Effectiveness of Food Fortification in Improving Nutritional Status of Mothers and Children in Indonesia
Abstract
1. Introduction
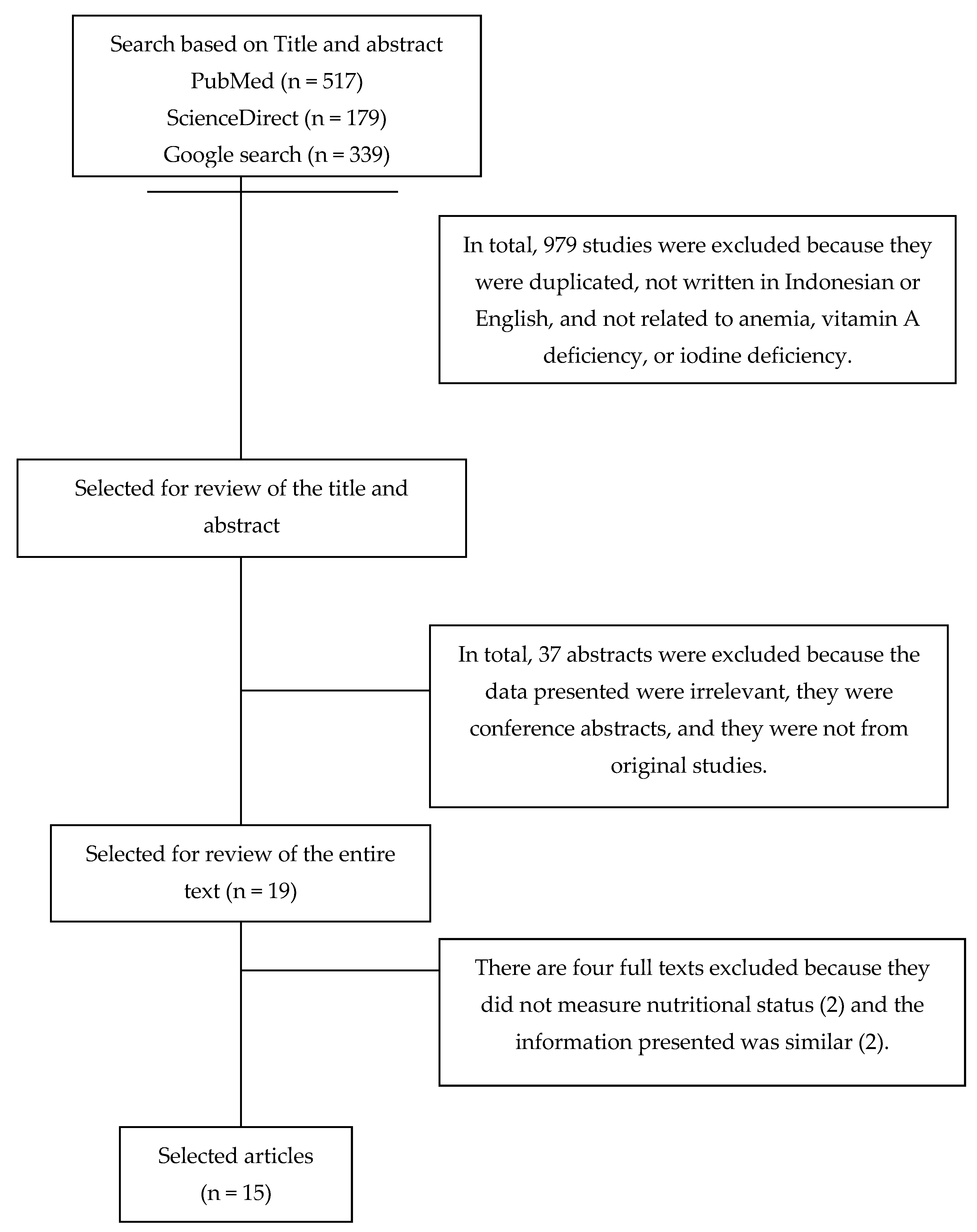
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ruel-Bergeron, J.C.; Stevens, G.A.; Sugimoto, J.D.; Roos, F.F.; Ezzati, M.; Black, R.E.; Kraemer, K. Global Update and Trends of Hidden Hunger, 1995-2011: The Hidden Hunger Index. PLoS ONE 2015, 10, e0143497. [Google Scholar] [CrossRef]
- Balitbangkes. Riset Kesehatan Dasar; Badan Penelitian dan Pengembangan Kesehatan Kementerian Kesehatan Republik Indonesia: Jakarta, Indonesia, 2018. [Google Scholar]
- Balitbangkes. Riset Kesehatan Dasar; Badan Penelitian dan Pengembangan Kesehatan Kementerian Kesehatan Republik Indonesia: Jakarta, Indonesia, 2013. [Google Scholar]
- Desmansyah, D.; Purnamasari, R.; Theodorus, T.; Waiman, S. Correlation between vivax malaria infection and iron deficiency in children. Paediatr. Indones. 2011, 51, 207–212. [Google Scholar] [CrossRef][Green Version]
- Zahrulianingdyah, A. The contribution of Indonesian women’s eating habit to iron deficiency anemia. Pakistan J. Nutr. 2016, 15, 1003–1007. [Google Scholar] [CrossRef][Green Version]
- Nurdia, D.S.; Sumarni, S.; Suyoko; Hakim, M.; Winkvist, A. Impact of intestinal helminth infection on anemia and iron status during pregnancy: A community based study in Indonesia. S. Asian J. Trop. Med. Public Health 2001, 32, 14–22. [Google Scholar]
- Andriastuti, M.; Ilmana, G.; Nawangwulan, S.A.; Kosasih, K.A. Prevalence of anemia and iron profile among children and adolescent with low socio-economic status. Int. J. Pediatr. Adolesc. Med. 2019. [Google Scholar] [CrossRef]
- Bening, S.; Margawati, A.; Rosidi, A. Zinc deficiency as risk factor for stunting among children aged 2-5 years. Universa Med. 2017, 36, 11–18. [Google Scholar] [CrossRef]
- Abdelhaleim, A.F.; Abdo Soliman, J.S.; Amer, A.Y.; Abdo Soliman, J.S. Association of Zinc Deficiency with Iron Deficiency Anemia and its Symptoms: Results from a Case-control Study. Cureus 2019, 11, e3811. [Google Scholar] [CrossRef]
- WHO. WHO Nutrition Landacape Information System (NLIS) Country Profile Indicators, Interpretation Guide; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Kementerian PPN/Bapennas. Rencana Pembangunan Jangka Menengah Nasional 2020–2024; Kementerian PPN/Bapennas: Jakarta, Indonesia, 2019. [Google Scholar]
- Arnold, T. Chapter 5.4 Nutrition-Specific and Nutrition-Sensitive Interventions. In Good Nutrition: Perspectives for the 21st Century; Karger: Basel, 2016; pp. 276–288. [Google Scholar]
- WHO. WHO and FAO Guidelines on Food Fortification with Micronutrients; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- Pilz, S.; März, W.; Cashman, K.D.; Kiely, M.E.; Whiting, S.J.; Holick, M.F.; Grant, W.B.; Pludowski, P.; Hiligsmann, M.; Trummer, C.; et al. Rationale and Plan for Vitamin D Food Fortification: A Review and Guidance Paper. Front. Endocrinol. (Lausanne) 2018, 9, 373. [Google Scholar] [CrossRef] [PubMed]
- Haas, J.D.; Luna, S.V.; Lung’aho, M.G.; Wenger, M.J.; Murray-Kolb, L.E.; Beebe, S.; Gahutu, J.-B.; Egli, I.M. Consuming Iron Biofortified Beans Increases Iron Status in Rwandan Women after 128 Days in a Randomized Controlled Feeding Trial. J. Nutr. 2016, 146, 1586–1592. [Google Scholar] [CrossRef]
- Finkelstein, J.L.; Fothergill, A.; Hackl, L.S.; Haas, J.D.; Mehta, S. Iron biofortification interventions to improve iron status and functional outcomes. Proc. Nutr. Soc. 2019, 78, 197–207. [Google Scholar] [CrossRef]
- Menteri Perindustrian. Peraturan Menteri Perindustrian Republik Indonesia Nomor 47 tahun 2018 tentang Perubahan Ketiga atas Peraturan Menteri Perindustrian Nomor 87/M-IND/PER/12/2013 tentang Pemberlakuan SNI Minyak Goreng Sawit Secara Wajib; Menteri Perindustrian Republik Indonesia: Jakarta, Indonesia, 2018. [Google Scholar]
- Minister of Industry. Minister of Industry and Trade Regulation Number 153/MPP/Kep/5/2001; Minister of Industry and Trade Republic of Indonesia: Jakarta, Indonesia, 2001. [Google Scholar]
- Presiden Republik Indonesia. Keputusan Presiden Republik Indonesia Nomor 69 Tahun 1994 tentang Pengadaan Garam Beriodium; Presiden Republik Indonesia: Jakarta, Indonesia, 1994. [Google Scholar]
- Sadighi, J.; Nedjat, S.; Rostami, R. Systematic review and meta-analysis of the effect of iron-fortified flour on iron status of populations worldwide. Public Health Nutr. 2019, 22, 3465–3484. [Google Scholar] [CrossRef]
- Athe, R.; Dwivedi, R.; Pati, S.; Mazumder, A.; Banset, U. Meta-analysis approach on iron fortification and its effect on pregnancy and its outcome through randomized, controlled trials. J. Fam. Med. Prim. Care 2020, 9, 513. [Google Scholar]
- Tam, E.; Keats, E.C.; Rind, F.; Das, J.K.; Bhutta, Z.A. Micronutrient Supplementation and Fortification Interventions on Health and Development Outcomes among Children Under-Five in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 289. [Google Scholar] [CrossRef]
- Pineda, O. Fortification of sugar with vitamin A. Food Nutr. Bull. 1998, 19, 131–136. [Google Scholar] [CrossRef]
- Favaro, R.M.D.; Miyasaaka, C.K.; Desai, I.D.; Dutra de Oliveira, J.E. Evaluation of the effect of heat treatment on the biological value of vitamin A fortified soybean oil. Nutr. Res. 1992, 12, 1357–1363. [Google Scholar] [CrossRef]
- Mendu, V.V.R.; Nair, K.P.M.; Athe, R. Systematic review and meta-analysis approach on vitamin A fortified foods and its effect on retinol concentration in under 10 year children. Clin. Nutr. ESPEN 2019, 30, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Hombali, A.S.; Solon, J.A.; Venkatesh, B.T.; Nair, N.S.; Peña-Rosas, J.P. Fortification of staple foods with vitamin A for vitamin A deficiency. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.A.R.; Christoforou, A.; Trieu, K.; McKenzie, B.L.; Downs, S.; Billot, L.; Webster, J.; Li, M. Iodine fortification of foods and condiments, other than salt, for preventing iodine deficiency disorders. Cochrane Database Syst. Rev. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Aburto, N.J.; Abudou, M.; Candeias, V.; Tiaxiang Wu, P. Effect and safety of salt iodization to prevent iodine deficiency disorders: A systematic review with meta-analyses WHO Library Cataloguing-in-Publication Data. In WHO eLibrary of Evidence for Nutrition Actions (eLENA); WHO: Geneva, Switzerland, 2014; pp. 91–93. [Google Scholar]
- Dijkhuizen, M.A.; Wieringa, F.T.; Soekarjo, D.; Van, K.T.; Laillou, A. Legal Framework for Food Fortification: Examples from Vietnam and Indonesia. Food Nutr. Bull. 2013, 34, S112–S123. [Google Scholar] [CrossRef]
- Sari, M.; Bloem, M.W.; de Pee, S.; Schultink, W.J.; Sastroamidjojo, S. Effect of iron-fortified candies on the iron status of children aged 4–6 y in East Jakarta, Indonesia. Am. J. Clin. Nutr. 2001, 73, 1034–1039. [Google Scholar] [CrossRef] [PubMed]
- Diana, A.; Mallard, S.R.; Haszard, J.J.; Purnamasari, D.M.; Nurulazmi, I.; Herliani, P.D.; Nugraha, G.I.; Gibson, R.S.; Houghton, L. Consumption of fortified infant foods reduces dietary diversity but has a positive effect on subsequent growth in infants from Sumedang district, Indonesia. PLoS ONE 2017, 12, e0175952. [Google Scholar] [CrossRef]
- Achadi, E.; Arifah, S.; Muslimatun, S.; Anggondowati, T.; Setiarini, A. Efektivitas Program Fortifikasi Minyak Goreng dengan Vitamin A terhadap Status Gizi Anak Sekolah di Kota Makasar. Kesmas Natl. Public Health J. 2010, 4, 255. [Google Scholar] [CrossRef]
- Sandjaja; Jusat, I.; Jahari, A.B.; Ifrad; Htet, M.K.; Tilden, R.L.; Soekarjo, D.; Utomo, B.; Moench-Pfanner, R.; Soekirman; et al. Vitamin A-fortified cooking oil reduces Vitamin A deficiency in infants, young children and women: Results from a programme evaluation in Indonesia. Public Health Nutr. 2015, 18, 2511–2522. [Google Scholar] [CrossRef] [PubMed]
- Sudikno, S.; Jus, I. The Impact of Vitamin A Fortified Vegetable Oil on Vitamin A Status of Children Under Five Years of Age: A Cohort Study. Health Sci. J. Indones. 2017, 8, 102–110. [Google Scholar] [CrossRef]
- Kasmawati. Pengaruh Pemberian Telur Beriodium terhadap Ekskresi Iodium Urin Penderita Defisiensi Yodium pada Anak Sekolah Dasar Kecamatan Pondidaha Kabupaten Konawe; Universitas Hasanuddin: Makassar, Indonesia, 2015. [Google Scholar]
- Samsudin, M.; Nurcahyani, Y.D.; Ihsan, N.; Litbang, B.; Magelang, G.; Jayan, K. Dampak Intervensi Garam Beriodium Berbagai Dosis Terhadap Status Iodium Dan Fungsi Tiroid Normal Pada Anak Sekolah Dasar. Media Gizi Mikro Indones. 2016, 8, 1–16. [Google Scholar]
- Samsudin, M.; Kusumawardani, H.; Prihatmi, E. Pengaruh penggunaan garam beriodium standar terhadap status iodium tinggi di daerah non endemik. Media Gizi Mikro Indones. 2015, 7, 57–66. [Google Scholar]
- Widayani, S. Efikasi Dan Preferensi Biskuit Yang Difortifikasi Vitamin A Dan Zat Besi (Fe) Dan Kaitannya Dengan Konsumsi, Status Gizi dan Respon Imun Anak Balita; IPB University: Bogor, Indonesia, 2007. [Google Scholar]
- Prihananto, V. Pengaruh Pemberian Pangan Yang Difortifikasi Zat Multi Gizi Mikro Terhadap Status Gizi Ibu Hamil Dan Berat Bayi Lahir; Dissertation; IPB University: Bogor, Indonesia, 2007. [Google Scholar]
- Saragih, B.; Syarief, H.; Riyadi, H.; Nasoetion, A. Pengaruh Pemberian Pangan Fortifikasi Zat Multi Gizi Mikro Pada Ibu Hamil Terhadap Pertumbuhan Linier, Tinggi Lutut Dan Status Anemia Bayi. Gizi Indones. 2007, 30. [Google Scholar] [CrossRef]
- Saragih, B.; Syarief, H.; Riyadi, H.; Nasoetion, A. Pangan yang difortifikasi zat gizi mikro pada ibu hamil meningkatkan perkembangan motorik bayi. J. Gizi Klin. Indones. 2012, 9, 16. [Google Scholar] [CrossRef]
- Toronju, S.A.; Syam, A.; Palutturi, S.; Arif, M. Study of Hemoglobin and Ferritin Profile as Indicators in Children Hematology of 12-15 Years Provided Local Rice Fortification. Int. J. Sci. Basic Appl. Res. 2017, 32, 352–364. [Google Scholar]
- Kurnia, P.; Rahmawaty, S. Efek Fortifikasi Fe dan Zn pada biskuit yang diolah dari kombinasi Tempe dan Bekatul untuk meningkatkan kadar Albumin Anak Balita Kurang Gizi dan Anemia. Eksplanasi 2010, 5, 1–14. [Google Scholar]
- Semba, R.D.; Moench-Pfanner, R.; Sun, K.; De Pee, S.; Akhter, N.; Rah, J.H.; Campbell, A.A.; Badham, J.; Bloem, M.W.; Kraemer, K. Consumption of micronutrient-fortified milk and noodles is associated with lower risk of stunting in preschool-aged children in Indonesia. Food Nutr. Bull. 2011, 32, 347–353. [Google Scholar] [CrossRef]
- BPS-Statistics Indonesia. Statistical Yearbook of Indonesia; BPS-Statistics Indonesia: Jakarta, Indonesia, 2019. [Google Scholar]
- Gera, T.; Sachdev, H.S.; Boy, E. Effect of iron-fortified foods on hematologic and biological outcomes: Systematic review of randomized controlled trials. Am. J. Clin. Nutr. 2012, 96, 309–324. [Google Scholar] [CrossRef] [PubMed]
- Minister of Health. Minister of Health Regulation No. 1452/MENKES/SK/X/2003; Minister of Health: Jakarta, Indonesia, 2003. [Google Scholar]
- Zofkova, I.; Davis, M.; Blahos, J. Trace elements have beneficial, as well as detrimental effects on bone homeostasis. Physiol. Res. 2017, 66, 391–402. [Google Scholar] [CrossRef]
- Toxqui, L.; Vaquero, M.P. Chronic iron deficiency as an emerging risk factor for osteoporosis: A hypothesis. Nutrients 2015, 7, 2324–2344. [Google Scholar] [CrossRef] [PubMed]
- Balogh, E.; Paragh, G.; Jeney, V. Influence of Iron on Bone Homeostasis. Pharmaceuticals 2018, 11, 107. [Google Scholar] [CrossRef] [PubMed]
- Owino, V.O.; Kasonka, L.M.; Sinkala, M.M.; Wells, J.K.; Eaton, S.; Darch, T.; Coward, A.; Tomkins, A.M.; Filteau, S.M. Fortified complementary foods with or without α-amylase treatment increase hemoglobin but do not reduce breast milk intake of 9-mo-old Zambian infants. Am. J. Clin. Nutr. 2007, 86, 1094–1103. [Google Scholar] [CrossRef] [PubMed]
- Ara, G.; Khanam, M.; Rahman, A.S.; Islam, Z.; Farhad, S.; Sanin, K.I.; Khan, S.S.; Rahman, M.M.; Majoor, H.; Ahmed, T. Effectiveness of micronutrient-fortified rice consumption on anaemia and zinc status among vulnerable women in Bangladesh. PLoS ONE 2019, 14, e0210501. [Google Scholar] [CrossRef]
- Angeles-agdeppa, I.; Capanzana, M.V.; Barba, C.V.C.; Florentino, R.F.; Takanashi, K. Efficacy of Iron-Fortified Rice in Reducing Anemia Among Schoolchildren in the Philippines. Int. J. Vitam. Nutr. Res. 2008, 78, 74–86. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Zhao, X.; Zhang, X.; Yin, S.; Piao, J.; Huo, J.; Yu, B.; Qu, N.; Lu, Q.; Wang, S.; et al. Studies on the Effectiveness of Nafeedta-Fortified Soy Sauce in Controlling Iron Deficiency: A Population-Based Intervention Trial. Food Nutr. Bull. 2005, 26, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Waller, A.W.; Andrade, J.E.; Mejia, L.A. Performance Factors Influencing Efficacy and Effectiveness of Iron Fortification Programs of Condiments for Improving Anemia Prevalence and Iron Status in Populations: A Systematic Review. Nutrients 2020, 12, 275. [Google Scholar] [CrossRef] [PubMed]
- Green, A.S.; Fascetti, A.J. Meeting the Vitamin A Requirement: The Efficacy and Importance of β-Carotene in Animal Species. Sci. World J. 2016, 2016, 7393620. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Chen, K.; Qu, P.; Liu, Y.-X.; Li, T.-Y. Effect of biscuits fortified with different doses of vitamin A on indices of vitamin A status, haemoglobin and physical growth levels of pre-school children in Chongqing. Public Health Nutr. 2010, 13, 1462–1471. [Google Scholar] [CrossRef] [PubMed]
- Allen, L.H. Anemia and iron deficiency: Effects on pregnancy outcome. Am. J. Clin. Nutr. 2000, 71, 1280S–1284S. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Huffman, S.L. Review of fortified food and beverage products for pregnant and lactating women and their impact on nutritional status. Matern. Child Nutr. 2011, 7, 19–43. [Google Scholar] [CrossRef] [PubMed]
- Darnton-Hill, I.; Mkparu, U.C. Micronutrients in Pregnancy in Low- and Middle-Income Countries. Nutrients 2015, 7, 1744–1768. [Google Scholar] [CrossRef]
- Branca, F.; Ferrari, M. Impact of Micronutrient Deficiencies on Growth: The Stunting Syndrome. Ann. Nutr. Metab. 2002, 46 (Suppl. 1), 8–17. [Google Scholar] [CrossRef]
- Habicht, J.-P.; Martorell, R.; Rivera, J.A. Nutritional Impact of Supplementation in the INCAP Longitudinal Study: Analytic Strategies and Inferences. J. Nutr. 1995, 125, 1042S–1050S. [Google Scholar]
- Okeyo, D.O. Impact of Food Fortification on Child Growth and Development during Complementary Feeding. Ann. Nutr. Metab. 2018, 73, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Das, J.K.; Salam, R.A.; Kumar, R.; Bhutta, Z.A. Micronutrient fortification of food and its impact on woman and child health: A systematic review. Syst. Rev. 2013, 2, 67. [Google Scholar] [CrossRef]
| No. | Reference | Year | Study Design | Sample Amount (n) | Group | Location (Province) | Duration (Days) |
|---|---|---|---|---|---|---|---|
| Iron | |||||||
| 1. | Sari [30] | 2001 | RCT | 132 | 4–6 years old | Jakarta | 21 |
| 2. | Diana [31] | 2017 | Cohort | 190 | 6 months followed up to 12 months old | West Java | 84 |
| Vitamin A | |||||||
| 1. | Achadi [32] | 2010 | Quasi-experimental | 394 | 8–9 years old | South Sulawesi | 84 |
| 2. | Sandjaja [33] | 2015 | Quasi experimental | Breastfeeding mother: 335, 12–59 months old: 477, 5–9 years old: 186, woman 15–29 years old: 171 | Breastfeeding mother, baby aged 6–11 months, children aged 12–59 months, children aged 5–9 years, women aged 15–29 years | West Java | 336 |
| 3. | Sudikno [34] | 2017 | Cohort | 126 | Children of poor family, 6–59 months old | West Java | 336 |
| Iodine | |||||||
| 1. | Kasmawati [35] | 2015 | Non-RCT | 26 | 10–12 years old with urinary iodine excretion value of <100 μg/L | South Sulawesi | 10 |
| 2. | Samsudin [37] | 2015 | Quasi-experimental | 160 | 4–9 years old | Central Java | 168 |
| 3. | Samsudin [36] | 2016 | RCT | 176 | 6–12 years old | Central Java | 168 |
| Multinutrient | |||||||
| 1. | Widayanti [38] | 2007 | RCT | 70 | ≤5 years old | West Java | 112 |
| 2. | Prihananto [39] | 2007 | RCT | 210 | Pregnant mothers | West Java | 168 |
| 3. | Saragih [40] | 2007 | Cohort | 120 | Pregnant mothers with babies up to 6 months old | West Java | 336 |
| 4. | Saragih [41] | 2012 | Cohort | 120 | Pregnant mothers with babies up to 6 months old | West Java | 336 |
| 5. | Kurnia [43] | 2010 | Quasi-experimental | 91 | ≤5 years old | Central Java | 84 |
| 6. | Semba [44] | 2011 | Cross-sectional | 302,190 | 6–59 months old | West Sumatera, Lampung, Banten, Jakarta, West Java, Central Java, East Java, West Nusa Tenggara, South Sulawesi | - |
| 7. | Diana [31] | 2017 | Cohort | 190 | 6 months followed up to 12 months old | West Java | 84 |
| 8. | Toruntju [42] | 2017 | RCT | 80 | Boys, 12–15 years old, with Hb concentration of 8–12 mg% | West Java | 168 |
| Study | Type and Level of Fortification | Food Vehicle |
|---|---|---|
| Iron | ||
| Sari [30] | Iron 30 mg, weekly dose | Candies |
| Diana [31] | Iron | Baby food |
| Vitamin A | ||
| Achadi [32] | Vitamin A: 13.6 mg retinol/kg | Cooking oil |
| Sandjaja [33] | Vitamin A: 13.6 mg retinol/kg | Cooking oil |
| Sudikno [34] | Vitamin A: 13.6 mg retinol/kg | Cooking oil |
| Iodine | ||
| Kasmawati [35] | Iodine: 0.4 mg/kg KIO3 | Eggs |
| Samsudin [37] | Iodine: ≥30 mg/kg KIO3 | Salt |
| Samsudin [36] | Iodine: 15–55 mg/kg KIO3 | Salt |
| Multinutrient | ||
| Widayanti [38] | 235.65 μg of vitamin A and 4.17 mg of iron/100 g of biscuits. 76 g in a week | Biscuits |
| Prihananto [39], Saragih [40], Saragih [41] |
| Vermicelli, milk, biscuits |
| Kurnia [43] | Iron and zinc 10 mg/100 g biscuits. 300 g in a week | Tempeh rice-bran biscuits |
| Semba [44] | Vitamin A, vitamin C, vitamin D, vitamin E, vitamin K, vitamin B12, thiamine, and riboflavin Vitamin B6, niacin, folic acid, and iron. | Milk and instant noodles |
| Diana [31] | Iron, zinc, calcium, vitamin A | Baby food |
| Toruntju [42] | Iron, Zn, vitamin B1, vitamin B3, folic acid, and vitamin B12 | Rice |
| Study | Outcome | |||
|---|---|---|---|---|
| Nutritional Status | Prevalence (%) | |||
| Nonfortification Group | Fortification Group | Nonfortification Group | Fortification Group | |
| Iron | ||||
| Sari [30] | ∆Hb (g/L) | Anemia (Hb < 11 g/dL) | ||
| ↑4.0 (95%CI: 2.0–6.0) | ↑10.2 (95%CI: 8.3–12) | ↓16.6 | ↓48.9 * | |
| SF (μg/l) | ID (SF < 12 μg/L) | |||
| ↑28% | ↑71% | ↓35.1 | ↓13.4 | |
| Diana [31] | BL/A | n/a | ||
| Iron: β = 0.22; 95% CI: 0.01–0.44 Others: β = 0.29; 95%CI: 0.09–0.48 | ||||
| W/BL (kg/cm) | ||||
| Iron: β = −0.22; 95%CI: −0.42–0.00 Others: β = −0.09; 95%CI: −0.29–0.11 | ||||
| W/A | ||||
| Iron: β= −0.03; 95%CI: −0.15–0.10 Others: β = 0.14; 95%CI: 0.02–0.26 | ||||
| Vitamin A | ||||
| Achadi [32] | SR (μg/dL) | Anemia (Hb < 11.5 g/dL) | ||
| 23 | 22.2 | 21.8 | 11.6. | |
| VAD (SR < 20 ug/dL) | ||||
| 38.4 | 38.8 ≥12 weeks: 26.6% <12 weeks: 42% | |||
| Sandjaja [33] | ∆SR (μg/dL) | KVA (SR < 20 ug/dL) | ||
| 6–11 months: 12.3 ** 12–23 months: 2.2 24–59 months: 6.4 5–9 years: 14.9 ** Breastfeeding mother: 13.1 ** Nonbreastfeeding mother aged 15–29 years: 19.1 ** | 6.5–18 | 0.6–6 * | ||
| Sudikno [34] | ∆SR (μg/dL) | VAD (SR < 20 ug/dL) | ||
| 29.36 ± 1.07 | 35.19 ± 0.89 ** | 19.0 | 5.6 * | |
| ∆Hb (g/L) | Anemia (Hb < 11 g/dL) | |||
| 11.18 ± 0.12 | 11.59 ± 0.14 | 43.7 | 28.6 ** | |
| Iodine | ||||
| Kasmawati [35] | ∆UIE (μg/L) | n/a | ||
| 6.38 | 12.4 ** | |||
| Samsudin [37] | UIE (μg/L) | ID (UIE < 100μg/L) | ||
| Coastal: 191 Noncoastal: 96 | Coastal: 148* Noncoastal: 83 | Coastal: 10.4 Noncoastal: 51.8 | Coastal: 28.6 Noncoastal: 60.2 | |
| Samsudin [36] | UIE (μg/L) | ID (UIE < 100μg/L) | ||
| 222 | 238 | 14 | 13 | |
| TSH (μIU/mL) | ||||
| 1.9(0.5–4.0) | 1.8 (0.2–5.9) | |||
| Multinutrient | ||||
| Widayanti [38] | ∆Hb (g/L) | Anemia (Hb < 11 g/dL) | ||
| ↑0.17 ± 1.05 | ↑ 0.67 ± 1.11 ** | ↓ 20 | ↓ 22.8 | |
| ∆SF (μg/L) | IDA (SF < 12μg/L) | |||
| ↑8.27 ± 4.55 | ↑ 11.43 ± 4.47 ** | ↓ 2.9 | ↓ 17.2 | |
| ∆SR (μg/dL) | VAD (SR < 20 ug/dL) | |||
| ↑4.38 ± 7.72 | ↑ 10.12 ± 7.84 ** | ↓ 22.6 | ↓ 44.1 | |
| ∆W/L (kg/cm) | Wasting | |||
| −0.07 ± 0.66 | −0.01 ± 1.07 | 14.3 | 5.7 | |
| Prihananto [39] | ∆Hb (g/L) | Anemia (Hb < 11 g/dL) | ||
| Pl: ↓1, C: ↓1.1 | ↓ 0.2 * | Pl: 77.6, C: 86.2 | 48.3 * | |
| ∆SF (μg/L) | ∆IDA (SF < 12μg/L) | |||
| Pl: ↓0.25, C: ↓0.32 | 0.23 a | Pl: ↑ 71.7, C: ↑ 63.3 | ↑ 39.4 | |
| BW (kg) | VAD (SR < 20 ug/dL) | |||
| Pl: 3.06 ± 0.34, C: 2.98 ± 0.32 | 3.01 ± 0.27 | Pl: 20.3, C: 39.7 | 17.2 | |
| LBW (BW < 2.5 kg) | ||||
| Pl: 5.3, C: 3.6 | 0 | |||
| Saragih [40] | ∆BL (cm) | n/a | ||
| Pl: 16.41 ± 1.41 C: 15.76 + 1.70 | 17.94 ± 1.83 * | |||
| ∆BL/A | ||||
| Pl: −0.26 ± 0.88 C: −0.52 ± 1.16 | 0.50 ± 0.92 * | |||
| ∆KH (cm) | ||||
| Pl: 4.02 ± 0.71 C: 3.80 ± 0.74 | 4.47 ± 0.64 | |||
| Saragih [41] | Hb (g/L) | Anemia (Hb < 11 g/dL) | ||
| Pl: 83.0–123.2 C: 70.6–120.3 | 95.7–120.0 | Pl: 44.4 C: 63.9 | 47.2 | |
| Anemia (Ht < 33%) | ||||
| Pl: 30.6 C: 38.9 | 27.8 | |||
| Kurnia [43] | Albumin (g/dL) | n/a | ||
| Pl: 1.09 ± 1.38C: 0.92 ± 0.41 | 0.95 ± 0.50 | |||
| W (kg) | ||||
| Pl: 0.99 ± 1.45C: 0.24 ± 0.65 | 0.61 ± 2.34 | |||
| Semba [44] | Milk | |||
| Stunting Village, OR = 0.87; 95% CI, 0.85 to 0.90 City, OR = 0.80; 95% CI, 0.76 to 0.85 | Village 56.2 City 53.7 | Village 43.4 ** City 42.8 ** | ||
| Noodles | ||||
| Village, OR = 0.95; 95% CI, 0.91 to 0.99 Jakarta, OR = 0.95; 95% CI, 0.91 to 1.01 | Village 53.6 City 51.5 | Village 45.6 ** City 45.9 ** | ||
| Toruntju [42] | ∆Hb (g/L) | n/a | ||
| ↑0.7 | ↑ 0.41 | |||
| ∆SF (μg/L) | ||||
| ↑0.77 | ↓ 9.94 | |||
| Sudikno [34] | ∆SR (μg/dL) | VAD (SR < 20 ug/dL) | ||
| 29.36 ± 1.07 | 35.19 ± 0.89 ** | 19.0 | 5.6 * | |
| ∆Hb (g/L) | Anemia (Hb < 11 g/dL) | |||
| 11.18 ± 0.12 | 11.59 ± 0.14 | 43.7 | 28.6 ** | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dewi, N.U.; Mahmudiono, T. Effectiveness of Food Fortification in Improving Nutritional Status of Mothers and Children in Indonesia. Int. J. Environ. Res. Public Health 2021, 18, 2133. https://doi.org/10.3390/ijerph18042133
Dewi NU, Mahmudiono T. Effectiveness of Food Fortification in Improving Nutritional Status of Mothers and Children in Indonesia. International Journal of Environmental Research and Public Health. 2021; 18(4):2133. https://doi.org/10.3390/ijerph18042133
Chicago/Turabian StyleDewi, Nikmah Utami, and Trias Mahmudiono. 2021. "Effectiveness of Food Fortification in Improving Nutritional Status of Mothers and Children in Indonesia" International Journal of Environmental Research and Public Health 18, no. 4: 2133. https://doi.org/10.3390/ijerph18042133
APA StyleDewi, N. U., & Mahmudiono, T. (2021). Effectiveness of Food Fortification in Improving Nutritional Status of Mothers and Children in Indonesia. International Journal of Environmental Research and Public Health, 18(4), 2133. https://doi.org/10.3390/ijerph18042133







