Socioecological Factors Influencing Sexual Health Experiences and Health Outcomes of Migrant Asian Women Living in ‘Western’ High-Income Countries: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Study Eligibility
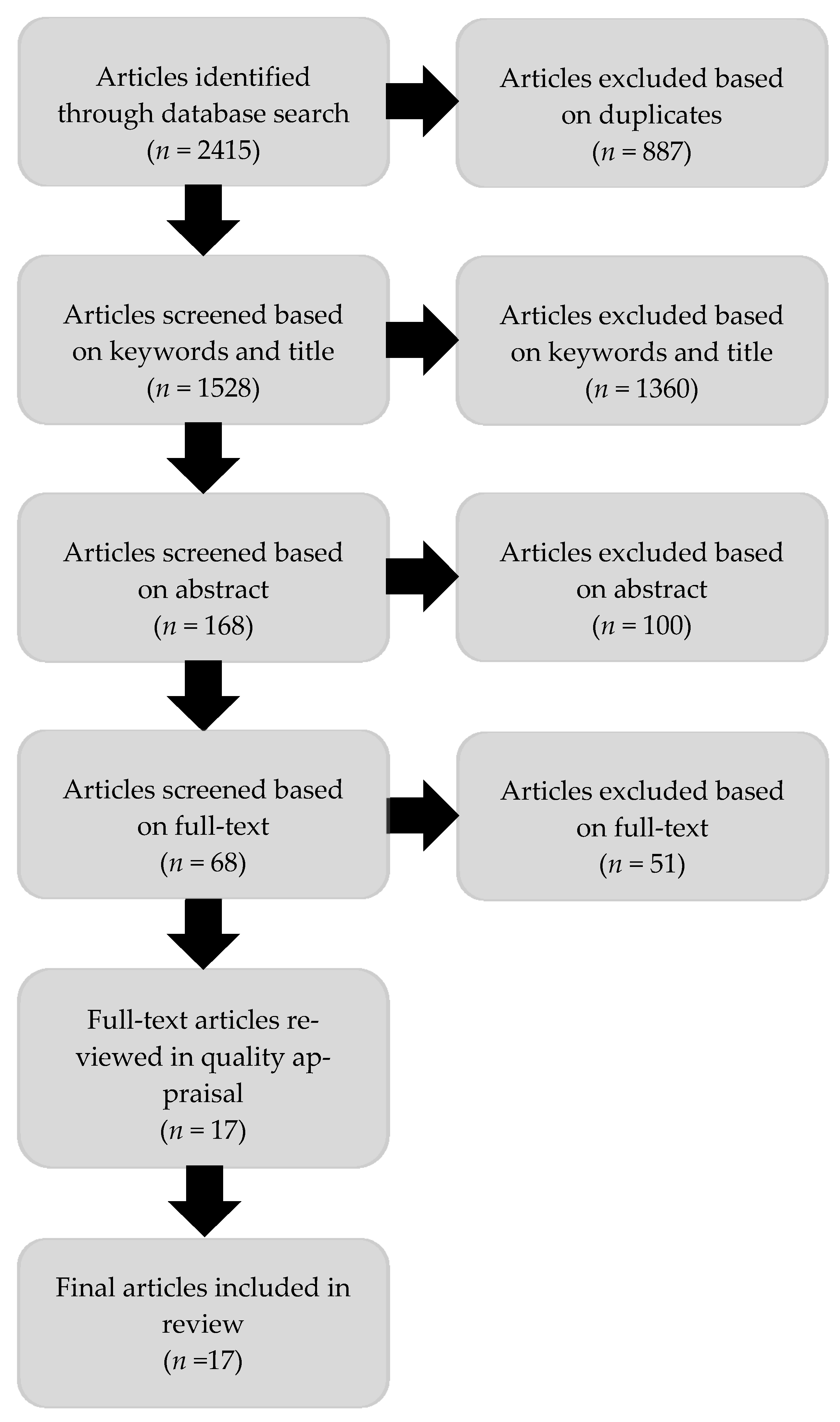
2.2. Search Strategy and Study Selection
2.3. Quality Appraisal and Data Extraction
3. Results
- Individual/personal factors, such as knowledge and behaviour;
- Interpersonal relationships, including partner, family, and peer influence;
- Institutional settings and institutions, including healthcare, workplaces, and schools;
- Societal/broad social factors, including social norms and policies.
3.1. Overview of Studies
3.2. Participant Characteristics
3.3. SEM Level—Individual
3.3.1. Sexual Education and Knowledge
3.3.2. Contraception Use
3.3.3. Attitudes towards Prevention
3.4. SEM Level—Interpersonal
3.5. SEM Level—Institutions
3.5.1. Navigating the Health System
3.5.2. Language
3.6. SEM Level—Societal
Attitudes towards Women and Women’s Sexuality
3.7. Recommendations for Research, Practice, and Policy
4. Discussion
4.1. Study Design and Reporting Limitations of Included Studies
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Robertson, S.; Ho, E.L.-E. Temporalities, materialities and connecting locales: Migration and mobility in Asia-Pacific cities. J. Ethn. Migr. Stud. 2016, 42, 2263–2271. [Google Scholar] [CrossRef]
- Pratt, G.; Yeoh, B. Transnational (Counter) Topographies. Gend. Place Cult. 2003, 10, 159–166. [Google Scholar] [CrossRef]
- Yeoh, B.S.A.; Ramdas, K. Gender, migration, mobility and transnationalism. Gend. Place Cult. 2014, 21, 1197–1213. [Google Scholar] [CrossRef]
- United Nations. International Migration Report 2017-Highlights; UN: New York, NY, USA, 2018. [Google Scholar]
- International Organization for Migration Global Migration Data Analysis Centre. Migration Data Portal. Available online: https://migrationdataportal.org/about (accessed on 4 November 2019).
- Sijapati, B. Womens Labour Migration from Asia and the Pacific: Opportunities and Challenges; International Organization for Migration: Bangkok, Tailand; Washington, DC, USA, 2016. [Google Scholar]
- Simon-Kumar, R. The ‘problem’ of Asian women’s sexuality: Public discourses in Aotearoa/New Zealand. Cult. Health Sex. 2009, 11, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Okazaki, S. Influences of culture on Asian Americans’ sexuality. J. Sex Res. 2002, 39, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Sechiyama, K. Patriarchy in East Asia: A Comparative Sociology of Gender; BRILL: Leiden, The Netherlands, 2013. [Google Scholar]
- Klugman, J.; Hanmer, L.; Twigg, S.; Hasan, T.; McCleary-Sills, J.; Santamaria, J. Voice and Agency: Empowering Women and Girls for Shared Prosperity; The World Bank: Washington, DC, USA, 2014. [Google Scholar]
- Essers, C.; Tedmanson, D. Upsetting ‘Others’ in the Netherlands: Narratives of Muslim Turkish Migrant Businesswomen at the Crossroads of Ethnicity, Gender and Religion. Gend. Work Organ. 2014, 21, 353–367. [Google Scholar] [CrossRef]
- Natter, K. Rethinking immigration policy theory beyond ‘Western liberal democracies’. Comp. Migr. Stud. 2018, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, A.U.; Couture-Carron, A.; Maticka-Tyndale, E. ‘Should I or Should I Not’?: An exploration of South Asian youth’s resistance to cultural deviancy. Int. J. Adolesc. Youth 2016, 21, 232–251. [Google Scholar] [CrossRef]
- Castañeda, H.; Holmes, S.M.; Madrigal, D.S.; Young, M.-E.D.; Beyeler, N.; Quesada, J. Immigration as a social determinant of health. Annu. Rev. Public Health 2015, 36, 375–392. [Google Scholar] [CrossRef]
- Mengesha, Z.B.; Dune, T.; Perz, J. Culturally and linguistically diverse women’s views and experiences of accessing sexual and reproductive health care in Australia: A systematic review. Sex. Health 2016, 13, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Multicultural Women’s Health Australia. Sexual and Reproductive Health Data Report; Multicultural Women’s Health Australia: Melbourne, Austrilia, 2016. [Google Scholar]
- Keygnaert, I.; Guieu, A.; Ooms, G.; Vettenburg, N.; Temmerman, M.; Roelens, K. Sexual and reproductive health of migrants: Does the EU care? Health Policy 2014, 114, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, I.; Aldridge, R.W.; Devakumar, D.; Orcutt, M.; Burns, R.; Barreto, M.L.; Dhavan, P.; Fouad, F.M.; Groce, N.; Guo, Y.; et al. The UCL–Lancet Commission on Migration and Health: The health of a world on the move. Lancet 2018, 392, 2606–2654. [Google Scholar] [CrossRef]
- Rutter, H.; Savona, N.; Glonti, K.; Bibby, J.; Cummins, S.; Finegood, D.T.; Greaves, F.; Harper, L.; Hawe, P.; Moore, L.; et al. The need for a complex systems model of evidence for public health. Lancet 2017, 390, 2602–2604. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An Ecological Perspective on Health Promotion Programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Golden, S.D.; Earp, J.A.L. Social ecological approaches to individuals and their contexts: Twenty years of health education & behavior health promotion interventions. Health Educ. Behav. 2012, 39, 364–372. [Google Scholar]
- Sallis, J.F.; Owen, N.; Fisher, E. Ecological models of health behavior. In Health Behavior: Theory, Research, and Practice; Jossey-Bass: San Francisco, CA, USA, 2015; Volume 5. [Google Scholar]
- Bronfenbrenner, U. Ecological Systems Theory; Jessica Kingsley Publishers: London, UK, 1992. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Rade, D.; Crawford, G.; Lobo, R.; Gray, C.; Brown, G. Sexual Health Help-Seeking Behavior among Migrants from Sub-Saharan Africa and South East Asia living in High Income Countries: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 1311. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, S.; Hallett, J.; Gray, C.; Lobo, R.; Crawford, G. What Works? Prevention and Control of Sexually Transmitted Infections and Blood-Borne Viruses in Migrants from Sub-Saharan Africa, Northeast Asia and Southeast Asia Living in High-Income Countries: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 1287. [Google Scholar] [CrossRef] [PubMed]
- Crawford, G.; Lobo, R.; Brown, G.; Macri, C.; Smith, H.; Maycock, B. HIV, Other Blood-Borne Viruses and Sexually Transmitted Infections amongst Expatriates and Travellers to Low- and Middle-Income Countries: A Systematic Review. Int. J. Environ. Res. Public Health 2016, 13, 1249. [Google Scholar] [CrossRef]
- Crawford, G.; Leavy, J.; Portsmouth, L.; Jancey, J.; Leaversuch, F.; Nimmo, L.; Reid-Dornbusch, L.; Hills, E. Development of a systematic review of public health interventions to prevent children drowning. Open J. Prev. Med. 2014, 4, 100–106. [Google Scholar] [CrossRef]
- The World Bank. World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519#East_Asia_and_Pacific (accessed on 21 June 2018).
- United Nations. Asia and the Pacific. Available online: https://www.un.org/en/sections/where-we-work/asia-and-pacific/index.html#:~:text=The%20UNOPS%20Asia%2C%20as%20well,Philippines%2C%20Sri%20Lanka%20and%20Thailand (accessed on 5 June 2020).
- World Health Organization. Defining Sexual Health: Report of a Technical Consultation on Sexual Health, 28–31 January 2002, Geneva; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Ivankovich, M.B.; Fenton, K.A.; Douglas, J.M. Considerations for National Public Health Leadership in Advancing Sexual Health. Public Health Rep. 2013, 128, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Bronfenbrenner, U. Toward an experimental ecology of human development. Am. Psychol. 1977, 32, 513. [Google Scholar] [CrossRef]
- Clarivate Analytics EndNote X9; Clarivate Analytics: Philadelphia, PA, USA, 2019.
- Mateen, F.J.; Oh, J.; Tergas, A.I.; Bhayani, N.H.; Kamdar, B.B. Titles versus titles and abstracts for initial screening of articles for systematic reviews. Clin. Epidemiol. 2013, 5, 89. [Google Scholar] [CrossRef] [PubMed]
- Veritas Health Innovation. Covidence Systematic Review Software; Veritas Health Innovation Melbourne: Melbourne, Austrilia, 2017. [Google Scholar]
- Joanna Briggs Institute. Joanna Briggs Institute Reviewers’ Manual, 2014 ed.; Joanna Briggs Institute: Adelaide, Australia, 2014. [Google Scholar]
- Åkerman, E.; Essén, B.; Westerling, R.; Larsson, E. Healthcare-seeking behaviour in relation to sexual and reproductive health among Thai-born women in Sweden: A qualitative study. Cult. Health Sex. 2017, 19, 194–207. [Google Scholar] [CrossRef]
- Åkerman, E.; Östergren, P.-O.; Essén, B.; Fernbrant, C.; Westerling, R. Knowledge and utilization of sexual and reproductive healthcare services among Thai immigrant women in Sweden. BMC Int. Health Hum. Rights 2016, 16, 25. [Google Scholar] [CrossRef]
- Burchard, A.; Laurence, C.; Stocks, N. Female International students and sexual health: A qualitative study into knowledge, beliefs and attitudes. Aust. Fam. Physician 2011, 40, 817. [Google Scholar]
- Burke, N.J.; Do, H.H.; Talbot, J.; Sos, C.; Ros, S.; Taylor, V.M. Protecting our Khmer daughters: Ghosts of the past, uncertain futures, and the human papillomavirus vaccine. Ethn. Health 2015, 20, 376–390. [Google Scholar] [CrossRef]
- Dhar, C.P.; Kaflay, D.; Dowshen, N.; Miller, V.A.; Ginsburg, K.R.; Barg, F.K.; Yun, K. Attitudes and Beliefs Pertaining to Sexual and Reproductive Health Among Unmarried, Female Bhutanese Refugee Youth in Philadelphia. J. Adolesc. Health 2017, 61, 791–794. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K.; Kelly, M.; Bateson, D.; Rutherford, A.; Stewart, M.; Richters, J. Contraceptive choices and sexual health of Japanese women living in Australia: A brief report from a qualitative study. Aust. Fam. Physician 2016, 45, 523. [Google Scholar] [PubMed]
- Nguyen, G.T.; Chen, B.; Chan, M. Pap testing, awareness, and acceptability of a human papillomavirus (HPV) vaccine among Chinese American women. J. Immigr. Minority Health 2012, 14, 803–808. [Google Scholar] [CrossRef]
- Pell, C.; Dabbhadatta, J.; Harcourt, C.; Tribe, K.; O’Connor, C. Demographic, migration status, and work-related changes in Asian female sex workers surveyed in Sydney, 1993 and 2003. Aust. N. Z. J. Public Health 2006, 30, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Verran, A.; Evans, S.; Lin, D.J.; Griffiths, F. The experiences and perceptions of family planning of female Chinese asylum seekers living in the UK. J. Fam. Plann Reprod Health Care 2015, 41, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Gagnon, A.J.; Merry, L.; Bocking, J.; Rosenberg, E.; Oxman-Martinez, J. South Asian migrant women and HIV/STIs: Knowledge, attitudes and practices and the role of sexual power. Health Place 2010, 16, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Micollier, E. Femininities on transnational journeys and sexual health risk: Experiences of Chinese immigrant women in Canada. Gend. Place Cult. 2017, 24, 1787–1806. [Google Scholar] [CrossRef]
- Wray, A.; Ussher, J.M.; Perz, J. Constructions and experiences of sexual health among young, heterosexual, unmarried Muslim women immigrants in Australia. Cult. Health Sex. 2014, 16, 76–89. [Google Scholar] [CrossRef]
- Hawa, R.N.; Underhill, A.; Logie, C.H.; Islam, S.; Loutfy, M. South Asian immigrant women’s suggestions for culturally-tailored HIV education and prevention programs. Ethn. Health 2017, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Raj, A.; Liu, R.; McCleary-Sills, J.; Silverman, J.G. South Asian victims of intimate partner violence more likely than non-victims to report sexual health concerns. J. Immigr. Health 2005, 7, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Khoei, E.M.; Whelan, A.; Cohen, J. Sharing beliefs: What sexuality means to Muslim Iranian women living in Australia. Cult. Health Sex. 2008, 10, 237–248. [Google Scholar] [CrossRef]
- Lindblad, F.; Signell, S. Degrading attitudes related to foreign appearance: Interviews with Swedish female adoptees from Asia. Adopt. Fostering 2008, 32, 46–59. [Google Scholar] [CrossRef]
- Richters, J.; Khoei, E.M. Concepts of sexuality and health among Iranian women in Australia. Aust. Fam. Physician 2008, 37, 190. [Google Scholar]
- Pottie, K.; Greenaway, C.; Feightner, J.; Welch, V.; Swinkels, H.; Rashid, M.; Narasiah, L.; Kirmayer, L.J.; Ueffing, E.; MacDonald, N.E.; et al. Evidence-based clinical guidelines for immigrants and refugees. CMAJ 2011, 183, E824–E925. [Google Scholar] [CrossRef]
- Ussher, J.M.; Perz, J.; Metusela, C.; Hawkey, A.J.; Morrow, M.; Narchal, R.; Estoesta, J. Negotiating Discourses of Shame, Secrecy, and Silence: Migrant and Refugee Women’s Experiences of Sexual Embodiment. Arch. Sex. Behav. 2017, 46, 1901–1921. [Google Scholar] [CrossRef]
- Metusela, C.; Ussher, J.; Perz, J.; Hawkey, A.; Morrow, M.; Narchal, R.; Estoesta, J.; Monteiro, M. “In My Culture, We Don’t Know Anything About That”: Sexual and Reproductive Health of Migrant and Refugee Women. Int. J. Behav. Med. 2017, 24, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Langer, A.; Meleis, A.; Knaul, F.M.; Atun, R.; Aran, M.; Arreola-Ornelas, H.; Bhutta, Z.A.; Binagwaho, A.; Bonita, R.; Caglia, J.M.; et al. Women and Health: The key for sustainable development. Lancet 2015, 386, 1165–1210. [Google Scholar] [CrossRef]
- George, A.S.; Amin, A.; de Abreu Lopes, C.M.; Ravindran, T.K.S. Structural determinants of gender inequality: Why they matter for adolescent girls’ sexual and reproductive health. BMJ 2020, 368, l6985. [Google Scholar] [CrossRef]
- Crenshaw, K. Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color. Stanf. Law Rev. 1991, 43, 1241–1299. [Google Scholar] [CrossRef]
- Salad, J.; Verdonk, P.; de Boer, F.; Abma, T.A. “A Somali girl is Muslim and does not have premarital sex. Is vaccination really necessary?” A qualitative study into the perceptions of Somali women in the Netherlands about the prevention of cervical cancer. Int. J. Equity Health 2015, 14, 68. [Google Scholar] [CrossRef] [PubMed]
- Ngum Chi Watts, M.C.; McMichael, C.; Liamputtong, P. Factors Influencing Contraception Awareness and Use: The Experiences of Young African Australian mothers. J. Refug. Stud. 2015, 28, 368–387. [Google Scholar] [CrossRef]
- Heard, E.; Fitzgerald, L.; Wigginton, B.; Mutch, A. Applying intersectionality theory in health promotion research and practice. Health Promot. Int. 2019. [Google Scholar] [CrossRef]
- Agu, J.; Lobo, R.; Crawford, G.; Chigwada, B. Migrant Sexual Health Help-Seeking and Experiences of Stigmatization and Discrimination in Perth, Western Australia: Exploring Barriers and Enablers. Int. J. Environ. Res. Public Health 2016, 13, 485. [Google Scholar] [CrossRef]
- Henderson, S.; Kendall, E. Culturally and linguistically diverse peoples’ knowledge of accessibility and utilisation of health services: Exploring the need for improvement in health service delivery. Aust. J. Prim. Health 2011, 17, 195–201. [Google Scholar] [CrossRef]
- Villa-Torres, L.; Gonzalez-Vazquez, T.; Fleming, P.J.; González-González, E.L.; Infante-Xibille, C.; Chavez, R.; Barrington, C. Transnationalism and health: A systematic literature review on the use of transnationalism in the study of the health practices and behaviors of migrants. Soc. Sci. Med. 2017, 183, 70–79. [Google Scholar] [CrossRef]
- Wohler, Y.; Dantas, J.A. Barriers accessing mental health services among culturally and linguistically diverse (CALD) immigrant women in Australia: Policy implications. J. Immigr. Minority Health 2017, 19, 697–701. [Google Scholar] [CrossRef] [PubMed]
- National Health Medical Research Council. Cultural Competency in Health: A Guide for Policy, Partnerships and Participation; National Health and Medical Research Council: Canberra, Australia, 2006. [Google Scholar]
- Spitzer, D.L.; Torres, S.; Zwi, A.B.; Khalema, E.N.; Palaganas, E. Towards inclusive migrant healthcare. BMJ 2019, 366, l4256. [Google Scholar] [CrossRef] [PubMed]
- Davies, A.A.; Basten, A.; Frattini, C. Migration: A social determinant of the health of migrants. Eurohealth 2009, 16, 10–12. [Google Scholar]
- Zimmerman, C.; Kiss, L.; Hossain, M. Migration and health: A framework for 21st century policy-making. PLoS Med. 2011, 8, e1001034. [Google Scholar] [CrossRef]
- Juárez, S.P.; Honkaniemi, H.; Dunlavy, A.C.; Aldridge, R.W.; Barreto, M.L.; Katikireddi, S.V.; Rostila, M. Effects of non-health-targeted policies on migrant health: A systematic review and meta-analysis. Lancet Glob. Health 2019, 7, e420–e435. [Google Scholar] [CrossRef]
- Lawless, A.P.; Williams, C.; Hurley, C.; Wildgoose, D.; Sawford, A.; Kickbusch, I. Health in All Policies: Evaluating the South Australian approach to intersectoral action for health. Can. J. Public Health Rev. Can. Sante Publique 2012, 103, S15–S19. [Google Scholar] [CrossRef]
- Laverack, G. ‘Leaving No One Behind’: The Challenge of Reaching Migrant Populations. Challenges 2018, 9, 37. [Google Scholar] [CrossRef]
- Baum, F.; MacDougall, C.; Smith, D. Participatory action research. J. Epidemiol. Community Health 2006, 60, 854–857. [Google Scholar] [CrossRef]
- Gray, C.; Crawford, G.; Lobo, R.; Maycock, B. Co-Designing an Intervention to Increase HIV Testing Uptake with Women from Indonesia At-Risk of HIV: Protocol for a Participatory Action Research Study. Methods Protoc. 2019, 2, 41. [Google Scholar] [CrossRef] [PubMed]
- Vujcich, D.; Wangda, S.; Roberts, M.; Lobo, R.; Maycock, B.; Kulappu Thanthirige, C.; Reid, A. Modes of administering sexual health and blood-borne virus surveys in migrant populations: A scoping review. PLoS ONE 2020, 15, e0236821. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Wickramage, K.; Vearey, J.; Zwi, A.B.; Robinson, C.; Knipper, M. Migration and health: A global public health research priority. BMC Public Health 2018, 18, 987. [Google Scholar] [CrossRef] [PubMed]
| Concept 1 (Mobility) |
| “Transient and Migrants” |
| “Emigrants and Immigrants” |
| Refugees |
| “International student” |
| Human migration |
| Concept 2 (Sex) |
| “Sexual health” |
| Sex education |
| HIV infections |
| Sexual Behaviour |
| Sexual Transmitted Diseases |
| Unsafe sex |
| Concept 3 (Gender) |
| Gender |
| Woman |
| Women |
| Feminist |
| Feminine |
| Female |
| Concept 4 (Asia) |
| All 48 countries, 3 territories included * |
| Asia, central |
| Asia, western |
| Asia |
| Asia, southeastern |
| Asia, northern |
| SEM Level | Themes Included | Number of Articles * (n) | Citations |
|---|---|---|---|
| Individual | Sexual health knowledge; contraception and condom use; attitudes towards prevention | 13 | [38,39,40,41,42,43,44,45,46,47,48,49,50] |
| Interpersonal | Sexual relationships and relationship power | 4 | [47,48,50,51] |
| Institutions | Health service access | 8 | [38,41,42,43,44,46,47,52] |
| Societal | Attitudes towards women | 5 | [40,42,49,52,53,54]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gray, C.; Crawford, G.; Maycock, B.; Lobo, R. Socioecological Factors Influencing Sexual Health Experiences and Health Outcomes of Migrant Asian Women Living in ‘Western’ High-Income Countries: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 2469. https://doi.org/10.3390/ijerph18052469
Gray C, Crawford G, Maycock B, Lobo R. Socioecological Factors Influencing Sexual Health Experiences and Health Outcomes of Migrant Asian Women Living in ‘Western’ High-Income Countries: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(5):2469. https://doi.org/10.3390/ijerph18052469
Chicago/Turabian StyleGray, Corie, Gemma Crawford, Bruce Maycock, and Roanna Lobo. 2021. "Socioecological Factors Influencing Sexual Health Experiences and Health Outcomes of Migrant Asian Women Living in ‘Western’ High-Income Countries: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 5: 2469. https://doi.org/10.3390/ijerph18052469
APA StyleGray, C., Crawford, G., Maycock, B., & Lobo, R. (2021). Socioecological Factors Influencing Sexual Health Experiences and Health Outcomes of Migrant Asian Women Living in ‘Western’ High-Income Countries: A Systematic Review. International Journal of Environmental Research and Public Health, 18(5), 2469. https://doi.org/10.3390/ijerph18052469







