Precautionary Behavior and Depression in Older Adults during the COVID-19 Pandemic: An Online Cross-Sectional Study in Hubei, China
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Procedure
2.3. Measurement
2.3.1. Demographic Information
2.3.2. Covariates
2.3.3. Precautionary Behaviors
2.3.4. Depression
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Characteristics of Depression
3.3. Association of Individual Precautionary Behaviors with Depression
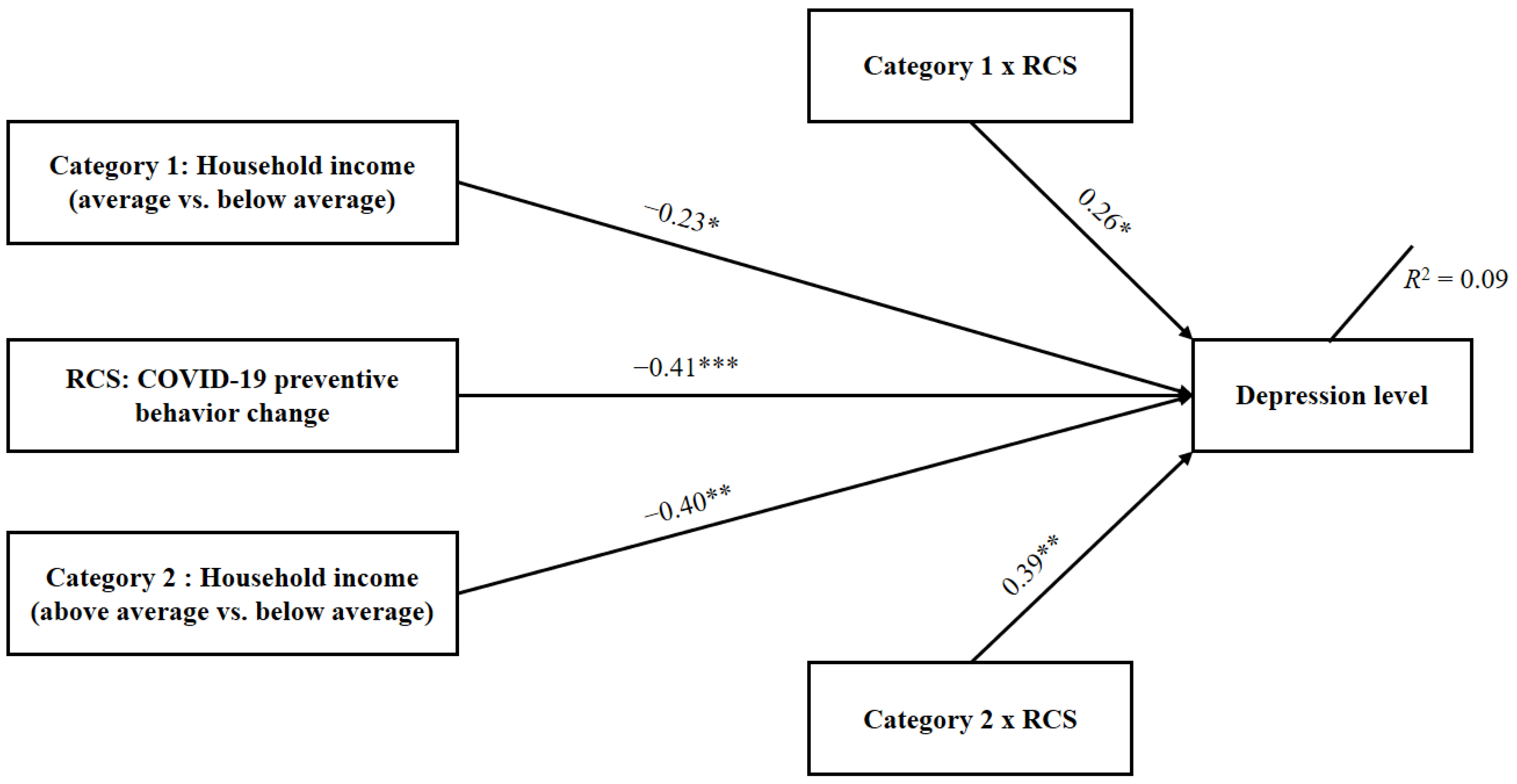
3.4. Moderating Effect of Socioeconomic Status
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 20 August 2020).
- Center for Systems Science and Engineering (CSSE) at Johns Hopkins University, USA. Available online: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 (accessed on 15 October 2020).
- National Health Commission of China. Update on the New Coronavirus Cases. Available online: http://health.people.com.cn/GB/26466/431463/431576/index.html (accessed on 15 October 2020).
- Sachs, J.D.; Horton, R.; Bagenal, J.; Amor, Y.B.; Caman, O.K.; Lafortune, G. The Lancet COVID-19 Commission. Lancet 2020, 396, 454–455. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.Z.; Ahmed, O.; Aibao, Z.; Hanbin, S.; Siyu, L.; Ahmad, A. Epidemic of COVID-19 in China and associated Psychological Problems. Asian J. Psychiatry 2020, 14, 102092. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 15 October 2020).
- Shahid, Z.; Kalayanamitra, R.; McClafferty, B.; Kepko, D.; Ramgobin, D.; Patel, R.; Aggarwal, C.S.; Vunnam, R.; Sahu, N.; Bhatt, D.; et al. COVID-19 and older adults: What we know. J. Am. Geriatr. Soc. 2020, 68, 926–929. [Google Scholar] [CrossRef]
- Khan, K.S.; Mamun, M.A.; Griffiths, M.D.; Ullah, I. The mental health impact of the COVID-19 pandemic across different cohorts. Int. J. Ment. Health Addict. 2020, 9, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Othman, N. Depression, Anxiety, and Stress in the Time of COVID-19 Pandemic in Kurdistan Region, Iraq. Kurd. J. Appl. Res. 2020, 5, 37–44. [Google Scholar] [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 1. [Google Scholar] [CrossRef]
- Guo, Y.; Cheng, C.; Zeng, Y.; Li, Y.; Zhu, M.; Yang, W.; Xu, H.; Li, X.; Leng, J.; Monroe-Wise, A.; et al. Mental health disorders and associated risk factors in quarantined adults during the COVID-19 outbreak in China: Cross-sectional study. J. Med. Internet Res. 2020, 22, e20328. [Google Scholar] [CrossRef]
- Yang, Y.; Li, W.; Zhang, Q.; Zhang, L.; Cheung, T.; Xiang, Y.T. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e19. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19) Advice for the Public. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 30 May 2020).
- Li, S.; Feng, B.; Liao, W.; Pan, W. Internet use, risk awareness, and demographic characteristics associated with engagement in preventive behaviors and testing: Cross-sectional survey on COVID-19 in the United States. J. Med. Internet Res. 2020, 22, e19782. [Google Scholar] [CrossRef]
- Chiu, N.C.; Chi, H.; Tai, Y.L.; Peng, C.C.; Tseng, C.Y.; Chen, C.C.; Tan, B.F.; Lin, C.Y. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: Retrospective national epidemiological surveillance study. J. Med. Internet Res. 2020, 22, e21257. [Google Scholar] [CrossRef] [PubMed]
- Stickley, A.; Matsubayashi, T.; Sueki, H.; Ueda, M. COVID-19 preventive behaviours among people with anxiety and depressive symptoms: Findings from Japan. Public Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Luo, Y.; He, P. Hypertension, socioeconomic status and depressive symptoms in Chinese middle-aged and older adults: Findings from the China health and retirement longitudinal study. J. Affect. Disord. 2019, 252, 237–244. [Google Scholar] [CrossRef]
- Niu, Z.; Wang, T.; Hu, P.; Mei, J.; Tang, Z. Chinese Public’s Engagement in Preventive and Intervening Health Behaviors During the Early Breakout of COVID-19: Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e19995. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Mundó, J.; Leonardi, M.; Chatterji, S.; Tobiasz-Adamczyk, B.; Koskinen, S.; Haro, J.M. The association between socioeconomic status and depression among older adults in Finland, Poland and Spain: A comparative cross-sectional study of distinct measures and pathways. J. Affect. Disord. 2018, 241, 311–318. [Google Scholar] [CrossRef]
- Flesia, L.; Monaro, M.; Mazza, C.; Fietta, V.; Colicino, E.; Segatto, B.; Roma, P. Predicting perceived stress related to the Covid-19 outbreak through stable psychological traits and machine learning models. J. Clin. Med. 2020, 9, 3350. [Google Scholar] [CrossRef]
- Adamson, M.M.; Phillips, A.; Seenivasan, S.; Martinez, J.; Grewal, H.; Kang, X.; Coetzee, J.; Luttenbacher, I.; Jester, A.; Harris, O.A.; et al. International prevalence and correlates of psychological stress during the global CoViD-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9248. [Google Scholar] [CrossRef]
- Yoo, K.B.; Park, E.C.; Jang, S.Y.; Kwon, J.A.; Kim, S.J.; Cho, K.H.; Park, S. Association between employment status change and depression in Korean adults. BMJ Open 2016, 6. [Google Scholar] [CrossRef] [PubMed]
- Segel-Karpas, D.; Ayalon, L.; Lachman, M.E. Loneliness and depressive symptoms: The moderating role of the transition into retirement. Aging Ment. Health 2018, 22, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, P.; Paswan, B. Lifestyle Behaviours and Mental Health Outcomes of Elderly: Modification of Socio-Economic and Physical Health Effects. Ageing Int. 2020, 1–35. [Google Scholar] [CrossRef]
- Mezuk, B.; Rafferty, J.A.; Kershaw, K.N.; Hudson, D.; Abdou, C.M.; Lee, H.; Jackson, J.S. Reconsidering the role of social disadvantage in physical and mental health: Stressful life events, health behaviors, race, and depression. Am. J. Epidemiol. 2010, 172, 1238–1249. [Google Scholar] [CrossRef] [PubMed]
- Jacka, F.N.; Cherbuin, N.; Anstey, K.J.; Butterworth, P. Dietary patterns and depressive symptoms over time: Examining the relationships with socioeconomic position, health behaviours and cardiovascular risk. PLoS ONE. 2014, 9, e87657. [Google Scholar] [CrossRef] [PubMed]
- Fiske, A.; Wetherell, J.L.; Gatz, M. Depression in older adults. Ann. Rev. Clinical. Psychol. 2009, 5, 363–389. [Google Scholar] [CrossRef] [PubMed]
- Rasche, P.; Wille, M.; Bröhl, C.; Theis, S.; Schäfer, K.; Knobe, M.; Mertens, A. Prevalence of health app use among older adults in Germany: National survey. JMIR mHealth uHealth 2018, 6, e26. [Google Scholar] [CrossRef]
- Ko, G.T.; Tang, J.; Chan, J.C.; Sung, R.; Wu, M.M.; Wai, H.P.; Chen, R. Lower BMI cut-off value to define obesity in Hong Kong Chinese: An analysis based on body fat assessment by bioelectrical impedance. Br. J. Nutr. 2001, 85, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Steiner, P.M.; Cook, T.D.; Shadish, W.R.; Clark, M.H. The importance of covariate selection in controlling for selection bias in observational studies. Psychol. Methods 2010, 15, 250. [Google Scholar] [CrossRef]
- Park, J.I.; Park, T.W.; Yang, J.C.; Chung, S.K. Factors associated with depression among elderly Koreans: The role of chronic illness, subjective health status, and cognitive impairment. Psychogeriatrics 2016, 16, 62–69. [Google Scholar] [CrossRef]
- Rankin, S.H.; Galbraith, M.E.; Johnson, S. Reliability and validity data for a Chinese translation of the Center for Epidemiological Studies-Depression. Psychol. Rep. 1993, 73 (Suppl. 3), 1291–1298. [Google Scholar] [CrossRef]
- Duan, Y.P.; Liang, W.; Guo, L.; Wienert, J.; Si, G.Y.; Lippke, S. Evaluation of a web-based intervention for multiple health behavior changes in patients with coronary heart disease in home-based rehabilitation: Pilot randomized controlled trial. J. Med. Internet Res. 2018, 20, e12052. [Google Scholar] [CrossRef]
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Castro-Schilo, L.; Grimm, K.J. Using residualized change versus difference scores for longitudinal research. J. Soc. Pers. Relatsh. 2018, 35, 32–58. [Google Scholar] [CrossRef]
- Miller, K.J.; Mesagno, C.; McLaren, S.; Grace, F.; Yates, M.; Gomez, R. Exercise, mood, self-efficacy, and social support as predictors of depressive symptoms in older adults: Direct and interaction effects. Front. Psychol. 2019, 10, 2145. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Kim, S.; Zhang, H. Changes in depressive symptoms among older adults with multiple chronic conditions: Role of positive and negative social support. Int. J. Environ. Res. Public Health 2017, 14, 16. [Google Scholar] [CrossRef]
- Barnett, A.; Zhang, C.J.; Johnston, J.M.; Cerin, E. Relationships between the neighborhood environment and depression in older adults: A systematic review and meta-analysis. Int. Psychogeriatr. 2018, 30, 1153–1176. [Google Scholar] [CrossRef]
- Liang, W.; Duan, Y.P.; Shang, B.R.; Wang, Y.P.; Hu, C.; Lippke, S. A web-based lifestyle intervention program for Chinese college students: Study protocol and baseline characteristics of a randomized placebo-controlled trial. BMC Public Health 2019, 19, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Keeter, S.; McGeeney, K.; Igielnik, R.; Mercer, A.; Mathiowetz, N. From telephone to the web: The challenge of mode of interview effects in public opinion polls. Pew Research Center. Available online: http://www.aapor.org/AAPOR_Main/media/AnnualMeetingProceedings/2015/I2-1-Keeter.pdf (accessed on 13 May 2015).

| n (%) | |
|---|---|
| Age (years), mean (SD): 67.55 (6.60) | |
| 60–69 | 354 (68.6) |
| 70–79 | 128 (24.8) |
| 80 and above | 34 (6.6) |
| Gender | |
| Male | 217 (42.1) |
| Female | 299 (57.9) |
| Marital status | |
| Single | 14 (2.7) |
| Married | 432 (83.7) |
| Divorced or widowed | 70 (13.6) |
| Living situation | |
| Alone | 48 (9.3) |
| With spouse/partners/Children | 468 (90.7) |
| Medical history of chronic diseases | |
| Yes | 262 (50.8) |
| No | 254 (49.2) |
| Education level | |
| Primary school or below | 45 (8.7) |
| Middle or high school | 231 (44.8) |
| College or above | 240 (46.5) |
| Occupational status | |
| Unemployed | 22 (4.3) |
| Pensioner or retired | 478 (92.6) |
| Part-time or full-time employment | 16 (3.1) |
| Household income | |
| Below average | 113 (21.9) |
| Average | 299 (57.9) |
| Above average | 104 (20.2) |
| BMI (kg/m2), mean (SD): 23.06 (2.67) | |
| <18.5 | 19 (3.7) |
| 18.5 ≤ BMI < 23 | 228 (44.2) |
| 23 ≤ BMI < 26 | 206 (39.9) |
| ≥26 | 63 (12.2) |
| Subjective health status | |
| Bad | 48 (9.3) |
| Satisfactory | 196 (38.0) |
| Excellent | 272 (52.7) |
| Infected cases of acquaintances | |
| Yes | 50 (9.7) |
| No | 466 (90.3) |
| Depression, mean (SD): 7.34 (5.23) | |
| No depressive symptom | 357 (69.2) |
| Have depressive symptoms | 159 (30.8) |
| Precautionary behaviors | |
| Before the outbreak of COVID-19, mean (SD): 3.12 (0.67) | |
| During the outbreak of COVID-19, mean (SD): 3.61 (0.40) | |
| Factors | Depression Mean (SD) | Significance |
|---|---|---|
| Age span | F2, 513 = 1.78, p = 0.17 | |
| 60–69 | 7.06 (5.04) | |
| 70–79 | 7.88 (5.45) | |
| 80 and above | 8.29 (6.08) | |
| Gender | t514 = −0.06, p = 0.95 | |
| Male | 7.33 (5.43) | |
| Female | 7.35 (5.09) | |
| Marital status | F2, 513 = 7.87, p < 0.001 | |
| Single | 9.07 (5.80) | |
| Married | 6.96 (5.07) | |
| Divorced or widowed | 9.57 (5.56) | |
| Living situation | t514 = 2.11, p = 0.035 | |
| Alone | 8.85 (5.34) | |
| With spouse/partners/Children | 7.19 (5.20) | |
| Medical history of chronic diseases | t514 = 1.66, p = 0.10 | |
| Yes | 7.72 (5.26) | |
| No | 6.96 (5.17) | |
| Education level | F2, 513 = 7.32, p = 0.001 | |
| Primary school or below | 10.07 (5.94) | |
| Middle or high school | 7.12 (5.02) | |
| College or above | 6.86 (5.13) | |
| Occupational status | F2, 513 = 1.24, p = 0.29 | |
| Unemployed | 9.01 (6.18) | |
| Pensioner or retired | 7.29 (5.22) | |
| Part-time or full-time employment | 6.75 (3.73) | |
| Household income | F2, 513 = 9.09, p < 0.001 | |
| Below average | 9.06 (5.72) | |
| Average | 7.08 (5.07) | |
| Above average | 6.24 (4.70) | |
| Body mass index (BMI) intervals | 23.06 (2.67) | F3, 512 = 0.62, p = 0.60 |
| BMI < 18.5 kg/m2 | 6.37 (4.70) | |
| 18.5 kg/m2 ≤ BMI < 23 kg/m2 | 7.62 (5.60) | |
| 23 kg/m2 ≤ BMI < 26 kg/m2 | 7.08 (4.88) | |
| BMI ≥ 26 kg/m2 | 7.48 (5.10) | |
| Subjective health status | F2, 513 = 17.25, p < 0.001 | |
| Bad | 10.44 (6.01) | |
| Satisfactory | 8.09 (5.32) | |
| Excellent | 6.26 (4.69) | |
| Infected cases of acquaintances | t514 = 2.95, p = 0.003 | |
| Yes | 9.40 (6.18) | |
| No | 7.12 (5.07) |
| Predictors of Depression | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | |
| Marital status | |||||||||
| Single (reference group) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Married | −0.08 | −3.08, 0.80 | 0.25 | −0.05 | −2.60, 1.18 | 0.46 | −0.03 | −2.28, 1.45 | 0.66 |
| Divorces or widowed | 0.04 | −1.41, 2.77 | 0.53 | 0.05 | −1.24, 2.84 | 0.44 | 0.07 | −1.01, 3.00 | 0.33 |
| Living situation | |||||||||
| Alone (reference group) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| With spouse/partners/children | <0.01 | −0.58, 0.65 | 0.91 | −0.01 | −0.66, 0.53 | 0.83 | 0.01 | −0.50, 0.68 | 0.76 |
| Education level | |||||||||
| Primary school or below (reference group) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Middle or high school | −0.18 | −3.06, −0.65 | 0.003 | −0.17 | −2.95, −0.60 | 0.003 | −00.16 | −2.81, −0.49 | 0.005 |
| College or above | −0.19 | −3.18, −0.75 | 0.002 | −0.19 | −3.17, −0.79 | 0.001 | −0.16 | −2.80, −0.45 | 0.007 |
| Household income | |||||||||
| Below average (reference group) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Average | −0.15 | −3.28, −1.27 | <0.001 | −0.11 | −1.98, −0.40 | 0.003 | −0.08 | −1.66, −0.10 | 0.027 |
| Above average | −0.18 | −3.28, −1.27 | <0.001 | −0.13 | −2.65, −0.66 | 0.001 | −0.10 | −2.33, −0.36 | 0.008 |
| Subjective health status | |||||||||
| Bad (reference group) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Satisfactory | N/A | N/A | N/A | −0.16 | −2.87, −0.63 | 0.002 | −0.16 | −2.85, −0.64 | 0.002 |
| Excellent | N/A | N/A | N/A | −0.33 | −4.53, −2.33 | <0.001 | −0.33 | −4.55, −2.39 | <0.001 |
| Infected cases of acquaintances | |||||||||
| Yes (reference group) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| No | N/A | N/A | N/A | −0.10 | −1.44, −0.40 | 0.001 | −0.11 | −1.47, −0.45 | <0.001 |
| Precautionary behaviors a | N/A | N/A | N/A | N/A | N/A | N/A | −0.18 | −1.24, −0.62 | <0.001 |
| R2 | 0.07, p < 0.001 | 0.12, p < 0.001 | 0.15, p < 0.001 | ||||||
| ΔR2 | N/A | 0.05, p < 0.001 | 0.03, p < 0.001 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liang, W.; Duan, Y.; Shang, B.; Hu, C.; Baker, J.S.; Lin, Z.; He, J.; Wang, Y. Precautionary Behavior and Depression in Older Adults during the COVID-19 Pandemic: An Online Cross-Sectional Study in Hubei, China. Int. J. Environ. Res. Public Health 2021, 18, 1853. https://doi.org/10.3390/ijerph18041853
Liang W, Duan Y, Shang B, Hu C, Baker JS, Lin Z, He J, Wang Y. Precautionary Behavior and Depression in Older Adults during the COVID-19 Pandemic: An Online Cross-Sectional Study in Hubei, China. International Journal of Environmental Research and Public Health. 2021; 18(4):1853. https://doi.org/10.3390/ijerph18041853
Chicago/Turabian StyleLiang, Wei, Yanping Duan, Borui Shang, Chun Hu, Julien Steven Baker, Zhihua Lin, Jiali He, and Yanping Wang. 2021. "Precautionary Behavior and Depression in Older Adults during the COVID-19 Pandemic: An Online Cross-Sectional Study in Hubei, China" International Journal of Environmental Research and Public Health 18, no. 4: 1853. https://doi.org/10.3390/ijerph18041853
APA StyleLiang, W., Duan, Y., Shang, B., Hu, C., Baker, J. S., Lin, Z., He, J., & Wang, Y. (2021). Precautionary Behavior and Depression in Older Adults during the COVID-19 Pandemic: An Online Cross-Sectional Study in Hubei, China. International Journal of Environmental Research and Public Health, 18(4), 1853. https://doi.org/10.3390/ijerph18041853









