Housing Quality in a Rural and an Urban Settlement in South Africa
Abstract
1. Introduction
2. Materials and Methods
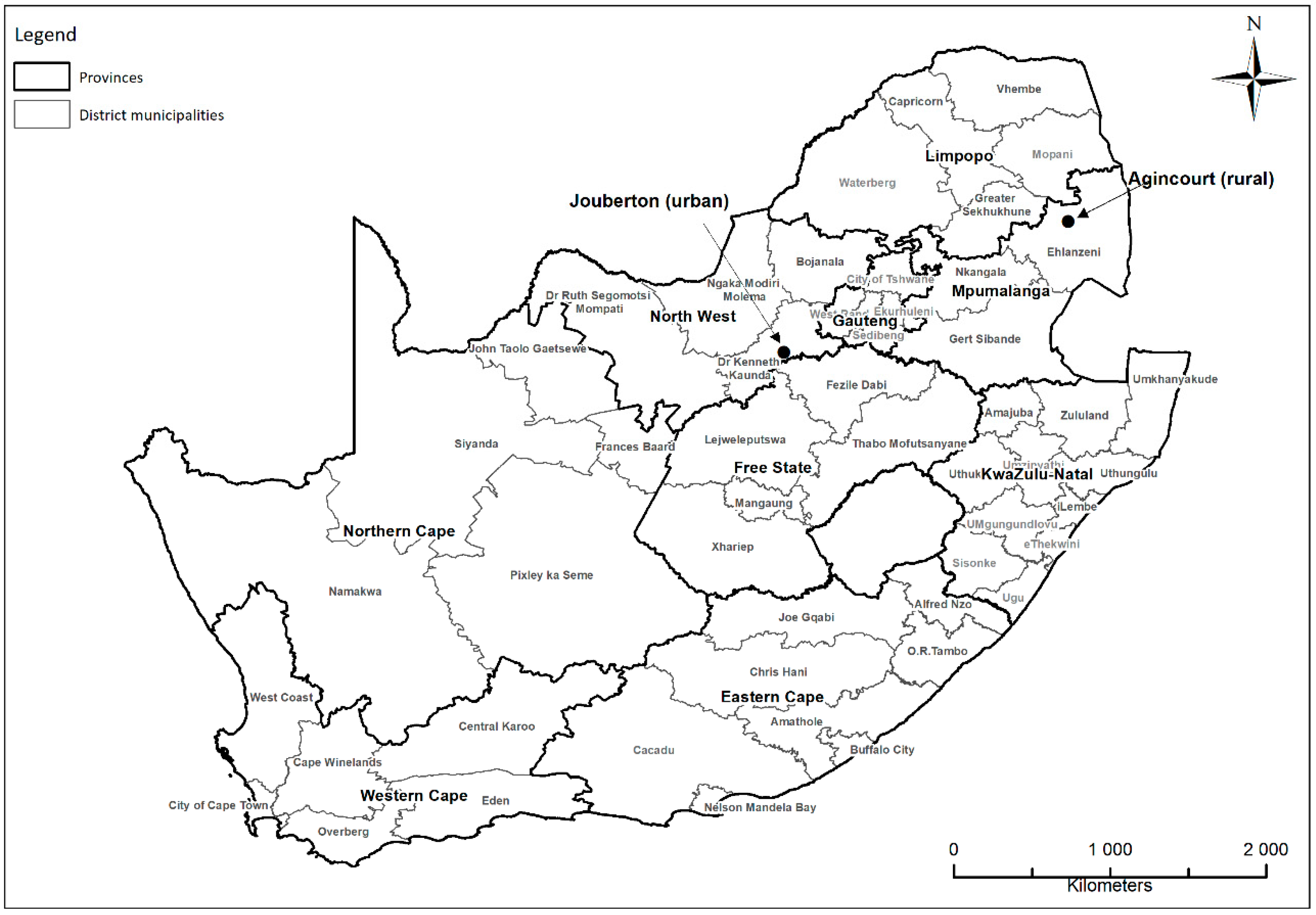
2.1. Study Setting and Design
2.2. Study Population and Sample
2.3. Data Collection and Methods
2.4. Data Analysis
3. Results
3.1. Water Supply
3.2. Fuel Use and Perceptions of Air Quality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Health Organization Housing and Health Guidelines. Geneva, Switzerland: World Health Organization 2018. Available online: https://www.who.int/publications/i/item/who-housing-and-health-guidelines (accessed on 16 November 2020).
- Prüss-Ustün, A.; Wolf, J.; Corvalán, C.; Neville, T.; Bos, R.; Neira, M. Diseases due to unhealthy environments: An updated estimate of the global burden of disease attributable to environmental determinants of health. J. Public Health 2017, 39, 464–475. [Google Scholar] [CrossRef]
- Bartram, J.; Cairncross, S. Hygiene, sanitation, and water: Forgotten foundations of health. PLoS Med. 2010, 7, e1000367. [Google Scholar] [CrossRef]
- Saunders-Hastings, P.; Crispo, J.A.; Sikora, L.; Krewski, D. Effectiveness of personal protective measures in reducing pandemic influenza transmission: A systematic review and meta-analysis. Epidemics 2017, 20, 1–20. [Google Scholar] [CrossRef]
- Mbakaya, B.C.; Lee, P.H.; Lee, R.L. Hand hygiene intervention strategies to reduce diarrhoea and respiratory infections among schoolchildren in developing countries: A systematic review. Int. J. Environ. Res. Public Health 2017, 14, 371. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.B.; Bruce, N.G.; Grigg, J.; Hibberd, P.L.; Kurmi, O.P.; Lam, K.-B.H.; Mortimer, K.; Asante, K.P.; Balakrishnan, K.; Balmes, J. Respiratory risks from household air pollution in low- and middle-income countries. Lancet Respir. Med. 2014, 2, 823–860. [Google Scholar] [CrossRef]
- World Health Organization. WHO guidelines for Indoor Air Quality: Household Fuel Combustion, Geneva, Switzerland, World Health Organization 2014. Available online: https://www.who.int/airpollution/guidelines/household-fuel-combustion/en/ (accessed on 16 November 2020).
- Quinn, A.K.; Bruce, N.; Puzzolo, E.; Dickinson, K.; Sturke, R.; Jack, D.W.; Mehta, S.; Shankar, A.; Sherr, K.; Rosenthal, J.P. An analysis of efforts to scale up clean household energy for cooking around the world. Energy Sustain. Dev. 2018, 46, 1–10. [Google Scholar] [CrossRef]
- Pope, C.A.; Ezzati, M.; Cannon, J.B.; Allen, R.T.; Jerrett, M.; Burnett, R.T. Mortality risk and PM 2.5 air pollution in the USA: An analysis of a national prospective cohort. Air Qual. Atmos. Health 2018, 11, 245–252. [Google Scholar] [CrossRef]
- Wang, B.; Liu, Y.; Li, Z.; Li, Z. Association of indoor air pollution from coal combustion with influenza-like illness in housewives. Environ. Pollut. 2016, 216, 646–652. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Zhang, W.; Li, S.; Zhang, Y.; Williams, G.; Huxley, R.; Ren, H.; Cao, W.; Guo, Y. The impact of ambient fine particles on influenza transmission and the modification effects of temperature in China: A multi-city study. Environ. Int. 2017, 98, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Rabie, T.; Curtis, V. Handwashing and risk of respiratory infections: A quantitative systematic review. Trop. Med. Int. Health 2006, 11, 258–267. [Google Scholar] [CrossRef]
- Liu, M.; Ou, J.; Zhang, L.; Shen, X.; Hong, R.; Ma, H.; Zhu, B.-P.; Fontaine, R.E. Protective effect of hand-washing and good hygienic habits against seasonal influenza: A case-control study. Medicine 2016, 95, e3046. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines for Drinking-Water Quality. Fourth ed. Geneva, Switzerland: World Health Organization 2011. Available online: https://www.who.int/water_sanitation_health/publications/gdwq4-with-add1-chapters/en/ (accessed on 16 November 2020).
- Kahn, K.; Collinson, M.A.; Gómez-Olivé, F.X.; Mokoena, O.; Twine, R.; Mee, P.; Afolabi, S.A.; Clark, B.D.; Kabudula, C.W.; Khosa, A. Profile: Agincourt health and socio-demographic surveillance system. Int. J. Epidemiol. 2012, 41, 988–1001. [Google Scholar] [CrossRef]
- Lebina, L.; Fuller, N.; Osoba, T.; Scott, L.; Motlhaoleng, K.; Rakgokong, M.; Abraham, P.; Variava, E.; Martinson, N.A. The use of Xpert MTB/Rif for active case finding among TB contacts in North West Province, South Africa. Tuberc. Res. Treat. 2016. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Gundry, S.W.; Wright, J.A.; Conroy, R.; du Preez, M.; Genthe, B.; Moyo, S.; Mutisi, C.; Ndamba, J.; Potgieter, N. Contamination of drinking water between source and point-of-use in rural household of South Africa and Zimbabwe: Implications for monitoring the Millenium Development Goal for water. Water Pract. Technol. 2006, 1, wpt2006032. [Google Scholar] [CrossRef]
- Wolf, J.; Prüss-Ustün, A.; Cumming, O.; Bartram, J.; Bonjour, S.; Cairncross, S.; Clasen, T.; Colford, J.M., Jr.; Curtis, V.; De France, J. Systematic review: Assessing the impact of drinking water and sanitation on diarrhoeal disease in low-and middle-income settings: Systematic review and meta-regression. Trop. Med. Int. Health 2014, 19, 928–942. [Google Scholar] [CrossRef]
- Shields, K.F.; Bain, R.E.; Cronk, R.; Wright, J.A.; Bartram, J. Association of supply type with fecal contamination of source water and household stored drinking water in developing countries: A bivariate meta-analysis. Environ. Health Perspect. 2015, 123, 1222–1231. [Google Scholar] [CrossRef] [PubMed]
- Kapwata, T.; Mathee, A.; Le Roux, W.J.; Wright, C.Y. Diarrhoeal disease in relation to possible household risk factors in South African villages. Int. J. Environ. Res. Public Health 2018, 15, 1665. [Google Scholar] [CrossRef]
- Luby, S.P.; Agboatwalla, M.; Painter, J.; Altaf, A.; Billhimer, W.L.; Hoekstra, R.M. Effect of intensive handwashing promotion on childhood diarrhea in high-risk communities in Pakistan: A randomized controlled trial. JAMA 2004, 291, 2547–2554. [Google Scholar] [CrossRef]
- Ikeda, T.; Kapwata, T.; Behera, S.K.; Minakawa, N.; Hashizume, M.; Sweijd, N.; Mathee, A.; Wright, C.Y. Climatic Factors in relation to diarrhoea hospital admissions in rural Limpopo, South Africa. Atmosphere 2019, 10, 522. [Google Scholar] [CrossRef]
- Bruce, N.; Pope, D.; Rehfuess, E.; Balakrishnan, K.; Adair-Rohani, H.; Dora, C. WHO indoor air quality guidelines on household fuel combustion: Strategy implications of new evidence on interventions and exposure–risk functions. Atmos. Environ. 2015, 106, 451–457. [Google Scholar] [CrossRef]
- Rylance, J.; Fullerton, D.G.; Scriven, J.; Aljurayyan, A.N.; Mzinza, D.; Barrett, S.; Wright, A.K.; Wootton, D.G.; Glennie, S.J.; Baple, K. Household air pollution causes dose-dependent inflammation and altered phagocytosis in human macrophages. Am. J. Respir. Cell Mol. Biol. 2015, 52, 584–593. [Google Scholar] [CrossRef]
- Bruce, N.G.; Dherani, M.K.; Das, J.K.; Balakrishnan, K.; Adair-Rohani, H.; Bhutta, Z.A.; Pope, D. Control of household air pollution for child survival: Estimates for intervention impacts. BMC Public Health 2013, 13, S8. [Google Scholar] [CrossRef]
- Peer, N.; Bradshaw, D.; Laubscher, R.; Steyn, N.; Steyn, K. Urban–rural and gender differences in tobacco and alcohol use, diet and physical activity among young black South Africans between 1998 and 2003. Glob. Health Action 2013, 6, 19216. [Google Scholar] [CrossRef]
- Mendell, M.J.; Mirer, A.G.; Cheung, K.; Tong, M.; Douwes, J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: A review of the epidemiologic evidence. Environ. Health Perspect. 2011, 119, 748–756. [Google Scholar] [CrossRef]
- United Nations-Habitat. The Right to Adequate Housing. Fact Sheet. Geneva, Switzerland: Office of the United Nations High Commissioner for Human Rights 2014. Available online: https://unhabitat.org/the-right-to-adequate-housing-fact-sheet-no-21rev-1 (accessed on 16 November 2020).
- Snider, G.; Carter, E.; Clark, S.; Yang, X.; Ezzati, M.; Schauer, J.J.; Wiedinmyer, C.; Baumgartner, J. Impacts of stove use patterns and outdoor air quality on household air pollution and cardiovascular mortality in southwestern China. Environ. Int. 2018, 117, 116–124. [Google Scholar] [CrossRef]


| Agincourt | Jouberton | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Year (n) | 2016 (50) n (%) | 2017 (53) n (%) | 2018 (56) n (%) | 2016-2018 (159) N (%) | 2016 (50) n (%) | 2017 (55) n (%) | 2018 (62) n (%) | 2016–2018 (167) N (%) | * p-Value Test for difference between Agincourt and Jouberton (2016 to 2018) |
| Type of dwelling | |||||||||
| Bricks-and-mortar dwelling built by professional builder | 32 (64%) | 31 (58%) | 29 (52%) | 92 (58%) | 39 (78%) | 48 (87%) | 56 (90%) | 143 (86%) | <0.001 |
| Bricks-and-mortar dwelling built by self | 11 (22%) | 20 (38%) | 26 (46%) | 57 (36%) | 6 (12%) | 5 (9%) | 4 (6%) | 15 (9%) | |
| Informal structure | 5 (10%) | 1 (2%) | 0 (0%) | 6 (4%) | 3 (6%) | 2 (4%) | 1 (2%) | 6 (4%) | |
| Other dwelling | 2 (4%) | 1 (2%) | 1 (2%) | 4 (3%) | 2 (4%) | 0 (0%) | 1 (2%) | 3 (2%) | |
| Age of the dwelling (years) | |||||||||
| 1–8 | 8 (16%) | 9 (17%) | 22 (40%) | 39 (25%) | 21 (42%) | 14 (25%) | 15 (24%) | 50 (30%) | 0.373 |
| 9–15 | 14 (28%) | 15 (28%) | 12 (21%) | 41 (26%) | 10 (20%) | 17 (31%) | 14 (23%) | 41 (25%) | |
| 16–23 | 17 (34%) | 13 (25%) | 12 (21%) | 42 (26%) | 13 (26%) | 10 (19%) | 9 (15%) | 32 (19%) | |
| >23 | 11 (22%) | 16 (30%) | 10 (18%) | 37 (23%) | 6 (12%) | 14 (25%) | 24 (39%) | 44 (26%) | |
| Median (IQR) | 18.5 (10–25) | 16 (11–25) | 10 (7–20) | 15 (9–23) | 10.5 (5–20) | 14 (8–24) | 15 (8–25) | 15 (8–24) | |
| Dwellings with kitchen detached from main dwelling | 33 (66%) | 34 (64%) | 43 (77%) | 110 (69%) | 10 (20%) | 7 (13%) | 9 (15%) | 26 (16%) | <0.001 |
| Dwellings with toilet located outside/separate from main dwelling | 39 (78%) | 36 (68%) | 49 (88%) | 124 (78%) | 25 (50%) | 23 (42%) | 27 (44%) | 75 (45%) | <0.001 |
| Dwellings with bathroom located outside/separate from main dwelling | 16 (32%) | 20 (38%) | 29 (52%) | 65 (41%) | 4 (8%) | 6 (11%) | 6 (10%) | 16 (10%) | <0.001 |
| Dwellings with corrugated metal sheet roof | 42 (84%) | 41 (77) | 38 (68) | 121 (76%) | 47 (94%) | 43 (78%) | 44 (72%) | 134 (81%) | 0.294 |
| Dwellings with no ceiling | 43 (86%) | 30 (57%) | 43 (77) | 116 (73%) | 39 (78%) | 40 (73%) | 51 (82%) | 130 (78%) | 0.305 |
| Cracks in walls | 29 (58%) | 18 (66%) | 19 (35%) | 66 (42%) | 30 (60%) | 43 (78%) | 23 (37%) | 96 (57%) | 0.005 |
| Leaking roofs | 24 (48%) | 19 (36%) | 28 (50%) | 71 (48%) | 26 (52%) | 28 (51%) | 33 (53%) | 87 (52%) | 0.179 |
| Leaking water pipes in or around dwelling | 5 (10%) | 3 (6%) | 4 (7%) | 12 (8%) | 5 (10%) | 16 (29%) | 13 (21%) | 34 (20%) | 0.002 |
| House has no ceilings | 7 (14%) | 23 (43%) | 13 (23%) | 43 (27%) | 11 (22%) | 15 (27%) | 11 (18%) | 37 (22%) | 0.305 |
| Fungus or mold on walls or ceiling | 7 (14%) | 8 (15%) | 6 (11%) | 21 (13%) | 3 (6%) | 6 (11%) | 1 (2%) | 10 (6%) | 0.232 |
| Agincourt | Jouberton | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Year (n) | 2016 (50) n (%) | 2017 (53) n (%) | 2018 (56) n (%) | 2016–2018 (159) N (%) | 2016 (50) n (%) | 2017 (55) n (%) | 2018 (62) n (%) | 2016–018 (167) N (%) | * p-Value Test for difference between Agincourt and Jouberton (2016 to 2018) |
| Primary water source: | |||||||||
| Indoor tap | 27 (54%) | 47 (89%) | 8 (14%) | 82 (52%) | 16 (32%) | 34 (62%) | 32 (52%) | 82 (49%) | <0.001 |
| Tap in yard | 10 (20%) | 3 (6%) | 18 (32%) | 31 (20%) | 34 (68%) | 21 (38%) | 30 (48%) | 85 (51%) | |
| Off-site tap | 7 (14%) | 2 (4%) | 2 (4%) | 11 (7%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Water tank | 0 (0%) | 1 (2%) | 9 (16%) | 10 (6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Water vendor or truck | 3 (6%) | 0 (0%) | 3 (5%) | 6 (4%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Borehole | 3 (6%) | 0 (0%) | 13 (23%) | 16 (10%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| River or stream or dam | 0 (0%) | 0 (0%) | 1 (2%) | 1 (1%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Number of different water sources: | |||||||||
| 1 | 4 (8%) | 1 (2%) | 17 (30%) | 22 (14%) | 37 (74%) | 39 (71%) | 36 (58%) | 112 (67%) | <0.001 |
| 2 | 7 (14%) | 3 (6%) | 20 (36%) | 30 (19%) | 13 (26%) | 14 (25%) | 25 (40%) | 52 (31%) | |
| 3 | 11 (22%) | 3 (6%) | 10 (18%) | 24 (15%) | 0 (0%) | 2 (4%) | 1 (2%) | 3 (2%) | |
| >4 | 28 (56%) | 46 (87%) | 9 (16%) | 83 (52%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Level of water risk [18]: | |||||||||
| Low risk (makes use of indoor tap only) | 2 (4%) | 1 (2%) | 1 (2%) | 4 (3%) | 4 (8%) | 23 (42%) | 8 (13%) | 35 (21%) | <0.001 |
| Moderate risk (outdoor tap, on or off-site) | 2 (4%) | 3 (6%) | 8 (14%) | 13 (8%) | 45 (90%) | 28 (51%) | 54 (87%) | 127 (76%) | |
| High risk (may use borehole, river, dam, stream, water vendor, water tank, or water truck) | 46 (92%) | 49 (92%) | 47 (84%) | 142 (89%) | 1 (2%) | 4 (7%) | 0 (0%) | 5 (3%) | |
| Drinking water is stored in a container | 47 (94%) | 53 (100%) | 54 (100%) | 154 (97%) | 38 (76%) | 38 (69%) | 39 (64%) | 115 (69%) | <0.001 |
| How long is water stored in a container? | |||||||||
| 1 day or less | 4 (9%) | 16 (30%) | 26 (50%) | 46 (30%) | 30 (79%) | 10 (26%) | 29 (78%) | 69 (61%) | <0.001 |
| 2–7 days | 9 (19%) | 11 (21%) | 8 (15%) | 28 (18%) | 7 (18%) | 28 (74%) | 8 (22%) | 43 (38%) | |
| 8 to 30 days | 20 (43%) | 12 (23%) | 13(25%) | 45 (29%) | 1 (3%) | 0 (0%) | 0 (0%) | 1 (1%) | |
| >30 days | 14 (30%) | 14 (26%) | 6 (11%) | 34 (22%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Flies and other insects sometimes get into the drinking water container | 11 (23%) | 13 (25%) | 16 (30%) | 40 (26%) | 6 (16%) | 5 (13%) | 3 (8%) | 14 (12%) | 0.006 |
| Frequency of water supply interruptions: | |||||||||
| Never/hardly ever/infrequently | 2 (4%) | 14 (26%) | 1 (2%) | 17 (11%) | 36 (72%) | 48 (87%) | 61 (98%) | 145 (87%) | <0.001 |
| Monthly | 10 (20%) | 7 (13%) | 5 (9%) | 22 (14%) | 13 (26%) | 7 (13%) | 1 (2%) | 21 (13%) | |
| Weekly | 27 (54%) | 30 (57%) | 8 (15%) | 65 (41%) | 1 (2%) | 0 (0%) | 0 (0%) | 1 (1%) | |
| Daily | 11 (22%) | 2 (4%) | 41 (75%) | 54 (34%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Access to running hot water | 0 (0%) | 3 (6%) | 0 (0%) | 3 (2%) | 3 (6%) | 9 (16%) | 9 (15%) | 21 (13%) | <0.001 |
| Type of toilet: | |||||||||
| Waterborne flush toilet | 0 (0%) | 5 (9%) | 0 (0%) | 5 (3%) | 50 (100%) | 55 (100%) | 59 (97%) | 164 (99%) | <0.001 |
| Pit latrine | 48 (96%) | 46 (87%) | 53 (96%) | 147 (93%) | 0 (0%) | 0 (0%) | 2 (3%) | 2 (1%) | |
| No toilet (make use of bush) | 2 (4%) | 2 (4%) | 2 (4%) | 6 (4%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Study Site | Agincourt | Jouberton | ^ p-Value Test for Difference between Agincourt and Jouberton Township | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Year (n) | 2016 (50) | 2017 (53) | 2018 (56) | 2016–2018 (159) | 2016 (50) | 2017 (55) | 2018 (62) | 2016–2018 (167) | |
| Main fuel used for cooking: | |||||||||
| Electricity | 15 (30%) | 33 (62%) | 41 (73%) | 89 (56%) | 45 (90%) | 52 (95%) | 58 (95%) | 155 (93%) | <0.001 |
| Gas | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (4%) | 1 (2%) | 1 (2%) | 4 (2%) | |
| Paraffin | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 3 (6%) | 1 (2%) | 2 (3%) | 6 (4%) | |
| Wood | 35 (70%) | 20 (38%) | 15 (27%) | 70 (44%) | 0 (0%) | 1 (2%) | 0 (0%) | 1 (1%) | |
| A secondary fuel is sometimes used for cooking | 36 (72%) | 38 (72%) | 49 (89%) | 123 (78%) | 32 (64%) | 25 (45%) | 30 (48%) | 87 (52%) | <0.001 |
| Main fuel used for space heating: | |||||||||
| Don’t heat the dwelling | 36 (72%) | 28 (53%) | 30 (54%) | 95 (60%) | 12 (24%) | 0 (0%) | 9 (16%) | 21 (13%) | <0.001 |
| Electricity | 6 (12%) | 14 (26%) | 24 (43%) | 44 (28%) | 29 (58%) | 47 (85%) | 45 (80%) | 121 (75%) | |
| Gas | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (2%) | 1 (2%) | 1 (2%) | 3 (2%) | |
| Paraffin | 0 (0%) | 1 (2%) | 0 (0%) | 1 (1%) | 4 (8%) | 1 (2%) | 1 (2%) | 6 (4%) | |
| Solid fuel (wood or coal) | 7 (14%) | 10 (19%) | 2 (4%) | 19 (12%) | 4 (8%) | 6 (11%) | 0 (0%) | 10 (6%) | |
| A secondary fuel is sometimes used for space heating | 3 (6%) | 2 (4%) | 10 (18%) | 15 (9%) | 8 (16%) | 10 (18%) | 5 (8%) | 23 (14%) | 0.215 |
| Fuel used to heat water for personal hygiene: | |||||||||
| Nothing (do not heat water) | 24 (48%) | 27 (51%) | 32 (58%) | 83 (53%) | 2 (4%) | 0 (0%) | 10 (17%) | 12 (7%) | <0.001 |
| Electricity/solar | 12 (24%) | 16 (30%) | 15 (27%) | 43 (27%) | 43 (86%) | 52 (95%) | 45 (76%) | 137 (84%) | |
| Gas | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (4%) | 1 (2%) | 1 (2%) | 4 (2%) | |
| Paraffin | 0 (0%) | 0 (0%) | 1 (2%) | 1 (1%) | 3 (6%) | 2 (4%) | 3 (5%) | 8 (5%) | |
| Solid fuel (wood or coal) | 14 (28%) | 10 (30%) | 6 (11%) | 30 (19%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Monthly household electricity expenditure (Rands): ~ | |||||||||
| < R50 (USD 3) | Data not collected # | 2 (4%) | 1 (2%) | 3 (3%) | Data not collected | 0 (0%) | 0 (0%) | 0 (0%) | <0.001 |
| R50–R99 (USD 3–6) | 6 (11%) | 3 (5%) | 9 (8%) | 0 (0%) | 0 (0%) | 0 (0%0 | |||
| R100–R499 | 29 (55%) | 28 (50%) | 57 ((52%) | 5 (9%) | 9 (15%) | 14 (12%) | |||
| >R500 (USD 30) | 16 (30%) | 24 (43%) | 40 (37%) | 50 (91%) | 53 (85%) | 103 (88%) | |||
| Average monthly household electricity expenditure (Rands): ~ | Data not collected # | x = 149 | x = 209 | x = 176 | Data not collected | x = 365 | x = 365 | x = 369; | <0.001 |
| n = 52; | n = 54; | n = 108; | n = 55; | n = 60; | n = 115; | ||||
| range = 20–500; | range = 50–950; | range = 0–950; | range = 100–1200; | range = 100–3000; | range = 100–3000; | ||||
| SD = 97.14; | SD = 154.73; | SD = 133.60; | SD = 387.01; | SD = 387.01; | SD = 308.89; | ||||
| median = 100; | median = 165; | median = 150; | median = 360; | median = 300; | median = 300; | ||||
| IQR = 50–300 | IQR = 100–400 | IQR = 50–500 | IQR = 150–600 | IQR = 100–700 | IQR = 100–900 | ||||
| Monthly paraffin household expenditure (Rands): ~ | |||||||||
| 0 Rands (USD 0) | Data not collected # | 48 (91%) | 40 (71%) | 88 (81%) | Data not collected | 43 (78%) | 30 (48%) | 73 (62%) | < 0.001 |
| R 10–R 100 (USD 0.6–6.0) | 5 (9%) | 15 (27%) | 20 (18%) | 8 (15%) | 24 (39%) | 32 (27%) | |||
| >R 100 (USD 6.0) | 0 (0%) | 1 (2%) | 1 (1%) | 4 (7%) | 8 (13%) | 12 (11%) | |||
| Average monthly household paraffin expenditure (Rands): ~ | Data not collected # | x = 35 | x = 33 | x = 6 | Data not collected | x = 122 | x = 37 | x = 22 | 0.074 |
| n = 5; | n = 16; | n = 109 | n = 12; | n = 25; | n = 110; | ||||
| range = 14–60; | range = 13–130; | range = 0–130 | range = 15–300 | range = 12–150; | range = 0–300; | ||||
| SD = 19.63; | SD = 29.92; | SD = 17.79 | SD = 97.18 | SD = 33.87; | SD = 51.81; | ||||
| median = 30; | median = 24; | median = 0 | median = 100; | median = 24; | median = 0; | ||||
| IQR = 0–39 | IQR = 17–39 | IQR = 0–50 | IQR = 50–150 | IQR = 13–60 | IQR = 0–150 | ||||
| Monthly household wood expenditure (Rands): ~ | |||||||||
| 0 Rands (USD 0) | Data not collected # | 34 (64%) | 28 (50%) | 62 (57%) | Data not collected | 49 (89%) | 45 (73%) | 94 (81%) | <0.001 |
| R 1–R 200 (USD 0.06–12) | 11 (21%) | 10 (18%) | 21 (19%) | 4 (7%) | 1 (2%) | 5 (4%) | |||
| >R 200 (USD 12) | 8 (15%) | 18 (32%) | 26 (24%) | 2(4%) | 16 (26) | 18 (15%) | |||
| Average monthly household wood expenditure (Rands): ~ | Data not collected # | x = 249 | x = 316 | x = 125 | Data not collected | x = 175 | x = 60 | x = 11 | 0.044 |
| n = 19; | n = 28; | n = 109; | n = 6; | n = 1; | n = 101; | ||||
| range = 80–500; | range = 80–500; | range = 0–1100; | range = 50–300; | range = 60–60; | range = 0–300; | ||||
| SD = 144.60; | SD = 225.20; | SD = 193.66; | SD = 88.03; | SD = 8.85; | SD = 46.23; | ||||
| median = 200; | median = 275; | median = 0; | median = 150; | median = 60; | median = 0; | ||||
| IQR = 100–450 | IQR = 70–500 | IQR = 0–500 | IQR = 150–150 | IQR = 0–0 | IQR = 0–150 | ||||
| The local neighborhood is not provided with waste collection services | 46 (92%) | 53 (100%) | 56 (100%) | 155 (97%) | 0 (0%) | 2 (4%) | 2 (3%) | 4 (2%) | <0.001 |
| Household waste is sometimes burned at home | 46 (92%) | 43 (81%) | 43 (77%) | 132 (83%) | 18 (36%) | 20 (36%) | 15 (24%) | 53 (32%) | <0.001 |
| Frequency of household waste burning (amongst those who burn waste): | |||||||||
| Daily | 4/46 (9%) | 11/43 (26%) | 2/43 (5%) | 17 (13%) | 1/18(6%) | 0/20 (0%) | 0/14 (0%) | 1 (2%) | <0.001 |
| Weekly or fortnightly | 34/46 (74%) | 22/43 (51%) | 40/43 (93%) | 96 (73%) | 3/18(17%) | 8/20 (40%) | 0/14 (0%) | 11 (21%) | |
| Monthly | 5/46 (11%) | 8/43 (18%) | 1/43 (2%) | 14 (11%) | 4/18(22%) | 12/20 (60%) | 4/14 (29%) | 20 (38%) | |
| Rarely | 3/46 (7%) | 2/43 (5%) | 0 (0%) | 5 (4%) | 10/18(56%) | 0/20 (0%) | 10/14 (71%) | 30 (38%) | |
| Respondent perceives neighborhood air is polluted | 31 (62%) | 43 (81%) | 28 (50%) | 102 (64%) | 32 (64%) | 4 (7%) | 19 (31%) | 55 (33%) | <0.001 |
| During windy weather the air gets very dusty | 36 (72%) | 43 (81%) | 44 (79%) | 123 (77%) | 45 (90%) | 54 (98%) | 53 (85%) | 152 (91%) | 0.001 |
| The household includes a smoker | 9 (18%) | 10 (19%) | 3 (5%) | 22 (14%) | 25 (50%) | 35 (64%) | 27 (44%) | 87 (52%) | <0.001 |
| The household keeps pets | 24 (48%) | 8 (15%) | 6 (11%) | 38 (24%) | 7 (14%) | 28 (51%) | 15 (24%) | 50 (30%) | 0.232 |
| The household keeps animals for food generation purposes # | Data not collected # | 15 (28%) | 12 (21%) | 27 (25%) | Data not collected | 5 (9%) | 1 (2%) | 6 (5%) | <0.001 |
| The road on which the house is located is unpaved | 46 (92%) | 51 (96%) | 55 (98%) | 106 (67%) | 34 (68%) | 31 (56%) | 48 (77%) | 79 (47%) | 0.003 |
| Area of yard/garden covered by vegetation | |||||||||
| <50% | 35 (70%) | 45 (85%) | 26 (48%) | 106 (68%) | 47 (94%) | 54 (98%) | 44 (72%) | 145 (87%) | <0.001 |
| >50% | 15 (30%) | 8 (15%) | 28 (52%) | 51 (32%) | 3 (6%) | 1 (2%) | 17 (28%) | 21 (13%) | |
| There are shade trees on the plot | 40 (80%) | 47 (89%) | 44 (79%) | 131 (82%) | 39 (78%) | 41 (75%) | 39 (63%) | 119 (71%) | 0.017 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mathee, A.; Moyes, J.; Mkhencele, T.; Kleynhans, J.; Language, B.; Piketh, S.; Moroe, E.; Wafawanaka, F.; Martinson, N.; McMorrow, M.; et al. Housing Quality in a Rural and an Urban Settlement in South Africa. Int. J. Environ. Res. Public Health 2021, 18, 2240. https://doi.org/10.3390/ijerph18052240
Mathee A, Moyes J, Mkhencele T, Kleynhans J, Language B, Piketh S, Moroe E, Wafawanaka F, Martinson N, McMorrow M, et al. Housing Quality in a Rural and an Urban Settlement in South Africa. International Journal of Environmental Research and Public Health. 2021; 18(5):2240. https://doi.org/10.3390/ijerph18052240
Chicago/Turabian StyleMathee, Angela, Jocelyn Moyes, Thulisa Mkhencele, Jackie Kleynhans, Brigitte Language, Stuart Piketh, Elias Moroe, Floidy Wafawanaka, Neil Martinson, Meredith McMorrow, and et al. 2021. "Housing Quality in a Rural and an Urban Settlement in South Africa" International Journal of Environmental Research and Public Health 18, no. 5: 2240. https://doi.org/10.3390/ijerph18052240
APA StyleMathee, A., Moyes, J., Mkhencele, T., Kleynhans, J., Language, B., Piketh, S., Moroe, E., Wafawanaka, F., Martinson, N., McMorrow, M., Tempia, S., Kahn, K., & Cohen, C. (2021). Housing Quality in a Rural and an Urban Settlement in South Africa. International Journal of Environmental Research and Public Health, 18(5), 2240. https://doi.org/10.3390/ijerph18052240






