Process of Work Disability: From Determinants of Sickness Absence Trajectories to Disability Retirement in a Long-Term Follow-Up of Municipal Employees
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Sickness Absence (SA)
2.3. Disability Pension Retirement and Mortality
2.4. Age and Socioeconomic Status
2.5. Lifestyle Factors
2.6. Morbidity
2.7. Working Conditions
2.8. Statistical Analyses
3. Results
3.1. Sickness Absence (SA) Trajectories
3.2. Determinants of SA Trajectories
3.2.1. Lifestyle-Related factors
3.2.2. Health problems
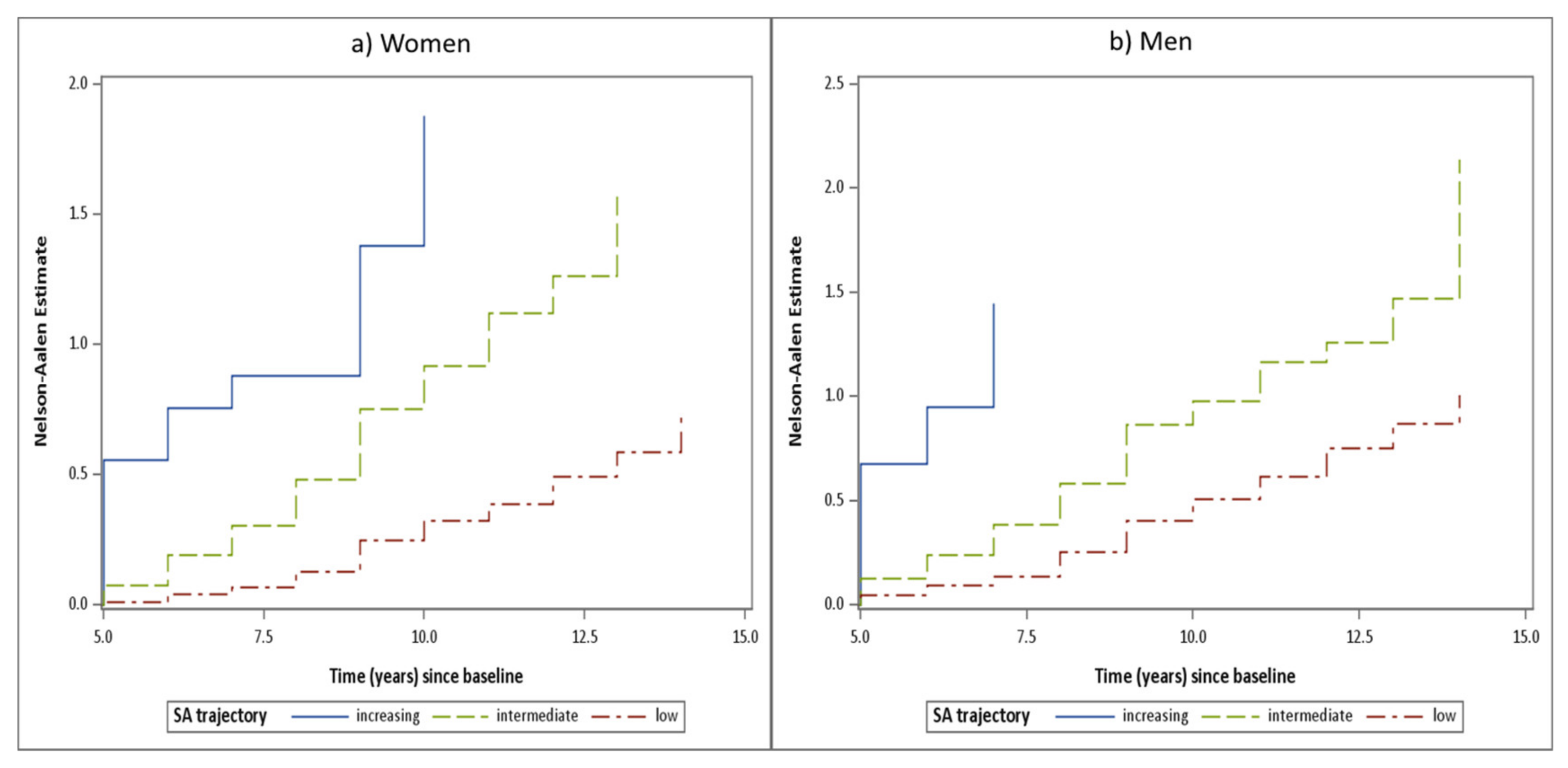
3.3. Sickness Absence Trajectories as Determinants of Disability Pension Retirement
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hultin, H.; Lindholm, C.; Malfert, M.; Moller, J. Short-term sick leave and future risk of sickness absence and unemployment—the impact of health status. BMC Public Health 2012, 12, 861. [Google Scholar] [CrossRef]
- Lund, T.; Kivimaki, M.; Labriola, M.; Villadsen, E.; Christensen, K.B. Using administrative sickness absence data as a marker of future disability pension: The prospective DREAM study of Danish private sector employees. Occup. Environ. Med. 2008, 65, 28–31. [Google Scholar] [CrossRef]
- Wallman, T.; Wedel, H.; Palmer, E.; Rosengren, A.; Johansson, S.; Eriksson, H.; Svärdsudd, K. Sick-leave track record and other potential predictors of a disability pension. A population based study of 8218 men and women followed for 16 years. BMC Public Health 2009, 9, 104. [Google Scholar]
- Pedersen, J.; Bjorner, J.B.; Burr, H.; Christensen, K.B. Transitions between sickness absence, work, unemployment, and disability in Denmark 2004–2008. Scand. J. Work Environ. Health 2012, 38, 516–526. [Google Scholar] [CrossRef]
- OECD. Sickness, Disability and Work: Breaking the Barriers; OECD Publishing: Paris, France, 2010. [Google Scholar]
- Leijten, F.R.; de Wind, A.; van den Heuvel, S.G.; Ybema, J.F.; van der Beek, A.J.; Robroek, S.J.; Burdorf, A. The influence of chronic health problems and work-related factors on loss of paid employment among older workers. J. Epidemiol. Community Health 2015, 69, 1058–1065. [Google Scholar] [CrossRef]
- Van Rijn, R.M.; Robroek, S.J.; Brouwer, S.; Burdorf, A. Influence of poor health on exit from paid employment: A systematic review. Occup. Environ. Med. 2014, 71, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Labriola, M.; Feveile, H.; Christensen, K.B.; Stroyer, J.; Lund, T. The impact of ergonomic work environment exposures on the risk of disability pension: Prospective results from DWECS/DREAM. Ergonomics 2009, 52, 1419–1422. [Google Scholar] [CrossRef] [PubMed]
- Lahelma, E.; Laaksonen, M.; Lallukka, T.; Martikainen, P.; Pietilainen, O.; Saastamoinen, P.; Gould, R.; Rahkonen, O. Working conditions as risk factors for disability retirement: A longitudinal register linkage study. BMC Public Health 2012, 12, 309. [Google Scholar] [CrossRef]
- Robroek, S.J.; Reeuwijk, K.G.; Hillier, F.C.; Bambra, C.L.; van Rijn, R.M.; Burdorf, A. The contribution of overweight, obesity, and lack of physical activity to exit from paid employment: A meta-analysis. Scand. J. Work Environ. Health 2013, 39, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Korhonen, T.; Smeds, E.; Silventoinen, K.; Heikkila, K.; Kaprio, J. Cigarette smoking and alcohol use as predictors of disability retirement: A population-based cohort study. Drug Alcohol Depend. 2015, 155, 260–266. [Google Scholar] [CrossRef]
- Jansson, C.; Alexanderson, K.; Kecklund, G.; Akerstedt, T. Clinically diagnosed insomnia and risk of all-cause and diagnosis-specific disability pension: A nationwide cohort study. Sleep Disord. 2013, 2013, 209832. [Google Scholar] [CrossRef] [PubMed]
- Lallukka, T.; Haaramo, P.; Lahelma, E.; Rahkonen, O. Sleep problems and disability retirement: A register-based follow-up study. Am. J. Epidemiol. 2011, 173, 871–881. [Google Scholar] [CrossRef]
- Bevan, S. Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Pract. Res. Clin. Rheumatol. 2015, 29, 356–373. [Google Scholar] [CrossRef]
- Henderson, M.; Harvey, S.B.; Overland, S.; Mykletun, A.; Hotopf, M. Work and common psychiatric disorders. J. R. Soc. Med. 2011, 104, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Dewa, C.S.; Loong, D.; Bonato, S. Work outcomes of sickness absence related to mental disorders: A systematic literature review. BMJ Open 2014, 4, e005533. [Google Scholar] [CrossRef] [PubMed]
- Laaksonen, M.; Pitkaniemi, J.; Rahkonen, O.; Lahelma, E. Work arrangements, physical working conditions, and psychosocial working conditions as risk factors for sickness absence: Bayesian analysis of prospective data. Ann. Epidemiol. 2010, 20, 332–338. [Google Scholar] [CrossRef]
- Allebeck, P.; Mastekaasa, A. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 5. Risk factors for sick leave—General studies. Scand. J. Public Health Suppl. 2004, 63, 49–108. [Google Scholar]
- Rosario, S.; Fonseca, J.A.; Nienhaus, A.; da Costa, J.T. Standardized assessment of psychosocial factors and their influence on medically confirmed health outcomes in workers: A systematic review. J. Occup. Med. Toxicol. 2016, 11, 19. [Google Scholar] [CrossRef][Green Version]
- Ervasti, J.; Kivimaki, M.; Head, J.; Goldberg, M.; Airagnes, G.; Pentti, J.; Oksanen, T.; Salo, P.; Suominen, S.; Jokela, M.; et al. Sociodemographic Differences Between Alcohol Use and Sickness Absence: Pooled Analysis of Four Cohort Studies. Alcohol Alcohol. 2018, 53, 95–103. [Google Scholar] [CrossRef]
- Lahti, J.; Laaksonen, M.; Lahelma, E.; Rahkonen, O. The impact of physical activity on sickness absence. Scand. J. Med. Sci. Sports 2010, 20, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Quist, H.G.; Thomsen, B.L.; Christensen, U.; Clausen, T.; Holtermann, A.; Bjorner, J.B.; Andersen, L.L. Influence of lifestyle factors on long-term sickness absence among female healthcare workers: A prospective cohort study. BMC Public Health 2014, 14, 1084. [Google Scholar] [CrossRef]
- Rahkonen, O.; Lallukka, T.; Kronholm, E.; Vahtera, J.; Lahelma, E.; Laaksonen, M. Sleep problems and sickness absence among middle-aged employees. Scand. J. Work Environ. Health 2012, 38, 47–55. [Google Scholar] [CrossRef]
- Piha, K.; Laaksonen, M.; Martikainen, P.; Rahkonen, O.; Lahelma, E. Interrelationships between education, occupational class, income and sickness absence. Eur. J. Public Health 2010, 20, 276–280. [Google Scholar] [CrossRef]
- Christensen, K.B.; Labriola, M.; Lund, T.; Kivimaki, M. Explaining the social gradient in long-term sickness absence: A prospective study of Danish employees. J. Epidemiol. Community Health 2008, 62, 181–183. [Google Scholar] [CrossRef]
- Bruusgaard, D.; Smeby, L.; Claussen, B. Education and disability pension: A stronger association than previously found. Scand. J. Public Health 2010, 38, 686–690. [Google Scholar] [CrossRef]
- Leinonen, T.; Martikainen, P.; Lahelma, E. Interrelationships between education, occupational social class, and income as determinants of disability retirement. Scand. J. Public Health 2012, 40, 157–166. [Google Scholar] [CrossRef]
- Hensing, G. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 4. Methodological aspects in sickness-absence research. Scand. J. Public Health Suppl. 2004, 63, 44–48. [Google Scholar] [CrossRef]
- Ilmarinen, J.; Tuomi, K.; Eskelinen, L.; Nygard, C.H.; Huuhtanen, P.; Klockars, M. Background and objectives of the Finnish research project on aging workers in municipal occupations. Scand. J. Work Environ. Health 1991, 17, 7–11. [Google Scholar] [PubMed]
- Nygård, C.H.; Huuhtanen, P.; Tuomi, K.; Martikainen, R. Perceived work changes between 1981 and 1992 among aging workers in Finland. Scand. J. Work Environ. Health 1997, 23, 12–19. [Google Scholar]
- Ilmarinen, J.; Suurnakki, T.; Nygård, C.H.; Landau, K. Classification of municipal occupations. Scand. J. Work Environ. Health 1991, 17, 12–29. [Google Scholar] [PubMed]
- Nagin, D.S.; Odgers, C.L. Group-based trajectory modeling in clinical research. Annu. Rev. Clin. Psychol. 2010, 6, 109–138. [Google Scholar] [CrossRef]
- Dekkers-Sanchez, P.M.; Hoving, J.L.; Sluiter, J.K.; Frings-Dresen, M.H. Factors associated with long-term sick leave in sick-listed employees: A systematic review. Occup. Environ. Med. 2008, 65, 153–157. [Google Scholar] [CrossRef]
- Nagin, D.S. Group-based trajectory modeling: An overview. Ann. Nutr. Metab. 2014, 65, 205–210. [Google Scholar] [CrossRef]
- Virtanen, M.; Kivimaki, M.; Zins, M.; Dray-Spira, R.; Oksanen, T.; Ferrie, J.E.; Okuloff, A.; Pentti, J.; Head, J.; Goldberg, M.; et al. Lifestyle-related risk factors and trajectories of work disability over 5 years in employees with diabetes: Findings from two prospective cohort studies. Diabet. Med. 2015, 32, 1335–1341. [Google Scholar] [CrossRef]
- Haukka, E.; Kaila-Kangas, L.; Ojajarvi, A.; Miranda, H.; Karppinen, J.; Viikari-Juntura, E.; Markku, H.; Leino-Arjas, P. Pain in multiple sites and sickness absence trajectories: A prospective study among Finns. PA 2013, 154, 306–312. [Google Scholar] [CrossRef]
- Bekker, M.H.; Rutte, C.G.; van Rijswijk, K. Sickness absence: A gender-focused review. Psychol. Health Med. 2009, 14, 405–418. [Google Scholar] [CrossRef] [PubMed]
- Laaksonen, M.; Martikainen, P.; Rahkonen, O.; Lahelma, E. Explanations for gender differences in sickness absence: Evidence from middle-aged municipal employees from Finland. Occup. Environ. Med. 2008, 65, 325–330. [Google Scholar] [CrossRef]
- White, M.; Wagner, S.; Schultz, I.Z.; Murray, E.; Bradley, S.M.; Hsu, V.; McGuire, L.; Schulz, W. Modifiable workplace risk factors contributing to workplace absence across health conditions: A stakeholder-centered best-evidence synthesis of systematic reviews. Work 2013, 45, 475–492. [Google Scholar] [CrossRef] [PubMed]
- Detaille, S.I.; Heerkens, Y.F.; Engels, J.A.; van der Gulden, J.W.; van Dijk, F.J. Common prognostic factors of work disability among employees with a chronic somatic disease: A systematic review of cohort studies. Scand. J. Work Environ. Health 2009, 35, 261–281. [Google Scholar] [CrossRef]
- Ervasti, J.; Mattila-Holappa, P.; Joensuu, M.; Pentti, J.; Lallukka, T.; Kivimaki, M.; Vahtera, J.; Virtanen, M. Predictors of Depression and Musculoskeletal Disorder Related Work Disability Among Young, Middle-Aged, and Aging Employees. J. Occup. Environ. Med. 2017, 59, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Sundstrup, E.; Jakobsen, M.D.; Mortensen, O.S.; Andersen, L.L. Joint association of multimorbidity and work ability with risk of long-term sickness absence: A prospective cohort study with register follow-up. Scand. J. Work Environ. Health 2017, 43, 146–154. [Google Scholar] [CrossRef]
- Salonen, L.; Blomgren, J.; Laaksonen, M. From long-term sickness absence to disability retirement: Diagnostic and occupational class differences within the working-age Finnish population. BMC Public Health 2020, 20, 1078. [Google Scholar] [CrossRef]
- Wagner, S.; White, M.; Schultz, I.; Murray, E.; Bradley, S.M.; Hsu, V.; McGuire, L.; Schulz, W. Modifiable worker risk factors contributing to workplace absence: A stakeholder-centred best-evidence synthesis of systematic reviews. Work 2014, 49, 541–558. [Google Scholar] [CrossRef]
- Duijts, S.F.; Kant, I.; Swaen, G.M.; van den Brandt, P.A.; Zeegers, M.P. A meta-analysis of observational studies identifies predictors of sickness absence. J. Clin. Epidemiol. 2007, 60, 1105–1115. [Google Scholar] [CrossRef]
- Lundborg, P. Does smoking increase sick leave? Evidence using register data on Swedish workers. Tob. Control. 2007, 16, 114–118. [Google Scholar]
- Laaksonen, M.; Piha, K.; Martikainen, P.; Rahkonen, O.; Lahelma, E. Health-related behaviours and sickness absence from work. Occup. Environ. Med. 2009, 66, 840–847. [Google Scholar] [CrossRef] [PubMed]
- Bang Christensen, K.; Lund, T.; Labriola, M.; Villadsen, E.; Bultmann, U. The fraction of long-term sickness absence attributable to work environmental factors: Prospective results from the Danish Work Environment Cohort Study. Occup. Environ. Med. 2007, 64, 487–489. [Google Scholar] [CrossRef] [PubMed]
- Lallukka, T.; Kaila-Kangas, L.; Koskinen, S.; Haukka, E.; Kausto, J.; Leino-Arjas, P.; Kaikkonen, R.; Halonen, J.; Shiri, R. Occupational exposures and sickness absence trajectories: A nationally representative seven-year follow-up study among Finnish working-aged people. Int J. Environ. Res. Public Health 2019, 16, 2099. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, M.L.; Rugulies, R.; Smith-Hansen, L.; Christensen, K.B.; Kristensen, T.S. Psychosocial work environment and registered absence from work: Estimating the etiologic fraction. Am. J. Ind. Med. 2006, 49, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Vaananen, A.; Toppinen-Tanner, S.; Kalimo, R.; Mutanen, P.; Vahtera, J.; Peiro, J.M. Job characteristics, physical and psychological symptoms, and social support as antecedents of sickness absence among men and women in the private industrial sector. Soc. Sci. Med. 2003, 57, 807–824. [Google Scholar] [CrossRef]
- Darr, W.; Johns, G. Work strain, health, and absenteeism: A meta-analysis. J. Occup. Health Psychol. 2008, 13, 293–318. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, P.; Siukola, A.; Lipiainen, L.; Liukkonen, V.; Pentti, J.; Vahtera, J. Trajectory analyses of sickness absence among industrial and municipal employees. Occup. Med. 2017, 67, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Tuomi, K.; Toikkanen, J.; Eskelinen, L.; Backman, A.L.; Ilmarinen, J.; Järvinen, E.; Klockars, M. Mortality, disability and changes in occupation among aging municipal employees. Scand. J. Work Environ. Health 1991, 17, 58–66. [Google Scholar]
- Laaksonen, M.; Blomgren, J.; Gould, R. Sickness allowance trajectories preceding disability retirement: A register-based retrospective study. Eur. J. Public Health 2016, 26, 1050–1055. [Google Scholar] [PubMed]
- Nygård, C.-H.; Suurnäkki, T.; Ilmarinen, J. Job Demands of Ageing Employees Over 12-Year Period. In FinnAge—Respect for the Aging: Action Programme to Promote Health, Work Ability and Well-Being Aging Workers 1990–1996; Ilmarinen, J., Louhevaara, V., Eds.; Finnish Institute of Occupational Health: Helsinki, Finland, 1999; pp. 251–259. [Google Scholar]
- Neupane, S.; Nygård, C.H.; Prakash, K.C.; von Bonsdorff, M.B.; von Bonsdorff, M.E.; Seitsamo, J.; Ilmarinen, J.; Leino-Arjas, P. Multisite musculoskeletal pain trajectories from midlife to old age: A 28-year follow-up of municipal employees. Occup. Environ. Med. 2018, 75, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Prada, S.; Demou, E.; Lalloo, D.; Avila-Palencia, I.; Sanati, K.A.; Sampere, M.; Freer, K.; Serra, C.; Macdonald, E.B. Effectiveness of very early workplace interventions to reduce sickness absence: A systematic review of the literature and meta-analysis. Scand. J. Work Environ. Health 2016, 42, 261–272. [Google Scholar] [CrossRef]
- Oakman, J.; Neupane, S.; Proper, K.I.; Kinsman, N.; Nygård, C.H. Workplace interventions to improve work ability: A systematic review and meta-analysis of their effectiveness. Scand. J. Work Environ. Health 2018, 44, 134–146. [Google Scholar] [CrossRef] [PubMed]

| a. Women | |||
|---|---|---|---|
| Characteristic | Sickness Absence Trajectory | ||
| Low (n = 2685) | Intermediate (n = 548) | Increasing (n = 227) | |
| Age (Mean, SD) | 50.3 (3.6) | 50.5 (3.6) | 51.7 (3.5) |
| Basic education (%) | |||
| Elementary school not completed | 14.5 | 20.3 | 25.3 |
| Elementary school completed | 47.5 | 55.8 | 52.4 |
| Complementary school completed | 38.0 | 23.8 | 22.2 |
| Family income (%) | |||
| Good | 40.7 | 33.8 | 32.7 |
| Satisfactory | 55.5 | 62.4 | 62.7 |
| Poor | 3.8 | 3.7 | 4.6 |
| Lifestyle factors | |||
| Smoking (%) | |||
| No | 89.7 | 88.4 | 85.2 |
| Yes | 10.3 | 11.6 | 14.8 |
| BMI (%) | |||
| Normal (<25 kg/m2) | 55.8 | 45.9 | 43.0 |
| Overweight (25–30 kg/m2) | 35.7 | 43.3 | 42.5 |
| Obese (>30 kg/m2) | 8.5 | 10.8 | 14.5 |
| Leisure-time physical activity (%) | |||
| At least twice a week | 32.9 | 29.9 | 24.7 |
| Once a week | 45.7 | 47.2 | 48.0 |
| Less frequently | 21.4 | 23.0 | 27.4 |
| Sleep problems (Mean, SD) | 3.3 (2.1) | 4.2 (2.4) | 4.6 (2.4) |
| Morbidity and injuries (%) | |||
| Musculoskeletal (yes vs. no) | 31.1 | 57.7 | 64.8 |
| Cardiovascular (yes vs. no) | 14.1 | 22.5 | 32.2 |
| Respiratory (yes vs. no) | 8.9 | 17.5 | 18.9 |
| Mental (yes vs. no) | 3.4 | 5.7 | 10.1 |
| Other diseases (yes vs. no) | 19.0 | 32.7 | 38.3 |
| Injuries (yes vs. no) | 7.8 | 15.7 | 20.3 |
| Working conditions (Mean, SD) | |||
| Awkward work postures | 5.0 (3.0) | 6.3 (2.8) | 6.6 (2.6) |
| Physical demands | 4.7 (2.7) | 5.8 (2.6) | 5.8 (2.6) |
| Physical and chemical exposures | 1.7 (1.6) | 2.2 (1.8) | 2.3 (1.8) |
| Satisfaction with management | 3.2 (1.8) | 3.4 (2.9) | 3.4 (1.9) |
| Job control | 5.5 (2.4) | 4.7 (2.5) | 4.7 (2.4) |
| Mental demands | 5.3 (3.0) | 4.4 (3.0) | 4.3 (3.3) |
| b. Men | |||
| Characteristic | Sickness Absence Trajectory | ||
| Low (n = 2028) | Intermediate (n = 491) | Increasing (n = 278) | |
| Age (Mean, SD) | 50.2 (3.6) | 50.8 (3.7) | 51.7 (3.5) |
| Basic education (%) | |||
| Elementary school not completed | 26.3 | 28.5 | 38.0 |
| Elementary school completed | 56.5 | 63.8 | 54.5 |
| Complementary school completed | 17.3 | 7.6 | 7.7 |
| Family income (%) | |||
| Good | 30.7 | 20.6 | 20.5 |
| Satisfactory | 64.2 | 72.2 | 73.3 |
| Poor | 5.2 | 7.2 | 6.2 |
| Lifestyle factors | |||
| Smoking (%) | |||
| No | 74.1 | 60.5 | 60.5 |
| Yes | 25.9 | 39.5 | 39.5 |
| BMI (%) | |||
| Normal (<25 kg/m2) | 38.2 | 35.4 | 35.6 |
| Overweight (25–30 kg/m2) | 52.2 | 53.1 | 50.9 |
| Obese (>30 kg/m2) | 9.6 | 11.5 | 13.5 |
| Leisure-time physical activity (%) | |||
| At least twice a week | 30.3 | 21.1 | 20.0 |
| Once a week | 48.0 | 52.9 | 47.4 |
| Less frequently | 21.7 | 25.9 | 32.6 |
| Sleep problems (Mean, SD) | 3.1 (2.1) | 4.0 (2.4) | 4.4 (2.3) |
| Morbidity and injuries (%) | |||
| Musculoskeletal (yes vs. no) | 28.4 | 50.1 | 54.7 |
| Cardiovascular (yes vs. no) | 18.7 | 24.2 | 32,0 |
| Respiratory (yes vs. no) | 7.8 | 14.7 | 14.0 |
| Mental (yes vs. no) | 3.7 | 8.2 | 6.1 |
| Other disease (yes vs. no) | 24.9 | 38.7 | 42.5 |
| Injuries (yes vs. no) | 13.4 | 20.8 | 20.5 |
| Working conditions | |||
| Awkward work postures | 4.4 (2.9) | 5.7 (2.6) | 5.6 (2.9) |
| Physical demands | 3.6 (2.5) | 4.1 (2.5) | 4.6 (2.6) |
| Physical and chemical exposures | 3.1 (2.4) | 4.0 (2.3) | 3.9 (2.2) |
| Satisfaction with management | 3.4 (1.9) | 3.6 (2.0) | 3.6 (1.9) |
| Job control | 4.8 (2.6) | 4.2 (2.4) | 4.2 (2.4) |
| Mental demands | 5.6 (2.9) | 5.4 (2.9) | 5.2 (2.8) |
| Model 1 | Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Intermediate vs. Low | Increasing vs. Low | Intermediate vs. Low | Increasing vs. Low | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Lifestyle factors | ||||||||
| Smoking (yes vs. no) | 1.15 | 0.84–1.59 | 0.71 | 0.28–1.80 | 1.16 | 0.82–1.64 | 0.55 | 0.21–1.46 |
| BMI, kg/m2 (ref: < 25) | ||||||||
| 25-30 | 1.55 | 1.24–1.93 | 1.47 | 0.84–2.59 | 1.31 | 1.03–1.65 | 1.13 | 0.63–2.04 |
| ≥30 | 1.71 | 1.21–2.43 | 3.79 | 1.97–7.31 | 1.26 | 0.86–1.85 | 2.13 | 1.03–4.40 |
| LTPA 2 (ref: At least twice a week) | ||||||||
| Once a week | 1.18 | 0.93–1.50 | 1.84 | 0.93–3.61 | 1.04 | 0.81–1.34 | 1.62 | 0.81–3.27 |
| Less frequently | 1.13 | 0.85–1.50 | 2.84 | 1.40–5.76 | 0.97 | 0.71–1.32 | 2.40 | 1.12–5.11 |
| Sleep problems (ref: no) | ||||||||
| Moderate | 1.35 | 1.03–1.76 | 1.17 | 0.56–2.45 | 1.11 | 0.84–1.47 | 0.92 | 0.43–1.98 |
| Frequent | 2.58 | 2.02–3.28 | 3.84 | 2.14–6.89 | 1.74 | 1.33–2.27 | 2.08 | 1.10–3.96 |
| Morbidity and injuries | ||||||||
| Musculoskeletal (yes vs. no) | 3.15 | 2.55–3.89 | 5.98 | 3.44–10.4 | 2.17 | 1.72–2.73 | 3.58 | 1.96–6.54 |
| Cardiovascular (yes vs. no) | 1.86 | 1.44–2.41 | 2.17 | 1.23–3.84 | 1.33 | 1.00–1.76 | 1.26 | 0.68–2.33 |
| Respiratory (yes vs. no) | 2.52 | 1.89–3.36 | 3.96 | 2.23–7.03 | 1.73 | 1.27–2.36 | 2.81 | 1.50–5.27 |
| Mental (yes vs. no) | 1.49 | 0.89–2.51 | 5.16 | 2.45–10.9 | 0.91 | 0.53–1.59 | 2.52 | 1.07–5.91 |
| Other diseases (yes vs. no) | 2.26 | 1.80–2.84 | 2.27 | 1.34–3.84 | 1.52 | 1.18–1.95 | 1.17 | 0.66–2.09 |
| Injuries (yes vs. no) | 2.03 | 1.48–2.79 | 3.44 | 1.86–6.36 | 1.28 | 0.90–1.81 | 2.02 | 1.03–3.95 |
| Working conditions | ||||||||
| Awkward work postures (ref: low) | ||||||||
| Moderate | 1.97 | 1.49–2.59 | 1.79 | 0.90–3.55 | 1.35 | 0.98–1.86 | 1.28 | 0.57–2.87 |
| High | 2.95 | 2.27–3.84 | 3.05 | 1.63–5.69 | 1.55 | 1.10–2.19 | 1.45 | 0.63–3.35 |
| Physical demands (ref: low) | ||||||||
| Moderate | 1.87 | 1.44–2.44 | 1.26 | 0.66–2.41 | 1.29 | 0.94–1.77 | 0.80 | 0.37–1.73 |
| High | 2.73 | 2.09–3.57 | 2.51 | 1.38–4.57 | 1.41 | 0.98–2.02 | 1.22 | 0.53–2.80 |
| Physical and chemical exposures (ref: low) | ||||||||
| Moderate | 1.43 | 1.11–1.85 | 1.56 | 0.85–2.87 | 1.09 | 0.83–1.44 | 1.03 | 0.53–1.97 |
| High | 2.00 | 1.55–2.57 | 1.83 | 0.99–3.38 | 1.04 | 0.77–1.39 | 0.78 | 0.39–1.58 |
| Satisfaction with management (ref: low) | ||||||||
| Moderate | 0.75 | 0.57–0.99 | 1.25 | 0.66–2.34 | 0.81 | 0.60–1.09 | 0.86 | 0.43–1.70 |
| High | 0.81 | 0.64–1.03 | 0.57 | 0.32–1.02 | 0.96 | 0.73–1.26 | 0.77 | 0.40–1.49 |
| Job control (ref: low) | ||||||||
| Moderate | 0.76 | 0.59–0.98 | 0.71 | 0.38–1.34 | 0.83 | 0.63–1.10 | 0.53 | 0.26–1.11 |
| High | 0.57 | 0.45–0.73 | 0.54 | 0.31–0.96 | 0.87 | 0.65–1.17 | 1.02 | 0.52–2.04 |
| Mental demands (ref: low) | ||||||||
| Moderate | 0.56 | 0.44–0.71 | 0.63 | 0.36–1.10 | 0.81 | 0.61–1.07 | 0.86 | 0.45–1.65 |
| High | 0.49 | 0.38–0.64 | 0.49 | 0.26–0.94 | 0.63 | 0.46–0.88 | 0.62 | 0.28–1.40 |
| Model 1 | Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Intermediate vs. Low | Increasing vs. Low | Intermediate vs. Low | Increasing vs. Low | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Lifestyle factors | ||||||||
| Smoking (yes vs. no) | 1.82 | 1.44–2.30 | 1.93 | 1.29–2.92 | 1.64 | 1.27–2.11 | 1.61 | 1.03–2.50 |
| BMI, kg/m2 (ref: < 25) | ||||||||
| 25-30 | 1.16 | 0.91–1.47 | 1.13 | 0.73–1.73 | 1.09 | 0.84–1.41 | 1.05 | 0.66–1.65 |
| ≥30 | 1.41 | 0.96–2.07 | 1.50 | 0.76–2.95 | 1.33 | 0.88–2.01 | 1.38 | 0.66–2.86 |
| LTPA 2 (ref: at least twice a week) | ||||||||
| Once a week | 1.46 | 1.10–1.93 | 2.01 | 1.12–3.63 | 1.19 | 0.88–1.61 | 1.58 | 0.85–2.97 |
| Less frequently | 1.55 | 1.12–2.14 | 3.42 | 1.86–6.30 | 1.11 | 0.78–1.58 | 2.35 | 1.20–4.60 |
| Sleep problems (ref: no) | ||||||||
| Moderate | 1.40 | 1.06–1.86 | 2.05 | 1.20–3.52 | 1.17 | 0.87–1.58 | 1.53 | 0.87–2.70 |
| Frequent | 2.36 | 1.81–3.08 | 4.32 | 2.66–7.00 | 1.51 | 1.11–2.03 | 2.30 | 1.35–3.93 |
| Morbidity and injuries | ||||||||
| Musculoskeletal (yes vs. no) | 2.49 | 1.97–3.13 | 3.53 | 2.36–5.28 | 1.70 | 1.31–2.20 | 2.28 | 1.45–3.57 |
| Cardiovascular (yes vs. no) | 1.32 | 1.00–1.73 | 2.06 | 1.34–3.17 | 0.94 | 0.70–1.26 | 1.33 | 0.84–2.11 |
| Respiratory (yes vs. no) | 1.97 | 1.40–2.78 | 2.64 | 1.53–4.55 | 1.31 | 0.89–1.91 | 1.42 | 0.78–2.57 |
| Mental (yes vs. no) | 2.52 | 1.59–4.00 | 3.03 | 1.44–6.35 | 1.80 | 1.09–2.95 | 1.68 | 0.76–3.71 |
| Other diseases (yes vs. no) | 2.11 | 1.67–2.67 | 2.18 | 1.45–3.27 | 1.53 | 1.18–1.98 | 1.29 | 0.83–2.02 |
| Injuries (yes vs. no) | 1.72 | 1.29–2.32 | 1.39 | 0.82–2.37 | 1.11 | 0.80–1.53 | 0.80 | 0.45–1.41 |
| Working conditions | ||||||||
| Awkward work postures (ref: low) | ||||||||
| Moderate | 2.50 | 1.85–3.37 | 1.49 | 0.88–2.53 | 1.80 | 1.26–2.57 | 0.81 | 0.44–1.52 |
| High | 3.42 | 2.51–4.67 | 3.25 | 1.97–5.36 | 1.92 | 1.29–2.86 | 1.25 | 0.65–2.41 |
| Physical demands (ref: low) | ||||||||
| Moderate | 1.19 | 0.90–1.59 | 1.61 | 0.94–2.77 | 0.97 | 0.71–1.32 | 1.37 | 0.77–2.42 |
| High | 1.83 | 1.39–2.39 | 2.66 | 1.60–4.41 | 1.07 | 0.78–1.47 | 1.62 | 0.90–2.91 |
| Physical and chemical exposures (ref: low) | ||||||||
| Moderate | 1.85 | 1.38–2.47 | 2.58 | 1.54–4.33 | 1.20 | 0.86–1.66 | 1.70 | 0.96–3.04 |
| High | 2.75 | 2.06–3.67 | 2.94 | 1.71–5.04 | 1.32 | 0.92–1.88 | 1.22 | 0.63–2.36 |
| Satisfaction with management (ref: low) | ||||||||
| Moderate | 1.09 | 0.82–1.46 | 0.87 | 0.54–1.39 | 1.33 | 0.98–1.81 | 1.04 | 0.62–1.73 |
| High | 0.75 | 0.57–0.97 | 0.34 | 0.21–0.56 | 1.06 | 0.79–1.42 | 0.49 | 0.28–0.85 |
| Job control (ref: low) | ||||||||
| Moderate | 0.69 | 0.53–0.90 | 0.66 | 0.41–1.04 | 0.79 | 0.60–1.06 | 0.82 | 0.50–1.36 |
| High | 0.50 | 0.38–0.66 | 0.40 | 0.24–0.67 | 0.84 | 0.61–1.17 | 0.92 | 0.51–1.65 |
| Mental demands (ref: low) | ||||||||
| Moderate | 0.82 | 0.63–1.09 | 0.98 | 0.63–1.53 | 0.91 | 0.69–1.21 | 1.19 | 0.76–1.88 |
| High | 0.87 | 0.67–1.14 | 0.47 | 0.27–0.80 | 1.03 | 0.78–1.36 | 0.60 | 0.34–1.03 |
| Sickness Absence Trajectories 1981–1985 | Model 1 | Model 2 | ||
|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | |
| Women | ||||
| Low | 1 | - | 1 | - |
| Intermediate | 3.19 | 2.74–3.71 | 3.05 | 2.62–3.56 |
| Increasing | 12.7 | 8.20–19.7 | 11.8 | 7.57–18.3 |
| Men | ||||
| Low | 1 | - | 1 | - |
| Intermediate | 2.10 | 1.80–2.46 | 2.04 | 1.74–2.34 |
| Increasing | 11.4 | 7.71–16.7 | 10.5 | 7.1–15.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leino-Arjas, P.; Seitsamo, J.; Nygård, C.-H.; K.C., P.; Neupane, S. Process of Work Disability: From Determinants of Sickness Absence Trajectories to Disability Retirement in a Long-Term Follow-Up of Municipal Employees. Int. J. Environ. Res. Public Health 2021, 18, 2614. https://doi.org/10.3390/ijerph18052614
Leino-Arjas P, Seitsamo J, Nygård C-H, K.C. P, Neupane S. Process of Work Disability: From Determinants of Sickness Absence Trajectories to Disability Retirement in a Long-Term Follow-Up of Municipal Employees. International Journal of Environmental Research and Public Health. 2021; 18(5):2614. https://doi.org/10.3390/ijerph18052614
Chicago/Turabian StyleLeino-Arjas, Päivi, Jorma Seitsamo, Clas-Håkan Nygård, Prakash K.C., and Subas Neupane. 2021. "Process of Work Disability: From Determinants of Sickness Absence Trajectories to Disability Retirement in a Long-Term Follow-Up of Municipal Employees" International Journal of Environmental Research and Public Health 18, no. 5: 2614. https://doi.org/10.3390/ijerph18052614
APA StyleLeino-Arjas, P., Seitsamo, J., Nygård, C.-H., K.C., P., & Neupane, S. (2021). Process of Work Disability: From Determinants of Sickness Absence Trajectories to Disability Retirement in a Long-Term Follow-Up of Municipal Employees. International Journal of Environmental Research and Public Health, 18(5), 2614. https://doi.org/10.3390/ijerph18052614









