Variety of Surgical Guides and Protocols for Bone Reduction Prior to Implant Placement: A Narrative Review
Abstract
1. Introduction
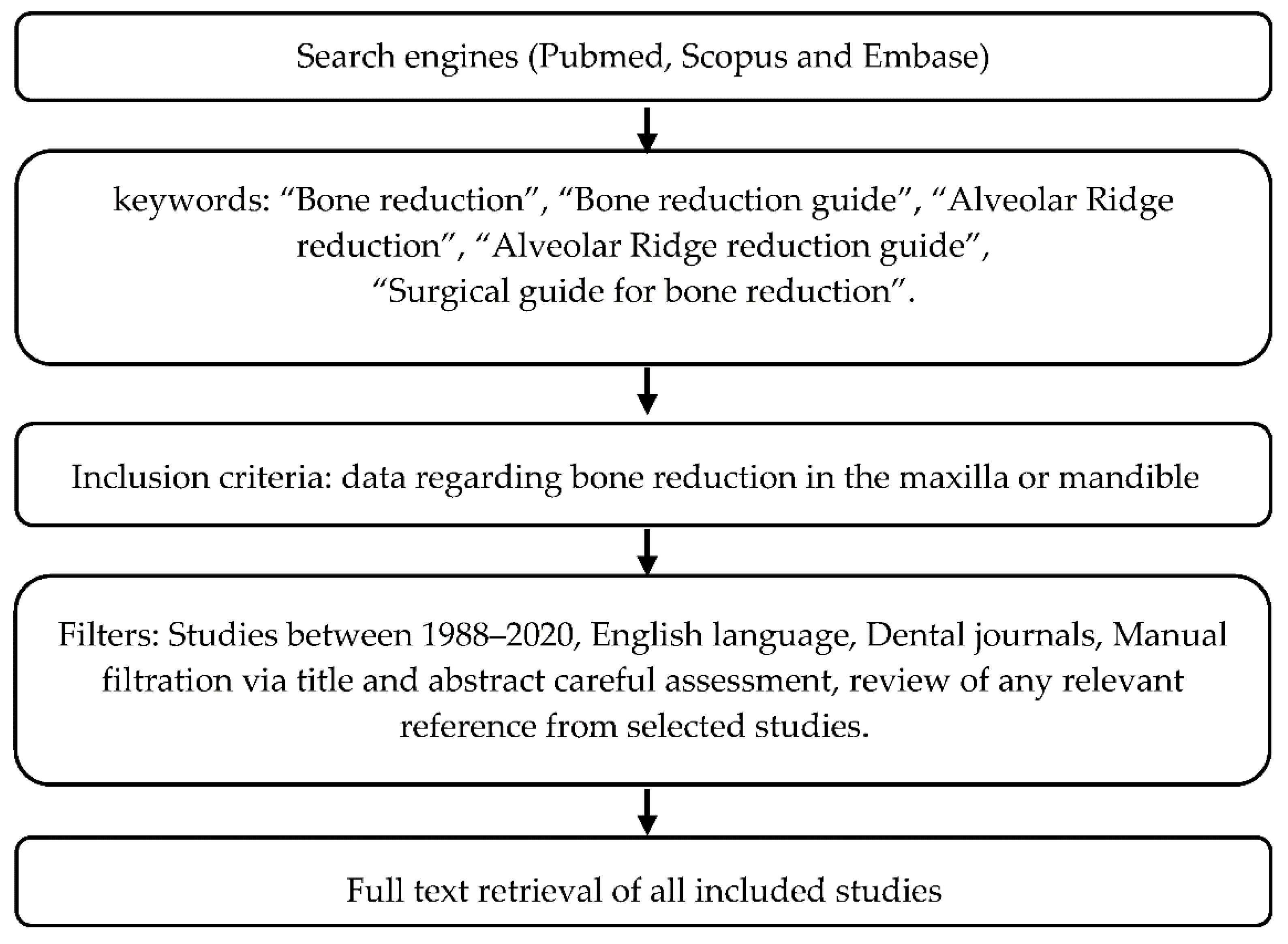
2. Materials and Methods
3. Results
3.1. Bone Reduction Guides: Techniques and Protocols
3.1.1. NOVUM System
3.1.2. “All-On-Four” Concept
3.1.3. Guided Bone Reduction and Drill Template
3.1.4. A Technique for Transferring a Patient’s Smile Line Using Gutta-Percha
3.1.5. Stackable Guides
3.1.6. Guides for Patients with a Terminal Dentition
3.1.7. The 3A-2B Rule
3.1.8. GuidedSmile Chrome-The “Scalloped Guide”
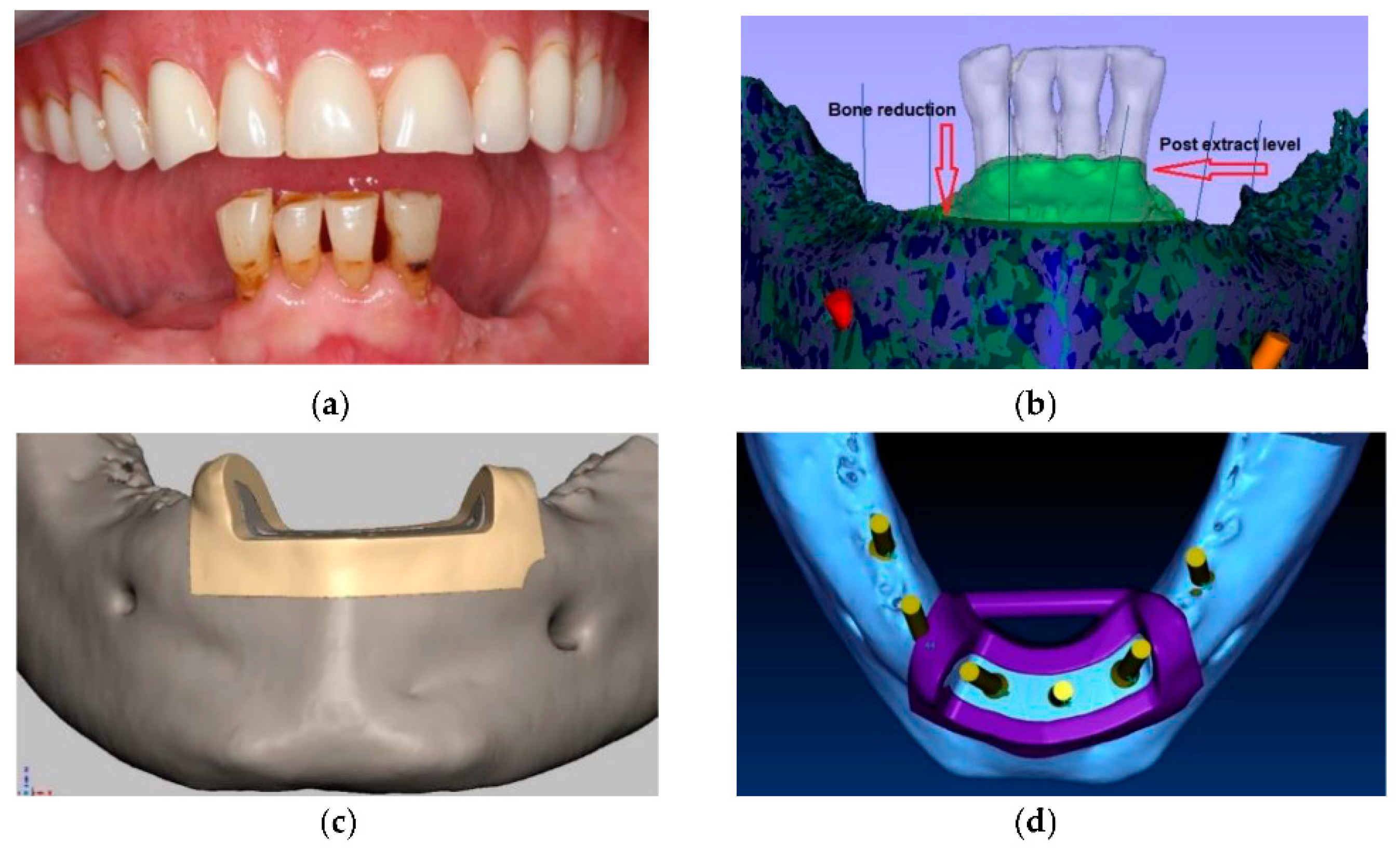
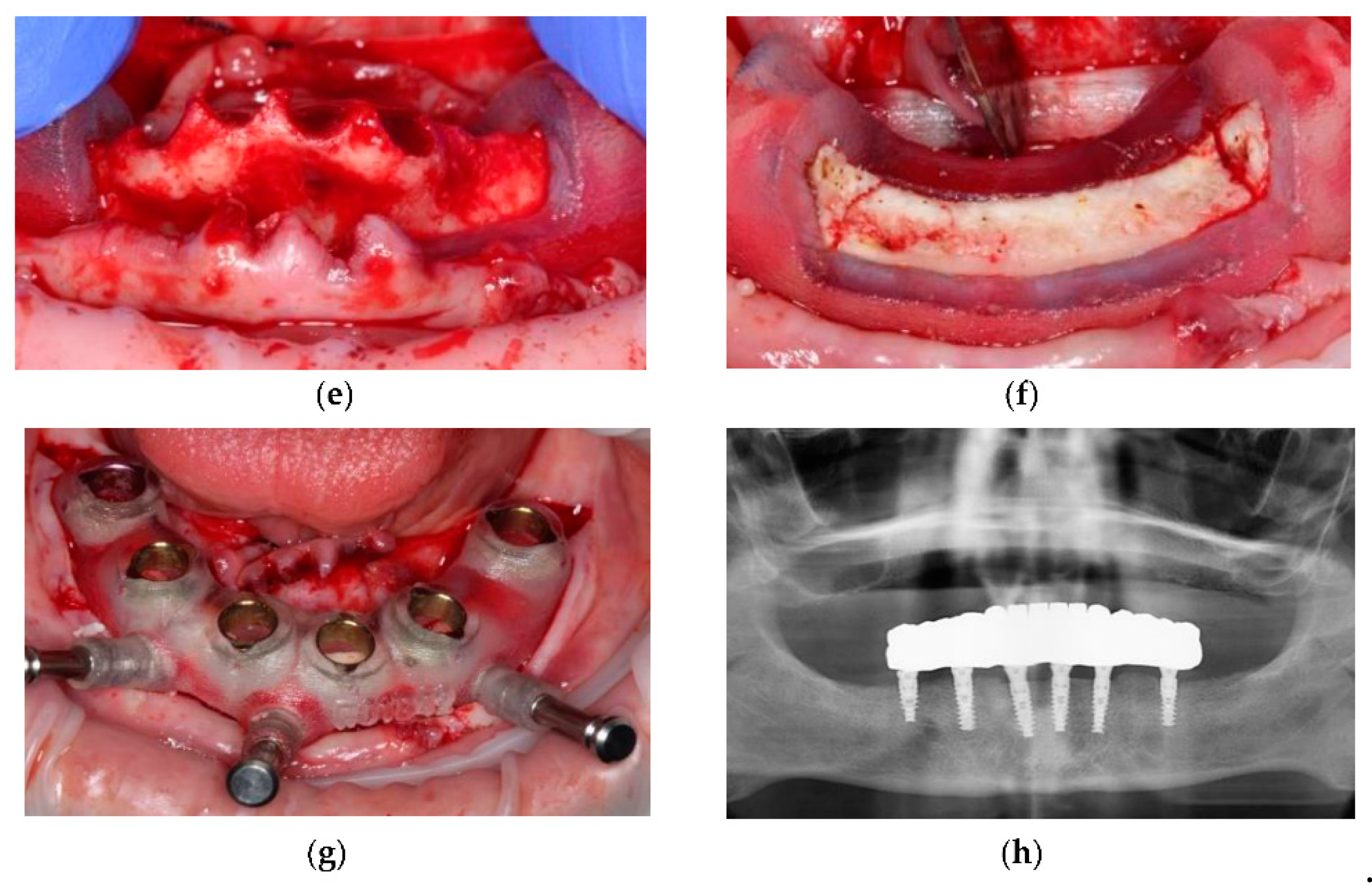
3.1.9. Magnetically Connected Guides
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pikos, M.A.; Magyar, C.W.; Llop, D.R. Guided full-arch immediate-function treatment modality for the edentulous and terminal dentition patient. Compend. Contin. Educ. Dent. Jamesburg NJ 1995 2015, 36, 116, 119–126, 128. [Google Scholar]
- Turkyilmaz, I.; Company, A.M.; McGlumphy, E.A. Should edentulous patients be constrained to removable complete dentures? The use of dental implants to improve the quality of life for edentulous patients. Gerodontology 2010, 27, 3–10. [Google Scholar] [CrossRef]
- Tremblay, G.; Ganz, S.D. Implant Dentistry for Complete Maxillary Rehabilitation: Two Innovative Protocols. Oral Health. 1 August 2018. Available online: https://www.oralhealthgroup.com/features/implant-dentistry-complete-maxillary-rehabilitation-two-innovative-protocols/ (accessed on 16 February 2021).
- Alzoubi, F.; Massoomi, N.; Nattestad, A. Bone Reduction to Facilitate Immediate Implant Placement and Loading Using CAD/CAM Surgical Guides for Patients With Terminal Dentition. J. Oral Implantol. 2016, 42, 406–410. [Google Scholar] [CrossRef]
- Marra, R.; Acocella, A.; Alessandra, R.; Ganz, S.D.; Blasi, A. Rehabilitation of Full-Mouth Edentulism: Immediate Loading of Implants Inserted with Computer-Guided Flapless Surgery Versus Conventional Dentures: A 5-Year Multicenter Retrospective Analysis and OHIP Questionnaire. Implant Dent. 2017, 26, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Cawood, J.I.; Howell, R.A. A classification of the edentulous jaws. Int. J. Oral Maxillofac. Surg. 1988, 17, 232–236. [Google Scholar] [CrossRef]
- Brånemark, P.I.; Engstrand, P.; Ohrnell, L.O.; Gröndahl, K.; Nilsson, P.; Hagberg, K.; Darle, C.; Lekholm, U. Brånemark Novum: A new treatment concept for rehabilitation of the edentulous mandible. Preliminary results from a prospective clinical follow-up study. Clin. Implant Dent. Relat. Res. 1999, 1, 2–16. [Google Scholar] [CrossRef]
- Parel, S.M.; Ruff, S.L.; Triplett, R.G.; Schow, S.R. Bone reduction surgical guide for the Novum implant procedure: Technical note. Int. J. Oral Maxillofac. Implant. 2002, 17, 715–719. [Google Scholar]
- Ganz, S.D. Techniques for the use of CT imaging for the fabrication of surgical guides. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2006, 14, 75–97. [Google Scholar] [CrossRef]
- Rinaldi, M.; Ganz, S.D.; Mottola, A. (Eds.) Computer-Guided Applications: For Dental Implants, Bone Grafting, and Reconstructive Surgery; Elsevier: Amsterdam, The Netherlands, 2015; p. 555. [Google Scholar]
- Ganz, S.A.T.I. Full-Arch Implant Surgical and Restorative Considerations Utilizing a Full Template Guidance Technique. Dentistry Today. 7 March 2020. Available online: https://www.dentistrytoday.com/implants/10597-full-arch-implant-surgical-and-restorative-considerations-utilizing-a-full-template-guidance-technique (accessed on 16 February 2021).
- Ganz, S. Three-Dimensional Imaging and Digital Workflow Protocols for Dental Implants and Bone Grafting. In Oral and Maxillofacial Surgery, 3th ed.; Fonseca, R., Ed.; Elsevier: St Louis, MO, USA, 2018; Volume 1, pp. 688–710. [Google Scholar]
- Aires, I.; Berger, J. Planning Implant Placement on 3D Stereolithographic Models Applied with Immediate Loading of Implant-Supported Hybrid Prostheses after Multiple Extractions: A Case Series. Int. J. Oral Maxillofac. Implant. 2016, 31, 172–178. [Google Scholar] [CrossRef]
- Ganz, S.D. CT-derived model-based surgery for immediate loading of maxillary anterior implants. Pract. Proced. Aesthetic Dent. 2007, 19, 311–318. [Google Scholar]
- Tonellini, G.; Saez Vigo, R.; Novelli, G. Double Guided Surgery in All-on-4(®) Concept: When Ostectomy Is Needed. Int. J. Dent. 2018, 2018, 2672549. [Google Scholar] [CrossRef] [PubMed]
- Bidra, A.S. Technique for systematic bone reduction for fixed implant-supported prosthesis in the edentulous maxilla. J. Prosthet. Dent. 2015, 113, 520–523. [Google Scholar] [CrossRef] [PubMed]
- Bidra, A.S. A technique for transferring a patient’s smile line to a cone beam computed tomography (CBCT) image. J. Prosthet. Dent. 2014, 112, 108–111. [Google Scholar] [CrossRef] [PubMed]
- Bidra, A.S.; Agar, J.R.; Parel, S.M. Management of patients with excessive gingival display for maxillary complete arch fixed implant-supported prostheses. J. Prosthet. Dent. 2012, 108, 324–331. [Google Scholar] [CrossRef]
- Keith, J.F.; Steven, M.M.; Carl, F.; Driscoll, M.A.; Freilich, A.D.; Guckes, K.L.K.; Thomas, J.M. The glossary of prosthodontic terms. J. Prosthet. Dent. 2005, 94, 10–92. [Google Scholar] [CrossRef]
- Salama, M.A.; Pozzi, A.; Clark, W.A.; Tadros, M.; Hansson, L.; Adar, P. The “Scalloped Guide”: A Proof-of-Concept Technique for a Digitally Streamlined, Pink-Free Full-Arch Implant Protocol. Int. J. Periodontics Restor. Dent. 2018, 38, 791–798. [Google Scholar] [CrossRef]
- Rojas-Vizcaya, F. Prosthetically guided bone sculpturing for a maxillary complete-arch implant-supported monolithic zirconia fixed prosthesis based on a digital smile design: A clinical report. J. Prosthet. Dent. 2017, 118, 575–580. [Google Scholar] [CrossRef]
- Barteaux, L.; Daelemans, P.; Malevez, C. A Surgical Stent for the Brånemark Novum® Bone Reduction Procedure. Clin. Implant Dent. Relat. Res. 2004, 6, 210–221. [Google Scholar] [CrossRef] [PubMed]
- Ganz, A.D.S.D. 3-D virtual planning concepts for implant-retained full-arch mandibular prostheses: The bone reduction guide. Dent. Trib. 2014, 3, 34–39. [Google Scholar]
- Misch, C.E.; Judy, K.W. Classification of partially edentulous arches for implant dentistry. Int. J. Oral Implantol. Implantol. 1987, 4, 7–13. [Google Scholar]
- Jensen, O.T.; Adams, M.W.; Cottam, J.R.; Parel, S.M.; Phillips, W.R., 3rd. The All-on-4 shelf: Maxilla. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2010, 68, 2520–2527. [Google Scholar] [CrossRef]
- Jensen, O.T. Complete arch site classification for all-on-4 immediate function. J. Prosthet. Dent. 2014, 112, 741–751.e742. [Google Scholar] [CrossRef]
- Jensen, O.T.; Adams, M.W.; Cottam, J.R.; Parel, S.M.; Phillips, W.R., 3rd. The all on 4 shelf: Mandible. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2011, 69, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Malo, P.; de Araujo Nobre, M.; Lopes, A. The use of computer-guided flapless implant surgery and four implants placed in immediate function to support a fixed denture: Preliminary results after a mean follow-up period of thirteen months. J. Prosthet. Dent. 2007, 97, S26–S34. [Google Scholar] [CrossRef]
- Lopes, A.; Maló, P.; de Araújo Nobre, M.; Sánchez-Fernández, E.; Gravito, I. The NobelGuide(®) All-on-4(®) Treatment Concept for Rehabilitation of Edentulous Jaws: A Retrospective Report on the 7-Years Clinical and 5-Years Radiographic Outcomes. Clin. Implant Dent. Relat. Res. 2017, 19, 233–244. [Google Scholar] [CrossRef]
- Amet, E.M.; Ganz, S.D. Implant treatment planning using a patient acceptance prosthesis, radiographic record base, and surgical template. Part 1: Presurgical phase. Implant Dent. 1997, 6, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Ganz, S.D. Advanced Case Planning with SimPlant. In The Art of Computer-Guided Implantology; Quintessence Publishing: Chicago, IL, USA, 2009. [Google Scholar]
- Ganz, S.A.T.I. Full-Arch Implant Surgical and Restorative Considerations: Innovative Digital Workflow Using a Verification Jig with Teeth. Dentistry Today. 27 January 2020. Available online: https://www.dentistrytoday.com/articles/10640 (accessed on 16 February 2021).
- CHROME. Digital, Full-Arch Guided Reconstruction. Available online: https://chromeguidedsmile.com/ (accessed on 11 June 2020).
- Rojas-Vizcaya, F. Biological aspects as a rule for single implant placement. The 3A-2B rule: A clinical report. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2013, 22, 575–580. [Google Scholar] [CrossRef]
- Groscurth, R.C.; Groscurth, S.U. Edentulous Surgical Guide. U.S. Patent 9,504,533, 29 November 2016. [Google Scholar]
- Costa, A.J.M.; Teixeira Neto, A.D.; Burgoa, S.; Gutierrez, V.; Cortes, A.R.G. Fully Digital Workflow with Magnetically Connected Guides for Full-Arch Implant Rehabilitation Following Guided Alveolar Ridge Reduction. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2020, 29, 272–276. [Google Scholar] [CrossRef]
- Gualini, F.; Gualini, G.; Cominelli, R.; Lekholm, U. Outcome of Brånemark Novum implant treatment in edentulous mandibles: A retrospective 5-year follow-up study. Clin. Implant Dent. Relat. Res 2009, 11, 330–337. [Google Scholar] [CrossRef]
- Geramipanah, F.; Sadighpour, L.; Hendi, A. Management of Limited Interocclusal Distance with the Aid of a Modified Surgical Guide: A Clinical Report. J. Dent. Tehran Iran 2017, 14, 105–108. [Google Scholar]
- Ahuja, S.; Cagna, D.R. Classification and management of restorative space in edentulous implant overdenture patients. J. Prosthet. Dent. 2011, 105, 332–337. [Google Scholar] [CrossRef]
- Faeghi Nejad, M.; Proussaefs, P.; Lozada, J. Combining guided alveolar ridge reduction and guided implant placement for all-on-4 surgery: A clinical report. J. Prosthet. Dent. 2016, 115, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Beretta, M.; Poli, P.P.; Tansella, S.; Maiorana, C. Virtually guided alveolar ridge reduction combined with computer-aided implant placement for a bimaxillary implant-supported rehabilitation: A clinical report. J. Prosthet. Dent. 2018, 120, 168–172. [Google Scholar] [CrossRef]
- Ataoglu, H.; Kucukkolbasi, H.; Ataoglu, T. Posterior segmental osteotomy of maxillary edentulous ridge: An alternative to vertical reduction. Int. J. Oral Maxillofac. Surg. 2002, 31, 558–559. [Google Scholar] [CrossRef] [PubMed]
- Marrelli, M.; Codispoti, B.; Shelton, R.M.; Scheven, B.A.; Cooper, P.R.; Tatullo, M.; Paduano, F. Dental Pulp Stem Cell Mechanoresponsiveness: Effects of Mechanical Stimuli on Dental Pulp Stem Cell Behavior. Front. Physiol. 2018, 9, 1685. [Google Scholar] [CrossRef] [PubMed]
- Spagnuolo, G.; Codispoti, B.; Marrelli, M.; Rengo, C.; Rengo, S.; Tatullo, M. Commitment of Oral-Derived Stem Cells in Dental and Maxillofacial Applications. Dent. J. 2018, 6, 72. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Marrelli, M.; Inchingolo, A.M.; Picciariello, V.; Inchingolo, A.D.; Dipalma, G.; Vermesan, D.; Cagiano, R. Clinical trial with bromelain in third molar exodontia. Eur. Rev. Med. Pharmacol. Sci. 2010, 14, 771–774. [Google Scholar] [PubMed]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Gentile, M.; Inchingolo, A.M.; Dipalma, G. Non-syndromic multiple supernumerary teeth in a family unit with a normal karyotype: Case report. Int. J. Med. Sci. 2010, 7, 378–384. [Google Scholar] [CrossRef] [PubMed]
| Method | Study Design | Perform Bone Remodeling in Full-Arch Restorations (Mandible or Maxilla) | How to Estimate the Amount before Surgery? | What Is the Rationale for Each Technique | Clinical Outcome |
|---|---|---|---|---|---|
| NOVUM System [7,22] | 50 participants (mandible), 150 implants, 6 mo-3 y follow-up [7]. 20 patients (mandible, 10 with stents, 10 without) [22] | Yes | Panoramic, lateral and intraoral periapical radiographs [7], Lateral cephalometric [22] | Introduction of one-stage implant insertion and prosthetic rehabilitation [7]. Surgical stent fabrication to support the NOVUM system [22]. | 98% survival rate, 98% prosthetic survival rate. Increased patient satisfaction; −1.25 mm mean marginal bone loss across 3 y follow-up [7]; Simple and cost-effective; Potential inaccurate plane of occlusion leading to tilted occlusal table. Increased prosthetic predictability (r = 0.9215) for patients treated using a stent [22]. |
| “All-on-Four” Concept [25,26,27,28,29] | Ref [25,26,27]—reviews 23 patients (both arches), 92 implants, 6 mo-21 mo follow-up [28] 111 patients (both arches), retrospective study of 532 implants (between 2005–2010) [29] | Yes | Clinical, Surgical software and radiographs (panoramic, CBCT). | Helps to avoid nerve injury, select implant sites, and establish the biomechanical advantage of increased anterior-posterior axis [27]. Nonaxial implant insertion and reduced number of implants [25]. | 97.8% survival rates, mean marginal bone loss 1.9 mm [28]. 94.5% survival rates, 97.8% prosthetic survival rates, mean marginal bone loss 1.3 mm, bruxing and smoking had negative effect on implant outcomes [29]. |
| Guided Bone Reduction and Drill Template [1,9,23] | Ref [1,9,23]—reviews | Yes | Ref [1]—Using CBCT data, clinical photographs, full-arch impressions and bite registrations [1] Ref [9]—CBCT and stereolithographic model fabrication [9] Ref [23]—CBCT and innovative softwares, followed by mucosal-supported template fabrication using 3D printing, stereolithographapy, or CAD-CAM process [23]. | Increased precision and accuracy of surgical and immediate provisionalization [1]. In cases of irregular bony architecture; inability to accurately determine relationship between desired tooth position and underlying bone [9]. Better understating of patient’s individual anatomy and proximity of vital structures, eliminating usage of ancillary appliances [23]. | Less time consuming procedure, increased patient satisfaction [1]. Predictable immediate prosthetic outcome; Increased accuracy using immediate insertion of parallel implants [9]. Reduced surgical and prosthetic complications, reduced laboratory work, better understanding of relationship between prosthesis and underlying structures [23]. |
| A technique for transferring a patient’s smile line using gutta-percha [16,17,30,31] | Ref [16,17]—Technical study | Yes | Clinical evaluation and CBCT. | Accurate bony reduction, especially in cases of limited prosthetic space, excessive mandibular gingival display, and esthetic zones. | Highly accurate and esthetic |
| Stackable Guides [10,11,32,33] | Case report [11] | Yes | CBCT and computer software | Accurate reduction using specialized software utilising CAD/CAM and 3D-Dicom data | |
| Guides for Patients with a Terminal Dentition [4] | Retrospective study. 5 patients (both arches), 26 implants | Yes | CBCT and computer software | Utilizing the terminal dentition to increase guide stability | Overall deviation means—1.98 mm |
| The 3A-2B rule [3,21,34] | Clinical report with 3y follow-up [21]. Clinical report with 1y follow-up [34] | Yes | Clinical photography, computer software (DSD, Radiographic Biological Ruler © [34]), CBCT, CAD/CAM [21] | Increased esthetics | Re-established maxillary incisal curve and lower lip relationship [21], Optimal restoration design [34] |
| GuidedSmile Chrome- The “Scalloped Guide” [20,35] | Technical study [20] | Yes | Clinical photography, computer software (DSD), CBCT, CAD/CAM | Minimize bony reduction and obtain accurate reductions; aids in hide the “transition zone”, optimize cleans ability | |
| Magnetically Connected Guides [36] | Technical study | Yes | Intra-oral scanner, clinical photographs, CBCT, CAM/CAM | Improved stability utilizing the magnets-embedded PMMA prosthesis | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mijiritsky, E.; Ben Zaken, H.; Shacham, M.; Cinar, I.C.; Tore, C.; Nagy, K.; Ganz, S.D. Variety of Surgical Guides and Protocols for Bone Reduction Prior to Implant Placement: A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 2341. https://doi.org/10.3390/ijerph18052341
Mijiritsky E, Ben Zaken H, Shacham M, Cinar IC, Tore C, Nagy K, Ganz SD. Variety of Surgical Guides and Protocols for Bone Reduction Prior to Implant Placement: A Narrative Review. International Journal of Environmental Research and Public Health. 2021; 18(5):2341. https://doi.org/10.3390/ijerph18052341
Chicago/Turabian StyleMijiritsky, Eitan, Hadar Ben Zaken, Maayan Shacham, Ihsan Caglar Cinar, Cem Tore, Katalin Nagy, and Scott D. Ganz. 2021. "Variety of Surgical Guides and Protocols for Bone Reduction Prior to Implant Placement: A Narrative Review" International Journal of Environmental Research and Public Health 18, no. 5: 2341. https://doi.org/10.3390/ijerph18052341
APA StyleMijiritsky, E., Ben Zaken, H., Shacham, M., Cinar, I. C., Tore, C., Nagy, K., & Ganz, S. D. (2021). Variety of Surgical Guides and Protocols for Bone Reduction Prior to Implant Placement: A Narrative Review. International Journal of Environmental Research and Public Health, 18(5), 2341. https://doi.org/10.3390/ijerph18052341







