Exposure to Occupational Hazards among Health Care Workers in Low- and Middle-Income Countries: A Scoping Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Charting of the Data
2.4. Collating and Summarising the Results
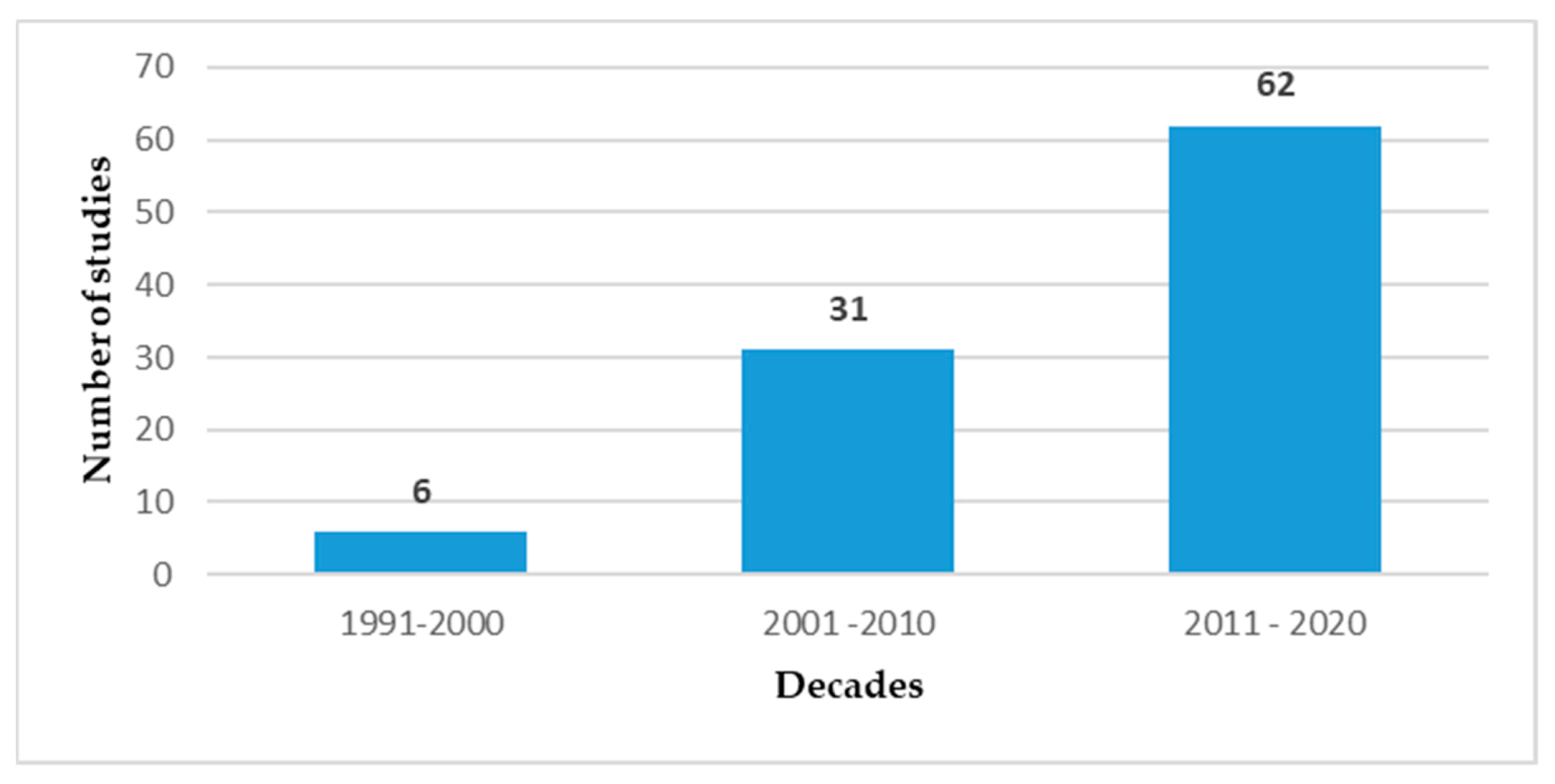
3. Results
4. Discussion
4.1. Biological Hazards
4.1.1. Bloodborne Pathogens
4.1.2. Tuberculosis
4.2. Psychosocial Hazards
4.2.1. Workplace Violence
4.2.2. Burnout
4.2.3. Work Environment and Job Satisfaction
4.3. Ergonomic Hazards
4.4. Chemical Hazards
4.5. Implications
4.6. Strengths and Limitations of the Review
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vecchio, D.; Sasco, A.J.; Cann, C.I. Occupational risk in health care and research. Am. J. Ind. Med. 2003, 43, 369–397. [Google Scholar] [CrossRef] [PubMed]
- The Lancet. COVID-19: Protecting health-care workers. Lancet 2020, 395, 922. [Google Scholar] [CrossRef]
- McDiarmid, M.A. Hazards of the health care sector: Looking beyond infectious disease. Ann. Glob. Health 2014, 80, 315–319. [Google Scholar] [CrossRef]
- Coggon, D.; Harris, E.; Poole, J.; Palmer, K. Mortality of workers exposed to ethylene oxide: Extended follow up of a British cohort. Occup. Environ. Med. 2004, 61, 358–362. [Google Scholar] [CrossRef]
- Ratner, P.A.; Spinelli, J.J.; Beking, K.; Lorenzi, M.; Chow, Y.; Teschke, K.; Le, N.D.; Gallagher, R.P.; Dimich-Ward, H. Cancer incidence and adverse pregnancy outcome in registered nurses potentially exposed to antineoplastic drugs. BMC Nurs. 2010, 9, 15. [Google Scholar] [CrossRef]
- Vaughan, T.L.; Stewart, P.A.; Teschke, K.; Lynch, C.F.; Swanson, G.M.; Lyon, J.L.; Berwick, M. Occupational exposure to formaldehyde and wood dust and nasopharyngeal carcinoma. Occup. Environ. Med. 2000, 57, 376–384. [Google Scholar] [CrossRef]
- Arif, A.A.; Delclos, G.L. Association between cleaning-related chemicals and work-related asthma and asthma symptoms among healthcare professionals. Occup. Environ. Med. 2012, 69, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Trapé, M.; Schenck, P.; Warren, A. Latex gloves use and symptoms in health care workers 1 year after implementation of a policy restricting the use of powdered gloves. Am. J. Infect. Control 2000, 28, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Davis, K.G.; Kotowski, S.E. Prevalence of musculoskeletal disorders for nurses in hospitals, long-term care facilities, and home health care: A comprehensive review. Hum. Factors 2015, 57, 754–792. [Google Scholar] [CrossRef]
- Phillips, J.P. Workplace violence against health care workers in the United States. N. Engl. J. Med. 2016, 374, 1661–1669. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C. Burnout: The Cost of Caring; Malor Books: Cambridge, MA, USA, 2003. [Google Scholar]
- National Institute of Occupational Health and Safety. State of the Sector: Healthcare and Social Assistance; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2009.
- Nuwayhid, I.A. Occupational health research in developing countries: A partner for social justice. Am. J. Public Health 2004, 94, 1916–1921. [Google Scholar] [CrossRef]
- Ingersoll, G.L.; Olsan, T.; Drew-Cates, J.; DeVinney, B.C.; Davies, J. Nurses’ job satisfaction, organizational commitment, and career intent. J. Nurs. Admin. 2002, 32, 250–263. [Google Scholar] [CrossRef]
- Liese, B.; Dussault, G. The State of the Health Workforce in Sub-Saharan Africa: Evidence of Crisis and Analysis of Contributing Factors; The World Bank: Washington, DC, USA, 2004. [Google Scholar]
- Owie, H.; Apanga, P. Occupational health hazards prevailing among healthcare workers in developing countries. J. AIDS Clin. Res. 2016, 7, 596. [Google Scholar]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Daudt, H.M.; van Mossel, C.; Scott, S.J. Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med. Res. Methodol. 2013, 13, 1–9. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Colquhoun, H.L.; Levac, D.; O’Brien, K.K.; Straus, S.; Tricco, A.C.; Perrier, L.; Kastner, M.; Moher, D. Scoping reviews: Time for clarity in definition, methods, and reporting. J. Clin. Epidemiol. 2014, 67, 1291–1294. [Google Scholar] [CrossRef]
- Peters, M.; Godfrey, C.; McInerney, P.; Soares, C.B.; Khalil, H.; Parker, D. Methodology for JBI Scoping Reviews. The Joanna Briggs Institute Reviewers’ Manual 2015; The Joanna Briggs Institute: Adelaide, Australia, 2015. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Sources and Classification of Health Workforce Statistics; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- World Bank. World Bank Country Classification 2020. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 17 April 2020).
- Joshi, R.; Reingold, A.L.; Menzies, D.; Pai, M. Tuberculosis among health-care workers in low-and middle-income countries: A systematic review. PLoS Med. 2006, 3, e494. [Google Scholar] [CrossRef]
- World Health Organization; International Labour Organization. Caring for Those Who Care: National Programmes for Occupational Health for Health Workers. Policy Brief; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Cavalcante, N.J.F.; Abreu, E.S.; Fernandes, M.E.L.; Richtmann, R.; Piovesana, M.N.; Yamada, F.T.; Carvalho, E.S. Risk of health care professionals acquiring HIV infection in Latin America. AIDS Care 1991, 3, 311–316. [Google Scholar] [CrossRef]
- Adegboye, A.A.; Moss, G.B.; Soyinka, F.; Kreiss, J.K. The epidemiology of needlestick and sharp instrument accidents in a Nigerian hospital. Infect. Control Hosp. Epidemiol. 1994, 15, 27–31. [Google Scholar] [CrossRef]
- Olubuyide, I. Doctors at risk of hepatitis B and HIV infection from patients in Nigeria. J. Roy. Soc. Health 1996, 116, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Gumodoka, B.; Favot, I.; Berege, Z.; Dolmans, W. Occupational exposure to the risk of HIV infection among health care workers in Mwanza Region, United Republic of Tanzania. Bull. World Health Organ. 1997, 75, 133–140. [Google Scholar]
- Khuri-Bulos, N.A.; Toukan, A.; Mahafzah, A.; Al Adham, M.; Faori, I.; Khader, I.A.; Rumeileh, Z.I.A. Epidemiology of needlestick and sharp injuries at a university hospital in a developing country: A 3-year prospective study at the Jordan University Hospital, 1993 through 1995. Am. J. Infect. Control 1997, 25, 322–329. [Google Scholar] [CrossRef]
- Gounden, Y.P.; Moodley, J. Exposure to human immunodeficiency virus among healthcare workers in South Africa. Int. J. Gynecol. Obstet. 2000, 69, 265–270. [Google Scholar] [CrossRef]
- Phipps, W.; Honghong, W.; Min, Y.; Burgess, J.; Pellico, L.; Watkins, C.W.; Guoping, H.; Williams, A. Risk of medical sharps injuries among Chinese nurses. Am. J. Infect. Control 2002, 30, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Talaat, M.; Kandeel, A.; El-Shoubary, W.; Bodenschatz, C.; Khairy, I.; Oun, S.; Mahoney, F.J. Occupational exposure to needlestick injuries and hepatitis B vaccination coverage among health care workers in Egypt. Am. J. Infect. Control 2003, 31, 469–474. [Google Scholar] [CrossRef]
- Kermode, M.; Jolley, D.; Langkham, B.; Thomas, M.S.; Crofts, N. Occupational exposure to blood and risk of bloodborne virus infection among health care workers in rural north Indian health care settings. Am. J. Infect. Control 2005, 33, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Kermode, M.; Jolley, D.; Langkham, B.; Thomas, M.S.; Holmes, W.; Gifford, S.M. Compliance with Universal/Standard Precautions among health care workers in rural north India. Am. J. Infect. Control 2005, 33, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Nsubuga, F.M.; Jaakkola, M.S. Needle stick injuries among nurses in sub-Saharan Africa. Trop. Med. Int. Health 2005, 10, 773–781. [Google Scholar] [CrossRef]
- Obi, S.; Waboso, P.; Ozumba, B. HIV/AIDS: Occupational risk, attitude and behaviour of surgeons in Southeast Nigeria. Int. J. STD AIDS 2005, 16, 370–373. [Google Scholar]
- Chelenyane, M.; Endacott, R. Self-reported infection control practices and perceptions of HIV/AIDS risk amongst emergency department nurses in Botswana. Accid. Emerg. Nurs. 2006, 14, 148–154. [Google Scholar] [CrossRef]
- Akinleye, A.A.; Omokhodion, F.O. Work practices of primary health care workers in urban and rural health facilities in south-west Nigeria. Aust. J. Rural Health 2008, 16, 47–48. [Google Scholar] [CrossRef] [PubMed]
- Okeke, E.; Ladep, N.; Agaba, E.; Malu, A. Hepatitis B vaccination status and needle stick injuries among medical students in a Nigerian university. Niger. J. Med. 2008, 17, 330–332. [Google Scholar] [CrossRef]
- Taegtmeyer, M.; Suckling, R.; Nguku, P.; Meredith, C.; Kibaru, J.; Chakaya, J.M.; Muchela, H.; Gilks, C. Working with risk: Occupational safety issues among healthcare workers in Kenya. AIDS Care 2008, 20, 304–310. [Google Scholar] [CrossRef]
- Chen, L.; Zhang, M.; Yan, Y.; Miao, J.; Lin, H.; Zhang, Y.; Wang, H.; Du, X.; Li, T. Sharp object injuries among health care workers in a Chinese province. AAOHN J. 2009, 57, 13–16. [Google Scholar] [CrossRef]
- Simon, L.P. Prevention and management of needlestick injury in Delhi. Br. J. Nurs. 2009, 18, 252–256. [Google Scholar] [CrossRef]
- Chakravarthy, M.; Singh, S.; Arora, A.; Sengupta, S.; Munshi, N. The epinet data of four Indian hospitals on incidence of exposure of healthcare workers to blood and body fluid: A multicentric prospective analysis. Indian J. Med. Sci. 2010, 64, 540–548. [Google Scholar] [CrossRef]
- Yacoub, R.; Al Ali, R.; Moukeh, G.; Lahdo, A.; Mouhammad, Y.; Nasser, M. Hepatitis B vaccination status and needlestick injuries among healthcare workers in Syria. J. Glob. Infect. Dis. 2010, 2, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Sangwan, B.; Kotwal, A.; Verma, A. Occupational exposure to blood and body fluids amongst health care workers in a teaching hospital of the armed forces. Med. J. Armed Forces India 2011, 67, 21–24. [Google Scholar] [CrossRef]
- Irmak, Z. Needlestick and sharps injury among nurses at a state hospital in Turkey. Aust. J. Adv. Nurs. 2012, 30, 48–55. [Google Scholar]
- Nasim, S.; Shahid, A.; Mustufa, M.A.; Arain, G.M.; Ali, G.; Taseer, I.-U.-H.; Talreja, K.L.; Firdous, R.; Iqbal, R.; Siddique, S.A.; et al. Biosafety perspective of clinical laboratory workers: A profile of Pakistan. J. Infect. Dev. Ctries. 2012, 6, 611–619. [Google Scholar] [CrossRef][Green Version]
- Omorogbe, V.E.; Omuemu, V.O.; Isara, A.R. Injection safety practices among nursing staff of mission hospitals in Benin City, Nigeria. Ann. Afr. Med. 2012, 11, 36–41. [Google Scholar]
- Phillips, E.K.; Simwale, O.J.; Chung, M.J.; Parker, G.; Perry, J.; Jagger, J.C. Risk of bloodborne pathogen exposure among Zambian healthcare workers. J. Infect. Public Health 2012, 5, 244–249. [Google Scholar] [CrossRef]
- Sethi, A.K.; Acher, C.W.; Kirenga, B.; Mead, S.; Donskey, C.J.; Katamba, A. Infection Control Knowledge, Attitudes, and Practices among Healthcare Workers at Mulago Hospital, Kampala, Uganda. Infect Control Hosp. Epidemiol. 2012, 33, 917–923. [Google Scholar] [CrossRef]
- Abkar, M.A.A.; Wahdan, I.M.H.; Sherif, A.A.R.; Raja’a, Y.A. Unsafe injection practices in Hodeidah governorate, Yemen. J. Infect. Public Health 2013, 6, 252–260. [Google Scholar] [CrossRef][Green Version]
- Afridi, A.A.K.; Kumar, A.; Sayani, R. Needle stick injuries-risk and preventive factors: A study among health care workers in tertiary care hospitals in Pakistan. Glob. J. Health Sci. 2013, 5, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Rajkumari, N.; Thanbuana, B.T.; John, N.V.; Gunjiyal, J.; Mathur, P.; Misra, M.C. A prospective look at the burden of sharps injuries and splashes among trauma health care workers in developing countries: True picture or tip of iceberg. Injury 2014, 45, 1470–1478. [Google Scholar] [CrossRef] [PubMed]
- Bekele, T.; Gebremariam, A.; Ahmed, K. Attitude, reporting behavour and management practice of occupational needle stick and sharps injuries among hospital healthcare workers in Bale zone, Southeast Ethiopia: A cross-sectional study. J. Occup. Med. Toxicol. 2015, 10, 42. [Google Scholar] [CrossRef]
- Priya, N.L.; Krishnan, K.U.; Jayalakshmi, G.; Vasanthi, S. An analysis of multimodal occupational exposure leading to blood borne infections among health care workers. Indian J. Pathol. Microbiol. 2015, 58, 66–68. [Google Scholar] [CrossRef] [PubMed]
- Sabermoghaddam, M.; Sarbaz, M.; Lashkardoost, H.; Kaviani, A.; Eslami, S.; Rezazadeh, J. Incidence of occupational exposure to blood and body fluids and measures taken by health care workers before and after exposure in regional hospitals of a developing country: A multicenter study. Am. J. Infect. Control 2015, 43, 1137–1138. [Google Scholar] [CrossRef] [PubMed]
- Türe, Z.; Ulu Kiliç, A.; Cevahir, F.; Altun, D.; Özhan, E.; Alp, E. Predictive factors for percutaneous and mucocutaneous exposure among healthcare workers in a developing country. J. Epidemiol. Glob. Health 2016, 6, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Konlan, K.D.; Aarah-Bapuah, M.; Kombat, J.M.; Wuffele, G.M. The level of nurses’ knowledge on occupational post exposure to Hepatitis B infection in the Tamale metropolis, Ghana. BMC Health Serv. Res. 2017, 17, 1–7. [Google Scholar] [CrossRef]
- Matsubara, C.; Sakisaka, K.; Sychareun, V.; Phensavanh, A.; Ali, M. Prevalence and risk factors of needle stick and sharp injury among tertiary hospital workers, Vientiane, Lao PDR. J. Occup. Health 2017, 59, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Geberemariyam, B.S.; Donka, G.M.; Wordofa, B. Assessment of knowledge and practices of healthcare workers towards infection prevention and associated factors in healthcare facilities of West Arsi District, Southeast Ethiopia: A facility-based cross-sectional study. Arch. Public Health 2018, 76, 69. [Google Scholar] [CrossRef] [PubMed]
- Mandić, B.; Mandić-Rajčević, S.; Marković-Denić, L.; Bulat, P. Occupational exposure to blood and bodily fluids among healthcare workers in Serbian general hospitals. Arh. Hig. Rada Toksikol. 2018, 69, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Hebo, H.J.; Gemeda, D.H.; Abdusemed, K.A. Hepatitis B and C viral infection: Prevalence, knowledge, attitude, practice, and occupational exposure among healthcare workers of Jimma University Medical Center, southwest Ethiopia. Sci. World J. 2019, 2019, 11. [Google Scholar] [CrossRef]
- Lien, L.T.; Hang, N.T.L.; Kobayashi, N.; Yanai, H.; Toyota, E.; Sakurada, S.; Huu Thuong, P.; Cuong, V.C.; Nanri, A.; Mizoue, T.; et al. Prevalence and risk factors for tuberculosis infection among hospital workers in Hanoi, Viet Nam. PLoS ONE 2009, 4, e6798. [Google Scholar] [CrossRef]
- Mathew, A.; David, T.; Thomas, K.; Kuruvilla, P.J.; Balaji, V.; Jesudason, M.V.; Samuel, P. Risk factors for tuberculosis among health care workers in South India: A nested case-control study. J. Clin. Epidemiol. 2013, 66, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Wei, Z.; Yang, M.; Quan, B.; Wang, Y.; Wu, Y.; Ji, B. Prevalence of latent tuberculosis infection among healthcare workers in China as detected by two interferon-gamma release assays. J. Hosp. Infect. 2013, 84, 323–325. [Google Scholar] [CrossRef]
- Whitaker, J.; Mirtskhulava, V.; Kipiani, M.; Harris, D.; Tabagari, N.; Kempker, R.; Blumberg, H. Prevalence and incidence of latent tuberculosis infection in Georgian healthcare workers. PLoS ONE 2013, 8, e58202. [Google Scholar] [CrossRef]
- Tudor, C.; Van der Walt, M.; Margot, B.; Dorman, S.E.; Pan, W.K.; Yenokyan, G.; Farley, J.E. Tuberculosis among health care workers in KwaZulu-Natal, South Africa: A retrospective cohort analysis. BMC Public Health 2014, 14, 891. [Google Scholar] [CrossRef]
- El-Sokkary, R.; Abu-Taleb, A.; El-Seifi, O.; Zidan, H.; Mortada, E.; El-Hossary, D.; Farag, S. Assessing the prevalence of latent tuberculosis among health care providers in Zagazig city, Egypt using Tuberculin skin test and Quantiferon-TB gold in-tube test. Cent. Eur. J. Public Health 2015, 23, 324–330. [Google Scholar] [PubMed]
- Tudor, C.; Van der Walt, M.L.; Margot, B.; Dorman, S.E.; Pan, W.K.; Yenokyan, G.; Farley, J.E. Occupational risk factors for tuberculosis among healthcare workers in KwaZulu-Natal, South Africa. Clin. Infect. Dis. 2016, 62, S255–S261. [Google Scholar] [CrossRef]
- He, W.; Chen, B.-D.; Lv, Y.; Zhou, Z.; Xu, J.-P.; Lv, P.-X.; Zhou, X.-H.; Ning, F.-G.; Li, C.-H.; Wang, D.-P. Use of low-dose computed tomography to assess pulmonary tuberculosis among healthcare workers in a tuberculosis hospital. Infect. Dis. Poverty 2017, 6, 68. [Google Scholar] [CrossRef]
- Erawati, M.; Andriany, M. The prevalence and demographic risk factors for latent tuberculosis infection (LTBI) among healthcare workers in Semarang, Indonesia. J. Multidiscip. Healthc. 2020, 13, 197–206. [Google Scholar] [CrossRef]
- Kisa, A.; Dziegielewski, S.F.; Ates, M. Sexual harassment and its consequences: A study within Turkish hospitals. J. Health Soc. Policy 2002, 15, 77–94. [Google Scholar] [CrossRef] [PubMed]
- Kamchuchat, C.; Chongsuvivatwong, V.; Oncheunjit, S.; Yip, T.W.; Sangthong, R. Workplace violence directed at nursing staff at a general hospital in Southern Thailand. J. Occup. Health 2008, 50, 201–207. [Google Scholar] [CrossRef]
- Aydin, B.; Kartal, M.; Midik, O.; Buyukakkus, A. Violence against general practitioners in Turkey. J. Interpers. Violence 2009, 24, 1980–1995. [Google Scholar] [CrossRef] [PubMed]
- Gimeno, D.; Barrientos-Gutiérrez, T.; Burau, K.D.; Felknor, S.A. Safety climate and verbal abuse among public hospital-based workers in Costa Rica. Work 2012, 42, 29–38. [Google Scholar] [CrossRef]
- Atan, Ş.U.; Baysan Arabaci, L.; Sirin, A.; Isler, A.; Donmez, S.; Unsal Guler, M.; Oflaz, U.; Yalcinkaya Ozdemir, G.; Yazar Tasbasi, F. Violence experienced by nurses at six university hospitals in T urkey. J. Psychiatr. Ment. Health Nurs. 2013, 20, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Khademloo, M.; Moonesi, F.S.; Gholizade, H. Health care violence and abuse towards nurses in hospitals in north of Iran. Glob. J. Health Sci. 2013, 5, 211–216. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Da Silva, A.T.C.; Peres, M.F.T.; de Souza Lopes, C.; Schraiber, L.B.; Susser, E.; Menezes, P.R. Violence at work and depressive symptoms in primary health care teams: A cross-sectional study in Brazil. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1347–1355. [Google Scholar] [CrossRef]
- Baig, L.A.; Shaikh, S.; Polkowski, M.; Ali, S.K.; Jamali, S.; Mazharullah, L.; Soomro, M.; Kumari, B.; Memon, S.; Maheshwari, G. Violence against health care providers: A mixed-methods study from Karachi, Pakistan. J. Emerg. Med. 2018, 54, 558–566. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Xie, F.; Wang, J.; Shi, Y.; Zhang, S.; Han, X.; Sun, Z.; Shi, L.; Li, Z.; Mu, H.; et al. Prevalence of workplace violence against Chinese nurses and its association with mental health: A cross-sectional survey. Arch. Psychiatr. Nurs. 2018, 32, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Abate, A.; Abebaw, D.; Birhanu, A.; Zerihun, A.; Assefa, D. Prevalence and associated factors of violence against hospital staff at Amanuel Mental Specialized Hospital in Addis Ababa, Ethiopia. Psychiatry J. 2019, 2019, 11. [Google Scholar] [CrossRef]
- Yenealem, D.G.; Woldegebriel, M.K.; Olana, A.T.; Mekonnen, T.H. Violence at work: Determinants & prevalence among health care workers, northwest Ethiopia: An institutional based cross sectional study. Ann. Occup. Environ. Med. 2019, 31, 8. [Google Scholar]
- Hacer, T.Y.; Ali, A. Burnout in physicians who are exposed to workplace violence. J. Forensic Leg. Med. 2020, 69, 101874. [Google Scholar] [CrossRef]
- Ashkar, K.; Romani, M.; Musharrafieh, U.; Chaaya, M. Prevalence of burnout syndrome among medical residents: Experience of a developing country. Postgrad. Med. J. 2010, 86, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Ayala, E.; Carnero, A.M. Determinants of burnout in acute and critical care military nursing personnel: A cross-sectional study from Peru. PLoS ONE 2013, 8, e54408. [Google Scholar] [CrossRef]
- Zubairi, A.J.; Noordin, S. Factors associated with burnout among residents in a developing country. Ann. Med. Surg. 2016, 6, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Colindres, C.V.; Bryce, E.; Coral-Rosero, P.; Ramos-Soto, R.M.; Bonilla, F.; Yassi, A. Effect of effort-reward imbalance and burnout on infection control among Ecuadorian nurses. Int. Nurs. Rev. 2018, 65, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.A.; Shamim, M.H.; Ali, L.; Taqi, A. Evaluation of job stress and burnout among anesthesiologists working in academic institutions in 2 major cities in Pakistan. Anesth. Analg. 2019, 128, 789–795. [Google Scholar] [CrossRef]
- Mumbwe, M.C.; McIsaac, D.; Jarman, A.; Bould, M.D. A cross-sectional survey to determine the prevalence of burnout syndrome among anesthesia providers in Zambian hospitals. Anesth. Analg. 2020, 130, 310–317. [Google Scholar] [CrossRef]
- Li, J.; Fu, H.; Hu, Y.; Shang, L.; Wu, Y.; Kristensen, T.S.; Mueller, B.H.; Hasselhorn, H.M. Psychosocial work environment and intention to leave the nursing profession: Results from the longitudinal Chinese NEXT study. Scand. J. Public Health 2010, 38, 69–80. [Google Scholar] [CrossRef]
- Ayamolowo, S.J.; Irinoye, O.; Oladoyin, M.A. Job satisfaction and work environment of primary health care nurses in Ekiti State, Nigeria: An exploratory study. Int. J. Caring Sci. 2013, 6, 531–542. [Google Scholar]
- Ogunlade, O.; Ogunfowokan, A. Clinical nurses’ satisfaction with night shift in selected hospitals in Ile-Ife, Osun state, Nigeria. Int. J. Caring Sci. 2014, 7, 129–139. [Google Scholar]
- Ayalew, E.; Workineh, Y. Job satisfaction and associated factors among nurses in Bahir Dar city administrative, North West Ethiopia, 2017. BMC Res. Notes 2019, 12, 319. [Google Scholar] [CrossRef]
- Smith, D.R.; Wei, N.; Zhao, L.; Wang, R.-S. Musculoskeletal complaints and psychosocial risk factors among Chinese hospital nurses. Occup. Med. 2004, 54, 579–582. [Google Scholar] [CrossRef] [PubMed]
- Tezel, A. Musculoskeletal complaints among a group of Turkish nurses. Int. J. Neurosci. 2005, 115, 871–880. [Google Scholar] [CrossRef]
- Fabunmi, A.A.; Oworu, J.O.; Odunaiya, N.A. Prevalence of musculoskeletal disorders among nurses in University College Hospital, Ibadan. West Afr. J. Nurs. 2008, 19, 21–25. [Google Scholar]
- De Castro, A.B.; Cabrera, S.L.; Gee, G.C.; Fujishiro, K.; Tagalog, E.A. Occupational health and safety issues among nurses in the Philippines. Workplace Health Saf. 2009, 57, 149–157. [Google Scholar]
- Karahan, A.; Kav, S.; Abbasoglu, A.; Dogan, N. Low back pain: Prevalence and associated risk factors among hospital staff. J. Adv. Nurs. 2009, 65, 516–524. [Google Scholar] [CrossRef]
- Mehrdad, R.; Dennerlein, J.T.; Haghighat, M.; Aminian, O. Association between psychosocial factors and musculoskeletal symptoms among Iranian nurses. Am. J. Ind. Med. 2010, 53, 1032–1039. [Google Scholar] [CrossRef]
- Tinubu, B.M.S.; Mbada, C.E.; Oyeyemi, A.L.; Fabunmi, A.A. Work-Related Musculoskeletal Disorders among Nurses in Ibadan, South-west Nigeria: A cross-sectional survey. BMC Musculoskelet. Disord. 2010, 11, 12. [Google Scholar] [CrossRef] [PubMed]
- Arsalani, N.; Fallahi-Khoshknab, M.; Josephson, M.; Lagerström, M. Musculoskeletal disorders and working conditions among Iranian nursing personnel. Int. J. Occup. Saf. Ergon. 2014, 20, 671–680. [Google Scholar] [CrossRef]
- Barzideh, M.; Choobineh, A.R.; Tabatabaee, H.R. Job stress dimensions and their relationship to musculoskeletal disorders in Iranian nurses. Work 2014, 47, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Munabi, I.G.; Buwembo, W.; Kitara, D.L.; Ochieng, J.; Mwaka, E.S. Musculoskeletal disorder risk factors among nursing professionals in low resource settings: A cross-sectional study in Uganda. BMC Nurs. 2014, 13, 7. [Google Scholar] [CrossRef]
- Yasobant, S.; Rajkumar, P. Work-related musculoskeletal disorders among health care professionals: A cross-sectional assessment of risk factors in a tertiary hospital, India. Indian J. Occup. Environ. Med. 2014, 18, 75–81. [Google Scholar] [CrossRef]
- Abaraogu, U.O.; Ezema, C.I.; Nwosu, C.K. Job stress dimension and work-related musculoskeletal disorders among southeast Nigerian physiotherapists. Int. J. Occup. Saf. Ergon. 2017, 23, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Amin, N.A.; Quek, K.F.; Oxley, J.A.; Noah, R.; Nordin, R. Emotional distress as a predictor of work-related musculoskeletal disorders in Malaysian nursing professionals. Int. J. Occup. Environ. Med. 2018, 9, 69–78. [Google Scholar] [CrossRef]
- Dlungwane, T.; Voce, A.; Knight, S. Prevalence and factors associated with low back pain among nurses at a regional hospital in KwaZulu-Natal, South Africa. Health SA Gesondheid 2018, 23, a1028. [Google Scholar] [CrossRef] [PubMed]
- Ike, E.; Olawumi, J. The prevalence, risk factors and coping measures of back pain among nurses in Federal Medical Centre, Abeokuta, Ogun state, Nigeria. Int. J. Caring Sci. 2018, 11, 955–968. [Google Scholar]
- Luan, H.D.; Hai, N.T.; Xanh, P.T.; Giang, H.T.; Thuc, P.V.; Hong, N.M.; Khue, P.M. Musculoskeletal disorders: Prevalence and associated factors among district hospital nurses in Haiphong, Vietnam. Biomed. Res. Int. 2018, e1–e9. [Google Scholar] [CrossRef]
- Dong, H.; Zhang, Q.; Liu, G.; Shao, T.; Xu, Y. Prevalence and associated factors of musculoskeletal disorders among Chinese healthcare professionals working in tertiary hospitals: A cross-sectional study. BMC Musculoskelet. Disord. 2019, 20, 175. [Google Scholar] [CrossRef] [PubMed]
- Baykal, U.; Seren, S.; Sokmen, S. A description of oncology nurses’ working conditions in Turkey. Eur. J. Oncol. Nurs. 2009, 13, 368–375. [Google Scholar] [CrossRef]
- Agrawal, A.; Bhatt, N.; Kk, S.; Singh, K.; Chaudhary, H.; Asawa, K. Prevalence of allergy to latex gloves among dental professionals in Udaipur, Rajasthan, India. Oral Health Prev. Dent. 2010, 8, 345–350. [Google Scholar]
- Amarasekera, M.; Rathnamalala, N.; Samaraweera, S.; Jinadasa, M. Prevalence of latex allergy among healthcare workers. Int. J. Occup. Med. Environ. Health 2010, 23, 391–396. [Google Scholar] [CrossRef]
- Phaswana, S.M.; Naidoo, S. The prevalence of latex sensitisation and allergy and associated risk factors among healthcare workers using hypoallergenic latex gloves at King Edward VIII Hospital, KwaZulu-Natal South Africa: A cross-sectional study. BMJ Open 2013, 3, e002900. [Google Scholar] [CrossRef][Green Version]
- Supapvanich, C.; Povey, A.C.; de Vocht, F. Respiratory and dermal symptoms in Thai nurses using latex products. Occup. Med. 2013, 63, 425–428. [Google Scholar] [CrossRef][Green Version]
- Köse, S.; Mandiracioğlu, A.; Tatar, B.; Gül, S.; Erdem, M. Prevalence of latex allergy among healthcare workers in Izmir (Turkey). Cent. Eur. J. Public Health 2014, 22, 262–265. [Google Scholar] [CrossRef][Green Version]
- Supapvanich, C.; Povey, A.; de Vocht, F. Latex sentization and risk factors in female nurses in Thai governmental hospitals. Int. J. Occup. Med. Environ. Health 2014, 27, 93–103. [Google Scholar] [CrossRef]
- Abbasi, K.; Hazrati, M.; Mohammadbeigi, A.; Ansari, J.; Sajadi, M.; Hosseinnazzhad, A.; Moshiri, E. Protection behaviors for cytotoxic drugs in oncology nurses of chemotherapy centers in Shiraz hospitals, South of Iran. Indian J. Med. Paediatr. Oncol. 2016, 37, 227–231. [Google Scholar]
- Elshaer, N. Adverse health effects among nurses and clinical pharmacists handling antineoplastic drugs: Adherence to exposure control methods. J. Egypt. Public Health Assoc. 2017, 92, 144–155. [Google Scholar] [CrossRef]
- Alehashem, M.; Baniasadi, S. Important exposure controls for protection against antineoplastic agents: Highlights for oncology health care workers. Work 2018, 59, 165–172. [Google Scholar] [CrossRef]
- Bayraktar-Ekincioglu, A.; Korubük, G.; Demirkan, K. An evaluation of chemotherapy drug preparation process in hospitals in Turkey—A pilot study. J. Oncol. Pharm. Pract. 2018, 24, 563–573. [Google Scholar] [CrossRef] [PubMed]
- Aluko, O.O.; Adebayo, A.E.; Adebisi, T.F.; Ewegbemi, M.K.; Abidoye, A.T.; Popoola, B.F. Knowledge, attitudes and perceptions of occupational hazards and safety practices in Nigerian healthcare workers. BMC Res. Notes 2016, 9, 71. [Google Scholar] [CrossRef]
- Tait, F.N.; Mburu, C.; Gikunju, J. Occupational safety and health status of medical laboratories in Kajiado County, Kenya. Pan Afr. Med. J. 2018, 29, 65–81. [Google Scholar] [PubMed]
- Lee, R. Occupational transmission of bloodborne diseases to healthcare workers in developing countries: Meeting the challenges. J. Hosp. Infect. 2009, 72, 285–291. [Google Scholar] [CrossRef]
- Garner, J.S. Guideline for isolation precautions in hospitals. Infect. Cont. Hosp. Epidemiol. 1996, 17, 54–80. [Google Scholar] [CrossRef]
- Menzies, D.; Joshi, R.; Pai, M. Risk of tuberculosis infection and disease associated with work in health care settings. Int. J. Tuberc. Lung Dis. 2007, 11, 593–605. [Google Scholar]
- Jesudas, C.D.; Thangakunam, B. Tuberculosis risk in health care workers. Indian J. Chest Dis. Allied Sci. 2013, 55, 149–154. [Google Scholar]
- Lanctôt, N.; Guay, S. The aftermath of workplace violence among healthcare workers: A systematic literature review of the consequences. Aggress. Violent Behav. 2014, 19, 492–501. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory Manual, 4th ed.; Mind Garden Inc.: Menlo Park, CA, USA, 2016. [Google Scholar]
- McHugh, M.D.; Kutney-Lee, A.; Cimiotti, J.P.; Sloane, D.M.; Aiken, L.H. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff. 2011, 30, 202–210. [Google Scholar] [CrossRef]
- World Health Organization. Health Workforce Requirements for Universal Coverage and the Sustainable Development Goals; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Andersson, G.B. Epidemiological features of chronic low-back pain. Lancet 1999, 354, 581–585. [Google Scholar] [CrossRef]
- Vieira, E.R.; Schneider, P.; Guidera, C.; Gadotti, I.C.; Brunt, D. Work-related musculoskeletal disorders among physical therapists: A systematic review. J. Back Musculoskelet. Rehabil. 2016, 29, 417–428. [Google Scholar] [CrossRef]
- Epstein, S.; Sparer, E.H.; Tran, B.N.; Ruan, Q.Z.; Dennerlein, J.T.; Singhal, D.; Lee, B.T. Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: A systematic review and meta-analysis. JAMA Surg. 2018, 153, e174947. [Google Scholar] [CrossRef]
- Sakzewski, L.; Naser-ud-Din, S. Work-related musculoskeletal disorders in dentists and orthodontists: A review of the literature. Work 2014, 48, 37–45. [Google Scholar] [CrossRef]
- McDiarmid, M.A. Advocating for the health worker. Ann. Glob. Health 2019, 85, 16. [Google Scholar] [CrossRef]


| Authors | Year | Topic | Origin | Participants | Type of Study | Methods | Findings |
|---|---|---|---|---|---|---|---|
| I. Bloodborne Pathogens | |||||||
| Cavalcante et al. [27] | 1991 | Occupational risk of acquiring HIV | Brazil | 651 health care workers from a teaching hospital | Prospective | Health care workers who reported accidental exposures to infective material from AIDS patients to the Infection Control Committee (n = 247) and those who had other risks of infection but no occupational exposures (n = 404) were interviewed and blood was collected for HIV testing at baseline, 90, 180 and 360 days later (for health care workers who reported accidents). | 247 health care workers reported 338 accidents and of these 115 were followed up for more than 6 months and 132 were lost to follow up. None tested positive for HIV. 50% of exposures occurred through needlestick or sharp injuries, 22% through contact of blood on mucous membranes, 28% through exposures to urine, faeces or cerebrospinal fluid from AIDs patients. The highest frequencies of injuries were reported by nurses, followed by physicians, laundry and housekeeping personnel and laboratory workers. Of the 404 health care workers with no occupational exposures, 6 were positive and had confirmed risk factors for HIV transmission. |
| Adegboye et al. [28] | 1994 | Needlestick and sharp object injuries and accidents; awareness of the risk of occupational exposure to HIV | Nigeria | 474 health care workers working in a university hospital complex, who were occupationally exposed to blood | Cross-sectional | Questionnaires on needlestick and sharp injuries in the past year and on knowledge on HIV transmission. | 27% of health care workers reported at least one needlestick injury in the past year. Circumstances resulting in needlestick injuries were unexpected patient movement (29%), handling or disposal of used needles (23%), needle recapping (18%), accidental stick by a colleague (18%), and needle disassembly (10%). 15% reported at least one sharp object injury in the past year and this most commonly involved broken glass from patient specimen containers (39%).The highest frequencies of injuries were reported by dental staff and surgeons. Almost all participants were aware of the risk of occupational exposure to HIV. |
| Olubuyide [29] | 1996 | Contact with HIV and Hepatitis B (HBV)-positive patients and needlestick injuries | Nigeria | 149 resident doctors in a teaching hospital in Nigeria | Cross-sectional | Questionnaire asking about contact with HIV/HBV patients, needlestick injuries, and precautions used. No time period was reported. | 93% reported contact with HIV/HBV patients, 9% had needlestick injuries (presumably lifetime) and 54% used universal precautions when performing procedures. |
| Gumodoka et al. [30] | 1997 | Injuries and use of personal protective equipment (PPE) to protect from HIV | United Republic of Tanzania | 403 health care workers from nine hospitals in the Mwanza region | Mixed methods | Questionnaires on the use of PPE and needlestick injuries and splashes. Observations and interviews were carried out in different sections of the hospitals to determine general hygiene practices. | Prick and splash incidents were reported frequently (at least 5 pinprick accidents and nine splashes per health care worker per year). The general hygiene measures to reduce the risk of HIV was not sufficient and PPE was not used consistently. |
| Khuri-Bulos et al. [31] | 1997 | Needlestick and sharp injuries | Jordan | 248 health care workers working in a tertiary care hospital | Prospective | Surveillance of sharps injuries over a 3 year period. Health care workers who reported sharps injuries during this period completed a questionnaire. Serum samples were collected at baseline and 6 months later to be tested for Hepatitis B, C and HIV. | Over the 3 year period, 248 health care workers reported needlestick injuries. Highest frequencies were reported by nurses (34.6%). The total average annual rate was 82:1000 health care workers per year. Only a minority of health care workers submitted a serum sample. |
| Gounden and Moodley [32] | 2000 | Injuries and use of personal protective equipment to protect from HIV | South Africa | 265 health care workers from a tertiary care hospital | Mix of retrospective and prospective | Health care workers were interviewed over a period of one year. | 13% reported accidental injuries with HIV-positive patients. The highest frequencies of injuries were among registrars. Compliance with universal precautions was suboptimal. 48% of the participants on post-exposure prophylaxis (PEP) did not complete their regimen; the side effects of PEP was reported as the main reason for discontinuation. |
| Phipps et al. [33] | 2002 | Needlestick injuries; and knowledge, attitudes and practices | China | 441 nurses working in 3 tertiary care hospitals in Hunan Province | Cross-sectional | Questionnaire on needlestick injuries in the past year, Hepatitis B knowledge and immunization status, and work practices. | 82% of the nurses reported experiencing a needlestick injury in the past year. These injuries occurred most frequently when separating a needle and syringe, recapping a needle, transporting needles for disposal, and giving injections. Only 8% reported the injuries to an authority. The majority never wore gloves when drawing blood, giving an injection or starting an intravenous line. 29% were not vaccinated against Hepatitis B. |
| Talaat et al. [34] | 2003 | Needlestick injuries and Hepatitis B vaccination status | Egypt | 1485 health care workers from health facilities in 2 governorates (Nile Delta and Upper Egypt) | Cross-sectional | Questionnaire on needlestick injuries and Hepatitis B vaccination status. | 36.6% reported at least one needlestick injury in the past 3 months. Two-hand recapping was the most common behaviour associated with needlestick injury. 15.8% reported being fully vaccinated against Hepatitis B; vaccination rates were lowest among housekeeping personnel. |
| Kermode et al. [35] | 2005 | Needlestick injuries | India | 266 health care workers from 7 rural health settings (hospitals with attached community health projects) in north India | Cross-sectional | Questionnaire on needlestick or sharps injuries in the past week, past year, and over the working lifetime. | 63% reported at least 1 needlestick injury in the last year and 73% over their working lifetime. Doctors and nurses were more likely to be exposed than student nurses and laboratory workers. |
| Kermode et al. [36] | 2005 | Compliance with universal precautions (UP) | India | 266 health care workers from 7 rural health settings (hospitals with attached community health projects) in north India | Cross-sectional | Questionnaire on 12 behaviours related to the practice of UP. | Compliance with UP was not optimal. Compliance with UP was associated with being in the job for a longer period, knowledge of bloodborne pathogen transmission, perceiving fewer barriers to safe practice and strong commitment to workplace safety climate. |
| Nsubuga and Jaakkola [37] | 2005 | Needlestick and sharps injuries and risk factors | Uganda | 526 midwives and nurses in a tertiary care hospital in Kampala | Cross-sectional | Questionnaire on needlestick injuries and risk factors. | 57% reported a needlestick injury in the last year and 82% in their entire career. The risk factors identified were lack of training, working for more than 40 h/week, recapping needles, and not using gloves when handling needles. Lack of training was the strongest predictor. |
| Obi et al. [38] | 2005 | Needlestick injuries and splashes, and use of personal protective equipment (PPE) | Nigeria | 264 surgeons from five tertiary health institutions in Southeast Nigeria | Cross-sectional | Questionnaire on needlestick injuries and splashes in the last 5 years, use of PPE, and attitudes towards care of HIV-infected patients. | 40.2% reported a needlestick injury and 26% reported blood splashes in the past five years. The highest frequencies were reported in resident surgeons. All wore protective aprons, 65.2% used double gloves and 30.3% used goggles during surgical procedures. 83% had some reservations about treating HIV-positive patients. |
| Chelenyane and Endacott [39] | 2006 | Infection control practices | Botswana | 22 health care workers from two referral hospitals emergency departments | Mixed methods | Questionnaire with multiple choice and open ended questions. | The majority of participants reported compliance with universal precautions. Barriers to compliance were lack of appropriate facilities, shortage of equipment and materials, inadequate staffing, and lack of training programs. |
| Akinleye and Omokhodion [40] | 2008 | Needlestick injuries and work practices | Nigeria | 270 primary health care workers from two urban and three rural local government areas | Cross-sectional | Questionnaire on needlestick injuries in the past year and work practices. | 32% reported a needlestick injury in the past year. Compliance with the use of gloves and hand washing were greater among rural than urban health workers. |
| Okeke et al. [41] | 2008 | Needlestick injuries and Hepatitis B vaccination status | Nigeria | 346 medical students in a tertiary institute | Cross-sectional | Questionnaire on needlestick injuries and splashes, and Hepatitis B vaccination status | 48% reported a previous needlestick injury and 27.7% reported being vaccinated against Hepatitis B. |
| Taegtmeyer et al. [42] | 2008 | Needlestick injuries (NSIs) and safety practices | Kenya | 650 health care workers from 11 health facilities in Thika District | Prospective | Questionnaires and semi-structured interviews; together with an intervention of introduction of biosafety measures, vaccination, and post-exposure prophylaxis (PEP). Surveys were conducted at baseline and at one year. | The incidence of NSIs was 0.97 per health care worker per year. After the institution of biosafety measures, there was a significant reduction in injuries, an increase in the health care workers accessing HIV testing and in the uptake of Hepatitis B vaccination uptake, but the uptake of PEP was low. |
| Chen et al. [43] | 2009 | Sharp object injuries | China | 831 health care workers from 9 hospitals in Fujian, who worked in departments with a high risk of occupational exposures to blood | Cross-sectional | Questionnaire on sharp object injuries in the past year. | 86.2% of the health care workers reported a sharps injury on the job and 71.3% said that it had occurred in the past year. Nurses reported the highest frequencies of injuries, followed by surgeons, anaesthetists, and laboratory workers. Disposable syringes caused most of the injuries. |
| Simon [44] | 2009 | Needlestick injuries | India | 50 nurses in a super-speciality tertiary care hospital in Delhi | Cross-sectional | Questionnaire on needlestick injuries, and knowledge and practices on needlestick injuries. | 70% had sustained a needlestick injury during their career, and of these the majority (71%) did not report it. There was a lack of awareness on prevention and management of NSIs. |
| Chakravarthy et al. [45] | 2010 | Sharps injuries, and blood and body fluid exposure incidents | India | 265 health care workers who reported sharps injuries and accidental blood and body fluid exposures to the Infection Control Committee of 4 tertiary referral hospitals | Retrospective review of data from sharp injury, and blood and body fluid exposure reports | Data were obtained from sharps injuries, and blood and body fluid exposures reports that were reported to the Infection Control Committees of the 4 hospitals. Data collection period ranged from 6 to 26 months. | 243 sharps injuries and 22 incidents of blood and body fluids exposures were reported in the cumulated 50 months of study. The highest frequencies of injuries were reported by nurses and housekeeping staff. The majority of the injuries were caused by disposable needles. |
| Yacoub et al. [46] | 2010 | Needlestick injuries and Hepatitis B vaccination status | Syria | 321 health care workers from three tertiary care hospitals in Aleppo | Cross-sectional | Questionnaire on needlestick injuries and Hepatitis B vaccination status. Blood was collected to test for Hepatitis B (HBsAg). | 76.6% reported at least one needlestick injury in the past year. Anaesthesiology technicians, doctors, nurses, and housekeeping had the greatest exposure risks. 56.1% reported being fully vaccinated against Hepatitis B; vaccination rates were lowest among housekeeping personnel. 2.8% tested positive for HBsAg. |
| Sangwan et al. [47] | 2011 | Needlestick injuries and splashes | India | 70 health care workers in a tertiary care hospital | Cross-sectional | Questionnaire on needlestick injuries and splashes in the past year, and reasons for not using PPE. | 71.43% reported a needlestick injury in the past year. The most frequent reasons for not using PPE were in emergencies and other co-workers not using them. Only 34% reported that adequate PPE was always provided. |
| Irmak [48] | 2012 | Needlestick and sharps injuries | Turkey | 143 nurses working patient care in a state hospital | Cross-sectional | Questionnaire on needlestick and sharps injuries in the past year. | 30.1% of the nurses reported at least one sharp object injury in the past year. The use of syringe needles was the most common cause of injury. 16.3% of the nurses were not wearing gloves when they sustained the injury. |
| Nasim et al. [49] | 2012 | Safe work practices and use of personal protective equipment | Pakistan | 1782 laboratory technicians from public sector hospitals and private hospital laboratories throughout Pakistan | Cross-sectional | Questionnaire on safe and unsafe work practices, and the use of personal protective equipment. | 31.9% did not use any kind of personal protective equipment, 46% reported reusing syringes, 43.2% regularly recapped needles after use, 67.2% said that standard operating procedures were not available, and 84.2% had no formal biosafety training. |
| Omorogbe et al. [50] | 2012 | Injection safety practices and use of PPE | Nigeria | 122 nurses from 6 mission hospitals in Benin city | Cross-sectional | Questionnaire adapted from the WHO injection safety assessment tool and observation of practices. | 55.8% reported recapping of needles and only 3.3% said that they regularly used gloves when giving injections. |
| Phillips et al. [51] | 2012 | Needlestick and sharps injuries | Zambia | 442 health care workers from five health facilities in Lusaka and Livingstone | Cross-sectional | Questionnaire on needlestick and sharps injuries in the past year. | The annual average sharps injury rate was 1.3 injuries/worker. The highest frequencies were reported by nurses and service workers. Syringe needles accounted for the majority of the injuries. 88% reported the availability of PPE, but only 8% were fully vaccinated against Hepatitis B. |
| Sethi et al. [52] | 2012 | Compliance with infection control practices | Uganda | 183 health care workers from a referral hospital in Kampala | Cross-sectional | Questionnaire on hand hygiene, barrier protection, and contact precautions. | 68.9% reported using gloves as barrier protection. Universal precautions were not always followed. The reasons for suboptimal infection control practices were lack of time and lack of resources. |
| Abkar et al. [53] | 2013 | Unsafe injection practices | Yemen | 127 health care workers from two hospitals and 6 rural health centres | Cross-sectional | Questionnaire and observation of injection practices. | There were several unsafe practices, particularly the recapping of needles after use, which occurred in 61.1% and 36.8% of the observations in the hospitals and health centres, respectively. |
| Afridi et al. [54] | 2013 | Needlestick injuries, Hepatitis B vaccination status and infection control measures | Pakistan | 497 health care workers from two tertiary care hospitals in Karachi | Cross-sectional | Questionnaire on needlestick injuries, Hepatitis B vaccination status and infection control measures. | 64% reported needlestick injuries during their career. Working for more than 5 years and working as a nurse were the factors associated with an increased risks. Injecting medicine, drawing blood, and two hand recapping of needles were the practices associated with needlestick injuries. 34% reported being vaccinated against Hepatitis B. Infection control measures were inadequate. |
| Rajkumari et al. [55] | 2014 | Needlestick injuries and splashes | India | 356 health care workers who reported sharps injuries and splashes in a tertiary hospital in New Delhi | Prospective | Surveillance of sharps injuries over a 2 years 5 months period. Health care workers who reported sharps injuries during this period completed a questionnaire. Blood samples were collected at baseline and 6 months later to be tested for Hepatitis B, C and HIV. | Highest frequencies of sharps injuries were reported by doctors (36.2%), followed by nurses (14.6%) and hospital waste disposal staff (7.6%). There was no seroconversion among the exposed health care workers. The majority (85.1%) of the injuries reported were from sharps (as compared to splashes). Only 55.3% were using PPE during the time of exposure. |
| Bekele et al. [56] | 2015 | Needlestick injury reporting and attitudes | Ethiopia | 340 health care workers from four hospitals of Bale zone | Cross-sectional | Questionnaire on needlestick injury reporting and attitudes. | 98.2% were aware of the risks of needlestick injuries.58.7% of needlestick injuries were not reported. The main reasons for not reporting were time constraints, sharps that caused the injury were not used by patients, the source patient did not have diseases of concern, and lack of knowledge of reporting. |
| Priya et al. [57] | 2015 | Needlestick injuries and splashes | India | 105 health care workers who reported sharps injuries and accidental blood and body fluid exposures to the anti-retroviral therapy centre of a tertiary care hospital | Retrospective review of data from sharp injury, and blood and body fluid exposure reports | Data from three years were obtained from sharps injuries, and blood and body fluid exposures reports that were reported to the Anti-retroviral therapy centre of a tertiary care hospital. | 105 health care workers reported an occupational exposure to blood and body fluids. The highest frequencies were reported by interns. Needlestick injuries were the commonest type of exposure (85%), followed by mucous membrane splash (13%) and exposure on intact skin (2%). The practices that resulted in exposures were blood withdrawal (45.7%), during surgical procedures (24.7%) and disposal of sharps (23%). |
| Sabermoghaddam et al. [58] | 2015 | Needlestick injuries and splashes | Iran | 371 health care workers from 6 government hospitals in the Northern Khorasan province | Cross-sectional | Questionnaire on needlestick injuries and splashes in the past year. | 44% reported a sharp object injury and 31% reported contact with blood and body fluids in the past year. 91% reported always using a safety box to deposit used needles, 35.9% reported washing their hands before and after examining patients, 41.5% reported using gloves, 58% had attended training on safe handling of sharps. 52% of those who were injured did not report the injury. |
| Türe et al. [59] | 2016 | Needlestick injuries and splashes, and risk factors | Turkey | 166 health care workers who reported sharps injuries and accidental blood and body fluid exposures to the Infection Control Committee of a tertiary care hospital | Retrospective review of data from sharp injuries, and blood and body fluid exposure reports | Data were obtained from sharps injuries, and blood and body fluid exposure reports that were reported to the Infection Control Committee. Data collection period was from August 2011 to June 2013. | 166 health care workers reported an occupational exposure to blood and body fluids. The occupational exposure incidence was 2.18 exposures/person-year. The highest frequencies of injuries were reported by nurses and cleaning staff. Having heavy workloads and long working hours increased the risk of exposures whereas increased work experience decreased the risk of exposures. |
| Konlan et al. [60] | 2017 | Hepatitis B vaccination status and practices to reduce occupational exposures | Ghana | 108 nurses from two hospitals within the Tamale metropolis | Cross-sectional | Questionnaire on Hepatitis B vaccination status and practices to reduce occupational exposures to Hepatitis B. | 64.8% said that they reported occupational exposures to Hepatitis B. 33.3% reported receiving 3 doses of Hepatitis B vaccination. Compliance with precautions to reduce occupational exposures was suboptimal. |
| Matsubara et al. [61] | 2017 | Needlestick and sharps injuries and risk factors | Lao PDR | 623 health care workers from 4 tertiary care hospitals in Vientiane Capital | Cross-sectional | Questionnaire on needlestick injuries over their entire career, and in the past 6 months, and injection practices based on the World Health Organization questionnaire on injection practices. | 11.4% reported a needlestick injury in the past 6 months and 42.1% in their entire career. The highest frequencies were reported by surgeons, dentists and cleaners. The injuries were caused by percutaneous injections (17.9%), suturing needles (17.0%), intravenous line insertion (17.0%), recapping needles (13.2%), disposal (10.4%), and others (24.5%). Protective factors for needlestick injuries identified were adequate availability of needles and syringes, and adequate training. |
| Geberemariyam et al. [62] | 2018 | Needlestick injures and infection control practices | Ethiopia | 648 health care workers with direct involvement in patient care in public health care facilities in one district | Cross-sectional | Questionnaire on needlestick injuries and infection control practices. | Only 36.3% reported safe infection prevention practices. Life-time prevalence of needlesticks and blood or body fluid exposure 32.4% and 39.0%, respectively, with 24.8% of them having >1 injuries. Exposures occurred mostly during intravenous catheter insertion, suturing, and recapping of needles. Factors associated with better infection control practices were profession, service years, presence of infection prevention committee and guideline, and ever taking training. |
| Mandić et al. [63] | 2018 | Needlestick injuries and splashes | Serbia | 5247 health care workers who routinely worked with blood from 17 general hospitals in Serbia | Cross-sectional | Questionnaire on needlestick injuries and splashes over their entire career and in the last year. | 39% reported an exposure to blood and body fluids in the past year and 66% over their entire career. The prevalence of needlestick injuries occurring in the last year was equal among genders, but it was more prevalent in women during the entire career. The highest frequencies were reported in nurses. |
| Hebo et al. [64] | 2019 | Exposure to blood and body fluids, practices of standard precautions and seroprevalance of Hepatitis B and C | Ethiopia | 240 health care workers from Jimma University Medical Center | Cross-sectional | Questionnaires on exposure to blood and body fluids and use of standard precautions. Blood was collected and tested for Hepatitis B and C. | 60% reported being ever exposed and 43% reported exposure in the past year to blood and body fluids through accidental splashes and sharps injuries. 2.5% of the samples was positive for HBsAg and 0.42% for anti-HCV antibodies. Only 42.6% had good practices of standard precautions. |
| II. Tuberculosis (TB) | |||||||
| Lien et al. [65] | 2009 | Prevalence of latent TB and risk factors | Vietnam | 150 health care workers from a TB hospital and 150 from a non-TB hospital in Hanoi | Cross-sectional | Questionnaire on occupational history; interferon-gamma release assay (IGRA), QuantiFERON-TB Gold In-Tube assay and one- and two-step tuberculin skin tests (TSTs) for TB infection. | Prevalence of TB infection was 47.3%, 61.1% and 66.3% as estimated by IGRA, one- and two-step TST, respectively. Working in a TB hospital, increasing age, lower education levels, and higher body mass index were associated with increased risk of IGRA positivity. |
| Mathew et al. [66] | 2013 | TB among health care workers | India | 101 health care workers with TB (cases) and 101 without TB in a tertiary care hospital in Vellore | Nested case–control | Questionnaire on occupational history and non-occupational exposure to TB. | Rate of active pulmonary TB was 314 per 100,000 person-years, which was 1.86 times higher than that of the general population. Body mass index <19 kg/m2, having frequent contact with patients, and working in the medical wards or microbiology laboratories were independently associated with increased risk of TB |
| Wei et al. [67] | 2013 | Prevalence of latent TB infection (LTBI) | China | 210 health care workers in a chest hospital in Harbin | Prospective | Questionnaire on occupational history; participants were tested with two interferon-gamma release assays (QuantiFERON-TB Gold In-Tube assay (GFT-GIT) and A.TB) and TST. Participants were observed for 2 years to check for the development of active tuberculosis. | Prevalence of LTBI was 76.5% by QFT-GIT, 65.7% by A.TB and 97.6% by TST, which was higher than that reported in the general population. Working as a nurse and age > 30 years were independently associated with increased risk of LTBI. |
| Whitaker et al. [68] | 2013 | Prevalence and risk of latent TB infection (LTBI) | Georgia | 319 health care workers in Georgia | Prospective longitudinal | Questionnaire, and tests for LTBI using the TST and QuantiFERON-TB Gold In-Tube Assay (QFT-GIT). The tests were repeated 6–26 months after baseline. | Prevalence at baseline was 67% by TST and 46% by QFT-GIT. Health care workers (HCWs) working in TB health care facilities had a higher prevalence of positive TST and QTF-GIT. Frequent contact with TB patients was associated with increased risk of QTF-GIT positivity only and increasing age was associated with increased risk of positivity of both tests. The conversions rates were high at 22.8/100 person-years (QTF-GIT) and 17.1/100 person-years (TST). Female HCWs had a decreased risk of TST conversion and older HCWs had an increased risk of QTF-GIT conversion. |
| Tudor et al. [69] | 2014 | TB incidence and risk factors | South Africa | 1313 health care workers from 3 district hospitals in KwaZulu-Natal | Retrospective | Occupational health medical records of 1313 health care workers were reviewed during the period of January 2006 and December 2010. | The TB incidence rate was 1958/100,000 person-years, which was two-fold greater than in the general population. An increased incidence of TB was seen in those working in TB wards, paediatric wards, outpatient departments and stores/workshops. Health care workers living with HIV had a greater incidence of TB. |
| El-Sokkary et al. [70] | 2015 | Latent TB infection (LTBI) prevalence and risk factors | Egypt | 132 health care workers from a chest Hospital in Zagazig city | Cross-sectional | Questionnaire and tests for LTBI using the TST and QuantiFERON-TB Gold In-Tube Assay (QFT-GIT). | Prevalence was 28.8% by QFT-GIT and 59.1% by TST. Being a nurse, working >10 years, smoking and diabetes were significantly associated with risk of LTBI. |
| Tudor et al. [71] | 2016 | Occupational risk factors for TB | South Africa | 145 health care workers (54 cases, 91 controls) from 3 district hospitals in KwaZulu-Natal | Case control | Cases were identified from the occupational health medical records between January 2006 and December 2010. | Health care workers with HIV and those who spent time working in areas with tuberculosis patients were at an increased risk of TB. |
| He et al. [72] | 2017 | Pulmonary tuberculosis status among health care workers as diagnosed with low-dose CT | China | 1012 health care workers from the Beijing Chest Hospital | Retrospective | Health examination data of 1012 health care workers which included low-dose lung CT examinations from January 2012 to November 2015 were analysed. | The incidence and prevalence rates of active TB were >2.8 times and >4.1 times greater than that of the general population of China. The majority (78.9%) of the health care workers with active TB worked in high-risk areas such as TB wards, outpatient clinics and radiology departments. |
| Erawati and Andriany [73] | 2020 | Latent TB infection (LTBI) prevalence and risk factors | Indonesia | 195 health care workers from 34 primary health centres in Semarang | Cross-sectional | Questionnaire and tests for LTBI using QuantiFERON-TB Gold In-Tube Assay (QFT-GIT). | Prevalence of LTBI was 23.6%. Health care workers with comorbidities were at increased risk of LTBI. |
| Authors | Year | Topic | Origin | Participants | Type of Study | Methods | Findings |
|---|---|---|---|---|---|---|---|
| I. Workplace Violence | |||||||
| Kisa et al. [74] | 2002 | Sexual harassment and work productivity | Turkey | 215 nurses from two hospitals in Turkey | Cross-sectional | Questionnaires on sexual harassment and work performance. | 73% reported being sexually harassed. The main perpetrators were physicians and patients, and these incidents occurred more commonly in the in-patient clinics. 45% reported a decline in work productivity following the incidents. |
| Kamchuchat et al. [75] | 2008 | Workplace violence | Thailand | 545 nurses working in a general hospital in southern Thailand | Mixed methods | Questionnaire modified from one developed by the Joint Program on Workplace Violence in the Health Sector and key informant interviews (n = 17). | The 12-month prevalence was 38.9% for verbal abuse, 3.1% for physical abuse and 0.7% for sexual harassment. The main perpetrators of verbal and physical abuse were patients and their family, while co-workers were the main perpetrators for sexual harassment. Younger age and working in high-risk areas (out-patient unit, emergency units, operating theatre, medical and surgical units) were associated with an increased risk of violence. |
| Aydin et al. [76] | 2009 | Workplace violence | Turkey | 522 general practitioners from 48 cities | Cross-sectional | Questionnaire on workplace violence. | 82.2% reported experiencing violence at work. Verbal abuse was the most common (89.3%), followed by physical violence (7.9%), economic (1.7%) and sexual violence (1.1%). Verbal and sexual violence was more common in women and physical and economic violence more common in men. Patients and their relatives was the most common source (91.1%). |
| Gimeno et al. [77] | 2010 | Prevalence of verbal abuse and its association with safety climate at work | Costa Rica | 625 health care workers working in 10 public hospitals in Costa Rica | Cross-sectional | Questionnaires on safety climate and verbal abuse. | 83.9% of the participants reported low safety climate levels. Prevalence of verbal abuse from all sources was 78.2%, with the most common being abuse from co-workers and patients. The odds of experiencing verbal abused increased with lower levels of safety climate. |
| Atan et al. [78] | 2012 | Workplace violence | Turkey | 441 nurses from 6 university hospitals | Cross-sectional | Questionnaires on workplace violence in the past year. | 60.8% reported some form of workplace violence, 59.4% verbal violence and 16.6% physical violence. The sources for verbal violence were patients (47.4%), visitors (39.5%), and health staff (10.7%) and for physical violence were patients (14.3%), visitors (5.0%) and health staff (0.5%). Of those who experienced violence, 42.9% reported a negative impact on their physical and/or psychological health and 42.9% reported a negative impact on work performance. |
| Khademloo et al. [79] | 2013 | Prevalence of physical and verbal abuse | Iran | 271 nurses from 5 hospitals in the north of Iran | Cross-sectional | Questionnaire on physical and verbal abuse experienced in the last year (Staff Observation Scale Revised (SOAS-R)). | 95.9% reported verbal abuse; the sources were patients (30.3%), family members (53.4%), and co-workers (16.1%). 29.1% reported physical abuse; the sources were patients (44.3%) and family members (55.6%). |
| da Silva et al. [80] | 2015 | Workplace violence and its association with depression | Brazil | 2940 primary health care workers from 66 health centres in Sao Paolo | Cross-sectional | Questionnaire on workplace violence (adapted from a WHO questionnaire on domestic violence), and depression and depressive symptoms (Brazilian version of the nine-item Patient Health Questionnaire). | The frequencies of violence experienced at work were: insults (44.9%), witnessing violence (29.5%), threats (24.8%), and physical aggression (2.3%). Exposure to violence was positively associated with depressive symptoms and probable major depression. |
| Baig et al. [81] | 2018 | Prevalence of workplace violence | Pakistan | 822 health care workers from hospitals, non-government organizations and ambulance services in Karachi | Mixed methods | Questionnaires on workplace violence; and 42 in-depth interviews and 17 focus group discussions. | 33.5% had experienced violence in the past year. Verbal violence was more common (30.5%) than physical violence (14.6%). The main source was from people who accompanied patients (58.1%). The main perceived causes of violence were failure to meet the expectations of patients, communication gaps, poor quality of services, inadequate security in facilities, heavy workloads, and lack of training to respond to violence. |
| Zhao et al. [82] | 2018 | Prevalence of workplace violence and association with mental health | China | 886 nurses from 8 tertiary hospitals in Heilongjiang Province | Cross-sectional | Questionnaires on workplace violence (Workplace Violence Scale), anxiety (Self-rating Anxiety Scale) and depression (Self-rating Depression Scale). | 67.2% reported workplace violence. Workplace violence was positively associated with anxiety and depression. Service years played a moderating role in the relationship between workplace violence and anxiety, and gender played a moderating role in the association between workplace violence and depression. |
| Abate et al. [83] | 2019 | Workplace violence and associated factors | Ethiopia | 435 health care workers from a tertiary care mental hospital in Addis Ababa | Cross-sectional | ILO/ICN/WHO/PSI Workplace Violence in the Health Sector Country Case Study Questionnaire. | 62.1% reported verbal violence, 36.8% physical violence and 21.8% sexual harassment. Age > 31 years and contact with patients were the associated factors. |
| Yenealem et al. [84] | 2019 | Prevalence and risk factors for violence at work | Ethiopia | 531 health care workers from Gondar city | Cross-sectional | Questionnaires adapted from the ILO/ICN/WHO/PSI Workplace Violence in the Health Sector Country Case Study Questionnaire. | 58.2% reported experiencing some form of violence, of which 53.1% reported verbal abuse, 22% physical attacks, and 7.2% sexual harassment. Working in emergency departments, working in shifts, having less work experience and being a nurse was associated with an increased risk of violence. |
| Hacer and Ali [85] | 2020 | Workplace violence and its association with burnout | Turkey | 310 physicians from Ordu province | Cross-sectional | Questionnaires on workplace violence and the Maslach Burnout Inventory. | 93.2% reported experiencing verbal violence, 86.1% psychological violence and 22.6% physical violence. The most common source of violence were patients and their relatives. Emotional exhaustion and depersonalization scores were significantly higher in those who had experienced violence. |
| II. Burnout | |||||||
| Ashkar et al. [86] | 2009 | Prevalence of burnout | Lebanon | 155 resident doctors from 2 tertiary care hospitals in Beirut | Cross-sectional | Questionnaires on occupational history and the Maslach Burnout Inventory for Health Service Workers. | 80% reported high levels of burnout in at least one domain. Prevalence according to subscales was: high levels of emotional exhaustion (EE)—67.7%, high depersonalisation (DP) scores—47.1% and low levels of personal accomplishment (PA)—23.9%. Working > 80 h/week, experiencing a major stress, getting > eight calls per month, and being female increased the risk of burnout |
| Ayala and Carnero [87] | 2013 | Demographic and occupational determinants of burnout | Peru | 93 nurses working in acute and critical care departments in a referral military hospital in Lima | Cross-sectional | Questionnaires on occupational history and the Maslach Burnout Inventory. | Higher emotional exhaustion scores were associated with having children and inversely associated with time working in the current department. Higher depersonalisation scores were associated with being single and working in the emergency room or intensive care unit. Higher personal achievement scores were associated with having children. |
| Zubairi and Noordin [88] | 2016 | Prevalence of burnout and risk factors | Pakistan | 82 resident doctors working in a university hospital in Karachi | Cross-sectional | Questionnaires on occupational history and the Maslach Burnout Inventory | 74.4% reported high levels of burnout on at least one subscale, and 12.2% reported burnout on all the three subscales. Prevalence according to subscales was: high levels of EE—60%, high DP scores—38% and low levels of PA—32%. Workload dissatisfaction, length of working hours, relationship with co-workers and lack of autonomy were associated with an increased risk of burnout |
| Colindres et al. [89] | 2018 | Association of psychosocial work environment, burnout and compliance with infection control measures | Ecuador | 333 nurses in four acute care facilities in Ecuador | Cross-sectional | Questionnaires on effort-reward imbalance, burnout (Copenhagen Burnout Inventory scale) and infection control compliance (modified Johns Hopkins University. School of Hygiene and Public Health Safety Climate Questionnaire). | 21% of nurses experienced effort reward imbalance and 35.8% had work-related burnout. 44.2% reported adhering to infection control practices. Increased effort-reward imbalance was associated with an increased risk of burnout. Burnout was independently associated with decreased adherence to infection control practices. |
| Khan et al. [90] | 2019 | Job stress and burnout | Pakistan | 447 anaesthesiologists from tertiary hospitals in Lahore and Karachi | Cross-sectional | Questionnaires on occupational history and the Maslach Burnout Inventory. | 39.4% showed moderate to high levels emotional exhaustion, 68.4% moderate to high levels of depersonalization, and 50.3% moderate to high levels of burnout in personal achievements. Working in Lahore, > 2 nights on call per week, and > 40 h/week work inside the operating room were associated with burnout. |
| Mumbwe et al. [91] | 2020 | Prevalence of burnout | Zambia | 160 anaesthesia providers (physicians and non-physicians) in Zambia | Cross-sectional | Questionnaires on occupational history and the Maslach Burnout Inventory. | Burnout was seen in 51.3% of participants. Prevalence according to subscales was: high levels of EE—66.3%, high DP scores—45% and low levels of PA—23.8%. Not being a physician and not having the right team to work with were significantly associated with burnout. |
| III. Work Environment and Job Satisfaction | |||||||
| Li et al. [92] | 2009 | Psychosocial work environment and intention to leave | China | 3088 nurses from 12 hospitals participated in the baseline study and 1521 in the one-year follow-up study | Longitudinal | Copenhagen Psychosocial Questionnaires. | Prevalence of intention to leave was 16.26% at baseline, and at one-year follow up, the incidence rate was 14.46%. Increased emotional demand, decreased workplace commitment, decreased meaning of work, and decreased job satisfaction were associated with intention to leave. |
| Ayamolowo et al. [93] | 2013 | Work environment and job satisfaction | Nigeria | 161 nurses working in public primary health care facilities in Ekiti State | Cross-sectional | Questionnaires assessing work environment (adapted from the World Health Professions Alliance checklist on environment for health care professionals) and job satisfaction (Minnesota Satisfaction Questionnaire (MSQ). | 44% of the nurses perceived their work environment to be of average quality and 31% as high quality. A majority (67.1%) of nurses reported low degrees of job satisfaction. There was a positive correlation between overall work environment and job satisfaction. |
| Ogunlade and Ogunfowokan. [94] | 2014 | Nurses’ experiences and satisfaction with night shift work | Nigeria | 186 nurses who did a roster including night shift in 2 tertiary hospitals in Ile-Ife | Cross-sectional | Questionnaires assessing experiences and satisfaction during night shift work. | Overall, 55.4% were fairly satisfied with their night shifts as compared to 1.6% who were very satisfied and 43.0% who were satisfied. Inadequate staffing and equipment for protection from hazards were the factors that contributed to the low satisfaction with night shifts. |
| Ayalew and Workineh [95] | 2019 | Job satisfaction and associated factors | Ethiopia | 220 nurses from public health facilities in Bahir Dar city | Cross-sectional | Questionnaire on job satisfaction using the Job satisfaction scale and Minnesota Questionnaire. | 43.6% were satisfied with their job. Advancement, recognition and work security were positively associated with job satisfaction. |
| Authors | Year | Topic | Origin | Participants | Type of Study | Methods | Findings |
|---|---|---|---|---|---|---|---|
| Smith et al. [96] | 2004 | Musculoskeletal complaints (MSCs) and psychosocial risk factors | China | 282 nurses from a tertiary care hospital in Shijiazhuang city | Cross-sectional | Standardized Nordic Questionnaire. | Prevalence of MSCs in the past 12 months was 70%. The most common site was the lower back (56%) followed by the neck (45%), shoulder (40%) and upper back (37%). High mental pressure, limited work support and performing boring and tedious tasks were associated with increased risk of MSCs. |
| Tezel [97] | 2005 | Musculoskeletal complaints (MSCs) | Turkey | 120 nurses from 4 hospitals in Ezrurum | Cross-sectional | Standardized Nordic Questionnaire. | 90% reported at least one MSC in the past 6 months. Low-back pain was the most common (69%), followed by neck (54%) and shoulder (46%) pain. |
| Fabunmi et al. [98] | 2008 | Prevalence of musculoskeletal disorders (MSD) | Nigeria | 214 nurses in a university hospital in Ibadan | Cross-sectional | Standardized Nordic Questionnaire. | 90.7% reported experiencing MSDs in the past 12 months. Low-back pain was the most common (78%). Job inexperience, volume and type of work were the predisposing factors. |
| de Castro et al. [99] | 2009 | Work-related injuries and back pain | Philippines | 690 nurses from 13 regions of the Philippines who were attending the Philippines Nurses Association annual national convention | Cross-sectional | Questionnaires on work related injuries/illness, reporting behaviour, and safety concerns. | 38.6% reported experiencing at least one occupational injury/illness in the past year and 78.2% reported experiencing back pain. Most of the injuries were not reported. The most frequent safety concerns reported were stress and overwork. |
| Karahan et al. [100] | 2009 | Prevalence of low-back pain and risk factors | Turkey | 1600 health care workers from 6 hospitals in 4 Turkish cities | Cross-sectional | Questionnaires on back pain and occupational history. | 61.3% reported at least one occurrence of low-back pain within the last 12 months. Age, female gender, smoking, occupation as a nurse, work stress and heavy lifting were associated with increased risks. |
| Mehrdad et al. [101] | 2010 | Musculoskeletal symptoms and association with psychosocial factors | Iran | 317 nurses from the Emam hospital in Tehran | Cross-sectional | Standardized Nordic Questionnaire and General Nordic questionnaire on psychosocial work environment. | 95% reported complaints in at least one body site in the past 12 months. Low back was the most common site (73.2%). Higher levels of stress was associated with increased risk of musculoskeletal complaints. |
| Tinubu et al. [102] | 2010 | Work-related musculoskeletal disorders (WMSDs) and risk factors | Nigeria | 128 nurses from 3 hospitals in Ibidan | Cross-sectional | Standardized Nordic Questionnaire. | 78% reported WMSDs in at least one body site in the past 12 months. WMSDs occurred mostly in low back (44.1%), neck (28.0%), and knees (22.4%). Working in the same position for long periods, lifting/transferring patients, bending or twisting, and handling many patients were the commonest risk factors. |
| Arsalani et al. [103] | 2014 | Prevalence of musculoskeletal disorders (MSD) and risk factors | Iran | 520 nurses working in 10 university hospitals in Tehran | Cross-sectional | Standardized Nordic Questionnaire and psychosocial working conditions from the Copenhagen Psychosocial Questionnaire. | 88% reported experiencing MSDs in the past 12 months, with the most common body regions being the lower back (65.3%), knees (56.2%) and neck (49.8%). Physical and psychosocial work demands and low control over their work, which lead to work-related stress, increased the risk of MSDs. Participants also reported inflexible work schedule, poor quality of devices for transferring patients, overexertion and job dissatisfaction. |
| Barzideh et al. [104] | 2014 | Prevalence of musculoskeletal disorders (MSD) and risk factors | Iran | 385 nurses working in 14 educational hospitals | Cross-sectional | Standardized Nordic questionnaire and Job Content Questionnaire. | 89.9% reported experiencing MSDs in the last 12 months. Lower back pain was the most common (61.8%). High psychological and physical job demands and low decision latitude were associated with increased risks. |
| Munabi et al. [105] | 2014 | Prevalence of musculoskeletal disorders (MSD) and risk factors | Uganda | 741 nurses from 5 hospitals in Uganda | Cross-sectional | Questionnaire adapted from the Standardized Nordic and standardized Dutch Musculoskeletal questionnaires. | 80.8% had experienced MSDs in the last 12 months. Low-back pain was the most common (61.9%). Working in a bent or twisted position, mental exhaustion and being absent from work for more than 6 months were associated with an increased risk. |
| Yasobant and Rajkumar [106] | 2014 | Work-related musculoskeletal disorders (WMSDs), and risk factors | India | 140 health care workers from a tertiary care hospital in Chennai | Cross-sectional | Standardized Nordic Musculoskeletal Questionnaire. | 50.7% reported symptoms in at least one body site in the past 12 months. Low back was the most common site (45.7%). Working in the same position for long periods, working in awkward and cramped positions, and performing repetitive tasks were the commonest risk factors. |
| Abaraogu et al. [107] | 2017 | Work-related musculoskeletal disorders (WMSDs) and job stress | Nigeria | 126 physiotherapists from hospitals in five states | Cross-sectional | Standardized Nordic Musculoskeletal Questionnaire and Job Content Questionnaire. | 82.1% reported symptoms in at least one body site in the last 12 months. Low back was the most common site (57.8%). There were high levels of stress in most of the job dimensions. However, no specific domains of job stress dimensions were associated with WMSDs. |
| Amin et al. [108] | 2018 | Prevalence of self-perceived emotional distress and musculoskeletal disorders (MSD) | Malaysia | 376 nurses working in public hospitals in the Klang valley | Cross-sectional | Standardized Nordic Musculoskeletal Questionnaire and short version of the Depression, Anxiety, and Stress Scale. | 73.1% had experienced MSDs in the last 12 months and neck was the most common site (48.9%). 75% reported emotional distress. Stress and anxiety were significantly associated with an increased risk of MSDs. |
| Dlungwane et al. [109] | 2018 | Low-back pain and risk factors | South Africa | 242 nurses from a regional hospital in KwaZulu-Natal | Cross-sectional | Questionnaire on back pain and risk factors. | The point prevalence of low-back pain was 59%. Frequent bending, maintaining prolonged positions and transferring patients were the risk factors. |
| Ike and Olawumi [110] | 2018 | Back pain and risk factors | Nigeria | 228 nurses working in a medical centre in Abeokuta | Cross-sectional | Questionnaire on back pain and risk factors. | The point prevalence of back pain was 39%. Maintaining a particular position for long periods and lifting patients were common risk factors. |
| Luan et al. [111] | 2018 | Prevalence of musculoskeletal disorders (MSD) and risk factors | Vietnam | 1179 nurses working in 15 district hospitals in Haiphong | Cross-sectional | Standardized Nordic Questionnaire. | 74.7% reported symptoms of MSDs in the last 12 months. Low back and neck were the most common sites (44.4% and 44.1%). Age, history of musculoskeletal disease, anxiety and absenteeism in the workplace were risk factors. |
| Dong et al. [112] | 2019 | Prevalence of musculoskeletal disorders (MSD) and risk factors | China | 14,720 health care workers from 8 tertiary hospitals in Shandong Province | Cross-sectional | Questionnaire incorporating the Standardized Nordic Musculoskeletal and the Dutch Musculoskeletal Questionnaires. | 91.2% reported symptoms in at least one body site in the last 12 months. Low back was the most common site (72.8%). MSDs were associated with increased work load, psychological fatigue, mental stress and certain ergonomic factors (bending, twisting). |
| Authors | Year | Topic | Origin | Participants | Type of Study | Methods | Findings |
|---|---|---|---|---|---|---|---|
| I. Chemical Hazards | |||||||
| Baykal et al. [113] | 2009 | Working conditions and safe handling practices of antineoplastic drugs | Turkey | 171 nurses who worked in oncology units and administered antineoplastic drugs in nine hospitals in Istanbul | Cross-sectional | Questionnaires on working conditions and safe handling practices of antineoplastic drugs were distributed. | 94.7% of the nurses reported wearing gloves, 89.5% wore masks, 52.0% wore gowns and 18.7% wore goggles. 40.4% reported preparing drugs in a biological safety cabinet, 37.4% said that they prepared the drugs in the nurses’ office and 15.8% said that they prepared the drugs in a room that was also used for other purposes such as meals. |
| Agrawal et al. [114] | 2010 | Exposure to latex and latex allergy | India | 163 dental professionals working in Udaipur city | Cross-sectional | Questionnaires on latex glove use and symptoms of latex allergy. | 16% reported allergy symptoms to latex gloves. 81.6% wore gloves for >5 h a day. The number of years of latex gloves use was significantly associated with allergic symptoms. |
| Amarasekera et al. [115] | 2010 | Exposure to latex and latex allergy | Sri-Lanka | 325 health care workers in a tertiary care hospital | Cross-sectional | Questionnaires latex gloves use and symptoms of latex allergy. | 16.3% reported latex allergy symptoms. 49.2% wore gloves for >1 h a day and 44.2% handled other rubber products at work. Longer duration of working as a health care worker and using gloves for >1 h/day were the risk factors associated with allergic symptoms. |
| Phaswana and Naidoo [116] | 2013 | Prevalence of latex sensitization and allergy with the use of hypoallergenic powder and lightly powdered latex gloves | South Africa | 501 health care workers (337 who used latex gloves and 164 administration staff who did not use latex gloves) in a tertiary care hospital in KwaZulu-Natal | Cross-sectional | Questionnaires on latex glove use and symptoms of latex allergy. Skin prick tests were conducted for latex sensitization. | Prevalence of latex sensitisation and allergy in exposed workers was 7.1% and 5.9%, respectively; and in unexposed workers it was 3.1% and 1.8%. Work-related allergy symptoms were significantly higher in exposed workers. A dose-response relationship was observed for powdered latex gloves. |
| Supapvanich et al. [117] | 2013 | Exposure to latex and latex allergy | Thailand | 899 nurses from three hospitals in Thailand | Cross-sectional | Questionnaires on respiratory and dermal symptoms that were attributed to latex gloves use. | 18% reported symptoms attributable to latex gloves use. Dermal symptoms were more frequently reported, particularly itchy skin and rash. Using >15 pairs of powdered latex gloves/day, using chlorhexidine and being an operating theatre nurse were the risk factors associated dermal symptoms. |
| Köse et al. [118] | 2014 | Exposure to latex and latex sensitization | Turkey | 1115 health care workers from an education and research hospital in Izmir | Cross-sectional | Questionnaires on latex gloves use and symptoms of latex allergy. Blood was tested for latex-specific IgE levels. | Prevalence of latex sensitization was 4.2%. Latex allergy was more common in nurses. |
| Supapvanich et al. [119] | 2014 | Exposure to latex and latex sensitization | Thailand | 363 nurses from two tertiary hospitals in Southern Thailand | Cross-sectional | Questionnaires on use of latex gloves and symptoms related to latex use. Latex sensitization was confirmed by detecting anti-latex IgE antibodies using a solid phase immunoassay. | The prevalence of latex sensitization was 4.4%. The prevalence of latex sensitization was higher in hospitals where gloves with higher protein levels were used. |
| Abbasi et al. [120] | 2016 | Safe handling practices of antineoplastic drugs | Iran | 86 nurses who worked in oncology units and administered antineoplastic drugs from six centres of chemotherapy in Shiraz | Cross-sectional | Questionnaires on the safe handling practices were distributed. Observation of work practices was performed using a check list. | Only about half of the nurses used personal protective equipment (PPE) during the administration of the drugs, and only about 5% used PPE during the administration and disposal of the drugs. Biological safety cabinets were used in all the hospitals and clinics included in the study. |
| Elshaer [121] | 2017 | Adherence to control measures used for handling of antineoplastic drugs | Egypt | 54 nurses and clinical pharmacists who were exposed to ADs and 54 who were not exposed, working in oncology centres in Alexandria city. | Cross-sectional | Questionnaires on adverse health effects and control measures were distributed. Nurses and clinical pharmacists who were exposed to ADs were compared to those who were not exposed. | Biological safety cabinets and ventilation devices were used by pharmacists but not by nurses. Significantly higher percentages of pharmacists reported safe handling practices and the use of PPE as compared to nurses. There was no medical surveillance program in the workplace. |
| Alehashem and Baniasadi [122] | 2018 | Safe-handling practices of antineoplastic drugs and control measures | Iran | 14 oncology health care workers filled 224 questionnaires in a tertiary care centre | Cross-sectional | 7–8 health care workers worked in the Oncology ward every day. They filled the questionnaire on safe handling practices for six weeks or 30 working days. | 20.56% reported carrying out drug preparations without any personal protective equipment. All preparations of antineoplastic drugs were reported to be performed in a biological safety cabinet. |
| Bayraktar-Ekincioglu et al. [123] | 2018 | Practices and safety measures when handling antineoplastic drugs | Turkey | 40 hospital pharmacists who handled chemotherapy from Turkey | Cross-sectional | Questionnaires on chemotherapy drug preparation processes and knowledge on the safety measures. | The majority (42.5%) reported using automated chemotherapy units and 30% prepared the drugs manually. The reported practices were not always consistent with published recommendations: use of double glove (63.6%), glasses (62.2%), hair cap (66.7%), foot covers (32.3%), masks (89.1%), coat (92.1%), closed-system drug transfer set (70.6%), and biological safety cabinet (91.7%). |
| II. Occupational Hazards (General) | |||||||
| Aluko et al. [124] | 2016 | Compliance with control measures | Nigeria | 290 health care workers in Osun state | Cross-sectional | Questionnaires on knowledge on occupational hazards and their control practices. | Participants were knowledgeable about the various types of occupational hazards (biological, chemical, physical, and ergonomic). Regarding control practices, 96.2% wore gloves and 77.2 practiced correct body posturing during clinical procedures, 93.8% reported safe disposals, and 62.4% were immunized against Hepatitis B. Only 52.1% always complied with standard procedures and the main reasons for non-compliance were lack of safety equipment and time constrains. |
| Tait et al. [125] | 2018 | Biological, chemical, and physical hazards in medical laboratories | Kenya | 204 laboratory workers in 108 medical laboratories in Kajiado county | Cross-sectional | Questionnaires on biological, chemical and physical hazards. | 65.6% were exposed to 1 + biological hazard, 38.2% handled un-labelled and un-marked chemicals; and 49.5% reported laboratory equipment dangerously placed. There were a large number of other risks. Strong correlations between protective measures within individuals. Control measures reported were occupational health and safety training and supervising staff (98%), proper medical waste containers (92.6%), first aid safety equipment (36.8%), chemical hygiene plans (25%) and chemical hoods (19.1%). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rai, R.; El-Zaemey, S.; Dorji, N.; Rai, B.D.; Fritschi, L. Exposure to Occupational Hazards among Health Care Workers in Low- and Middle-Income Countries: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 2603. https://doi.org/10.3390/ijerph18052603
Rai R, El-Zaemey S, Dorji N, Rai BD, Fritschi L. Exposure to Occupational Hazards among Health Care Workers in Low- and Middle-Income Countries: A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(5):2603. https://doi.org/10.3390/ijerph18052603
Chicago/Turabian StyleRai, Rajni, Sonia El-Zaemey, Nidup Dorji, Bir Doj Rai, and Lin Fritschi. 2021. "Exposure to Occupational Hazards among Health Care Workers in Low- and Middle-Income Countries: A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 5: 2603. https://doi.org/10.3390/ijerph18052603
APA StyleRai, R., El-Zaemey, S., Dorji, N., Rai, B. D., & Fritschi, L. (2021). Exposure to Occupational Hazards among Health Care Workers in Low- and Middle-Income Countries: A Scoping Review. International Journal of Environmental Research and Public Health, 18(5), 2603. https://doi.org/10.3390/ijerph18052603






