Carpal Tunnel Syndrome: A National Survey to Monitor Knowledge and Operating Methods
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Settings
2.3. Development of the Questionnaire
2.4. Data Collection
2.5. Data Analysis
3. Results
3.1. Subjects
3.2. Primary Outcome
3.3. Secondary Outcome
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- Age:
- <29 years
- 30–39 years
- 40–49 years
- >50 years
- Gender:
- Male
- Female
- Years of clinical practice:
- <5 years
- 5–10 years
- 11–20 years
- >20 years
- Current academic degree (select the highest degree):
- Bachelor’s degree in Physiotherapy
- First level university master degree
- Master of science degree in Rehabilitation Sciences of Health Professions
- PhD degree
- Workplace:
- Hospital
- Private practice
- Rehabilitation Center specialized in hand and wrist rehabilitation
- Sports club, association or federation
- University (teaching or research activity)
- Field of work:
- Musculoskeletal
- Geriatric
- Neurological
- Other
- Italian Region:
- North
- South
- Center
- Patients with Carpal Tunnel Syndrome/year:
- 1–5
- 6–10
- 11–15
- 15
- Carpal Tunnel Syndrome: what is it?
- A neurological condition caused by compression of the median nerve due to an increase in pressure within the carpal tunnel
- A neurological condition caused by compression of the ulnar nerve due to an increase in pressure within the carpal tunnel
- A pathology that affects the flexor tendons of the fingers in the passage within the carpal tunnel due to functional overload
- A pathology affecting the median nerve due to an increase in pressure within the Guyon canal
- Which of these causes do you think is the most likely for developing Carpal Tunnel Syndrome?
- Collagen alteration
- Reduction of space within the Guyon canal
- Reduction of space within the carpal canal
- Presence of a scaphoid osteophyte
- Do you think that a patient with Carpal Tunnel Syndrome is the responsibility of the physical therapist?
- Yes
- No
- Yes, but only in the case of preventive median nerve conduction studies (electromyography-EMG)
- Yes, but only in the case of a preventive specialist medical examination
- Which risk factors seem to be most associated with Carpal Tunnel Syndrome?
- Female gender, obesity, diabetes and pregnancy
- Age (<70), male gender and diabetes
- Alcohol, smoking and hormonal pathologies
- Diabetes, male gender, age (>60)
- Do you agree that there is an association between Carpal Tunnel Syndrome and computer use?
- Yes
- No
- Only when exceeding 10 h per day
- If it is accompanied with the use of a non-ergonomic mouse
- What signs and symptoms can characterize Carpal Tunnel Syndrome?
- Alteration of the sensitivity of the palm, in particular of the thenar eminence
- Altered sensitivity, tingling and numbness of the first three fingers
- Joint limitation of the radiocarpal joint
- Strength deficit of the muscles of the hypothenar eminence
- During the physical examination it is possible to find:
- Hypotrophy of the dorsal and palmar aspect of the hand, including thenar and hypothenar eminence
- Hypotrophy of the hypothenar eminence
- Hypotrophy of the thenar eminence
- Oedema localized to the distal joints
- Best tools for the examination of tactile sensitivity:
- A pin
- The Semmes-Weinstein Monofilament
- There is no appropriate tool
- The description of the patient is sufficient
- Which clinical tests would you use most frequently during the evaluation of a patient with probable Carpal Tunnel Syndrome?
- Wrist flexion test (Phalen’s test), nerve percussion test (Tinel’s sign), Functional Dexterity test and two-point discrimination
- Phalen’s maneuver, Upper Limb Neurodynamic Test 3 (ULNT-3 for ulnar nerve), two-point discrimination test
- Resisted wrist extension test (Cozen’s test), sensitivity evaluation in the thenar eminence and in the palmar aspect of the hand
- Phalen’s maneuver, Upper Limb Neurodynamic Test 1 (ULNT-1 for median nerve) and test for stability between the scaphoid and other carpal bones (Watson’s Test)
- What outcome measures would you use to evaluate the patient with Carpal Tunnel Syndrome?
- Administration of a pain scale, such as the Visual Analog Scale (VAS) or the Numeric Pain Rating Scale (NPRS)
- Measurement of strength with dynamometer and manual dexterity
- Measurement of strength with dynamometer and of sensitivity, manual dexterity, strength and pain and administration of a questionnaire for the evaluation of symptoms and function
- Interview with the patient
- Would you advice-or directly build-an orthotic for the management of patients with Carpal Tunnel Syndrome?
- Yes
- No
- No, it’s contraindicated
- Yes, but only if the disorder is accompanied by rhizarthrosis
- How is the evidence supporting the use of instrumental therapies in the management of patients with Carpal Tunnel Syndrome?
- Weak/moderate, but I still use them in my clinical practice
- Weak/moderate; I don’t use instrumental therapies in my clinical practice
- Strong, therefore I use them in my clinical practice
- Strong, but I don’t use them in my clinical practice
- Do you think that the neural mobilization techniques (neurodynamic) and tendon gliding exercises are supported by evidence in literature?
- Yes, there is strong evidence and that’s why I use these techniques in my clinical practice
- Yes, there is strong evidence but I don’t use these techniques in my clinical practice
- No, there is limited evidence and that’s why I don’t use these techniques in my clinical practice
- There is limited evidence, but I still use these techniques in my clinical practice
- Which treatment strategy would you use most frequently for the management of patients with Carpal Tunnel Syndrome?
- Massage therapy, instrumental therapy
- Education, manual therapy, myofascial therapy, therapeutic exercise
- Joint mobilization of the radiocarpal joint, stretching
- None of the previous answers
- Do you think that psychosocial factors involving the processes of central sensitization can influence outcomes of patients with Carpal Tunnel Syndrome?
- Yes, and I adapt my clinical practice accordingly
- Yes, but I don’t know how to adapt my clinical practice
- No, psychosocial factors do not influence the outcomes of these patients
- Yes, and my clinical practice is only aimed at the education and explanation of these processes
- Do you think that the surgical approach can be the solution for patients with Carpal Tunnel Syndrome?
- Never
- Yes, in cases of failure of conservative treatment (persistence of symptoms)
- Yes, always
- Yes, in the presence of stenosing tenosynovitis
Appendix B
| Question | Possible Choices | Frequency | Percentage | Missing |
|---|---|---|---|---|
| Q:9 Carpal Tunnel Syndrome: what is it? | A neurological condition caused by compression of the median nerve due to an increase in pressure within the carpal tunnel | 469 | 92.3 | 0 |
| A neurological condition caused by compression of the ulnar nerve due to an increase in pressure within the carpal tunnel | 5 | 0.98 | ||
| A pathology that affects the flexor tendons of the fingers in the passage within the carpal tunnel due to functional overload | 16 | 3.15 | ||
| A pathology affecting the median nerve due to an increase in pressure within the Guyon canal | 18 | 3.54 | ||
| Q:10 Which of these causes do you think is the most likely for developing Carpal Tunnel Syndrome? | Collagen alteration | 13 | 2.56 | 1 |
| Reduction of space within the Guyon canal | 37 | 7.28 | ||
| Reduction of space within the carpal canal | 455 | 89.6 | ||
| Presence of a scaphoid osteophyte | 2 | 0.39 | ||
| Q:11 Do you think that a patient with Carpal Tunnel Syndrome is the responsibility of the physical therapist? | Yes | 360 | 70.9 | 0 |
| No | 4 | 0.80 | ||
| Yes, but only in the case of preventive median nerve conduction studies (electromyography-EMG) | 66 | 12.99 | ||
| Yes, but only in the case of a preventive specialist medical examination | 78 | 15.35 | ||
| Q:12 Which risk factors seem to be most associated with Carpal Tunnel Syndrome? | Female gender, obesity, diabetes and pregnancy | 448 | 88.20 | 1 |
| Age (<70), male gender and diabetes | 14 | 2.75 | ||
| Alcohol, smoking and hormonal pathologies | 26 | 5.12 | ||
| Diabetes, male gender, age (>60) | 20 | 3.94 | ||
| Q:13 Do you agree that there is an association between Carpal Tunnel Syndrome and computer use? | Yes | 298 | 58.70 | 1 |
| No | 89 | 17.50 | ||
| Only when exceeding 10 hours per day | 83 | 16.30 | ||
| If it is accompanied with the use of a non-ergonomic mouse | 37 | 7.30 | ||
| Q:14 What signs and symptoms can characterize Carpal Tunnel Syndrome? | Alteration of the sensitivity of the palm, in particular of the thenar eminence | 80 | 15.70 | 0 |
| Altered sensitivity, tingling and numbness of the first three fingers | 415 | 81.70 | ||
| Joint limitation of the radiocarpal joint | 5 | 0.98 | ||
| Strength deficit of the muscles of the hypothenar eminence | 8 | 1.57 | ||
| Q:15 During the physical examination it is possible to find? | Hypotrophy of the dorsal and palmar aspect of the hand, including thenar and hypothenar eminence | 81 | 15.95 | 2 |
| Hypotrophy of the hypothenar eminence | 31 | 6.10 | ||
| Hypotrophy of the thenar eminence | 380 | 74.80 | ||
| Oedema localized to the distal joints | 14 | 2.75 | ||
| Q:16 Best tools for the examination of tactile sensitivity? | A pin | 90 | 17.70 | 5 |
| The Semmes-Weinstein Monofilament | 264 | 52.00 | ||
| There is no appropriate tool | 76 | 15.00 | ||
| The description of the patient is sufficient | 73 | 14.40 | ||
| Q:17 Which clinical tests would you use most frequently during the evaluation of a patient with probable Carpal Tunnel Syndrome? | Wrist flexion test (Phalen’s maneuver), nerve percussion test (Tinel’s sign), Functional Dexterity test and two-point discrimination | 341 | 67.12 | 8 |
| Phalen’s maneuver, Upper Limb Neurodynamic Test 3 (ULNT-3 for ulnar nerve), two-point discrimination test | 33 | 6.48 | ||
| Resisted wrist extension test (Cozen’s test), sensitivity evaluation in the thenar eminence and in the palmar aspect of the hand | 35 | 6.89 | ||
| Phalen’s maneuver, Upper Limb Neurodynamic Test 1 (ULNT-1 for median nerve) and test for stability between the scaphoid and other carpal bones (Watson’s Test) | 91 | 17.91 | ||
| Q:18 What outcome measures would you use to evaluate the patient with Carpal Tunnel Syndrome? | Administration of a pain scale, such as the Visual Analog Scale (VAS) or the Numeric Pain Rating Scale (NPRS) | 42 | 8.27 | 3 |
| Measurement of strength with dynamometer and manual dexterity | 8 | 1.57 | ||
| Measurement of strength with dynamometer and of sensitivity, manual dexterity, strength and pain and administration of a questionnaire for the evaluation of symptoms and function | 423 | 83.27 | ||
| Interview with the patients | 32 | 6.28 | ||
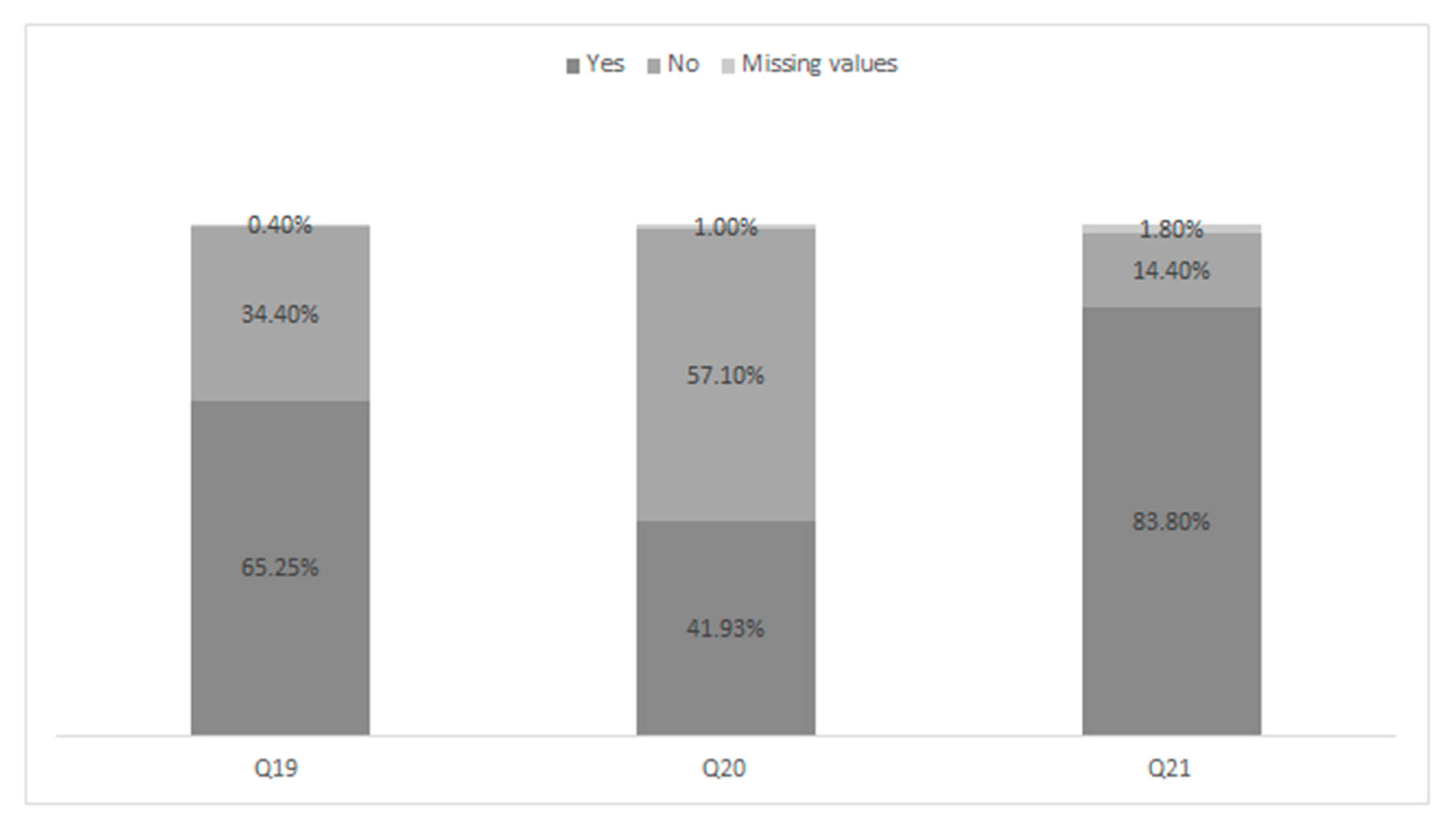
| Q:19 Would you advice-or directly build–an orthotic for the management of patients with Carpal Tunnel Syndrome? | Yes | 269 | 52.95 | 2 |
| No | 163 | 32.28 | ||
| No, it’s contraindicated | 12 | 2.46 | ||
| Yes, but only if the disorder is accompanied by rhizarthrosis | 62 | 12.30 | ||
| Q:20 How is the evidence supporting the use of instrumental modalities in the management of patients with Carpal Tunnel Syndrome? | Weak/moderate, but I still use them in my clinical practice | 194 | 38.20 | 5 |
| Weak/moderate; I don’t use instrumental therapies in my clinical practice | 285 | 56.10 | ||
| Strong, therefore I use them in my clinical practice | 19 | 3.73 | ||
| Strong, but I don’t use them in my clinical practice | 5 | 0.98 | ||
| Q:21 Do you think that the neural mobilization techniques (neurodynamic) and tendon gliding exercises are supported by evidence in literature? | Yes, there is strong evidence and that’s why I use these techniques in my clinical practice | 175 | 34.40 | 9 |
| Yes, there is strong evidence but I don’t use these techniques in my clinical practice | 38 | 7.51 | ||
| No, there is limited evidence and that’s why I don’t use these techniques in my clinical practice | 38 | 7.51 | ||
| There is limited evidence, but I still use these techniques in my clinical practice | 251 | 49.40 | ||
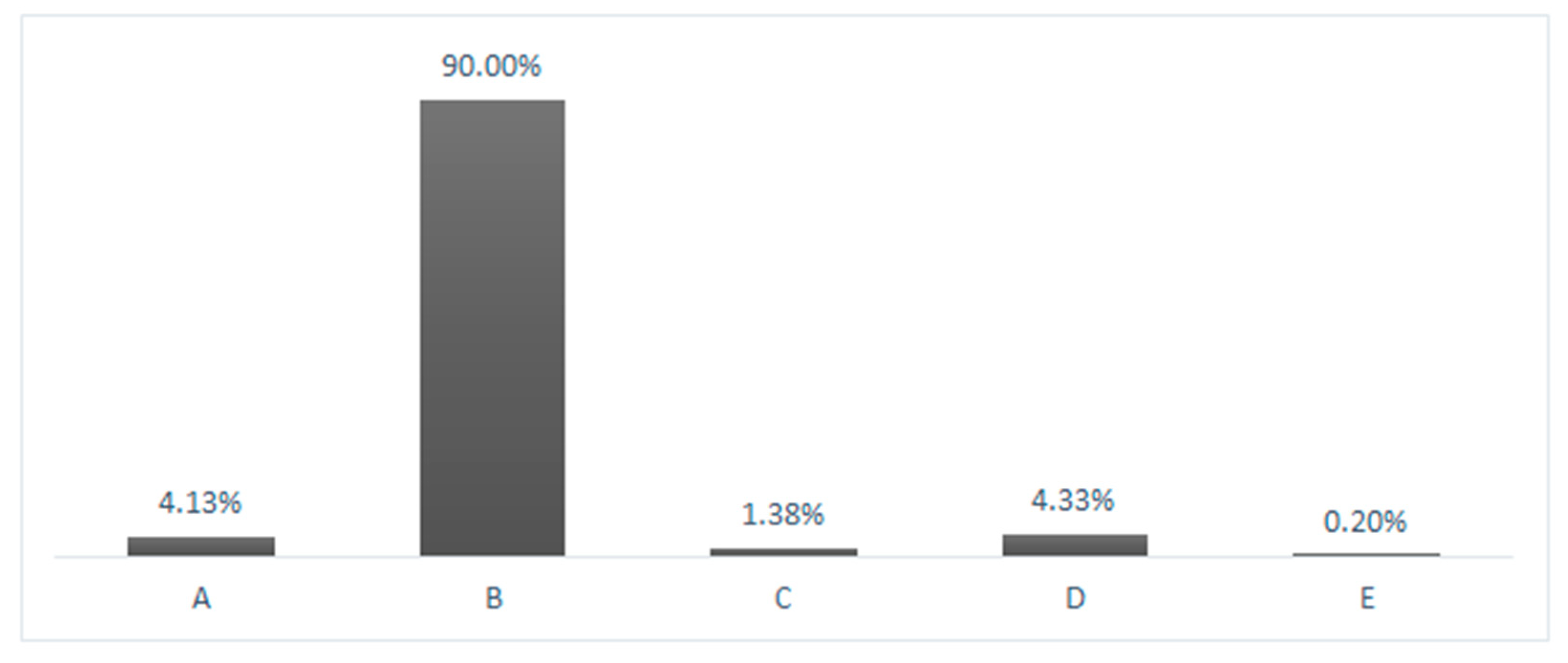
| Q:22 Which treatment strategy would you use most frequently for the management of patients with Carpal Tunnel Syndrome? | Massage therapy, instrumental therapy | 21 | 4.13 | 1 |
| Education, manual therapy, myofascial therapy, therapeutic exercise | 457 | 89.88 | ||
| Joint mobilization of the radiocarpal joint, stretching | 7 | 1.38 | ||
| None of the previous answers | 22 | 4.33 | ||
| Q:23 Do you think that psychosocial factors involving the processes of central sensitization can influence outcomes of patients with Carpal Tunnel Syndrome? | Yes, and I adapt my clinical practice accordingly | 364 | 71.68 | 2 |
| Yes, but I don’t know how to adapt my clinical practice | 83 | 16.34 | ||
| No, psychosocial factors do not influence the outcomes of these patients | 23 | 4.48 | ||
| Yes, and my clinical practice is only aimed at the education and explanation of these processes | 36 | 7.09 | ||
| Q:24 Do you think that the surgical approach can be the solution for patients with Carpal Tunnel Syndrome? | Never | 12 | 2.36 | 1 |
| Yes, in cases of failure of conservative treatment (persistence of symptoms) | 468 | 92.08 | ||
| Yes, always | 6 | 1.18 | ||
| Yes, in the presence of stenosing tenosynovitis | 21 | 4.13 |
References
- Lawrence, R.C.; Felson, D.T.; Helmick, C.G.; Arnold, L.M.; Choi, H.; Deyo, R.A.; Gabriel, S.; Hirsch, R.; Hochberg, M.C.; Hunder, G.G.; et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part II. Arthritis Rheum. 2007, 58, 26–35. [Google Scholar] [CrossRef]
- Dale, A.M.; Harris-Adamson, C.; Rempel, D.; Gerr, F.; Hegmann, K.; Silverstein, B.; Burt, S.; Garg, A.; Kapellusch, J.; Merlino, L.; et al. Prevalence and incidence of carpal tunnel syndrome in US working populations: Pooled analysis of six prospective studies. Scand. J. Work. Environ. Health 2013, 39, 495–505. [Google Scholar] [CrossRef]
- ANMIL. Musculoskeletal and Biomechanical Overload Disorders of Workers in the Commercial Sector: A Comparative Picture. 2013. Available online: http://www.ctr.it/back_end/files_news/1577.pdf (accessed on 10 January 2021).
- INAIL. Accidents and Occupational Diseases, Inail Open Data for the First Five Months of 2019–2020 Are Online. 2020. Available online: https://www.inail.it/cs/internet/comunicazione/sala-stampa/comunicati-stampa/com-stampa-open-data-maggio-2020.html (accessed on 10 January 2021).
- Spector, J.T.; Turner, J.A.; Fulton-Kehoe, D.; Franklin, G. Pre-surgery disability compensation predicts long-term disability among workers with carpal tunnel syndrome. Am. J. Ind. Med. 2012, 55, 816–832. [Google Scholar] [CrossRef][Green Version]
- Nuckols, T.; Conlon, C.; Robbins, M.; Dworsky, M.; Lai, J.; Roth, C.P.; Levitan, B.; Seabury, S.; Seelam, R.; Asch, S.M. Quality of care for work-associated carpal tunnel syndrome. J. Occup. Environ. Med. 2017, 59, 47–53. [Google Scholar] [CrossRef]
- Wright, C.; Smith, B.; Wright, S.; Weiner, M.; Wright, K.; Rubin, D. Who develops carpal tunnel syndrome during pregnancy: An analysis of obesity, gestational weight gain, and parity. Obstet. Med. 2014, 7, 90–94. [Google Scholar] [CrossRef]
- Shiri, R.; Pourmemari, M.H.; Falahhassani, K.; Viikarijuntura, E. The effect of excess body mass on the risk of carpal tunnel syndrome: A meta-analysis of 58 studies. Obes. Rev. 2015, 16, 1094–1104. [Google Scholar] [CrossRef]
- Harris-Adamson, C.; Eisen, A.E.; Dale, A.M.; Evanoff, B.; Hegmann, K.T.; Thiese, M.S.; Kapellusch, J.M.; Garg, A.; Burt, S.; Bao, S.; et al. Personal and workplace psychosocial risk factors for carpal tunnel syndrome: A pooled study cohort. Occup. Environ. Med. 2013, 70, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Harris-Adamson, C.; Eisen, A.E.; Kapellusch, J.; Garg, A.; Hegmann, K.T.; Thiese, M.S.; Dale, A.M.; Evanoff, B.; Burt, S.; Bao, S.; et al. Biomechanical risk factors for carpal tunnel syndrome: A pooled study of 2474 workers. Occup. Environ. Med. 2014, 72, 33–41. [Google Scholar] [CrossRef]
- Harris-Adamson, C.; Eisen, A.E.; Neophytou, A.; Kapellusch, J.; Garg, A.; Hegmann, K.T.; Thiese, M.S.; Dale, A.M.; Evanoff, B.; Bao, S.; et al. Biomechanical and psychosocial exposures are independent risk factors for carpal tunnel syndrome: Assessment of confounding using causal diagrams. Occup. Environ. Med. 2016, 73, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Al-Hashem, F.H.; Khalid, M.-E.M. The effect of long-term use of computer mouse devices on median nerve entrapment. Neuroscience 2008, 13, 131–135. [Google Scholar]
- Andersen, J.H.; Fallentin, N.; Thomsen, J.F.; Mikkelsen, S. Risk factors for neck and upper extremity disorders among computers users and the effect of interventions: An overview of systematic reviews. PLoS ONE 2011, 6, e19691. [Google Scholar] [CrossRef]
- Mediouni, Z.; Bodin, J.; Dale, A.M.; Herquelot, E.; Carton, M.; Leclerc, A.; Fouquet, N.; Dumontier, C.; Roquelaure, Y.; Evanoff, B.; et al. Carpal tunnel syndrome and computer exposure at work in two large complementary cohorts. BMJ Open 2015, 5, e008156. [Google Scholar] [CrossRef]
- Petit, A.; Ha, C.; Bodin, J.; Rigouin, P.; Descatha, A.; Brunet, R.; Goldberg, M.; Roquelaure, Y. Risk factors for carpal tunnel syndrome related to the work organization: A prospective surveillance study in a large working population. Appl. Ergon. 2015, 47, 1–10. [Google Scholar] [CrossRef]
- Rempel, D.M.; Keir, P.J.; Bach, J.M. Effect of wrist posture on carpal tunnel pressure while typing. J. Orthop. Res. 2008, 26, 1269–1273. [Google Scholar] [CrossRef] [PubMed]
- Calandruccio, J.H.; Thompson, N.B. Carpal tunnel syndrome. Orthop. Clin. N. Am. 2018, 49, 223–229. [Google Scholar] [CrossRef]
- Kozak, A.; Schedlbauer, G.; Wirth, T.; Euler, U.; Westermann, C.; Nienhaus, A. Association between work-related biomechanical risk factors and the occurrence of carpal tunnel syndrome: An overview of systematic reviews and a meta-analysis of current research. BMC Musculoskelet. Disord. 2015, 16, 231. [Google Scholar] [CrossRef]
- Mattioli, S.; Violante, F.S.; Bonfiglioli, R. Upper-extremity and neck disorders associated with keyboard and mouse use. Handb. Clin. Neurol. 2015, 131, 427–433. [Google Scholar] [CrossRef]
- Coenen, P.; Van Der Molen, H.F.; Burdorf, A.; Huysmans, M.; Straker, L.; Frings-Dresen, M.H.; Van Der Beek, A.J. Associations of screen work with neck and upper extremity symptoms: A systematic review with meta-analysis. Occup. Environ. Med. 2019, 76, 502–509. [Google Scholar] [CrossRef]
- Giannini, F.; Cioni, R.; Mondelli, M.; Padua, R.; Gregori, B.; D’Amico, P.; Padua, L. A new clinical scale of carpal tunnel syndrome: Validation of the measurement and clinical-neurophysiological assessment. Clin. Neurophysiol. 2002, 113, 71–77. [Google Scholar] [CrossRef]
- Wang, W.L.; Buterbaugh, K.; Kadow, T.R.; Goitz, R.J.; Fowler, J.R. A prospective comparison of diagnostic tools for the diagnosis of carpal tunnel syndrome. J. Hand Surg. 2018, 43, 833–836.e2. [Google Scholar] [CrossRef]
- de-la-Llave-Rincon, A.I.; Puentedura, E.J.; Fernandez-de-las-Penas, C. New advances in the mechanisms and etiology of carpal tunnel syndrome. Discov. Med. 2012, 13, 343–348. [Google Scholar]
- Fernández-De-Las-Peñas, C.; De-La-Llave-Rincón, A.I.; Cescon, C.; Barbero, M.; Arias-Buría, J.L.; Falla, D. Influence of clinical, psychological, and psychophysical variables on long-term treatment outcomes in carpal tunnel syndrome: Evidence from a randomized clinical trial. Pain Pract. 2019, 19, 644–655. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Fernández-Muñoz, J.J.; Navarro-Pardo, E.; Da-Silva-Pocinho, R.F.; Ambite-Quesada, S.; Pareja, J.A. Identification of subgroups of women with carpal tunnel syndrome with central sensitization. Pain Med. 2016, 17, 1749–1756. [Google Scholar] [CrossRef]
- Soon, B.; Vicenzino, B.; Schmid, A.B.; Coppieters, M.W. Facilitatory and inhibitory pain mechanisms are altered in patients with carpal tunnel syndrome. PLoS ONE 2017, 12, e0183252. [Google Scholar] [CrossRef]
- Sartorio, F.; Vercelli, S.; Bravini, E.; Zanetta, A.; Bargeri, S.; Pisano, F.; Ferriero, G. Assessment of dexterity and diagnostic accuracy of the Functional Dexterity Test in patients with carpal tunnel syndrome. La Med. Lav. 2018, 109, 31–39. [Google Scholar]
- D’Arcy, C.A.; McGee, S. Does this Patient have carpal tunnel syndrome? JAMA 2000, 283, 3110. [Google Scholar] [CrossRef]
- Trillos, M.-C.; Soto, F.; Briceno-Ayala, L. Upper limb neurodynamic test 1 in patients with clinical diagnosis of carpal tunnel syndrome: A diagnostic accuracy study. J. Hand Ther. 2018, 31, 333–338. [Google Scholar] [CrossRef]
- Erickson, M.; Lawrence, M.; Jansen, C.W.S.; Coker, D.; Amadio, P.; Cleary, C. Hand pain and sensory deficits: Carpal tunnel syndrome. J. Orthop. Sports Phys. Ther. 2019, 49, CPG1–CPG85. [Google Scholar] [CrossRef]
- Huisstede, B.M.; Fridén, J.; Coert, J.H.; Hoogvliet, P. Carpal tunnel syndrome: Hand surgeons, hand therapists, and physical medicine and rehabilitation physicians agree on a multidisciplinary treatment guideline—Results from the European Handguide Study. Arch. Phys. Med. Rehabil. 2014, 95, 2253–2263. [Google Scholar] [CrossRef]
- Ma, H.; Kim, I. The diagnostic assessment of hand elevation test in carpal tunnel syndrome. J. Korean Neurosurg. Soc. 2012, 52, 472–475. [Google Scholar] [CrossRef] [PubMed]
- Durham, C.O.; VanRavenstein, K. It’s all in the wrist. Orthop. Nurs. 2017, 36, 323–327. [Google Scholar] [CrossRef]
- Burton, C.L.; Chesterton, L.S.; Chen, Y.; Van Der Windt, D.A. Clinical course and prognostic factors in conservatively managed carpal tunnel syndrome: A systematic review. Arch. Phys. Med. Rehabil. 2016, 97, 836–852.e1. [Google Scholar] [CrossRef]
- 741/94 L. Professional Profile of the Italian Physiotherapist. Gazzetta Ufficiale. 9 January 1995. Available online: http://www.salute.gov.it/imgs/C_17_normativa_1867_allegato.pdf (accessed on 10 January 2021).
- Alfonso, C.; Jann, S.; Massa, R.; Torreggiani, A. Diagnosis, treatment and follow-up of the carpal tunnel syndrome: A review. Neurol. Sci. 2010, 31, 243–252. [Google Scholar] [CrossRef]
- Villafañe, J.H.; Valdes, K.; O’Brien, V.; Seves, M.; Cantero-Téllez, R.; Berjano, P. Conservative management of thumb carpometacarpal osteoarthritis: An Italian survey of current clinical practice. J. Bodyw. Mov. Ther. 2018, 22, 37–39. [Google Scholar] [CrossRef]
- Stephens, G.; O’Neill, S.; French, H.P.; Fearon, A.; Grimaldi, A.; O’Connor, L.; Woodley, S.; Littlewood, C. A survey of physiotherapy practice (2018) in the United Kingdom for patients with greater trochanteric pain syndrome. Musculoskelet. Sci. Pract. 2019, 40, 10–20. [Google Scholar] [CrossRef]
- Grieve, R.; Palmer, S. Physiotherapy for plantar fasciitis: A UK-wide survey of current practice. Physiotherapy 2017, 103, 193–200. [Google Scholar] [CrossRef]
- MacDermid, J.C.; Wojkowski, S.; Kargus, C.; Marley, M.; Stevenson, E. Hand therapist management of the lateral epicondylosis: A survey of expert opinion and practice patterns. J. Hand Ther. 2010, 23, 18–30. [Google Scholar] [CrossRef]
- Cantero-Tellez, R.; Valdes, K.; Garcia-Orza, S.; Villafane, J. Current practice patterns after carpal tunnel release. A survey of clinical practice trends across the world. Mathews J. Orthop. 2018, 3, 019. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for reporting results of internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Bury, J.; Littlewood, C. Rotator cuff disorders: A survey of current (2016) UK physiotherapy practice. Shoulder Elb. 2017, 10, 52–61. [Google Scholar] [CrossRef]
- Pieters, L.; Voogt, L.; Bury, J.; Littlewood, C.; Feijen, S.; Cavaggion, C.; Struyf, F. Rotator CUFF disorders: A survey of current physiotherapy practice in Belgium and the Netherlands. Musculoskelet. Sci. Pract. 2019, 43, 45–51. [Google Scholar] [CrossRef]
- Brindisino, F.; Matteuzzi, I.; Bury, J.; McCreesh, K.; Littlewood, C. Rotator cuff disorders: A survey of current (2018) Italian physiotherapy practice. Physiother. Pract. Res. 2020, 41, 11–22. [Google Scholar] [CrossRef]
- Fan, W.; Yan, Z. Factors affecting response rates of the web survey: A systematic review. Comput. Hum. Behav. 2010, 26, 132–139. [Google Scholar] [CrossRef]
- Regmi, P.R.; Waithaka, E.; Paudyal, A.; Simkhada, P.; Van Teijlingen, E. Guide to the design and application of online questionnaire surveys. Nepal J. Epidemiol. 2017, 6, 640–644. [Google Scholar] [CrossRef]
- Rossettini, G.; Palese, A.; Geri, T.; Fiorio, M.; Colloca, L.; Testa, M. Physical therapists’ perspectives on using contextual factors in clinical practice: Findings from an Italian national survey. PLoS ONE 2018, 13, e0208159. [Google Scholar] [CrossRef]
- Haberman, S.J. The analysis of residuals in cross-classified tables. Biometrics 1973, 29, 205. [Google Scholar] [CrossRef]
- Beasley, T.M.; Schumacker, R.E. Multiple regression approach to analyzing contingency tables: Post hoc and planned comparison procedures. J. Exp. Educ. 1995, 64, 79–93. [Google Scholar] [CrossRef]
- García-Pérez, M.A.; Núñez-Antón, V. Cellwise residual analysis in two-way contingency tables. Educ. Psychol. Meas. 2003, 63, 825–839. [Google Scholar] [CrossRef]
- Graham, B.; Peljovich, A.E.; Rempel, D.; Rozental, T.D.; Salajegheh, M.K.; Keith, M.W.; Jevsevar, D.S.; Shea, K.G.; Bozic, K.J.; Adams, J.; et al. The American academy of orthopaedic surgeons evidence-based clinical practice guideline on. J. Bone Jt. Surg. 2016, 98, 1750–1754. [Google Scholar] [CrossRef]
- Carpal tunnel syndrome: A summary of clinical practice guideline recommendations—Using the evidence to guide physical therapist practice. J. Orthop. Sports Phys. Ther. 2019, 49, 359–360. [CrossRef] [PubMed]
- Peñas, C.F.-D.-L.; Ortega-Santiago, R.; De La Llave-Rincón, A.I.; Martínez-Perez, A.; Díaz, H.F.-S.; Martínez-Martín, J.; Pareja, J.A.; Cuadrado-Pérez, M.L. Manual physical therapy versus surgery for carpal tunnel syndrome: A randomized parallel-group trial. J. Pain 2015, 16, 1087–1094. [Google Scholar] [CrossRef]
- Shi, Q.; Bobos, P.; Lalone, E.A.; Warren, L.; MacDermid, J.C. Comparison of the short-term and long-term effects of surgery and nonsurgical intervention in treating carpal tunnel syndrome: A systematic review and meta-analysis. HAND 2018, 15, 13–22. [Google Scholar] [CrossRef]
- Rahman Shiri, K.F.-H. Computer use and carpal tunnel syndrome: A meta-analysis. J. Neurol. Sci. 2015, 15, 15–19. [Google Scholar] [CrossRef]
- Mediouni, Z.; De Roquemaurel, A.; Dumontier, C.; Becour, B.; Garrabe, H.; Roquelaure, Y.; Descatha, A. Is carpal tunnel syndrome related to computer exposure at work? A review and meta-analysis. J. Occup. Environ. Med. 2014, 56, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Wipperman, J.; Goerl, K. Carpal tunnel syndrome: Diagnosis and management. Am. Fam. Physician 2016, 94, 993–999. [Google Scholar]
- Burton, C.; Chesterton, L.S.; Davenport, G. Diagnosing and managing carpal tunnel syndrome in primary care. Br. J. Gen. Pract. 2014, 64, 262–263. [Google Scholar] [CrossRef]
- Padua, L.; Coraci, D.; Erra, C.; Pazzaglia, C.; Paolasso, I.; Loreti, C.; Caliandro, P.; Hobson-Webb, L.D. Carpal tunnel syndrome: Clinical features, diagnosis, and management. Lancet Neurol. 2016, 15, 1273–1284. [Google Scholar] [CrossRef]
- Ballestero-Pérez, R.; Plaza-Manzano, G.; Urraca-Gesto, A.; Romo-Romo, F.; Atín-Arratibel, M.D.L.Á.; Pecos-Martín, D.; Gallego-Izquierdo, T.; Romero-Franco, N. Effectiveness of nerve gliding exercises on carpal tunnel syndrome: A systematic review. J. Manip. Physiol. Ther. 2017, 40, 50–59. [Google Scholar] [CrossRef]
- Kim, S.-D. Efficacy of tendon and nerve gliding exercises for carpal tunnel syndrome: A systematic review of randomized controlled trials. J. Phys. Ther. Sci. 2015, 27, 2645–2648. [Google Scholar] [CrossRef]
- Page, M.J.; O’Connor, D.; Pitt, V.; Massy-Westropp, N. Exercise and mobilisation interventions for carpal tunnel syndrome. Cochrane Database Syst. Rev. 2012, 6, CD009899. [Google Scholar] [CrossRef]
- Huisstede, B.M.; Hoogvliet, P.; Franke, T.P.; Randsdorp, M.S.; Koes, B.W. Carpal tunnel syndrome: Effectiveness of physical therapy and electrophysical modalities. An updated systematic review of randomized controlled trials. Arch. Phys. Med. Rehabil. 2018, 99, 1623–1634.e23. [Google Scholar] [CrossRef]
- Nunez, F.; Vranceanu, A.-M.; Ring, D. Determinants of pain in patients with carpal tunnel syndrome. Clin. Orthop. Relat. Res. 2010, 468, 3328–3332. [Google Scholar] [CrossRef]
- Fernández-Muñoz, J.J.; Palacios-Ceña, M.; Cigarán-Méndez, M.; Ortega-Santiago, R.; De-La-Llave-Rincón, A.I.; Salom-Moreno, J.; Fernández-De-Las-Peñas, C. Pain is associated to clinical, psychological, physical, and neurophysiological variables in women with carpal tunnel syndrome. Clin. J. Pain 2016, 32, 122–129. [Google Scholar] [CrossRef]
- Lehn, A.; Bullock-Saxton, J.; Newcombe, P.; Carson, A.; Stone, J. Survey of the perceptions of health practitioners regarding Functional Neurological Disorders in Australia. J. Clin. Neurosci. 2019, 67, 114–123. [Google Scholar] [CrossRef]
- Kozakiewicz, R.T.; Bowyer, B.L. Quantitative testing and thermography in carpal tunnel syndrome. Phys. Med. Rehabil. Clin. N. Am. 1997, 8, 503–511. [Google Scholar] [CrossRef]
- Graham, B. The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J. Bone Jt. Surg. 2008, 90, 2587–2593. [Google Scholar] [CrossRef]
- Lee, C.-H.; Lin, Y.-T.; Wu, C.-T.; Lin, C.-H.; Chen, S.-H.; Hsu, C.-C. Sonoelastography in the diagnosis of carpal tunnel syndrome. Ann. Plast. Surg. 2021. [Google Scholar] [CrossRef]
- Parish, R.; Morgan, C.; Burnett, C.A.; Baker, B.C.; Manning, C.; Sisson, S.K.; Shipp, E.R. Practice patterns in the conservative treatment of carpal tunnel syndrome: Survey results from members of the American Society of Hand Therapy. J. Hand Ther. 2020, 33, 346–353. [Google Scholar] [CrossRef]
- Giovannico, G.; Brindisino, F.; Pappaccogli, M.; Saltalamacchia, A.; Bonetti, F.; Tavarnelli, M.; Mezzetti, M.; Delitto, A. A description of physical therapists knowledge in basic competence examination of musculo-skeletal conditions an Italian national cross-sectional survey. Muscle Ligaments Tendons J. 2020, 10, 686. [Google Scholar] [CrossRef]
- Basson, A.; Olivier, B.; Ellis, R.; Coppieters, M.; Stewart, A.; Mudzi, W. The effectiveness of neural mobilization for neuromusculoskeletal conditions: A systematic review and meta-analysis. J. Orthop. Sports Phys. Ther. 2017, 47, 593–615. [Google Scholar] [CrossRef]
- Lim, Y.H.; Chee, D.Y.; Girdler, S.; Lee, H.C. Median nerve mobilization techniques in the treatment of carpal tunnel syndrome: A systematic review. J. Hand Ther. 2017, 30, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Wolny, T. The use of neurodynamic techniques in the conservative treatment of carpal tunnel syndrome—A critical appraisal of the literature. Ortop. Traumatol. Rehabil. 2017, 19, 427–440. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, P.C.; Muñoz, J.J.F.; Palacios-Ceña, P.M.; Navarro-Pardo, E.; Ambite-Quesada, P.S.; Salom-Moreno, P.J. Direct and indirect effects of function in associated variables such as depression and severity on pain intensity in women with carpal tunnel syndrome. Pain Med. 2015, 16, 2405–2411. [Google Scholar] [CrossRef]
- Leppänen, O.V.; Jokihaara, J.; Jämsen, E.; Karjalainen, T. Survey of hand surgeons’ and therapists’ perceptions of the benefit of common surgical procedures of the hand. J. Plast. Surg. Hand Surg. 2017, 52, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Jamal, A.; Temsah, M.-H.; A Khan, S.; Al-Eyadhy, A.; Koppel, C.; Chiang, M.F. Mobile phone use among medical residents: A cross-sectional multicenter survey in Saudi Arabia. JMIR mHealth uHealth 2016, 4, e61. [Google Scholar] [CrossRef] [PubMed]
- Ball, H.L. Conducting online surveys. J. Hum. Lact. 2018, 35, 413–417. [Google Scholar] [CrossRef] [PubMed]
| Answers (n) | Percentage (%) | Missing (n) | ||
|---|---|---|---|---|
| Q 1-Age | <29 | 231 | 44.85 | 0 |
| 30–39 | 167 | 32.43 | ||
| 40–49 | 66 | 12.82 | ||
| ≥50 | 51 | 9.90 | ||
| Q 2-Gender | Female | 260 | 50.49 | 0 |
| Male | 255 | 49.51 | ||
| Q 3-Years of experience | <5 years | 219 | 42.52 | 0 |
| 5–10 years | 110 | 21.36 | ||
| 11–20 years | 123 | 23.88 | ||
| >20 years | 63 | 12.23 | ||
| Q 4-University degree | Three-year degree | 279 | 54.28 | 1 |
| University Master | 169 | 32.88 | ||
| Master’s degree | 56 | 10.89 | ||
| Doctorate | 3 | 0.58 | ||
| Q 5-Where do you do business | Public body (hospital) | 72 | 14.01 | 1 |
| Private body | 412 | 80.16 | ||
| Wrist/hand specialized body | 15 | 2.92 | ||
| Society | 8 | 1.56 | ||
| University | 7 | 1.36 | ||
| Q 6-Business area | Skeletal muscle | 391 | 76.22 | 2 |
| Geriatric | 49 | 9.55 | ||
| Neurological | 59 | 11.50 | ||
| Other | 14 | 2.73 | ||
| Q 7-Region of origin | Northern Italy | 247 | 47.96 | 0 |
| Southern Italy | 115 | 22.33 | ||
| Center of Italy | 153 | 29.71 | ||
| Q 8-Number of cases per year | 1–5 | 341 | 66.60 | 3 |
| 6–10 | 106 | 20.70 | ||
| 11–15 | 35 | 6.84 | ||
| >15 | 30 | 5.86 |
| Educational Qualifications | ||||
|---|---|---|---|---|
| Correct Answer per Question | Bachelor’s Degree | University Master | Master’s Degree or Doctorate | p Values |
| Q9—CTS is a neurological condition caused by compression of the median nerve due to an increase in pressure within the carpal tunnel | 88.5% (247/508) | 98.2% (166/508) | 93.2% (55/508) | 0.001 * |
| Adjusted residuals | 3.50 | 3.50 | 0.30 | |
| Residual’s p-values (Bonferroni p-values = 0.008) | 0.0004 | 0.0004 | 0.7641 | |
| Q10—CTS is caused by reduction of space within the carpal canal | 87.1% (242/508) | 93.5% (158/508) | 91.5% (54/508) | 0.084 |
| Q11—Patients with CTS are responsibility of the physiotherapist | 63.0% (175/508) | 80.5% (136/508) | 81.4% (48/508) | 0.001 * |
| Adjusted residuals | 4.43 | 3.38 | 1.90 | |
| Residual’s p-values (Bonferroni p-values = 0.0055) | 0.0000 | 0.0007 | 0.0574 | |
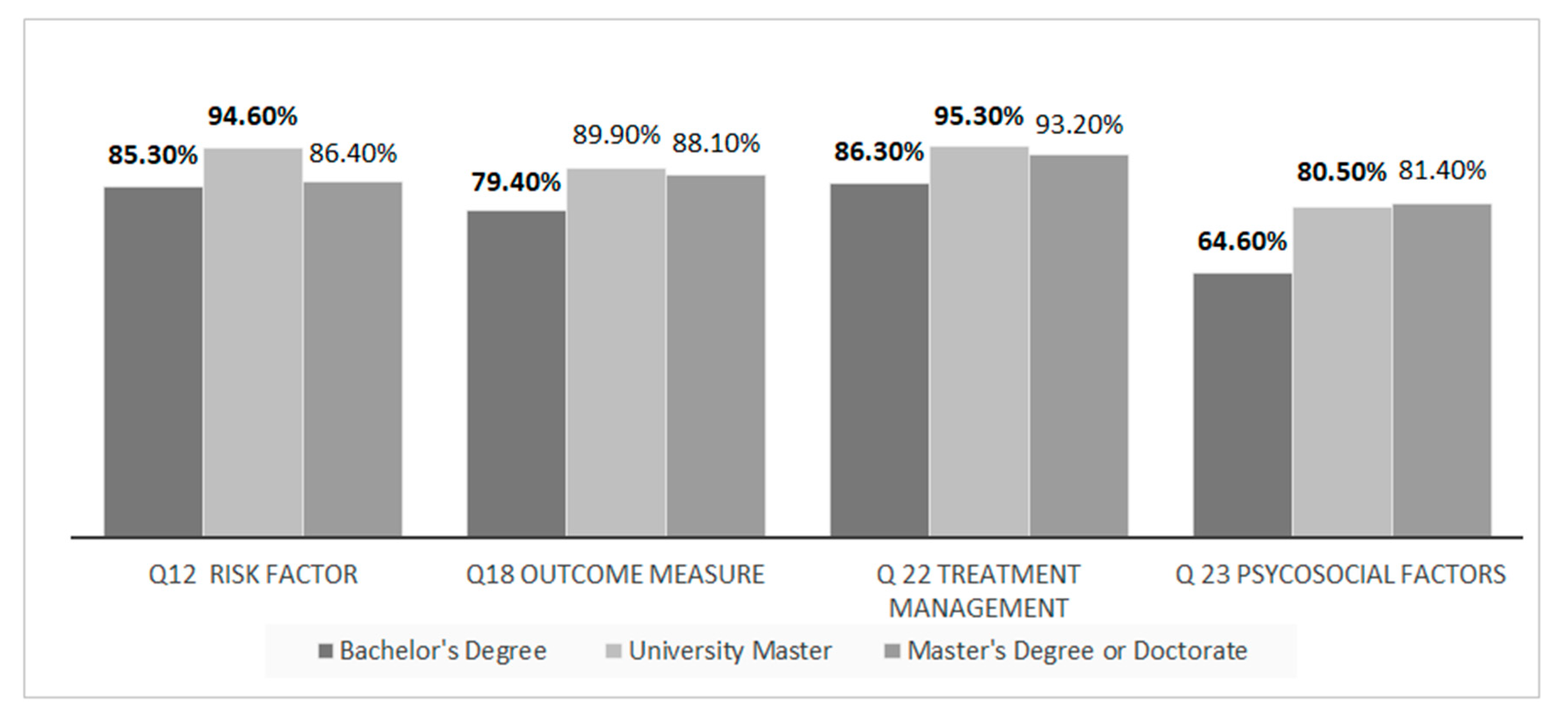
| Q12—Female gender, obesity, diabetes and pregnancy are risk factors for CTS | 85.3% (238/508) | 94.6% (159/508) | 86.4% (51/508) | 0.010 * |
| Adjusted residuals | 2.53 | 3.04 | 0.54 | |
| Residual’s p-values (Bonferroni p-values = 0.0083) | 0.0114 | 0.0023 | 0.58919 | |
| Q13—There’s no association between CTS and computer | 61.9% (172/508) | 52.1% (88/508) | 62.7% (37/508) | 0.088 |
| Q14—Altered sensitivity, tingling and numbness of the first three fingers are the main characters of CTS | 80.3% (224/508) | 83.4% (141/508) | 83.1% (49/508) | 0.843 |
| Q15—In patients with CTS is possible to find hypotrophy of the thenar eminence | 71.2% (198/508) | 81.0% (136/508) | 78% (46/508) | 0.150 |
| Q16—The Semmes-Weinstein Monofilaments are the best tool for the tactile sensitivity examination | 35.3% (97/508) | 77.4% (130/508) | 61% (36/508) | 0.000 * |
| Adjusted residuals | 8.47 | 7.95 | 1.41 | |
| Residual’s p-values (Bonferroni p-values = 0.0041) | 0.0000 | 0.0000 | 0.15853 | |
| Q17—Wrist flexion test (Phalen’s test), nerve percussion test (Tinel’s sign), Functional Dexterity test and two-point discrimination are most used clinical test | 66.3% (181/508) | 71.4% (120/508) | 67.2% (39/508) | 0.068 |
| Q18—Measurement of strength with dynamometer and of sensitivity, manual dexterity, strength and pain and administration of a questionnaire for the evaluation of symptoms and function are the most used outcome evaluation tools | 79.4% (220/508) | 89.9% (151/508) | 88.1% (52/508) | 0.010 * |
| Adjusted residuals | 3.04 | 2.57 | 0.94 | |
| Residual’s p-values (Bonferroni p-values = 0.0055) | 0.00236 | 0.01016 | 0.34721 | |
| Q19—I advice or build an orthotic | 50.9% (142/508) | 57.5% (96/508) | 50.8% (30/508) | 0.073 |
| Q20—I don’t use instrumental therapies in my clinical practice; supporting evidences are weak/moderate | 52.6% (144/508) | 61.5% (104/508) | 61% (36/508) | 0.145 |
| Q21—There is limited evidence on neural and tendon glide techniques and that’s why I don’t use it in my clinical practice | 47.1% (128/508) | 52.7% (88/508) | 57.6% (34/508) | 0.152 |
| Q22—Education, manual therapy, myofascial therapy, therapeutic exercise are most used treatment strategies | 86.3% (240/508) | 95.3% (161/508) | 93.2% (55/508) | 0.006 * |
| Adjusted residuals | 3.15 | 2.75 | 0.85 | |
| Residual’s p-values (Bonferroni p-values = 0.0083) | 0.00163 | 0.00595 | 0.39532 | |
| Q23—I adapt my clinical practice accordingly with the influence of psychosocial factors on the patient outcome | 64.6% (179/508) | 80.5% (136/508) | 81.4% (48/508) | 0.002 * |
| Adjusted residuals | 4.00 | 3.05 | 2.63 | |
| Residual’s p-values (Bonferroni p-values = 0.0055) | 0.00006 | 0.00228 | 0.08543 | |
| Q24—the surgical approach can be a solution in cases of failure of conservative treatment (persistence of symptoms) | 90.6% (252/508) | 96.4% (163/508) | 88.1% (52/508) | 0.037 * |
| Adjusted residuals | 1.53 | 2.48 | 1.27 | |
| Residual’s p-values (Bonferroni p-values = 0.00833) | 0.12601 | 0.01313 | 0.20408 | |
| Place of Professional Activity | ||||||
|---|---|---|---|---|---|---|
| Correct Answer per Question | Hospital | Private Practice | Rehabilitation Clinic | Sport Society | University | p Value |
| Q9—CTS is a neurological condition caused by compression of the median nerve due to an increase in pressure within the carpal tunnel | 93.4% (384/508) | 87.1% (61/50) | 100% (15/508) | 71.4% (5/508) | 100% (4/508) | 0.051 |
| Q10—CTS is caused by reduction of space within the carpal canal | 91.0% (373/508) | 81.4% (57/50) | 100% (15/508) | 85.7% (6/508) | 75.0% (3/508) | 0.069 |
| Q11—Patients with CTS are responsibility of the physiotherapist | 71.0% (292/508) | 72.9% (51/50) | 66.7% (10/508) | 57.1% (4/508) | 75.0% (3/508) | 0.983 |
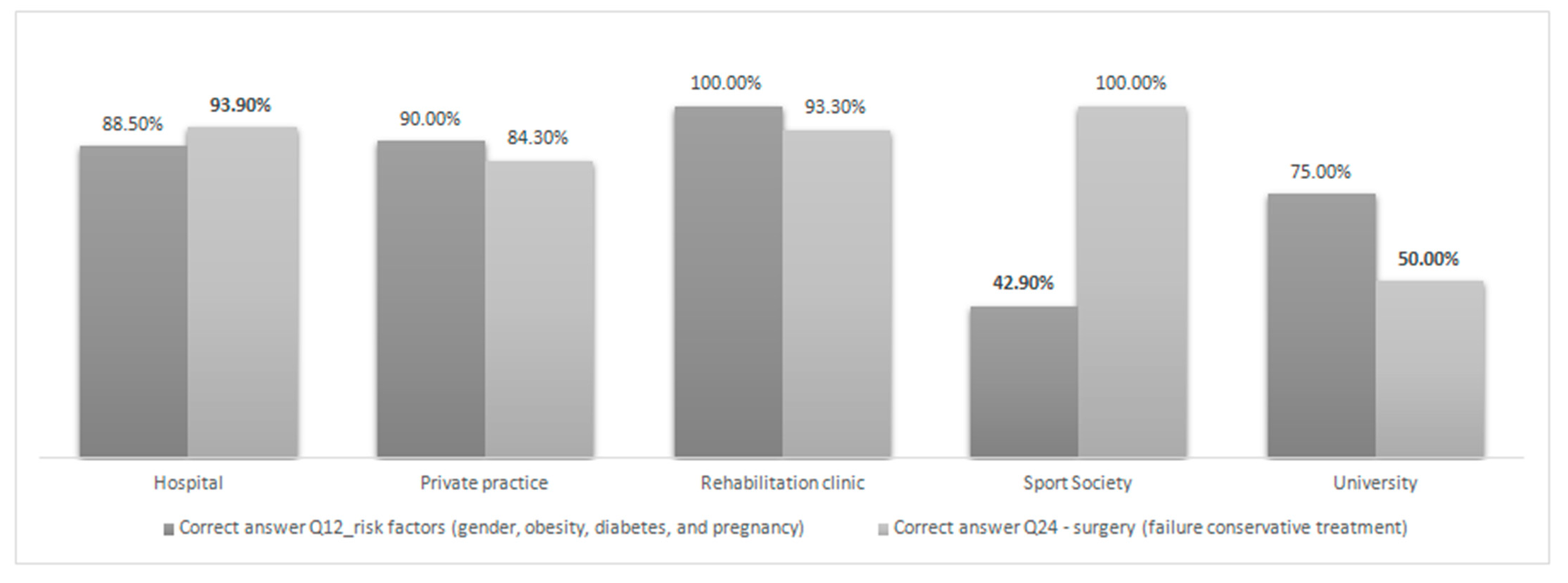
| Q12—Female gender, obesity, diabetes and pregnancy are risk factors for CTS | 88.5% (363/508) | 90.0% (63/50) | 100.0% (15/508) | 42.9% (3/508) | 75% (3/508) | 0.002 * |
| Adjusted residuals | 0.28 | 0.47 | 1.43 | 3.78 | 0.83 | |
| Residual’s p-values (Bonferroni p-value = 0.005) | 0.77947 | 0.63835 | 0.15271 | 0.00015 | 0.40653 | |
| Q13—There’s no association between CTS and computer | 57.6% (236/508) | 67.1% (47/50) | 46.7% (7/508) | 57.1% (4/508) | 100% (4/508) | 0.699 |
| Q14—Altered sensitivity, tingling and numbness of the first three fingers are the main characters of CTS | 83.0% (341/508) | 72.9% (51/50) | 86.7% (13/508) | 71.4% (5/508) | 100% (4/508) | 0.462 |
| Q15—In patients with CTS is possible to find hypotrophy of the thenar eminence | 76.3% (312/508) | 68.6% (48/50) | 86.7% (13/508) | 42.9% (3/508) | 100% (4/508) | 0.596 |
| Q16—The Semmes-Weinstein Monofilaments are the best tool for the tactile sensitivity examination | 52.2% (212/508) | 47.1% (33/50) | 86.7% (3/508) | 57.1% (4/508) | 50% (2/508) | 0.252 |
| Q17—Wrist flexion test (Phalen’s test), nerve percussion test (Tinel’s sign), Functional Dexterity test and two-point discrimination are most used clinical test | 67.2% (272/508) | 67.6% (46/50) | 93.3% (14/508) | 71.4% (5/508) | 75% (3/508) | 0.229 |
| Q18—Measurement of strength with dynamometer and of sensitivity, manual dexterity, strength and pain and administration of a questionnaire for the evaluation of symptoms and function are the most used outcome evaluation tools | 84.1% (345/508) | 82.4% (56/50) | 86.7% (13/508) | 71.4% (5/508) | 100% (4/508) | 0.836 |
| Q19—I advice or build an orthotic | 53.2% (218/508) | 50.7% (35/50) | 80.0% (12/508) | 28.6% (2/508) | 25% (1/508) | 0.123 |
| Q20—I don’t use instrumental therapies in my clinical practice; supporting evidences are weak/moderate | 58.5% (238/508) | 53.6% (37/50) | 33.3% (5/508) | 42.9% (3/508) | 50% (2/508) | 0.612 |
| Q21—There is limited evidence on nerve and tendon glide techniques and that’s why I don’t use it in my clinical practice | 50.2% (203/508) | 50% (34/50) | 53.3% (8/508) | 42.9% (3/508) | 75% (3/508) | 0.900 |
| Q22—Education, manual therapy, myofascial therapy, therapeutic exercise are most used treatment strategies | 90.3% (371/508) | 92.8% (64/50) | 80.0% (12/508) | 100% (7/508) | 75% (3/508) | 0.390 |
| Q23—I adapt my clinical practice accordingly with the influence of psychosocial factors on the patient outcome | 71% (291/508) | 75.4% (52/50) | 73.3% (11/508) | 100% (7/508) | 75% (3/508) | 0.861 |
| Q24—the surgical approach can be a solution in cases of failure of conservative treatment (persistence of symptoms) | 93.9% (385/508) | 84.3% (59/50) | 93.3% (14/508) | 100% (7/508) | 50% (2/508) | 0.001 * |
| Adjusted residuals | 2.81 | 2.71 | 0.15 | 0.77 | 3.18 | |
| Residual’s p-values (Bonferroni p-value = 0.005) | 0.00495 | 0.00672 | 0.88076 | 0.44129 | 0.00147 | |
| Number of CTS Patients/Year | |||||
|---|---|---|---|---|---|
| Correct Answer per Question | 1–5 | 6–10 | 11–15 | >15 | p Value |
| Q9—CTS is a neurological condition caused by compression of the median nerve due to an increase in pressure within the carpal tunnel | 93.4% (312/508) | 91.5% (97/508) | 80.0% (28/508) | 96.7% (29/508) | 0.031 * |
| Adjusted residuals | 1.34 | 0.33 | 2.82 | 0.93 | |
| Residual’s p-values (Bonferroni p-value = 0.0062) | 0.18024 | 0.74139 | 0.00480 | 0.35237 | |
| Q10—CTS is caused by reduction of space within the carpal canal | 90.4% (302/508) | 87.7% (93/508) | 91.4% (32/508) | 86.2% (25/508) | 0.771 |
| Q11—Patients with CTS are responsibility of the physiotherapist | 72.2% (241/508) | 70.8% (75/508) | 60.0% (21/508) | 70% (21/508) | 0.784 |
| Q12—Female gender, obesity, diabetes and pregnancy are risk factors for CTS | 88.6% (295/508) | 84.9% (90/508) | 88.6% (31/508) | 100% (30/508) | 0.155 |
| Q13—There’s no association between CTS and computer | 57.2% (191/508) | 56.2% (59/508) | 68.6% (24/508) | 70% (21/508) | 0.281 |
| Q14—Altered sensitivity, tingling and numbness of the first three fingers are the main characters of CTS | 81.7% (273/508) | 83% (88/508) | 77.1% (27/508) | 83.3% (25/508) | 0.239 |
| Q15—In patients with CTS is possible to find hypotrophy of the thenar eminence | 77.2% (257/508) | 74.3% (78/508) | 57.1% (20/508) | 76.7% (23/508) | 0.308 |
| Q16—The Semmes-Weinstein Monofilaments are the best tool for the tactile sensitivity examination | 53.3% (177/508) | 51.0% (53/508) | 48.6% (17/508) | 53.3% (16/508) | 0.619 |
| Q17—Wrist flexion test (Phalen’s test), nerve percussion test (Tinel’s sign), Functional Dexterity test and two-point discrimination are most used clinical test | 64.4% (212/508) | 71.4% (75/508) | 77.1% (27/508) | 89.7% (26/508) | 0.033 * |
| Adjusted residuals | 2.57 | 0.78 | 1.17 | 2.55 | |
| Residual’s p-values (Bonferroni p-value = 0.0031) | 0.01016 | 0.43539 | 0.24200 | 0.01077 | |
| Q18—Measurement of strength with dynamometer and of sensitivity, manual dexterity, strength and pain and administration of a questionnaire for the evaluation of symptoms and function are the most used outcome evaluation tools | 86.1% (285/508) | 81.1% (86/508) | 68.6% (24/508) | 83.3% (25/508) | 0.120 |
| Q19—I advice or build an orthotic | 55.1% (183/508) | 49.1% (52/508) | 45.7% (16/508) | 60.0% (18/508) | 0.310 |
| Q20—I don’t use instrumental therapies in my clinical practice; supporting evidences are weak/moderate | 60.6% (200/508) | 52.8% (56/508) | 45.7% (16/508) | 40.0% (12/508) | 0.060 |
| Q21—There is limited evidence on neural and tendon glide techniques and that’s why I don’t use it in my clinical practice | 50.2% (165/508) | 50% (52/508) | 48.6% (17/508) | 53.3% (16/508) | 0.612 |
| Q22—Education, manual therapy, myofascial therapy, therapeutic exercise are most used treatment strategies | 92.2% (307/508) | 88.7% (94/508) | 80% (28/508) | 83.3% (25/508) | 0.060 |
| Q23—I adapt my clinical practice accordingly with the influence of psychosocial factors on the patient outcome | 71.1% (236/508) | 74.5% (79/508) | 71.4% (25/508) | 70.0% (21/508) | 0.948 |
| Q24—the surgical approach can be a solution in cases of failure of conservative treatment (persistence of symptoms) | 90.4% (301/508) | 95.3% (101/508) | 97.1% (34/508) | 96.7% (29/508) | 0.174 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scalise, V.; Brindisino, F.; Pellicciari, L.; Minnucci, S.; Bonetti, F. Carpal Tunnel Syndrome: A National Survey to Monitor Knowledge and Operating Methods. Int. J. Environ. Res. Public Health 2021, 18, 1995. https://doi.org/10.3390/ijerph18041995
Scalise V, Brindisino F, Pellicciari L, Minnucci S, Bonetti F. Carpal Tunnel Syndrome: A National Survey to Monitor Knowledge and Operating Methods. International Journal of Environmental Research and Public Health. 2021; 18(4):1995. https://doi.org/10.3390/ijerph18041995
Chicago/Turabian StyleScalise, Valentina, Fabrizio Brindisino, Leonardo Pellicciari, Silvia Minnucci, and Francesca Bonetti. 2021. "Carpal Tunnel Syndrome: A National Survey to Monitor Knowledge and Operating Methods" International Journal of Environmental Research and Public Health 18, no. 4: 1995. https://doi.org/10.3390/ijerph18041995
APA StyleScalise, V., Brindisino, F., Pellicciari, L., Minnucci, S., & Bonetti, F. (2021). Carpal Tunnel Syndrome: A National Survey to Monitor Knowledge and Operating Methods. International Journal of Environmental Research and Public Health, 18(4), 1995. https://doi.org/10.3390/ijerph18041995








