoor Air 2012, 22, 132–139. [Google Scholar] [CrossRef]
- Ranathunga, N.; Perera, P.; Nandasena, S.; Sathiakumar, N.; Kasturiratne, A.; Wickremasinghe, R. Effect of household air pollution due to solid fuel combustion on childhood respiratory diseases in a semi urban population in Sri Lanka. BMC Pediatrics 2019, 19. [Google Scholar] [CrossRef] [Green Version]
- Han, J.; Liu, S.; Zhang, J.; Zhou, L.; Fang, Q.; Zhang, J.; Zhang, Y. The impact of temperature extremes on mortality: A time-series study in Jinan, China. BMJ Open 2017, 7. [Google Scholar] [CrossRef]
- Fernandez-Raga, M.; Tomas, C.; Fraile, R. Human mortality seasonality in Castile-Leon, Spain, between 1980 and 1998: The influence of temperature, pressure and humidity. Int. J. Biometeorol. 2010, 54, 379–392. [Google Scholar] [CrossRef] [PubMed]
- Son, J.Y.; Bell, M.L.; Lee, J.T. The impact of heat, cold, and heat waves on hospital admissions in eight cities in Korea. Int. J. Biometeorol. 2014, 58, 1893–1903. [Google Scholar] [CrossRef] [PubMed]
- Walker, N.; Johnston, V.; Glover, M.; Bullen, C.; Trenholme, A.; Chang, A.; Morris, P.; Segan, C.; Brown, N.; Fenton, D.; et al. Effect of a family-centered, secondhand smoke intervention to reduce respiratory illness in indigenous infants in Australia and New Zealand: A randomized controlled trial. Nicotine Tob. Res. 2015, 17, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Håberg, S.E.; Stigum, H.; Nystad, W.; Nafstad, P. Effects of pre- and postnatal exposure to parental smoking on early childhood respiratory health. Am. J. Epidemiol. 2007, 166, 679–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.-H.; Cho, S.J.; White, S.K.; Cox-Ganser, J.M. Changes in respiratory and non-respiratory symptoms in occupants of a large office building over a period of moisture damage remediation attempts. PLoS ONE 2018, 13, e0191165. [Google Scholar] [CrossRef] [Green Version]
- Karvonen, A.M.; Hyvärinen, A.; Korppi, M.; Haverinen-Shaughnessy, U.; Renz, H.; Pfefferle, P.I.; Remes, S.; Genuneit, J.; Pekkanen, J. Moisture damage and asthma: A birth cohort study. Pediatrics 2015, 135, e598–e606. [Google Scholar] [CrossRef] [Green Version]
- Bräuner, E.V.; Andersen, C.E.; Sørensen, M.; Andersen, Z.J.; Gravesen, P.; Ulbak, K.; Hertel, O.; Pedersen, C.; Overvad, K.; Tjønneland, A. Residential radon and lung cancer incidence in a Danish cohort. Environ. Res. 2012, 118, 130–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dempsey, S.; Lyons, S.; Nolan, A. High radon areas and lung cancer prevalence: Evidence from Ireland. J. Environ. Radioact. 2018, 182, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Reid, A.; Heyworth, J.; De Klerk, N.; Musk, A. The mortality of women exposed environmentally and domestically to blue asbestos at Wittenoom, Western Australia. Occup. Environ. Med. 2008, 65, 743–749. [Google Scholar] [CrossRef]
- Visonà, S.D.; Villani, S.; Manzoni, F.; Chen, Y.; Ardissino, G.; Russo, F.; Moretti, M.; Javan, G.T.; Osculati, A. Impact of asbestos on public health: A retrospective study on a series of subjects with occupational and non-occupational exposure to asbestos during the activity of Fibronit plant (Broni, Italy). J. Public Health Res. 2018, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dales, R.; Ruest, K.; Guay, M.; Marro, L.; David Miller, J. Residential fungal growth and incidence of acute respiratory illness during the first two years of life. Environ. Res. 2010, 110, 692–698. [Google Scholar] [CrossRef]
- Shendell, D.G.; Mizan, S.S.; Yamamoto, N.; Peccia, J. Associations between quantitative measures of fungi in home floor dust and lung function among older adults with chronic respiratory disease: A pilot study. J. Asthma 2012, 49, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, S.S.C.; Solé, D.; Camargos, P.; De Andrade, C.R.; Ibiapina, C.C. Factors associated with asthma expression in adolescents. J. Bras. De Pneumol. 2018, 44, 12–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dong, G.H.; Qian, Z.; Wang, J.; Trevathan, E.; Ma, W.; Chen, W.; Xaverius, P.K.; Buckner-Petty, S.; Ray, A.; Liu, M.M.; et al. Residential characteristics and household risk factors and respiratory diseases in Chinese women: The Seven Northeast Cities (SNEC) Study. Sci. Total Environ. 2013, 463–464, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.C.; Wilson, A.; Mickley, L.J.; Ebisu, K.; Sulprizio, M.P.; Wang, Y.; Peng, R.D.; Yue, X.; Dominici, F.; Bell, M.L. Who among the Elderly Is Most Vulnerable to Exposure to and Health Risks of Fine Particulate Matter from Wildfire Smoke? Am. J. Epidemiol. 2017, 186, 730–735. [Google Scholar] [CrossRef]
- Shaposhnikov, D.; Revich, B.; Bellander, T.; Bedada, G.B.; Bottai, M.; Kharkova, T.; Kvasha, E.; Lezina, E.; Lind, T.; Semutnikova, E.; et al. Mortality related to air pollution with the Moscow heat wave and wildfire of 2010. Epidemiology 2014, 25, 359–364. [Google Scholar] [CrossRef] [Green Version]
- Cipolla, M.; Bruzzone, M.; Stagnaro, E.; Ceppi, M.; Izzotti, A.; Culotta, C.; Piccardo, M.T. Health Issues of Primary School Students Residing in Proximity of an Oil Terminal with Environmental Exposure to Volatile Organic Compounds. Biomed Res. Int. 2016, 2016, 4574138. [Google Scholar] [CrossRef] [Green Version]
- Jiang, W.; Lu, C.; Miao, Y.; Xiang, Y.; Chen, L.; Deng, Q. Outdoor particulate air pollution and indoor renovation associated with childhood pneumonia in China. Atmos. Environ. 2018, 174, 76–81. [Google Scholar] [CrossRef]
- Murray, E.L.; Klein, M.; Brondi, L.; McGowan, J.E.; Van Mels, C.; Brooks, W.A.; Kleinbaum, D.; Goswami, D.; Ryan, P.B.; Bridges, C.B. Rainfall, household crowding, and acute respiratory infections in the tropics. Epidemiol. Infect. 2012, 140, 78–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trianti, S.M.; Samoli, E.; Rodopoulou, S.; Katsouyanni, K.; Papiris, S.A.; Karakatsani, A. Desert dust outbreaks and respiratory morbidity in Athens, Greece. Environ. Health 2017, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thalib, L.; Al-Taiar, A. Dust storms and the risk of asthma admissions to hospitals in Kuwait. Sci. Total Environ. 2012, 433, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Linares, C.; Díaz, J.; Tobías, A.; de Miguel, J.M.; Otero, A. Impact of urban air pollutants and noise levels over daily hospital admissions in children in Madrid: A time series analysis. Int. Arch. Occup. Environ. Health 2006, 79, 143–152. [Google Scholar] [CrossRef]
- Li, L.; Hart, J.E.; Coull, B.A.; Cao, S.J.; Spengler, J.D.; Adamkiewicz, G. Effect of residential greenness and nearby parks on respiratory and allergic diseases among middle school adolescents in a Chinese city. Int. J. Environ. Res. Public Health 2019, 16, 991. [Google Scholar] [CrossRef] [Green Version]
- Liu, W.; Huang, C.; Hu, Y.; Zou, Z.; Zhao, Z.; Sundell, J. Association of building characteristics, residential heating and ventilation with asthmatic symptoms of preschool children in Shanghai: A cross-sectional study. Indoor Built Environ. 2014, 23, 270–283. [Google Scholar] [CrossRef]
- Nguyen, T.; Lurie, M.; Gomez, M.; Reddy, A.; Pandya, K.; Medvesky, M. The National Asthma Survey—New York State: Association of the home environment with current asthma status. Public Health Rep. 2010, 125, 877–887. [Google Scholar] [CrossRef]
- Medina, R.M.; Zock, J.P.; Kogevinas, M.; Sunyer, J.; Basagaña, X.; Schwartz, J.; Burge, P.S.; Moore, V.; Antó, J.M. Short-term respiratory effects of cleaning exposures in female domestic cleaners. Eur. Respir. J. 2006, 27, 1196–1203. [Google Scholar] [CrossRef] [Green Version]
- Mengersen, K.; Morawska, L.; Wang, H.; Murphy, N.; Tayphasavanh, F.; Darasavong, K.; Holmes, N. The effect of housing characteristics and occupant activities on the respiratory health of women and children in Lao PDR. Sci. Total Environ. 2011, 409, 1378–1384. [Google Scholar] [CrossRef] [Green Version]
- Turunen, M.; Iso-Markku, K.; Pekkonen, M.; Haverinen, S.U. Statistical associations between housing quality and health among Finnish households with children-Results from two (repeated) national surveys. Sci. Total Environ. 2017, 574, 1580–1587. [Google Scholar] [CrossRef]
- Herrera, R.; Berger, U.; Von Ehrenstein, O.S.; Díaz, I.; Huber, S.; Muñoz, D.M.; Radon, K. Estimating the causal impact of proximity to gold and copper mines on respiratory diseases in Chilean children: An application of targeted maximum likelihood estimation. Int. J. Environ. Res. Public Health 2018, 15, 39. [Google Scholar] [CrossRef] [Green Version]
- Pun, V.C.; Tian, L.; Ho, K.F. Particulate matter from re-suspended mineral dust and emergency cause-specific respiratory hospitalizations in Hong Kong. Atmos. Environ. 2017, 165, 191–197. [Google Scholar] [CrossRef] [Green Version]
- Eom, S.Y.; Cho, E.B.; Oh, M.K.; Kweon, S.S.; Nam, H.S.; Kim, Y.D.; Kim, H. Increased incidence of respiratory tract cancers in people living near Portland cement plants in Korea. Int. Arch. Occup. Environ. Health 2017, 90, 859–864. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, K.; Koriyama, C.; Akiba, S. Increased mortality of respiratory diseases, including lung cancer, in the area with large amount of ashfall from mount Sakurajima volcano. J. Environ. Public Health 2012. [Google Scholar] [CrossRef] [PubMed]
- Rappold, A.G.; Reyes, J.; Pouliot, G.; Cascio, W.E.; Diaz-Sanchez, D. Community Vulnerability to Health Impacts of Wildland Fire Smoke Exposure. Environ. Sci. Technol. 2017, 51, 6674–6682. [Google Scholar] [CrossRef] [PubMed]
- Özkaynak, H.; Xue, J.; Spengler, J.; Wallace, L.; Pellizzari, E.; Jenkins, P. Personal exposure to airborne particles and metals: Results from the particle team study in Riverside, California. J. Expo. Anal. Environ. Epidemiol. 1996, 6, 57–78. [Google Scholar]
- Tong, Z.; Chen, Y.; Malkawi, A.; Adamkiewicz, G.; Spengler, J.D. Quantifying the impact of traffic-related air pollution on the indoor air quality of a naturally ventilated building. Environ. Int. 2016, 89–90, 138–146. [Google Scholar] [CrossRef]
- Ma, W.; Xu, X.; Peng, L.; Kan, H. Impact of extreme temperature on hospital admission in Shanghai, China. Sci. Total Environ. 2011, 409, 3634–3637. [Google Scholar] [CrossRef]
- Zhao, Q.; Zhao, Y.; Li, S.; Zhang, Y.; Wang, Q.; Zhang, H.; Qiao, H.; Li, W.; Huxley, R.; Williams, G.; et al. Impact of ambient temperature on clinical visits for cardio-respiratory diseases in rural villages in northwest China. Sci. Total Environ. 2018, 612, 379–385. [Google Scholar] [CrossRef]
- Sidhu, M.K.; Ravindra, K.; Mor, S.; John, S. Household air pollution from various types of rural kitchens and its exposure assessment. Sci. Total Environ. 2017, 586, 419–429. [Google Scholar] [CrossRef]
- Kukla, L.; Hrubá, D.; Tyrlík, M. Trends in respiratory morbidity of children in relation to their passive smoking exposure. Cent. Eur. J. Public Health 2006, 14, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Leung, L.T.; Ho, S.Y.; Wang, M.P.; Lo, W.S.; Lam, T.H. Exposure to secondhand smoke from neighbours and respiratory symptoms in never-smoking adolescents in Hong Kong: A cross-sectional study. BMJ Open 2015, 5, e008607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Öberg, M.; Jaakkola, M.S.; Woodward, A.; Peruga, A.; Prüss-Ustün, A. Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. Lancet 2011, 377, 139–146. [Google Scholar] [CrossRef]
- Mitchell, E.A.; Beasley, R.; Keil, U.; Montefort, S.; Odhiambo, J. The association between tobacco and the risk of asthma, rhinoconjunctivitis and eczema in children and adolescents: Analyses from phase three of the ISAAC programme. Thorax 2012, 67, 941–949. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vanker, A.; Gie, R.P.; Zar, H.J. The association between environmental tobacco smoke exposure and childhood respiratory disease: A review. Expert Rev. Respir. Med. 2017, 11, 661–673. [Google Scholar] [CrossRef] [PubMed]
- Catelinois, O.; Rogel, A.; Laurier, D.; Billon, S.; Hemon, D.; Verger, P.; Tirmarche, M. Lung cancer attributable to indoor radon exposure in France: Impact of the risk models and uncertainty analysis. Environ. Health Perspect. 2006, 114, 1361–1366. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo-González, M.; Ruano-Ravina, A.; Torres-Durán, M.; Kelsey, K.T.; Provencio, M.; Parente-Lamelas, I.; Leiro-Fernández, V.; Vidal-García, I.; Castro-Añón, O.; Martínez, C. Lung cancer and residential radon in never-smokers: A pooling study in the Northwest of Spain. Environ. Res. 2019, 172, 713–718. [Google Scholar] [CrossRef] [PubMed]
- Ferrante, D.; Mirabelli, D.; Tunesi, S.; Terracini, B.; Magnani, C. Pleural mesothelioma and occupational and non-occupational asbestos exposure: A case-control study with quantitative risk assessment. Occup. Environ. Med. 2016, 73, 147–153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pyana Kitenge, J.; Kapinga Kayembe, D.; Tshibangu Muamba, M.; Kachil Rubing, H.; De Vos, B.; Van Bouwel, J.; Nemery, B. Malignant mesothelioma in Sub-Saharan Africa: A case report from Lubumbashi, DR Congo. Environ. Res. 2019, 176. [Google Scholar] [CrossRef]
- Jakkola, J.J.K.; Parise, H.; Kislitsin, V.; Lebedeva, N.I.; Spengler, J.D. Asthma, Wheezing, and Allergies in Russian Schoolchildren in Relation to New Surface Materials in the Home. Am. J. Public Health 2004, 94, 560–562. [Google Scholar] [CrossRef]
- Li, A.; Sun, Y.; Liu, Z.; Xu, X.; Sun, H.; Sundell, J. The influence of home environmental factors and life style on children’s respiratory health in Xi’an. Chin. Sci. Bull. 2014, 59, 2024–2030. [Google Scholar] [CrossRef]
- Canova, C.; Jarvis, D.; Walker, S.; Cullinan, P. Systematic review of the effects of domestic paints on asthma related symptoms in people with or without asthma. J. Asthma 2013, 50, 1020–1030. [Google Scholar] [CrossRef]
- Piazza, T.; Lee, R.H.; Hayes, J. Survey of the Use of Ozone-Generating Air Cleaners by the California Public; University of California: Berkeley, CA, USA, 2006. [Google Scholar]
- Scheepers, P.T.J.; De Hartog, J.J.; Reijnaerts, J.; Beckmann, G.; Anzion, R.; Poels, K.; Godderis, L. Influence of combined dust reducing carpet and compact air filtration unit on the indoor air quality of a classroom. Environ. Sci. Process. Impacts 2015, 17, 316–325. [Google Scholar] [CrossRef] [PubMed]
- Environment Protection Agency. Controlling Pollutants and Sources: Indoor Air Quality Design Tools for Schools. Available online: https://www.epa.gov/iaq-schools/controlling-pollutants-and-sources-indoor-air-quality-design-tools-schools#Carpet (accessed on 21 April 2020).
- Behrens, T.; Maziak, W.; Weiland, S.; Rzehak, P.; Siebert, E.; Keil, U. Symptoms of asthma and the home environment. The ISAAC I and III cross-sectional surveys in Münster, Germany. Int. Arch. Allergy Immunol. 2005, 137, 53–61. [Google Scholar] [CrossRef]
- Matus, M.S.; Sánchez, T.; Martínez-Gutiérrez, J.; Cerda, J.; Helia Molina, M.; Valenzuela, P.M. Indoor environmental risk factors for pediatric respiratory diseases in an underserved community in Santiago, Chile. Int. J. Child Health Hum. Dev. 2014, 7, 249. [Google Scholar]
- Potts, J.F.; Rona, R.J.; Oyarzun, M.J.; Amigo, H.; Bustos, P. Indoor risk factors for cough and their relation to wheeze and sensitization in Chilean young adults. Am. J. Public Health 2008, 98, 680–686. [Google Scholar] [CrossRef]
- Becher, R.; Høie, A.H.; Bakke, J.V.; Holøs, S.B.; Øvrevik, J. Dampness and moisture problems in Norwegian homes. Int. J. Environ. Res. Public Health 2017, 14, 1241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sweileh, W.M.; Al-Jabi, S.W.; Sa’Ed, H.Z.; Sawalha, A.F. Outdoor air pollution and respiratory health: A bibliometric analysis of publications in peer-reviewed journals (1900–2017). Multidiscip. Respir. Med. 2018, 13, 15. [Google Scholar] [CrossRef] [Green Version]
- WHO. World Health Statistics 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Results; Institute for Health Metrics and Evaluation: Seattle, WA, USA, 2017. [Google Scholar]
- Lelieveld, J.; Evans, J.S.; Fnais, M.; Giannadaki, D.; Pozzer, A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 2015, 525, 367–371. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Household Air Pollution and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health (accessed on 15 August 2020).
- Bonjour, S.; Adair-Rohani, H.; Wolf, J.; Bruce, N.G.; Mehta, S.; Prüss-Ustün, A.; Lahiff, M.; Rehfuess, E.A.; Mishra, V.; Smith, K.R. Solid fuel use for household cooking: Country and regional estimates for 1980–2010. Environ. Health Perspect. 2013, 121, 784–790. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. WHO Guidelines for Indoor Air Quality: Household Fuel Combustion; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- WHO. Worldwide Burden of Disease from Exposure to Second-Hand Smoke; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Oluwole, O.; Ana, G.R.; Arinola, G.O.; Wiskel, T.; Falusi, A.G.; Huo, D.; Olopade, O.I.; Olopade, C.O. Effect of stove intervention on household air pollution and the respiratory health of women and children in rural Nigeria. Air Qual. Atmos. Health 2013, 6, 553–561. [Google Scholar] [CrossRef]
- Khan, M.N.; Nurs, C.Z.B.; Mofizul Islam, M.; Islam, M.R.; Rahman, M.M.; Nurs, C.Z.B. Household air pollution from cooking and risk of adverse health and birth outcomes in Bangladesh: A nationwide population-based study. Environ. Health 2017, 16, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World health Organization. WHO Releases Country Estimates on Air Pollution Exposure and Health Impact. Available online: https://www.who.int/news/item/27-09-2016-who-releases-country-estimates-on-air-pollution-exposure-and-health-impact (accessed on 8 February 2021).
- Global Carbon Atlas. Global Carbon Project. Available online: http://www.globalcarbonatlas.org/en/CO2-emissions (accessed on 15 June 2020).
- Ban, J.; Xu, D.; He, M.Z.; Sun, Q.; Chen, C.; Wang, W.; Zhu, P.; Li, T. The effect of high temperature on cause-specific mortality: A multi-county analysis in China. Environ. Int. 2017, 106, 19–26. [Google Scholar] [CrossRef] [Green Version]
- Zhang, D.S.; He, J.; Gao, S.H.; Hu, B.K.; Ma, S.L. Correlation analysis for the attack of respiratory diseases and meteorological factors. Chin. J. Integr. Med. 2011, 17, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Liu, J.; Chen, F.; Shamsi, B.H.; Wang, Q.; Jiao, F.; Qiao, Y.; Shi, Y. Impact of meteorological factors on lower respiratory tract infections in children. J. Int. Med Res. 2016, 44, 30–41. [Google Scholar] [CrossRef] [Green Version]
- Zielinski, J.M. Mapping of Residential Radon in the World; University of Ottawa: Ottawa, ON, Canada, 2014. [Google Scholar]
- Delgermaa, V.; Takahashi, K.; Park, E.-K.; Le, G.V.; Hara, T.; Sorahan, T. Global mesothelioma deaths reported to the World Health Organization between 1994 and 2008. Bull. World Health Organ. 2011, 89, 716–724. [Google Scholar] [CrossRef] [PubMed]
- International TEFL Academy. The Top 9 Public Transportation Systems Around the World. Available online: https://www.internationalteflacademy.com/blog/the-top-10-public-transportation-systems-around-the-world (accessed on 16 February 2021).
- Milner, J.; Shrubsole, C.; Das, P.; Jones, B.; Ridley, I.; Chalabi, Z.; Hamilton, I.; Armstrong, B.; Davies Prof, M.; Wilkinson, P. Home energy efficiency and radon related risk of lung cancer: Modelling study. BMJ (Online) 2014, 348, f7493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crawley, J.; Wingfield, J.; Elwell, C. The relationship between airtightness and ventilation in new UK dwellings. Build. Serv. Eng. Res. Technol. 2019, 40, 274–289. [Google Scholar] [CrossRef] [Green Version]
- Atkinson, J.; Chartier, Y.; Pessoa-Silva, C.L.; Jensen, P.; Li, A.; Seto, W.-H. Natural Ventilation for Infection Control in Health-Care Settings; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- Heiselberg, P.; Bjørn, E.; Nielsen, P.V. Impact of open windows on room air flow and thermal comfort. Int. J. Vent. 2002, 1, 91–100. [Google Scholar] [CrossRef]
- Heiselberg, P.K. Principles of Hybrid Ventilation. In International Energy Agency Annex 35 Final Report; Department of Building Technology and Structural Engineering, Aalborg University: Aalborg, Denmark, 2002. [Google Scholar]
- Torres-Duque, C.; Maldonado, D.; Pérez-Padilla, R.; Ezzati, M.; Viegi, G. Biomass fuels and respiratory diseases: A review of the evidence. Proc. Am. Thorac. Soc. 2008, 5, 577–590. [Google Scholar] [CrossRef]
- Sk, R.; Rasooly, M.H.; Barua, S. Do fuel type and place of cooking matter for acute respiratory infection among Afghan children? Evidence from the Afghanistan DHS 2015. J. Biosoc. Sci. 2019, 140–153. [Google Scholar] [CrossRef] [PubMed]
- Behrooz, L.; Balekian, D.S.; Faridi, M.K.; Espinola, J.A.; Townley, L.P.; Camargo, C.A., Jr. Prenatal and postnatal tobacco smoke exposure and risk of severe bronchiolitis during infancy. Respir. Med. 2018, 140, 21–26. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Report on the Global Tobacco Epidemic 2017: Monitoring Tobacco Use and Prevention Policies; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- WHO. WHO Report on the Global Tobacco Epidemic, 2009: Implementing Smoke-Free Environments; WHO: Geneva, Switzerland, 2009. [Google Scholar]

| Source | Number of Articles from Source | % | % of Article Type in Selected Literature |
|---|---|---|---|
| Journals | |||
| Science of the Total Environment | 18 | 5.0 | 99 |
| Environmental Research | 18 | 5.0 | |
| International Journal of Environmental Research and Public Health | 15 | 4.2 | |
| Environment Health Perspectives | 15 | 4.2 | |
| Environmental International | 13 | 3.6 | |
| Environmental Health: A Global Access Science Source | 11 | 3.1 | |
| Environmental Pollution | 10 | 2.8 | |
| American Journal of Respiratory and Critical Care Medicine | 9 | 2.5 | |
| PLoS ONE | 9 | 2.5 | |
| Others | 240 | 67.0 | |
| Total number of journals | 358 | ||
| Conference papers | |||
| Conference papers | 2 | 100.0 | 1 |
| Respiratory Risk Factor | Mitigation Solutions Suggested in the Literature | Number of Studies in the Review |
|---|---|---|
| Living close to city areas, main roads, highways or industrial areas | Improvement in public transport to reduce road traffic | 6 |
| Provide ventilation with pollutant-free air using filtration | 5 | |
| Vehicle fleet improvement | 5 | |
| Fossil fuel substitution | 2 | |
| Close the windows facing roadways | 1 | |
| Installation of air purifiers in indoor environments | 1 | |
| Exposure to solid fuel | Use of cleaner fuel (LPG and electricity) | 30 |
| Use of cleaner stoves with adequate ventilation | 20 | |
| Community education on the health effects of smoke from cooking | 6 | |
| Have a separate kitchen (indoor or outdoor) | 4 | |
| More ventilation in cooking areas | 3 | |
| Keep children away during cooking | 3 | |
| Meteorological factors | Improvement of household thermal performance through heating and insulation | 3 |
| Use air-conditioning during heat waves | 3 | |
| Employ an early warning system to inform extreme temperature events | 3 | |
| Exposure to ETS | Reduce postnatal tobacco smoke exposure by preventing parents from returning to smoking (cessation counselling) | 5 |
| Promote a tobacco-free environment in both households and communities | 4 | |
| Increase tobacco taxes and ban tobacco advertising, promotion and sponsorship | 4 | |
| Educate families to reduce infant tobacco smoke exposure | 3 | |
| Moisture or mould damage | Improve indoor ventilation | 6 |
| Effectively repair water leaks | 1 | |
| Remove visible mould and dampness | 1 | |
| Exposure to radon | Installation of radon proof membrane across the complete footprint of the new housing constructions | 2 |
| Use of gas permeable layer, mechanical barrier or gravel foundation to avoid soil gas entry | 2 | |
| Installation of an air distribution system to prevent soil air supply | 2 | |
| Adequate ventilation and heat recovery system in airtight houses | 2 | |
| Installation of radon sumps or positive pressure system | 2 | |
| Enhance public awareness on radon exposure risk and methods to reduce radon exposure at homes | 5 | |
| Compulsory radon level monitoring and provide incentives or subsidies for remediation works in existing buildings | 2 | |
| Exposure to indoor asbestos fiber | Installation of dust collectors in an asbestos manufacturing plant to prevent the emission of plant dust to the outdoor environment | 1 |
| Remove asbestos-containing material by trained professional | 1 | |
| Restrict or ban asbestos-related products | 1 | |
| Carpet floors and HDM | Proper maintenance of carpet floors (regular vacuum cleaning) | 1 |
| Presence of pets | Reduce the level of endotoxin and dog and cat allergens in homes | 2 |
| Exposure to wildland fires | Keep windows closed | 2 |
| Use air cleaners to improve indoor air quality | 2 | |
| Employ an early warning system and advise people to stay indoors during wildfires | 1 | |
| Exposure to VOCs | Adequate ventilation during periods of home renovations | 1 |
| Avoid indoor renovation exposure for expectant mothers and infants | 1 | |
| Exposure to dust storms | Doors should have proper sealing quality, and houses should be closed during dust storm events | 4 |
| Take measures to reduce wind erosion in desserts | 1 | |
| Establish an early warning system for dust storms | 1 | |
| Pollen | Identify pollen allergen seasons | 1 |
| Replace non-allergic cultivated plant species | 1 | |
| Use of ozone emitting air cleaners | Have adequate ventilation in rooms with air purifiers | 1 |
| Avoid the use of O3 producing air purifiers | 1 | |
| Daily cleaning activities (ammonia or chlorine-based cleaners) | Produce healthier cleaning products for households | 1 |
| Avoid unnecessary use of cleaning products | 1 | |
| Have stricter regulations to reduce chemical exposure. Inform the public by labelling the risks associated with chemicals in consumer products | 1 |
| Rank | Mitigation Solution | No of Articles | Associated Risk Factor |
|---|---|---|---|
| 1 | Use of cleaner fuel (LPG and electricity) | 30 | Exposure to solid fuel |
| 2 | Use of cleaner stoves with adequate ventilation | 20 | Exposure to solid fuel |
| 3 | Improvement in public transport to reduce road traffic | 6 | Living close to city areas, main roads, highways or industrial areas |
| 4 | Improve indoor ventilation | 6 | Moisture or mould damage |
| 5 | Community education on the health effects of smoke from cooking | 6 | Exposure to solid fuel |
| 6 | Provide ventilation with pollutant-free air using filtration | 5 | Living close to city areas, main roads, highways or industrial areas |
| 7 | Vehicle fleet improvement | 5 | Living close to city areas, main roads, highways or industrial areas |
| 8 | Reduce postnatal tobacco smoke exposure by preventing parents from returning to smoking (cessation counselling) | 5 | Exposure to ETS |
| 9 | Enhance public awareness on radon exposure risk and methods to reduce radon exposure at homes | 5 | Exposure to radon |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wimalasena, N.N.; Chang-Richards, A.; Wang, K.I.-K.; Dirks, K.N. Housing Risk Factors Associated with Respiratory Disease: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 2815. https://doi.org/10.3390/ijerph18062815
Wimalasena NN, Chang-Richards A, Wang KI-K, Dirks KN. Housing Risk Factors Associated with Respiratory Disease: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(6):2815. https://doi.org/10.3390/ijerph18062815
Chicago/Turabian StyleWimalasena, Nipuni Nilakshini, Alice Chang-Richards, Kevin I-Kai Wang, and Kim N. Dirks. 2021. "Housing Risk Factors Associated with Respiratory Disease: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 6: 2815. https://doi.org/10.3390/ijerph18062815
APA StyleWimalasena, N. N., Chang-Richards, A., Wang, K. I.-K., & Dirks, K. N. (2021). Housing Risk Factors Associated with Respiratory Disease: A Systematic Review. International Journal of Environmental Research and Public Health, 18(6), 2815. https://doi.org/10.3390/ijerph18062815









