Assessing Patient Safety Culture in Hospital Settings
Abstract
1. Introduction
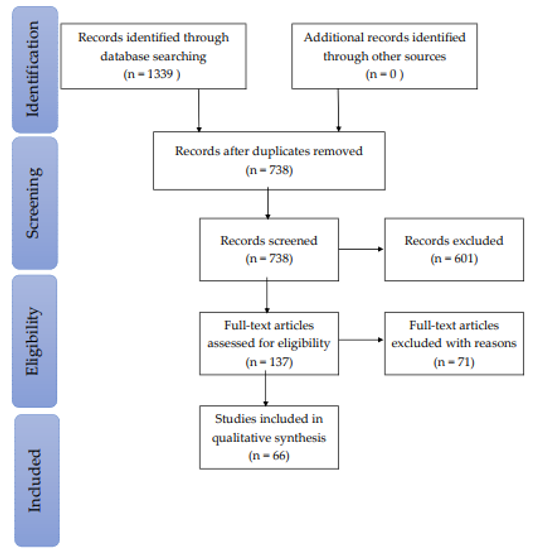
2. Materials and Methods
- What research instruments are used to study patient safety culture?
- What are the essential dimensions of patient safety culture assessment?
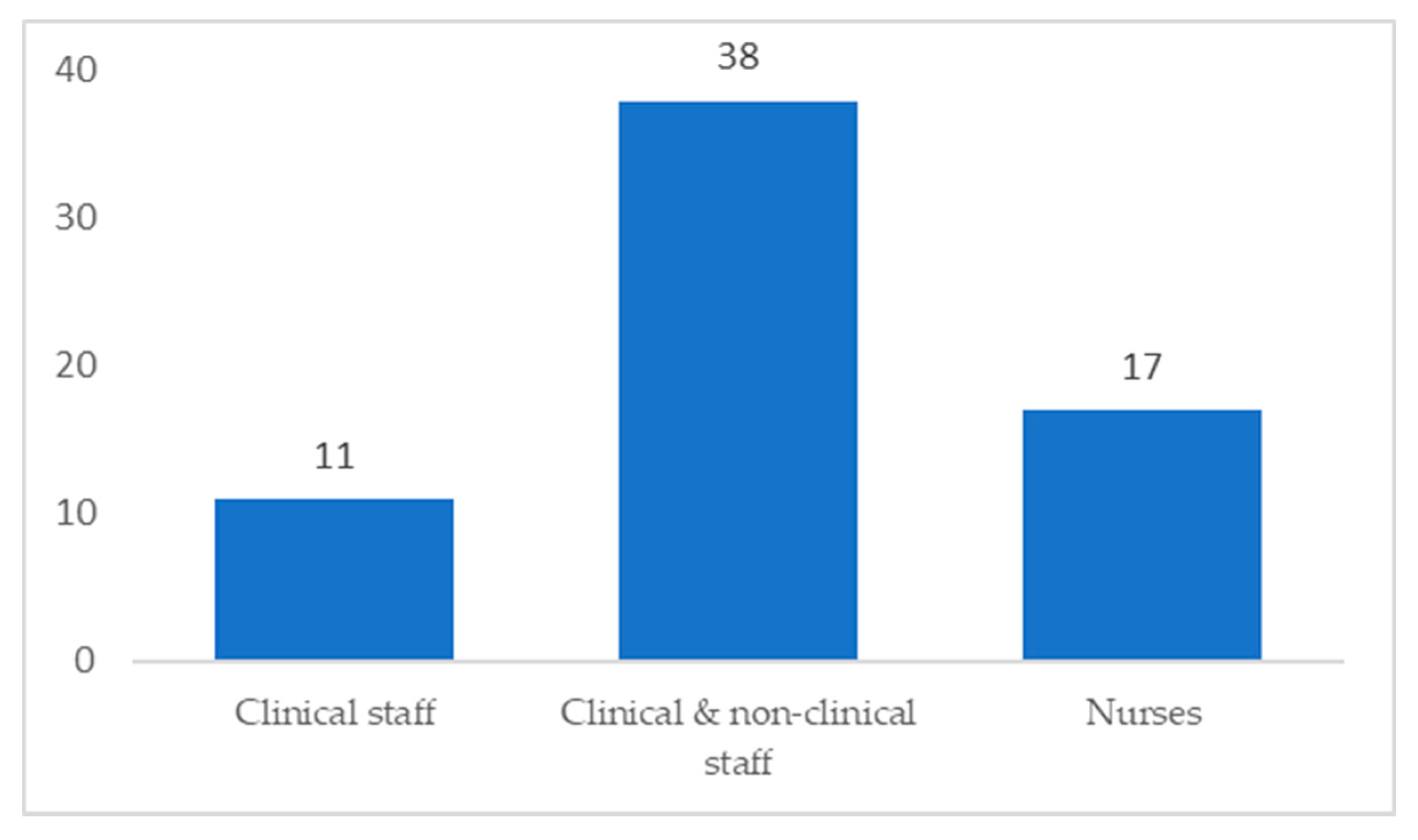
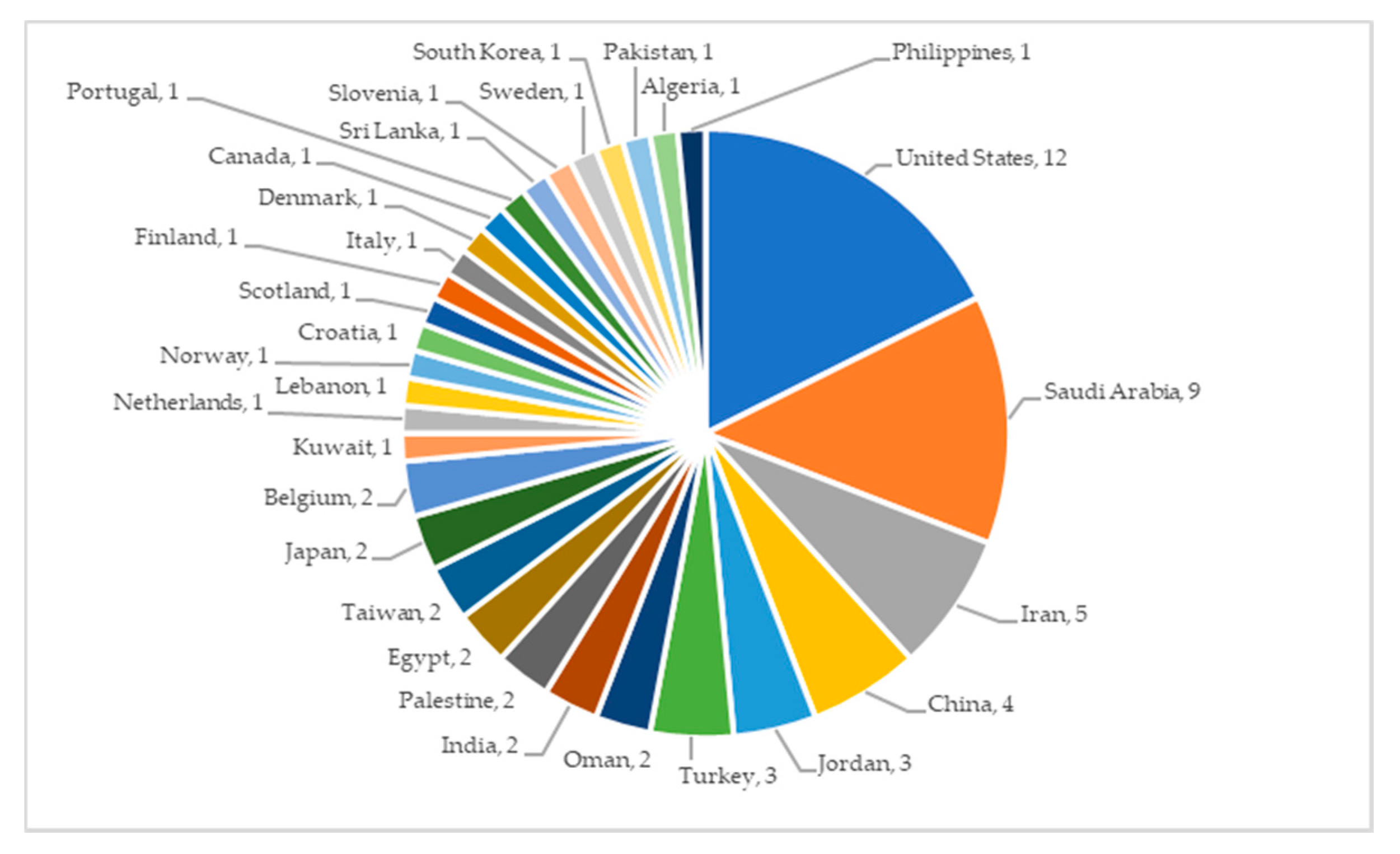
3. Results
4. Discussion
4.1. PSC Instruments
4.1.1. Hospital Survey on Patient Safety Culture (HSPSC)
4.1.2. Safety Attitudes Questionnaire (SAQ)
4.1.3. Patient Safety Climate in Health Care Organizations (PSCHO)
4.1.4. Scottish Hospital Safety Questionnaire (SHSQ)
4.1.5. Modified Stanford Instrument-2006
4.2. PSC Dimensions
4.2.1. Teamwork
4.2.2. Organizational and Behavioral Learning
4.2.3. Reporting of Errors and Safety Awareness
4.2.4. Gender and Demographics
4.2.5. Work Experience
4.2.6. Staffing
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Colla, J.B.; Bracken, A.C.; Kinney, L.M.; Weeks, W.B. Measuring Patient Safety Climate: A Review of Surveys. Qual. Saf. Health Care 2005, 364–366. [Google Scholar] [CrossRef]
- Gaal, S.; Verstappen, W.; Wolters, R.; Lankveld, H.; van Weel, C.; Wensing, M. Prevalence and Consequences of Patient Safety Incidents in General Practice in the Netherlands: A Retrospective Medical Record Review Study. Implement. Sci. 2011, 6. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Road Safety: Time for Action; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Nieva, V.F.; Sorra, J. Safety Culture Assessment: A Tool for Improving Patient Safety in Healthcare Organizations. BMJ Qual. Saf. 2003, 12, ii17–ii23. [Google Scholar] [CrossRef] [PubMed]
- González-Formoso, C.; Martín-Miguel, M.V.; Fernández-Domínguez, M.J.; Rial, A.; Lago-Deibe, F.I.; Ramil-Hermida, L.; Pérez-García, M.; Clavería, A. Adverse Events Analysis as an Educational Tool to Improve Patient Safety Culture in Primary Care: A Randomized Trial. BMC Fam. Pract. 2011, 12. [Google Scholar] [CrossRef]
- Kohn, L.T.; Corrigan, J.; Donaldson, M.S. To Err Is Human: Building a Safer Health System; National Academies Press: Washington, DC, USA, 1999. [Google Scholar]
- Ghobashi, M.M.; El-Ragehy, H.A.G.; Mosleh, H.; Al-Doseri, F.A. Assessment of Patient Safety Culture in Primary Health Care Settings in Kuwait. Epidemiol. Biostat. Public Health 2014, 11, e9101-1–e9101-9. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 21, e1000097. [Google Scholar]
- Hawker, S.; Payne, S.; Kerr, C.; Hardey, M.; Powell, J. Appraising the Evidence: Reviewing Disparate Data Systematically. Qual. Health Res. 2002, 12, 1284–1299. [Google Scholar] [CrossRef]
- Elamin, M.B.; Flynn, D.N.; Bassler, D.; Briel, M.; Alonso-Coello, P.; Karanicolas, P.J.; Guyatt, G.H.; Malaga, G.; Furukawa, T.A.; Kunz, R.; et al. Choice of Data Extraction Tools for Systematic Reviews Depends on Resources and Review Complexity. J. Clin. Epidemiol. 2009, 506–510. [Google Scholar] [CrossRef] [PubMed]
- Tacconelli, E. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. Lancet Infect. Dis. 2010, 10, 226. [Google Scholar] [CrossRef]
- Alshammari, F.; Pasay-an, E.; Alboliteeh, M.; Alshammari, M.H.; Susanto, T.; Villareal, S.; Indonto, M.C.L.; Gonzales, F. A Survey of Hospital Healthcare Professionals’ Perceptions toward Patient Safety Culture in Saudi Arabia. Int. J. Afr. Nurs. Sci. 2019, 11. [Google Scholar] [CrossRef]
- Aljabri, D.I. Assessment of Patient Safety Culture in Saudi Hospital in Eastern Region, Aljabri, 2012. J. King Abdulaziz Univ. Med. Sci. 2012, 19, 43–58. [Google Scholar]
- Güneş, Ü.Y.; Gürlek, Ö.; Sönmez, M. A Survey of the Patient Safety Culture of Hospital Nurses in Turkey. Collegian 2016, 23, 225–232. [Google Scholar] [CrossRef]
- Abdelhai, R.; Abdelaziz, S.B.; Ghanem, N.S. Assessing Patient Safety Culture And Factors Affecting It Among Health Care Providers At Cairo University Hospitals. J. Am. Sci. 2012, 8, 277–285. [Google Scholar]
- Aboshaiqah, A.E.; Baker, O.G. Assessment of Nurses’ Perceptions of Patient Safety Culture in a Saudi Arabia Hospital. J. Nurs. Care Qual. 2013, 28, 272–280. [Google Scholar] [CrossRef]
- Aboul-Fotouh, A.M.; Ismail, N.A.; Elarab, H.S.E.; Wassif, G.O. Assessment of Patient Safety Culture among Health-Care Providers at a Teaching Hospital in Cairo, Egypt. East. Mediterr. Health J. 2012, 18, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Moussavi, F.; Moghri, J.; Gholizadeh, Y.; Karami, A.; Najjari, S.; Mehmandust, R.; Asghari, M.; Asghari, H. Assessment of Patient Safety Culture among Personnel in the Hospitals Associated with Islamic Azad University in Tehran in 2013. Electron. Phys. 2013, 5, 664. [Google Scholar] [CrossRef]
- Hamdan, M.; Saleem, A.A. oof. Assessment of Patient Safety Culture in Palestinian Public Hospitals. Int. J. Qual. Health Care 2013, 25, 167–175. [Google Scholar] [CrossRef]
- Alahmadi, H.A. Assessment of Patient Safety Culture in Saudi Arabian Hospitals. Qual. Saf. Health Care 2010, 19. [Google Scholar] [CrossRef]
- El-Sayed Desouky, D.; Alraqi, A.; Alsofyani, R.; Alghamdi, N. Assessment of Patient Safety Culture in Tertiary Health Care Settings in Taif City, Saudi Arabia. Middle East J. Fam. Med. 2019, 17, 4–11. [Google Scholar]
- Ali, H.; Ibrahem, S.Z.; al Mudaf, B.; al Fadalah, T.; Jamal, D.; El-Jardali, F. Baseline Assessment of Patient Safety Culture in Public Hospitals in Kuwait. BMC Health Serv. Res. 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Al-Awa, B.; al Mazrooa, A.; Rayes, O.; el Hati, T.; Devreux, I.; Al-Noury, K.; Habib, H.; El-Deek, B.S. Benchmarking the Post-Accreditation Patient Safety Culture at King Abdulaziz University Hospital. Ann. Saudi Med. 2012, 32, 143–150. [Google Scholar] [CrossRef]
- Alswat, K.; Abdalla, R.A.M.; Titi, M.A.; Bakash, M.; Mehmood, F.; Zubairi, B.; Jamal, D.; El-Jardali, F. Improving Patient Safety Culture in Saudi Arabia (2012–2015): Trending, Improvement and Benchmarking. BMC Health Serv. Res. 2017, 17. [Google Scholar] [CrossRef]
- Bahrami, M.A.; Chalak, M.; Montazeralfaraj, R.; Dehghani Tafti, A. Iranian Nurses’ Perception of Patient Safety Culture. Iran. Red Crescent Med. J. 2014, 16. [Google Scholar] [CrossRef] [PubMed]
- Khater, W.A.; Akhu-Zaheya, L.M.; Al-Mahasneh, S.I.; Khater, R. Nurses’ Perceptions of Patient Safety Culture in Jordanian Hospitals. Int. Nurs. Rev. 2015, 62, 82–91. [Google Scholar] [CrossRef]
- Elsous, A.; Akbari Sari, A.; AlJeesh, Y.; Radwan, M. Nursing Perceptions of Patient Safety Climate in the Gaza Strip, Palestine. Int. Nurs. Rev. 2017, 64, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Ammouri, A.A.; Tailakh, A.K.; Muliira, J.K.; Geethakrishnan, R.; al Kindi, S.N. Patient Safety Culture among Nurses. Int. Nurs. Rev. 2015, 62, 102–110. [Google Scholar] [CrossRef]
- Al-Mandhari, A.; Al-Zakwani, I.; Al-Kindi, M.; Tawilah, J.; Dorvlo, A.S.S.; Al-Adawi, S. Patient Safety Culture Assessment in Oman. Oman Med. J. 2014, 29, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Davoodi, R.; Shabestari, M.M.; Tak-Biri, A.; Soltanifar, A.; Sabouri, G.; Rahmani, S.; Moghiman, T. Patient Safety Culture Based on Medical Staff Attitudes in Khorasan Razavi Hospitals, Northeastern Iran. Iran. J. Public Health 2013, 42, 1292. [Google Scholar] [PubMed]
- Bahrami, M.A.; Montazeralfaraj, R.; Chalak, M.; Tafti, A.D.; Tehrani, G.A.; Ardakani, S.E. Patient Safety Culture Challenges: Survey Results of Iranian Educational Hospitals. Middle East J. Sci. Res. 2013, 14, 641–649. [Google Scholar] [CrossRef]
- El-Jardali, F.; Sheikh, F.; Garcia, N.A.; Jamal, D.; Abdo, A. Patient Safety Culture in a Large Teaching Hospital in Riyadh: Baseline Assessment, Comparative Analysis and Opportunities for Improvement. BMC Health Serv. Res. 2014, 14. [Google Scholar] [CrossRef]
- Top, M.; Tekingündüz, S. Patient Safety Culture in a Turkish Public Hospital: A Study of Nurses’ Perceptions about Patient Safety. Systemic Pract. Action Res. 2015, 28, 87–110. [Google Scholar] [CrossRef]
- Kiaei, M.Z.; Ziaee, A.; Mohebbifar, R.; Khoshtarkib, H.; Ghanati, E.; Ahmadzadeh, A.; Teymoori, S.; Khosravizadeh, O.; Zieaeeha, M. Patient Safety Culture in Teaching Hospitals in Iran: Assessment by the Hospital Survey on Patient Safety Culture (HSOPSC). J. Health Manag. Inf. Sci. 2016, 3, 51–56. [Google Scholar]
- Ugurluoglu, O.; Ugurluoglu, E.; Payziner, P.D.; Ozatkan, Y. Patient Safety Culture IN TURKEY, Ugurluoglu, 2012, Pakistan. J. Med. Sci. Q. 2012, 28, 463–467. [Google Scholar]
- El-Jardali, F.; Jaafar, M.; Dimassi, H.; Jamal, D.; Hamdan, R. The Current State of Patient Safety Culture in Lebanese Hospitals: A Study at Baseline. Int. J. Qual. Health Care 2010, 22, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Fujita, S.; Seto, K.; Ito, S.; Matsumoto, K.; Huang, C.C.; Hasegawa, T. The Impact of Nurse Working Hours on Patient Safety Culture: A Cross-National Survey Including Japan, the United States and Chinese Taiwan Using the Hospital Survey on Patient Safety Culture. BMC Health Serv. Res. 2013, 13. [Google Scholar] [CrossRef] [PubMed]
- Fujita, S.; Seto, K.; Ito, S.; Wu, Y.; Huang, C.-C.; Hasegawa, T. The Characteristics of Patient Safety Culture in Japan, Taiwan and the United States. BMC Health Serv. Res. 2013, 13, 1–10. [Google Scholar] [CrossRef]
- Chakravarty, B.A.; Sahu, M.A.; Biswas, B.M.; Chatterjee, S.C.K.; Rath, S. A Study of Assessment of Patient Safety Climate in Tertiary Care Hospitals. Med. J. Armed. Forces India 2015, 71, 152–157. [Google Scholar] [CrossRef]
- Danielsson, M.; Rutberg, H.; Årestedt, K. A National Study of Patient Safety Culture in Hospitals in Sweden. J. Patient Saf. 2017, 15, 328. [Google Scholar] [CrossRef] [PubMed]
- Wagner, C.; Smits, M.; Sorra, J.; Huang, C.C. Assessing Patient Safety Culture in Hospitals across Countries. Int. J. Qual. Health Care 2013, 25, 213–221. [Google Scholar] [CrossRef]
- Jafree, S.R.; Zakar, R.; Zakar, M.Z.; Fischer, F. Assessing the Patient Safety Culture and Ward Error Reporting in Public Sector Hospitals of Pakistan. Saf. Health 2017, 3. [Google Scholar] [CrossRef]
- Ito, S.; Seto, K.; Kigawa, M.; Fujita, S.; Hasagawa, T.; Hasegawa, T. Development and Applicability of Hospital Survey on Patient Safety Culture (HSOPS) in Japan. BMC Health Serv. Res. 2011, 11. [Google Scholar] [CrossRef] [PubMed]
- Brborović, H.; Šklebar, I.; Brborović, O.; Brumen, V.; Mustajbegović, J. Development of a Croatian Version of the US Hospital Survey on Patient Safety Culture Questionnaire: Dimensionality and Psychometric Properties. Postgrad. Med. J. 2014, 90, 125–132. [Google Scholar] [CrossRef]
- Amarapathy, M.; Sridharan, S.; Perera, R.; Handa, Y. Factors Affecting Patient Safety Culture in A Tertiary Care Hospital In Sri Lanka. Int. J. Sci. Technol. Res. 2013, 2, 173–180. [Google Scholar]
- Feng, X.; Bobay, K.; Krejci, J.W.; Mccormick, B.L. Factors Associated with Nurses’ Perceptions of Patient Safety Culture in China: A Cross-Sectional Survey Study. J. Evid. Based Med. 2012, 5, 50–56. [Google Scholar] [CrossRef]
- Nie, Y.; Mao, X.; Cui, H.; He, S.; Li, J.; Zhang, M. Hospital Survey on Patient Safety Culture in China. BMC Health Serv. Res. 2013, 13. [Google Scholar] [CrossRef]
- Robida, A. Hospital Survey on Patient Safety Culture in Slovenia: A Psychometric Evaluation. Int. J. Qual. Health Care 2013, 25, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Hellings, J.; Schrooten, W.; Klazinga, N.S.; Vleugels, A. Improving Patient Safety Culture. Int. J. Health Care Qual. Assur. 2010, 23, 489–506. [Google Scholar] [CrossRef]
- Olsen, E. Influence from Organisational Factors on Patient Safety and Safety Behaviour among Nurses and Hospital Staff. Int. J. Organ. Anal. 2018, 26, 382–395. [Google Scholar] [CrossRef]
- Chen, I.-C.; Li, H.-H. Measuring Patient Safety Culture in Taiwan Using the Hospital Survey on Patient Safety Culture (HSOPSC). BMC Health Serv. Res. 2010, 10, 152. [Google Scholar] [CrossRef]
- Sorra, J.S.; Dyer, N. Multilevel Psychometric Properties of the AHRQ Hospital Survey on Patient Safety Culture. BMC Health Serv. Res. 2010, 10, 199. [Google Scholar] [CrossRef]
- Zaheer, S.; Ginsburg, L.; Chuang, Y.T.; Grace, S.L. Patient Safety Climate (PSC) Perceptions of Frontline Staff in Acute Care Hospitals: Examining the Role of Ease of Reporting, Unit Norms of Openness, and Participative Leadership. Health Care Manag. Rev. 2015, 40, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Agnew, C.; Flin, R.; Mearns, K. Patient Safety Climate and Worker Safety Behaviours in Acute Hospitals in Scotland. J. Saf. Res. 2013, 45, 95–101. [Google Scholar] [CrossRef]
- Ramos, R.R.; Calidgid, C.C. Patient Safety Culture among Nurses at a Tertiary Government Hospital in the Philippines. Appl. Nurs. Res. 2018, 44, 67–75. [Google Scholar] [CrossRef]
- Bagnasco, A.; Tibaldi, L.; Chirone, P.; Chiaranda, C.; Panzone, M.S.; Tangolo, D.; Aleo, G.; Lazzarino, L.; Sasso, L. Patient Safety Culture: An Italian Experience. J. Clin. Nurs. 2011, 20, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.M.; Choi, J.S. Patient Safety Culture Associated With Patient Safety Competencies among Registered Nurses. J. Nurs. Scholarsh. 2018, 50, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Turunen, H.; Partanen, P.; Kvist, T.; Miettinen, M.; Vehviläinen-Julkunen, K. Patient Safety Culture in Acute Care: A Web-Based Survey of Nurse Managers’ and Registered Nurses’ Views in Four Finnish Hospitals. Int. J. Nurs. Pract. 2013, 19, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Rajalatchumi, A.; Ravikumar, T.S.; Muruganandham, K.; Thulasingam, M.; Selvaraj, K.; Reddy, M.M.; Jayaraman, B. Perception of Patient Safety Culture among Health-Care Providers in a Tertiary Care Hospital, South India. J. Nat. Sci. Biol. Med. 2018, 9, 14–18. [Google Scholar] [CrossRef]
- Zhao, X.; Liu, W.; Wang, Y.; Zhang, L. Survey and Analysis of Patient Safety Culture in a County Hospital. Fam. Med. Community Health 2017, 5, 299–310. [Google Scholar] [CrossRef]
- Zhou, P.; Bundorf, M.K.; Gu, J.; He, X.; Xue, D. Survey on Patient Safety Climate in Public Hospitals in China. BMC Health Serv. Res. 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Eiras, M.; Escoval, A.; Grillo, I.M.; Silva-Fortes, C. The Hospital Survey on Patient Safety Culture in Portuguese Hospitals: Instrument Validity and Reliability. Int. J. Health Care Qual. Assur. 2014, 27, 111–122. [Google Scholar] [CrossRef]
- Abualrub, R.F.; Abu Alhijaa, E.H. The Impact of Educational Interventions on Enhancing Perceptions of Patient Safety Culture among Jordanian Senior Nurses. Nurs. Forum 2014, 49, 139–150. [Google Scholar] [CrossRef]
- Saleh, A.M.; Darawad, M.W.; Al-Hussami, M. The Perception of Hospital Safety Culture and Selected Outcomes among Nurses: An Exploratory Study. Nurs. Health Sci. 2015, 17, 339–346. [Google Scholar] [CrossRef]
- Kristensen, S.; Badsberg, J.H.; Rigshospitalet, J.A.; Bartels, P. The Patient Safety Climate in Danish Hospital Units CoCo-Graphical Models View Project Deepening Our Understanding of Quality Improvement in Europe (DUQuE) View Project. Danish Med. J. 2015, 62, A5153. [Google Scholar]
- Vlayen, A.; Schrooten, W.; Wami, W.; Cand, P.; Aerts, M.; Barrado, L.G.; Claes, N.; Hellings, J. Variability of Patient Safety Culture in Belgian Acute Hospitals. J. Patient Saf. 2015, 11, 110–121. [Google Scholar] [CrossRef]
- Boughaba, A.; Aberkane, S.; Fourar, Y.O.; Djebabra, M. Study of Safety Culture in Healthcare Institutions: Case of an Algerian Hospital. Int. J. Health Care Qual. Assur. 2019, 32, 1081–1097. [Google Scholar] [CrossRef]
- Blegen, M.A.; Gearhart, S.; O_Brien, R.; Sehgal, N.L.; Alldredge, B.K. AHRQ’s Hospital Survey on Patient Safety Culture: Psychometric Analyses. J. Patient Saf. 2009, 5, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Etchegaray, J.M.; Thomas, E.J. Comparing Two Safety Culture Surveys: Safety Attitudes Questionnaire and Hospital Survey on Patient Safety. BMJ Qual. Saf. 2012, 21, 490–498. [Google Scholar] [CrossRef]
- Mardon, R.E.; Khanna, K.; Sorra, J.; Dyer, N.; Famolaro, T. Exploring Relationships between Hospital Patient Safety Culture and Adverse Events. J. Patient Saf. 2010, 6, 226–232. [Google Scholar] [CrossRef]
- Lee, S.H.; Phan, P.H.; Dorman, T.; Weaver, S.J.; Pronovost, P.J. Handoffs, Safety Culture, and Practices: Evidence from the Hospital Survey on Patient Safety Culture. BMC Health Serv. Res. 2016, 16. [Google Scholar] [CrossRef] [PubMed]
- McFadden, K.L.; Henagan, S.C.; Gowen, C.R. The Patient Safety Chain: Transformational Leadership’s Effect on Patient Safety Culture, Initiatives, and Outcomes. J. Oper. Manag. 2009, 27, 390–404. [Google Scholar] [CrossRef]
- Sexton, J.B.; Helmreich, R.L.; Neilands, T.B.; Rowan, K.; Vella, K.; Boyden, J.; Roberts, P.R.; Thomas, E.J. The Safety Attitudes Questionnaire: Psychometric Properties, Benchmarking Data, and Emerging Research. BMC Health Serv. Res. 2006, 6. [Google Scholar] [CrossRef] [PubMed]
- Singer, S.; Meterko, M.; Baker, L.; Gaba, D.; Falwell, A.; Rosen, A. Workforce Perceptions of Hospital Safety Culture: Development and Validation of the Patient Safety Climate in Healthcare Organizations Survey. Health Serv. Res. 2007, 1999–2021. [Google Scholar] [CrossRef] [PubMed]
- Singer, S.; Lin, S.; Falwell, A.; Gaba, D.; Baker, L. Relationship of Safety Climate and Safety Performance in Hospitals. Health Serv. Res. 2009, 44, 399–421. [Google Scholar] [CrossRef]
- Hansen, L.O.; Williams, M.V.; Singer, S.J. Perceptions of Hospital Safety Climate and Incidence of Readmission. Health Serv. Res. 2011, 46, 596–616. [Google Scholar] [CrossRef] [PubMed]
- Singer, S.J.; Falwell, A.; Gaba, D.M.; Baker, L.C. Patient Safety Climate in US Hospitals: Variation by Management Level. Med. Care 2008, 46, 1149–1150. [Google Scholar] [CrossRef] [PubMed]


| Row | Step |
|---|---|
| Keywords 1 | “safety culture” OR “safety climate” OR “patient safety culture” OR “patient safety climate” OR “patient safety” |
| Keywords 2 | “perception” OR “measure” OR “evaluate” or “assess” OR “survey” OR “instrument ” OR “tool” |
| Keywords 3 | “hospital ” OR “teaching” OR “tertiary” |
| Keywords 4 | “nurse” OR “doctor” OR “physician” OR “staff” OR “health professional” |
| Search | #1 AND #2 AND #3 AND #4 |
| Instrument/Year/Country/Reference | Aim(s) | Strength(s) | Limitation(s) | Finding(s) | Quality Score |
|---|---|---|---|---|---|
| HSPSC, 2019, Saudi Arabia [12] | Investigate the perceptions of healthcare professionals toward PSC in hospitals throughout the Hail region |
| Only four hospitals considered for data collection. |
| 32 |
| HSPSC, 2012, Saudi Arabia, [13] | Identify general strengths and recognize areas of patient safety improvements |
| Response rate among participants was 61%. Only two general hospitals considered |
| 27 |
| HSPSC, 2016, Turkey, [14] | Explore and describe nurses’ perceptions of PSC |
| Only nurses in four hospitals (one university hospital and three general hospitals), and nurses consiered for collecting data |
| 27 |
| HSPSC, 2012, Egypt, [15] | Assess PSC perceptions among healthcare providers and identify factors that may critically affect PSC |
| No response rate reported |
| 27 |
| HSPSC, 2013, Saudi Arabia, [16] | Identify factors that nurses perceive as contributing to the PSC |
| Only Nurses in one Tertiary care hospital considered for collecting data. |
| 28 |
| HSPSC, 2012, Egypt, [17] | Assess healthcare providers’ perceptions of PSC within the organization and determine factors that play a role in PSC |
|
| 29 | |
| HSPSC, 2013, Iran, [18] | Assess the PSC at Islamic Azad University hospitals |
|
| 24 | |
| HSPSC, 2013. Palestine, [19] | Assess the prevalent PSC in Palestinian public hospitals |
| Response rate was 51.2% |
| 25 |
| HSPSC, 2010, Saudi Arabia, [20] | Evaluate the extent to which the culture supports patient safety at Saudi hospitals |
|
| 31 | |
| HSPSC, 2019, Saudi Arabia, [21] | Evaluate the PSC in Saudi hospitals and improve patient safety and quality of care by implementing safety systems and creating a culture of safety |
| Only one Tertiary hospital considered |
| 25 |
| HSPSC, 2018, Kuwait, [22] | Examine the association between the predictors and outcomes of PSC |
| Response rate was 60.5% |
| 33 |
| HSPSC, 2012, Saudi Arabia, [23] | Perform an unbiased assessment of the impact of accreditation on PSC |
| Only nurses in one university hospital considered for collecting data |
| 30 |
| HSPSC, 2017, Saudi Arabia, [24] | Reassess PSC in a large multi-site healthcare facility in Riyadh, Kingdom of Saudi Arabia, and compare it with an earlier assessment conducted in 2012, benchmarked against regional and international studies |
| Only one Tertiary care teaching hospital considered. Response rate was 56.7% |
| 33 |
| HSPSC, 2014, Iran, [25] | Assess the safety culture in two educational hospitals |
| Only nurses in two teaching hospitals considered |
| 29 |
| HSPSC, 2015, Jordan, [26] | Assess PSC in Jordanian hospitals from nurses’ perspectives |
| Only nurses considered |
| 34 |
| SAQ, 2017, Palestine, [27] | Assess the perception of nurses regarding PSC and determine whether it is significantly affected by the nurses’ position, age, experience, and working hours |
| Only nurses in four public general hospitals considered |
| 33 |
| HSPSC, 2015, Oman, [28] | Investigate nurses’ perceptions of PSC and identify the factors needed to develop and maintain a culture of safety among nurses | Only nurses in four governmental hospitals considered. No Response rate reported. |
| 33 | |
| HSPSC, 2014, Oman, [29] | Illustrate the PSC in Oman and compare the average positive response rates in PSC between Oman and the U.S., Taiwan, and Lebanon |
| Only five secondary and tertiary care hospitals considered. No Response rate reported. |
| 33 |
| HSPSC, 2013, Iran, [30] | Estimate the relation between PSC and three characteristics of teaching hospitals (number of beds, education condition, and proficiency status) |
|
| 29 | |
| HSPSC, 2013, Iran, [31] | Assess nurses’ perceptions of PSC in these hospitals |
| Only nurses in two teaching hospital sconsidered |
| 21 |
| HSPSC, 2014, Saudi Arabia, [32] | Present findings of a baseline assessment of PSC, compare results with regional and international studies, and explore the association between PSC predictors and outcomes, considering respondent characteristicsand facility size |
| Only one tertiary care university teaching hospital considered |
| 34 |
| HSPSC, 2015, Turkey, [33] | Investigate nurses’ perceptions of PSC |
| Only nurses in one public hospital considered for collecting data |
| 30 |
| HSPSC, 2016, Iran, [34] | Evaluate the current status of PSC among hospitals in three central Iran provinces |
| No Response rate reported |
| 21 |
| HSPSC, 2012, Turkey, [35] | Assess health personnel perspectives of PSC in a 900-bed university hospital in Ankara, Turkey |
| Only one university hospital considered. Response rate was 43% |
| 21 |
| HSPSC, 2010, Lebanon, [36] | Conduct a baseline assessment of PSC in Lebanese hospitals |
| Response rate was 55.56% |
| 31 |
| HSPSC, 2013, Japan and Taiwan, [37] | Clarify the impact of long nurse working hours on PSC in Japan, the U.S., and Chinese Taiwan using HSPSC |
| Only nurses considered for collecting data. Response rate was Japan = 4047 (58.1%) U.S. = 106,710 (37.0%) Taiwan = 5714 (56.3%) |
| 29 |
| HSPSC, 2013, Japan and Taiwan, [38] | Investigate the characteristics of PSC in Japan, Taiwan, and the U.S. |
| Response rate in U.S. = 35.2% |
| 30 |
| SAQ, 2015, India, [39] | Explore composite patient safety climate, assess various dimensions of patient safety climate in three hospitals, and identify future directions for developing a strong safety climate |
| Only three tertiary care hospitals considered |
| 28 |
| HSPSC, 2017, Sweden, [40] | Investigate the PSC in all Swedish hospitals; compare the culture among managers, physicians, registered nurses, and enrolled nurses; and identify factors associated with high overall patient safety |
| Only three work areas: general wards, emergency care, and psychiatry care considered. Response rate was 47.4% |
| 30 |
| HSPSC, 2013 Netherlands, [41] | Examine similarities and differences in hospital PSC in three countries: the Netherlands, the U.S., and Taiwan |
| U.S. Response rate was 52% |
| 24 |
| HSPSC, 2017, Pakistan, [42] | Present descriptive statistics for patient safety standards | Only two public hospitals considered. Response rate was 38.4% |
| 21 | |
| HSPSC, 201,, Japan, [43] | Examine the validity and applicability of the HSPSC in Japan and compare the factor structure to the original U.S. study |
|
| 31 | |
| HSPSC, 2013, Croatia, [44] | Determine whether all 12 dimensions of the U.S. HSPSC are applicable, valid, and reliable for Croatian healthcare workers |
| Only four Croatian hospitals considered. Response rate was 32.69% |
| 33 |
| HSPSC, 2013, Sri Lanka, [45] | Assess the current PSC in a tertiary care hospital |
| Considering only one tertiary care hospital. No Response rate reported |
| 28 |
| HSPSC, 2012, China, [46] | Explore nurses’ perceptions of PSC and factors associated with those perceptions | Considering only nurses in one university teaching hospital. No Response ratereported |
| 30 | |
| HSPSC, 2013, China, [47] | Explore the attitudes and perceptions of PSC for healthcare workers in China and compare the psychometric properties of an adapted translation of the HSPSC in Chinese hospitals with those of the U.S. |
|
| 30 | |
| HSPSC, 2013, Slovenia, [48] | Study the psychometric properties of a translated version of the HSPSC in a Slovenian setting |
| Considering only three acute general hospitals. Response rate was 55% |
| 28 |
| HSPSC, 2010, Belgium, [49] | Describe a PSC improvement approach in five Belgian hospitals |
| Five Belgian acute hospitals (three private hospitals and one public hospital) |
| 31 |
| HSPSC, 2017, Norway, [50] | Explore organizational factors influencing patient safety and safety behavior among nurses and other hospital staff |
| Considering only one university hospital. Response rate was 49% |
| 34 |
| HSPSC, 2010, Taiwan, [51] | Assess the PSC in Taiwan and attempt to provide an explanation for some of the phenomena that are unique in Taiwan |
|
| 35 | |
| HSPSC, 2010, U.S., [52] | Examine the multilevel psychometric properties of the survey |
| Response rate was 55% |
| 33 |
| MSI-2006, 2015, Canada, [53] | Examine in detail how ease of reporting, unit norms of openness, and participative leadership influence front-line staff perceptions of PSC within healthcare organizations |
|
| 35 | |
| SHSQ, 2013, Scotland, [54] | Obtain a measure of hospital safety climate from a sample of National Health Service (NHS) acute hospitals in Scotland and determine whether these scores are associated with worker safety behaviors and patient and worker injuries |
| Considering only six acute hospitals in Scotland. Response rate was 23% |
| 27 |
| HSPSC, 2018, Philippines, [55] | Assess PSC among nurses at a government hospital |
| Only nurses in one tertiary government hospital considered |
| 29 |
| HSPSC, 2011, Italy, [56] | Determine the level of awareness regarding PSC among health professionals working at a hospital in northern Italy |
| Only one hospital in northern Italy considered. |
| 22 |
| HSPSC, 2018, South Korea [57] | Investigate the relationships between registered nurses’ perceptions of PSC in their workplace and their patient safety competency—attitudes, skills, and knowledge |
| Considering only nurses in in one university hospital |
| 28 |
| HSPSC, 2013, Finland, [58] | Explore and compare nurse managers’ s’ and registered nurses views on PSC to discover whether there are differences between their views |
| Considering only nurses in four acute care hospitals. Response rate was 17% |
| 27 |
| HSPSC, 2018, India, [59] | Assess the perceptions of PSC among healthcare providers at a public sector tertiary care hospital in South India |
| Considering only one tertiary government hospital |
| 28 |
| HSPSC, 2017, China, [60] | Use the HSPSC to survey PSC in a county hospital in Beijing to determine the strengths and weaknesses of PSC in this hospital |
| Considering only one county hospital. |
| 30 |
| PSCHO, 2015, China, [61] | Describe staff’s perceptions of PSC in public hospitals and determine how perceptions of PSC differ between different types of workers in the U.S. and China |
|
| 26 | |
| HSPSC, 2014, Portugal, [62] | Determine the validity and reliability of the AHRQ Hospital Survey on Patient Safety Culture (HSPSC) Portuguese version |
| Response rate was 21.8% |
| 24 |
| HSPSC, 2014, Jordan, [63] | Examine the impact of patient safety educational interventions among senior nurses on their perceptions of safety culture and the rate of reported adverse events, pressure ulcers, and patient falls |
| Considering only nurses in one specialized hospital. Response rate was 57% |
| 34 |
| HSPSC, 2015, Jordan, [64] | Examine nurses’ perceptions of the hospital safety culture in Jordan and identify the relationships between aspects of hospital safety culture and selected safety outcomes | Considering only nurses in five Jordanian hospitals. Response rate was 61% |
| 30 | |
| SAQ, 2015, Denmark, [65] | Describe and analyze the patient safety climate in 15 Danish hospital units |
| Considering only five hospitals |
| 26 |
| HSPSC, 2015, Belgium, [66] | Measure differences in safety culture perceptions within Belgian acute hospitals and examine variability based on language, work area, staff position, and work experience |
| Response rate was 51.7% |
| 30 |
| HSPSC, 2019, Algeria, [67] | Measure safety culture dimensions in order to improve and promote healthcare in Algeria |
| Considering only one General hospital. No Response rate reported |
| 25 |
| HSPSC, 2009, U.S., [68] | Analyze the psychometric properties of the Agency for Healthcare Research and Quality Hospital Survey on Patient Safety Culture (HSPSC) |
| Only three hospitals (an academic teaching hospital, a managed care organization hospital, and a private not-for-profit community hospital) considered |
| 32 |
| HSPSC and SAQ, 2012, U.S., [69] | Examine the reliability and predictive validity of two patient safety culture surveys- Safety Attitudes Questionnaire (SAQ) and Hospital Survey on Patient Safety Culture (HSPSC)-when administered to the same participants. Additionally, to determine the ability to convert HSOPS scores to SAQ scores. |
| Response rate was 54%. Only non-physician employees considered. |
| 34 |
| HSPSC, 2010, U.S., [70] | Examine relationships between the Agency for Healthcare Research and Quality’s (AHRQ) Hospital Survey of Patient Safety Culture and rates of in-hospital complications and adverse events as measured by the AHRQ Patient Safety Indicators (PSIs) |
|
| 28 | |
| HSPSC, 2016, U.S., [71] | Analyze how different elements of patient safety culture is associated with clinical handoffs and perceptions of patient safety |
|
| 35 | |
| HSPSC, 2009, U.S., [72] | Investigate the existence of a patient safety chain for hospitals |
| Response rate was 59.3%. |
| 26 |
| SAQ, 2006, U.S., UK, and NZ, [73] | Describe the survey’s background, psychometric characteristics, provide benchmarking data, discuss how the survey can be used, and note emerging areas of research |
|
| 30 | |
| PSCHO, 2007, U.S., [74] | Describe the development of an instrument for assessing workforce perceptions of hospital safety culture and to assess its reliability and validity |
| response rate was 51% |
| 29 |
| PSCHO, 2009, U.S., [75] | Examine the relationship between measures of hospital safety climate and hospital performance on selected Patient Safety Indicators (PSIs). |
| Response rate was 52%. |
| 31 |
| PSCHO, 2011, U.S., [76] | Define the relationship between hospital patient safety climate (a measure of hospitals’ organizational culture as related to patient safety) and hospitals’ rates of rehospitalization within 30 days of discharge |
| Response rate was 38.5 % |
| 24 |
| PSCHO, 2008, U.S., [77] | Determine whether frontline workers and supervisors perceive a more negative patient safety climate than senior managers in their institutions. |
|
| 34 |
| Survey | PSC Dimensions |
|---|---|
| HSPSC | Management support for PS Teamwork within units Teamwork across units Communication openness Frequency of events reported Feedback and communication about errors Organizational learning—continuous improvement Nonpunitive responses to errors Handoffs and transitions Staffing Supervisor/manager expectations and actions that promote PS Overall perceptions of PS |
| SAQ | Teamwork climate Safety climate Job satisfaction Stress recognition Perceptions of management Working conditions |
| PSCHO | Engagement of senior managers Organizational resources Overall emphasis on PS Unit safety norms Unit support and recognition for safety efforts Fear of blame Fear of shame |
| MSI | Organization leadership for safety Unit leadership for safety Perceived state of safety Shame and repercussions of reporting Safety learning behaviors |
| SHSQ | Supervisors’ expectations and actions Organizational learning/improvement Teamwork within hospital units Communication openness Feedback and communication about error Non-punitive responses to errors Staffing Hospital management support for PS Teamwork across hospital units Hospital handoffs Frequency of incident reporting Overall perceptions of safety |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Azyabi, A.; Karwowski, W.; Davahli, M.R. Assessing Patient Safety Culture in Hospital Settings. Int. J. Environ. Res. Public Health 2021, 18, 2466. https://doi.org/10.3390/ijerph18052466
Azyabi A, Karwowski W, Davahli MR. Assessing Patient Safety Culture in Hospital Settings. International Journal of Environmental Research and Public Health. 2021; 18(5):2466. https://doi.org/10.3390/ijerph18052466
Chicago/Turabian StyleAzyabi, Abdulmajeed, Waldemar Karwowski, and Mohammad Reza Davahli. 2021. "Assessing Patient Safety Culture in Hospital Settings" International Journal of Environmental Research and Public Health 18, no. 5: 2466. https://doi.org/10.3390/ijerph18052466
APA StyleAzyabi, A., Karwowski, W., & Davahli, M. R. (2021). Assessing Patient Safety Culture in Hospital Settings. International Journal of Environmental Research and Public Health, 18(5), 2466. https://doi.org/10.3390/ijerph18052466







