Non-Incised Papilla Surgical Approach and Leukocyte Platelet-Rich Fibrin in Periodontal Reconstruction of Deep Intrabony Defects: A Case Series
Abstract
1. Introduction
2. Materials and Methods
2.1. Pre-Surgical or Anti-Inflammatory Phase
2.2. Surgical Phase
2.3. Post-Surgical Phase
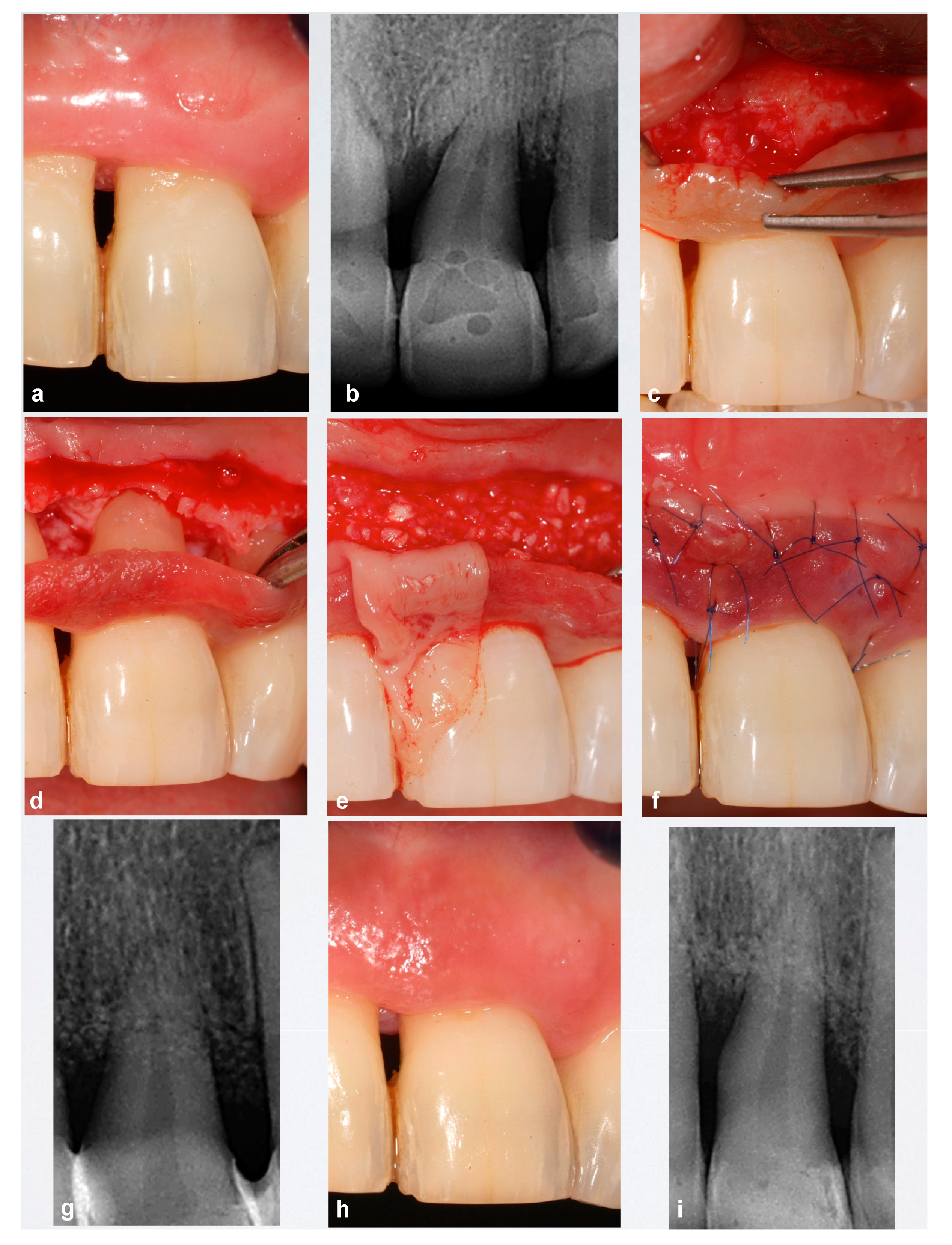
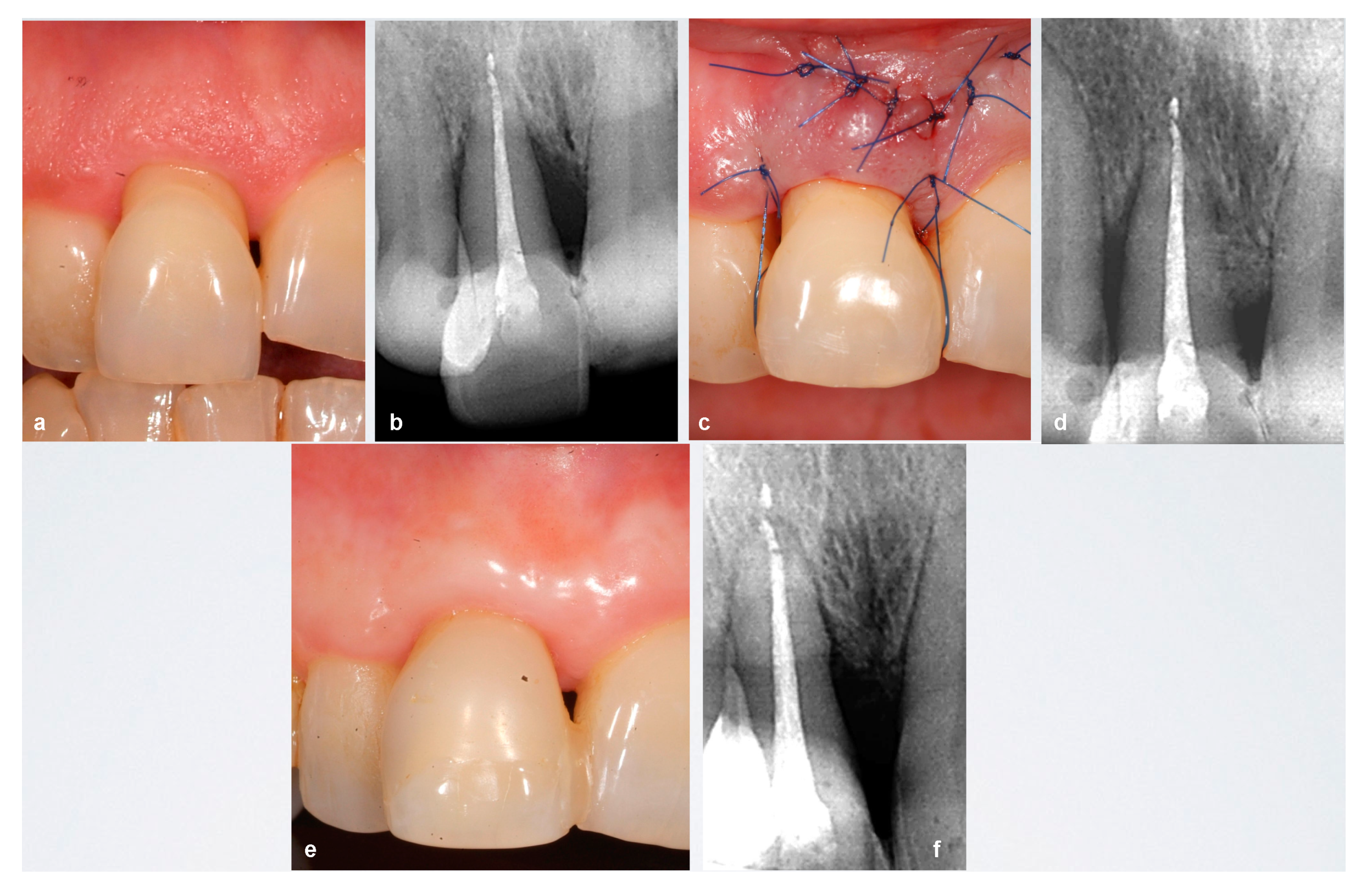
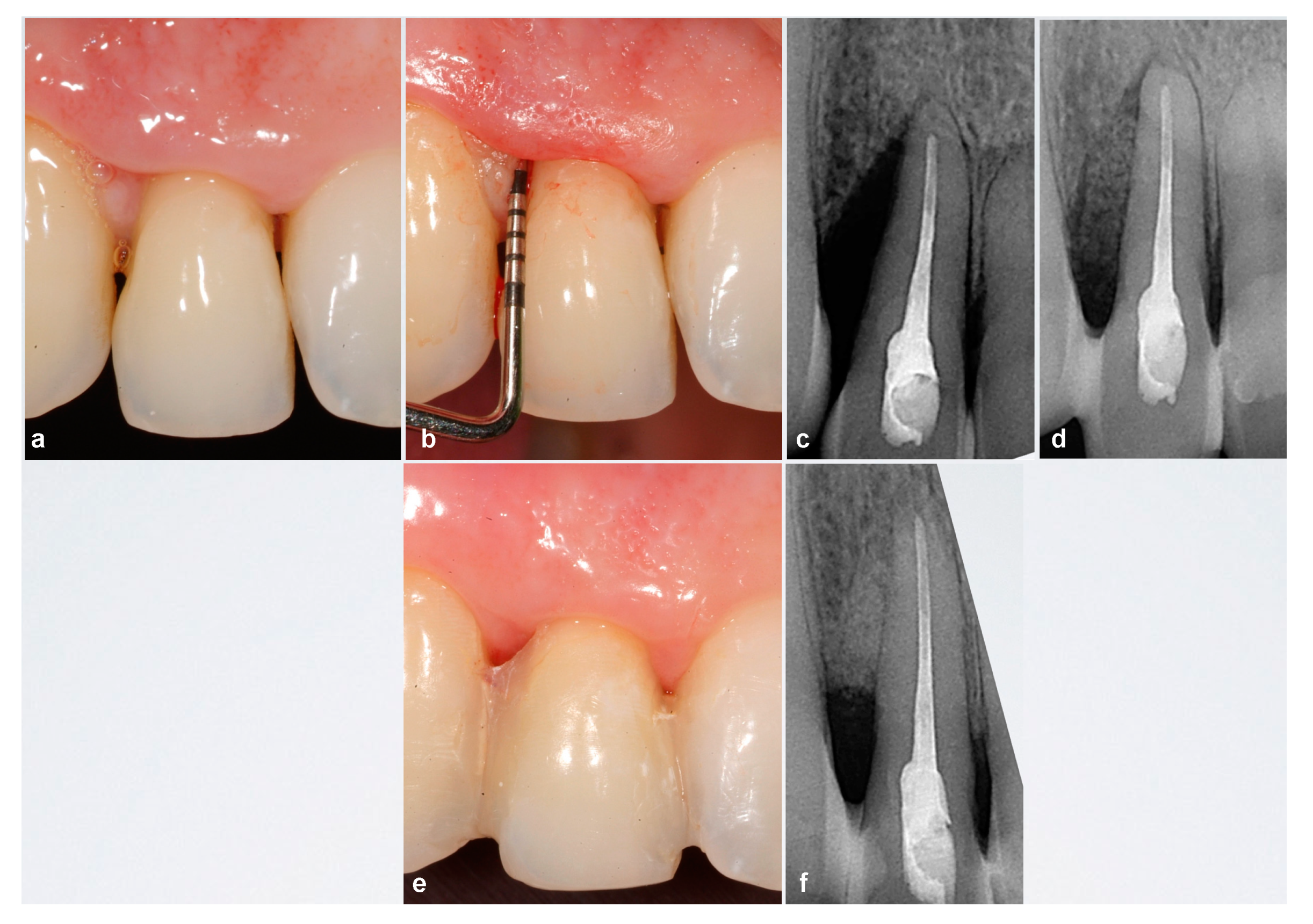
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Sculean, A.; Kiss, A.; Miliauskaite, A.; Schwarz, F.; Arweiler, N.B.; Hannig, M. Ten-year results following treatment of intra-bony defects with enamel matrix proteins and guided tissue regeneration. J. Clin. Periodontol. 2008, 35, 817–824. [Google Scholar] [CrossRef]
- Pretzl, B.; Kim, T.-S.; Steinbrenner, H.; Dörfer, C.; Himmer, K.; Eickholz, P. Guided tissue regeneration with bioabsorbable barriers III 10-year results in infrabony defects. J. Clin. Periodontol. 2009, 36, 349–356. [Google Scholar] [CrossRef]
- Prato, G.P.; Cortellini, P. Thirty-year stability after regeneration of a deep intrabony defect: A case report. J. Clin. Periodontol. 2016, 43, 857–862. [Google Scholar] [CrossRef]
- Wachtel, H.; Schenk, G.; Böhm, S.; Weng, D.; Zuhr, O.; Hürzeler, M.B. Microsurgical access flap and enamel matrix derivative for the treatment of periodontal intrabony defects: A controlled clinical study. J. Clin. Periodontol. 2003, 30, 496–504. [Google Scholar] [CrossRef]
- Cortellini, P.; Tonetti, M.S. A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intra-bony defects: A novel approach to limit morbidity. J. Clin. Periodontol. 2007, 34, 87–93. [Google Scholar] [CrossRef]
- Cortellini, P.; Nieri, M.; Prato, G.P.; Tonetti, M.S. Single minimally invasive surgical technique with an enamel matrix derivative to treat multiple adjacent intra-bony defects: Clinical outcomes and patient morbidity. J. Clin. Periodontol. 2008, 35, 605–613. [Google Scholar] [CrossRef]
- Cortellini, P.; Tonetti, M.S. Improved wound stability with a modified minimally invasive surgical technique in the regenera-tive treatment of isolated interdental intrabony defects. J. Clin. Periodontol. 2009, 36, 157–163. [Google Scholar] [CrossRef]
- Cortellini, P.; Tonetti, M.S. Clinical and radiographic outcomes of the modified minimally invasive surgical technique with and without regenerative materials: A randomized-controlled trial in intra-bony defects. J. Clin. Periodontol. 2011, 38, 365–373. [Google Scholar] [CrossRef]
- Trombelli, L.; Farina, R.; Franceschetti, G.; Calura, G. Single-Flap Approach with Buccal Access in Periodontal Reconstructive Procedures. J. Periodontol. 2009, 80, 353–360. [Google Scholar] [CrossRef]
- Trombelli, L.; Simonelli, A.; Pramstraller, M.; Wikesjö, U.M.E.; Farina, R. Single flap approach with and without guided tissue re-generation and a hydroxyapatite biomaterial in the management of intraosseous periodontal defects. J. Periodontol. 2010, 81, 1256–1263. [Google Scholar] [CrossRef]
- Trombelli, L.; Simonelli, A.; Schincaglia, G.P.; Cucchi, A.; Farina, R. Single-flap approach for surgical debridement of deep in-traosseous defects: A randomized controlled trial. J. Periodontol. 2012, 83, 27–35. [Google Scholar] [CrossRef]
- Trombelli, L.; Simonelli, A.; Minenna, L.; Rasperini, G.; Farina, R. Effect of a Connective Tissue Graft in Combination with a Single Flap Approach in the Regenerative Treatment of Intraosseous Defects. J. Periodontol. 2017, 88, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Farina, R.; Simonelli, A.; Rizzi, A.; Pramstraller, M.; Cucchi, A.; Trombelli, L. Early postoperative healing following buccal single flap approach to access intraosseous periodontal defects. Clin. Oral Investig. 2012, 17, 1573–1583. [Google Scholar] [CrossRef]
- Farina, R.; Simonelli, A.; Minenna, L.; Rasperini, G.; Trombelli, L. Single-flap approach in combination with enamel matrix deriva-tive in the treatment of periodontal intraosseous defects. Int. J. Periodontics Restor. Dent. 2014, 34, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Farina, R.; Simonelli, A.; Minenna, L.; Rasperini, G.; Schincaglia, G.P.; Tomasi, C.; Trombelli, L. Change in the Gingival Margin Profile After the Single Flap Approach in Periodontal Intraosseous Defects. J. Periodontol. 2015, 86, 1038–1046. [Google Scholar] [CrossRef]
- Mishra, A.; Avula, H.; Pathakota, K.R.; Avula, J. Efficacy of modified minimally invasive surgical technique in the treatment of human intrabony defects with or without use of rhPDGF-BB gel: A randomized controlled trial. J. Clin. Periodontol. 2013, 40, 172–179. [Google Scholar] [CrossRef]
- Schincaglia, G.P.; Hebert, E.; Farina, R.; Simonelli, A.; Trombelli, L. Single versus double flap approach in periodontal regenera-tive treatment. J. Clin. Periodontol. 2015, 42, 557–566. [Google Scholar] [CrossRef]
- Ferrarotti, F.; Romano, F.; Gamba, M.N.; Quirico, A.; Giraudi, M.; Audagna, M.; Aimetti, M. Human intrabony defect regeneration with micrografts containing dental pulp stem cells: A randomized controlled clinical trial. J. Clin. Periodontol. 2018, 45, 841–850. [Google Scholar] [CrossRef]
- Saito, A.; Bizenjima, T.; Takeuchi, T.; Suzuki, E.; Sato, M.; Yoshikawa, K.; Kitamura, Y.; Matsugami, D.; Aoki, H.; Kita, D.; et al. Treatment of intrabony periodontal defects using rhFGF-2 in combination with deproteinized bovine bone mineral or rhFGF-2 alone: A 6-month randomized controlled trial. J. Clin. Periodontol. 2019, 46, 332–341. [Google Scholar] [CrossRef]
- Moreno Rodriguez, J.A.; Caffesse, R.G. Nonincised Papillae Surgical Approach (NIPSA) in Periodontal Regeneration: Prelimi-nary Results of a Case Series. Int. J. Periodontics Restor. Dent. 2018, 38, 105–111. [Google Scholar] [CrossRef]
- Moreno Rodríguez, J.A.; Ortiz Ruiz, A.J.; Caffesse, R.G. Periodontal reconstructive surgery of deep intraosseous defects using an apical approach. Non-incised papillae surgical approach (NIPSA): A retrospective cohort study. J. Periodontol. 2019, 90, 454–464. [Google Scholar] [CrossRef] [PubMed]
- Moreno Rodríguez, J.A.; Ortiz Ruiz, A.J.; Zamora, G.P.; Pecci-Lloret, M.; Caffesse, R.G. Connective Tissue Grafts with Nonincised Papillae Surgical Approach for Periodontal Reconstruction in Noncontained Defects. Int. J. Periodontics Restor. Dent. 2019, 39, 781–787. [Google Scholar] [CrossRef]
- Burkhardt, R.; Magaz, V.R.; Hämmerle, C.H.; Lang, N.P. Interposition of a connective tissue graft or a collagen matrix to enhance wound stability—An experimental study in dogs. J. Clin. Periodontol. 2016, 43, 366–373. [Google Scholar] [CrossRef]
- Zucchelli, G.; Mazzotti, C.; Tirone, F.; Mele, M.; Bellone, P.; Mounssif, I. The connective tissue graft wall technique and enamel matrix derivative to improve root coverage and clinical attachment levels in Miller Class IV gingival recession. Int. J. Periodontics Restor. Dent. 2014, 34, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.; Thomas, R.; Mehta, D.S. An Update on the Protocols and Biologic Actions of Platelet Rich Fibrin in Dentistry. Eur. J. Prosthodont. Restor. Dent. 2017, 25, 64–72. [Google Scholar]
- Miron, R.J.; Fujioka-Kobayashi, M.; Bishara, M.; Zhang, Y.; Hernandez, M.; Choukroun, J. Platelet-Rich Fibrin and Soft Tissue Wound Healing: A Systematic Review. Tissue Eng. Rev. 2017, 23, 83–99. [Google Scholar] [CrossRef]
- Gassling, V.; Douglas, T.; Warnke, P.H.; Açil, Y.; Wiltfang, J.; Becker, S.T. Platelet-rich fibrin membranes as scaffolds for periosteal tissue engineering. Clin. Oral Implant. Res. 2010, 21, 543–549. [Google Scholar] [CrossRef]
- Gassling, V.; Hedderich, J.; Açil, Y.; Purcz, N.; Wiltfang, J.; Douglas, T. Comparison of platelet rich fibrin and collagen as osteo-blast-seeded scaffolds for bone tissue engineering applications. Clin. Oral Implant. Res. 2013, 24, 320–328. [Google Scholar] [CrossRef]
- Castro, A.B.; Meschi, N.; Temmerman, A.; Pinto, N.; Lambrechts, P.; Teughels, W.; Quirynen, M. Regenerative potential of leucocyte- and platelet-rich fibrin. Part A: Intra-bony defects, furcation defects and periodontal plastic surgery. A systematic review and meta-analysis. J. Clin. Periodontol. 2016, 44, 67–82. [Google Scholar] [CrossRef] [PubMed]
- Temmerman, A.; Vandessel, J.; Castro, A.; Jacobs, R.; Teughels, W.; Pinto, N.; Quirynen, M. The use of leucocyte and platelet-rich fibrin in socket management and ridge preservation: A split-mouth, randomized, controlled clinical trial. J. Clin. Periodontol. 2016, 43, 990–999. [Google Scholar] [CrossRef]
- Dragonas, P.; Katsaros, T.; Avila-Ortiz, G.; Chambrone, L.; Schiavo, J.; Palaiologou, A. Effects of leukocyte–platelet-rich fibrin (L-PRF) in different intraoral bone grafting procedures: A systematic review. Int. J. Oral Maxillofac. Surg. 2019, 48, 250–262. [Google Scholar] [CrossRef]
- Cortellini, P.; Tonetti, M.S. Evaluation of the effect of tooth vitality on regenerative outcomes in infrabony defects. J. Clin. Perio-dontol. 2001, 28, 672–679. [Google Scholar] [CrossRef]
- Cortellini, P.; Stalpers, G.; Mollo, A.; Tonetti, M.S. Periodontal regeneration versus extraction and prosthetic replacement of teeth severely compromised by attachment loss to the apex: 5-year results of an ongoing randomized clinical trial. J. Clin. Periodontol. 2011, 38, 915–924. [Google Scholar] [CrossRef]
- Sobczak-Zagalska, H.; Emerich, K. Best Splinting Methods in Case of Dental Injury–A Literature Review. J. Clin. Pediatr. Dent. 2020, 44, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Trombelli, L.; Farina, R.; Minenna, L.; Toselli, L.; Simonelli, A. Regenerative Periodontal Treatment with the Single Flap Ap-proach in Smokers and Nonsmokers. Int. J. Periodontics Restor. Dent. 2018, 38, e59–e67. [Google Scholar] [CrossRef] [PubMed]
- Persson, R.E.; Rollender, L.G.; Laurell, L.; Persson, G.R. Horizontal Alveolar Bone Loss and Vertical Bone Defects in an Adult Patient Population. J. Periodontol. 1998, 69, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Liu, Y.; Xu, T.; Zhao, H.; Hou, J.; Wu, Y.; Zhang, D. The Additional Effect of Autologous Platelet Concentrates to Coronally Advanced Flap in the Treatment of Gingival Recessions: A Systematic Review and Meta-Analysis. Biomed. Res. Int. 2019, 2019, 2587245. [Google Scholar] [CrossRef]
- Lekovic, V.; Milinkovic, I.; Aleksic, Z.; Jankovic, S.; Stankovic, P.; Kenney, E.B.; Camargo, P.M. Platelet-rich fibrin and bovine porous bone mineral vs. platelet-rich fibrin in the treatment of intrabony periodontal defects. J. Periodontal Res. 2012, 47, 409–417. [Google Scholar] [CrossRef]
- Muthu, K.; Saravanan, D.; Rethinam, S.; Thangapandian, A. The combined effect of bioactive glass and platelet-rich fibrin in treating human periodontal intrabony defects—A clinicoradiographic study. Contemp. Clin. Dent. 2019, 10, 110. [Google Scholar] [CrossRef]
- Del Corso, M.; Vervelle, A.; Simonpieri, A.; Jimbo, R.; Inchingolo, F.; Sammartino, G.; Dohan Ehrenfest, D.M. Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 1: Periodontal and dentoalveolar surgery. Curr. Pharm. Biotechnol. 2012, 13, 1207–1230. [Google Scholar] [CrossRef]
- Bosshardt, D.D. Biological mediators and periodontal regeneration: A review of enamel matrix proteins at the cellular and molecular levels. J. Clin. Periodontol. 2008, 35, 87–105. [Google Scholar] [CrossRef]
- Tu, Y.-K.; Woolston, A.; Faggion, C.M. Do bone grafts or barrier membranes provide additional treatment effects for infrabony lesions treated with enamel matrix derivatives? A network meta-analysis of randomized-controlled trials. J. Clin. Periodontol. 2010, 37, 59–79. [Google Scholar] [CrossRef]
- Matarasso, M.; Iorio-Siciliano, V.; Blasi, A.; Ramaglia, L.; Salvi, G.E.; Sculean, A. Enamel matrix derivative and bone grafts for peri-odontal regeneration of intrabony defects. A systematic review and meta-analysis. Clin. Oral Investig. 2015, 19, 1581–1593. [Google Scholar] [CrossRef] [PubMed]
- Dohan, D.M.; Choukroun, J.; Diss, A.; Dohan, S.L.; Dohan, A.J.J.; Mouhyi, J.; Gogly, B. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part III: Leucocyte activation: A new feature for platelet concentrates? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, e51–e55. [Google Scholar] [CrossRef]
- Pitzurra, L.; Jansen, I.D.C.; De Vries, T.J.; Hoogenkamp, M.A.; Loos, B.G. Effects of L-PRF and A-PRF+ on periodontal fibroblasts in in vitro wound healing experiments. J. Periodontal Res. 2019, 55, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Patel, G.K.; Gaekwad, S.S.; Gujjari, S.K.; Kumar, S.C.V. Platelet-Rich Fibrin in Regeneration of Intrabony Defects: A Randomized Con-trolled Trial. J. Periodontol. 2017, 88, 1192–1199. [Google Scholar] [CrossRef]
- Shah, M.; Deshpande, N.; Bharwani, A.; Nadig, P.; Doshi, V.; Dave, D. Effectiveness of autologous platelet-rich fibrin in the treatment of intra-bony defects: A systematic review and meta-analysis. J. Indian Soc. Periodontol. 2014, 18, 698–704. [Google Scholar]
- Bajaj, P.; Pradeep, A.R.; Agarwal, E.; Rao, N.S.; Naik, S.B.; Priyanka, N.; Kalra, N. Comparative evaluation of autologous platelet-rich fibrin and platelet-rich plasma in the treatment of mandibular degree II furcation defects: A randomized controlled clinical trial. J. Periodontal Res. 2013, 48, 573–581. [Google Scholar] [CrossRef]
- Aroca, S.; Keglevich, T.; Barbieri, B.; Gera, I.; Etienne, D. Clinical Evaluation of a Modified Coronally Advanced Flap Alone or in Combination with a Platelet-Rich Fibrin Membrane for the Treatment of Adjacent Multiple Gingival Recessions: A 6-Month Study. J. Periodontol. 2009, 80, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, K.; Chandra, C.; Agarwal, K.; Kumar, N. Lateral sliding bridge flap technique along with platelet rich fibrin and guided tissue regeneration for root coverage. J. Indian Soc. Periodontol. 2013, 17, 801–805. [Google Scholar] [CrossRef]
- Bharti, V.; Singh, J. Laterally positioned flap-revised technique along with platelet rich fibrin in the management of Miller class II gingival recession. Dent. Res. J. 2013, 10, 268–273. [Google Scholar] [CrossRef] [PubMed]

| Tooth | PPD | CAL | REC | TP | |||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 12 m | Baseline | 12 m | Baseline | 12 m | Baseline | 12 m | ||
| Case 1 | 24 | 7 | 4 | 12 | 7 | 5 | 3 | −5 | −5 |
| Case 2 | 21 | 9 | 4 | 11 | 5 | 2 | 1 | 0 | 1 |
| Case 3 | 11 | 8 | 3 | 10 | 4 | 2 | 1 | 2 | 2 |
| Case 4 | 12 | 9 | 3 | 10 | 5 | 1 | 2 | 1 | 1 |
| Mean ± SD | 8.25 ± 0.95 | 3.5 ± 0.57 | 10.75 ± 0.95 | 5.25 ± 1.25 | 2.5 ± 1.7 | 1.75 ± 0.95 | −0.5 ± 2.69 | −0.25 ± 2.7 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pardo-Zamora, G.; Moreno-Rodríguez, J.A.; Ortiz-Ruíz, A.J. Non-Incised Papilla Surgical Approach and Leukocyte Platelet-Rich Fibrin in Periodontal Reconstruction of Deep Intrabony Defects: A Case Series. Int. J. Environ. Res. Public Health 2021, 18, 2465. https://doi.org/10.3390/ijerph18052465
Pardo-Zamora G, Moreno-Rodríguez JA, Ortiz-Ruíz AJ. Non-Incised Papilla Surgical Approach and Leukocyte Platelet-Rich Fibrin in Periodontal Reconstruction of Deep Intrabony Defects: A Case Series. International Journal of Environmental Research and Public Health. 2021; 18(5):2465. https://doi.org/10.3390/ijerph18052465
Chicago/Turabian StylePardo-Zamora, Guillermo, José Antonio Moreno-Rodríguez, and Antonio J. Ortiz-Ruíz. 2021. "Non-Incised Papilla Surgical Approach and Leukocyte Platelet-Rich Fibrin in Periodontal Reconstruction of Deep Intrabony Defects: A Case Series" International Journal of Environmental Research and Public Health 18, no. 5: 2465. https://doi.org/10.3390/ijerph18052465
APA StylePardo-Zamora, G., Moreno-Rodríguez, J. A., & Ortiz-Ruíz, A. J. (2021). Non-Incised Papilla Surgical Approach and Leukocyte Platelet-Rich Fibrin in Periodontal Reconstruction of Deep Intrabony Defects: A Case Series. International Journal of Environmental Research and Public Health, 18(5), 2465. https://doi.org/10.3390/ijerph18052465






