Mortality Risk Factors for Individuals Experiencing Homelessness in Catalonia (Spain): A 10-Year Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Population and Sample
2.3. Procedure
2.4. Sample Information
3. Results
4. Discussion
4.1. Main Mortality Figures
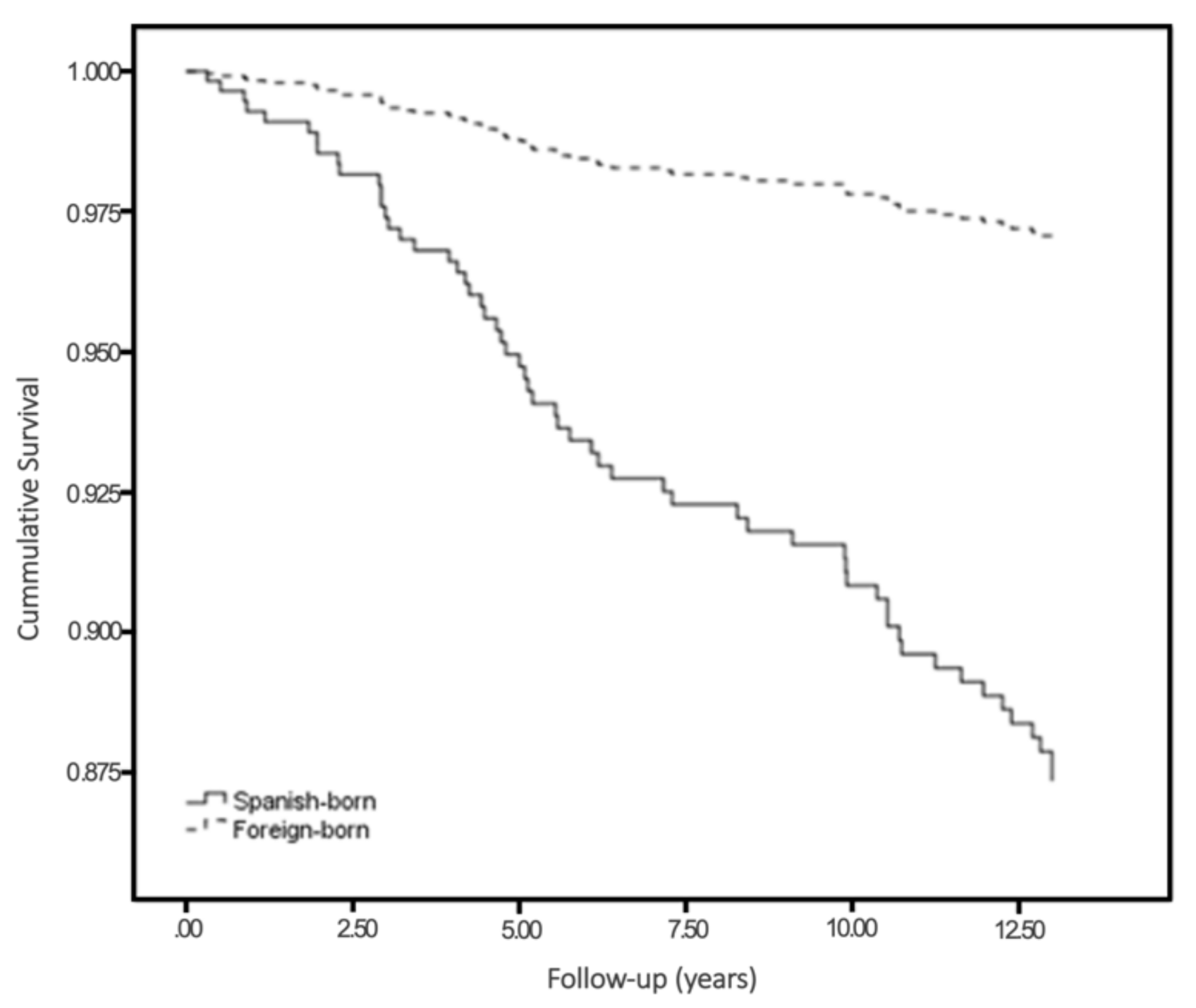
4.2. The Effect of Origin
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Termorshuizen, F.; Van Bergen, A.P.; Smit, R.B.; Smeets, H.; Van Ameijden, E.J. Mortality and psychiatric disorders among public mental health care clients in Utrecht: A register-based cohort study. Int. J. Soc. Psychiatry 2014, 60, 426–435. [Google Scholar] [CrossRef] [PubMed]
- Nusselder, W.J.; Slockers, M.; Krol, L.; Slockers, C.; Looman, C.; Van Beeck, E. Mortality and Life Expectancy in Homeless Men and Women in Rotterdam: 2001–2010. PLoS ONE 2013, 8, e73979. [Google Scholar] [CrossRef]
- Nilsson, S.F.; Hjorthøj, C.R.; Erlangsen, A.; Nordentoft, M. Psychiatric disorders and mortality among people in homeless shelters in Denmark: A nationwide register-based cohort study. Lancet 2011, 377, 2205–2214. [Google Scholar] [CrossRef]
- Aldridge, R.W.; Story, A.; Hwang, S.W.; Nordentoft, M.; Luchenski, S.A.; Hartwell, G.; Tweed, E.J.; Lewer, D.; Katikireddi, S.V.; Hayward, A.C. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: A systematic review and meta-analysis. Lancet 2018, 391, 241–250. [Google Scholar] [CrossRef]
- Fazel, S.; Geddes, J.R.; Kushel, M. The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet 2014, 384, 1529–1540. [Google Scholar] [CrossRef]
- Hwang, S.W. Mortality Among Men Using Homeless Shelters in Toronto, Ontario. JAMA 2000, 283, 2152–2157. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.W.; Lebow, J.M.; Bierer, M.F.; O’Connell, J.J.; Orav, E.J.; Brennan, T.A. Risk factors for death in homeless adults in Boston. Arch. Intern. Med. 1998, 158, 1454–1460. [Google Scholar] [CrossRef]
- Vuillermoz, C.; Aouba, A.; Grout, L.; Vandentorren, S.; Tassin, F.; Moreno-Betancur, M.; Jougla, É.; Rey, G. Mortality among homeless people in France, 2008–2010. Eur. J. Public Heal. 2016, 26, 1028–1033. [Google Scholar] [CrossRef]
- Nordentoft, M.; Wandall-Holm, N. 10 year follow up study of mortality among users of hostels for homeless people in Co-penhagen. BMJ 2003, 327, 81. [Google Scholar] [CrossRef]
- Morrison, D.S. Homelessness as an independent risk factor for mortality: Results from a retrospective cohort study. Int. J. Epidemiol. 2009, 38, 877–883. [Google Scholar] [CrossRef]
- Hwang, S.W.; Wilkins, R.; Tjepkema, M.; O’Campo, P.J.; Dunn, J.R. Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. BMJ 2009, 339, b4036. [Google Scholar] [CrossRef] [PubMed]
- FEANTSA and Foundation Abbé Pierre. Fourth Overview of Housing Exclusion in Europe 2019; FEANTSA: Brussels, Belgium, 2019. [Google Scholar]
- Schoibl, H.; Snopek, J.; Ripka, S.; Sillanpäa, V.; Boccadoro, N.; Teller, N.; Feher, B.; O’Sullivan, E.; Wygnanska, J.; Knutagard, M.; et al. The Costs of Homelessness in Europe—An Assessment of the Curret Evidence Base; EOH: Brussels, Belgium, 2013. [Google Scholar]
- van Leerdam, J. Analysing Costs and Benefits of Homelessness Policies in the Netherlands: Lessons for Europe. Eur. J. Homelessness 2013, 7, 157–181. [Google Scholar]
- Agence Nouvelle des Solidarités Actives. Le Logement D’abord, et Après—Bilan et Propositions pour la Généralisation du Logement d’abord en France; Agence Nouvelle des Solidarités Actives: Paris, France, 2017. [Google Scholar]
- Fazel, S.; Khosla, V.; Doll, H.; Geddes, J. The prevalence of mental disorders among the homeless in western countries: Sys-tematic review and meta-regression analysis. PLoS Med. 2008, 5, e225. [Google Scholar] [CrossRef] [PubMed]
- Borhade, A.; Dey, S. Do migrants have a mortality advantage? Lancet 2018, 392, 2517–2518. [Google Scholar] [CrossRef]
- Dhadda, A.; Greene, G. ‘The Healthy Migrant Effect’ for Mental Health in England: Propensity-score Matched Analysis Using the EMPIRIC Survey. J. Immigr. Minor. Health 2018, 20, 799–808. [Google Scholar] [CrossRef] [PubMed]
- Laporte, A.; Vandentorren, S.; Détrez, M.-A.; Douay, C.; Le Strat, Y.; Le Méner, E. Prevalence of mental disorders and ad-dictions among homeless people in the Greater Paris Area, France. Int. J. Environ. Res. Public Health 2018, 15, 241. [Google Scholar] [CrossRef]
- Busch-Geertsema, V.; Culhane, D.; Fitzpatrick, S. Developing a global framework for conceptualising and measuring home-lessness. Habitat Int. 2016, 55, 124–132. [Google Scholar] [CrossRef]
- INE. Encuesta sobre las Personas sin Hogar; Instituto Nacional de Estadística: Madrid, Spain, 2012. [Google Scholar]
- FEANTSA. ETHOS—European Typology of Homelessness and Housing Exclusion, Brussels. 2005. Available online: http://www.feantsa.org/download/en-16822651433655843804.pdf (accessed on 1 April 2005).
- Calvo, F.; Carbonell, X.; Badia, M. Homelessness and Unemployment During the Economic Recession: The Case of the City of Girona. Eur. Sci. J. ESJ 2018, 14, 1857–7881. [Google Scholar] [CrossRef][Green Version]
- Urquia, M.L.; Gagnon, A.J. Glossary: Migration and health. J. Epidemiol. Community Health 2011, 65, 467–472. [Google Scholar] [CrossRef]
- Gimeno-Feliu, L.A.; Calderón-Larrañaga, A.; Diaz, E.; Laguna-Berna, C.; Poblador-Plou, B.; Coscollar-Santaliestra, C.; Prados-Torres, A. The definition of immigrant status matters: Impact of nationality, country of origin, and length of stay in host country on mortality estimates. BMC Public Health 2019, 19, 247. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Publishing: Arlinghton, VA, USA; Washington, DC, USA, 2013. [Google Scholar]
- Beijer, U.; Andréasson, A.; Agren, G.; Fugelstad, A. Mortality, mental disorders and addiction: A 5-year follow-up of 82 homeless men in Stockholm. Nord J. Psychiatry 2007, 61, 363–368. [Google Scholar] [CrossRef]
- Guijarro, M.; Peláez, Ó. La longevidad globalizada: Un análisis de la esperanza de vida en España (1900–2050). Scr. Nova 2007, 12, 256–280. [Google Scholar]
- Idescat. Statistical Yearbook of Catalonia. Unemployment Rate. By Sex. Provinces. 2017. Available online: https://www.idescat.cat/pub/?id=aec&n=318&lang=en (accessed on 12 May 2018).
- CatSalut. Epidemiological Data; CatSalut: Girona, Spain, 2017. [Google Scholar]
- Campbell, D.J.; Campbell, R.B.; Ziegler, C.; McBrien, K.A.; Hwang, S.W.; Booth, G.L. Interventions for improved diabetes control and self-management among those experiencing homelessness: Protocol for a mixed methods scoping review. Syst. Rev. 2019, 8, 1–6. [Google Scholar] [CrossRef]
- Honkaniemi, H.; Bacchus-Hertzman, J.; Fritzell, J.; Rostila, M. Mortality by country of birth in the Nordic countries—A systematic review of the literature. BMC Public Health 2017, 17, 511. [Google Scholar] [CrossRef]
- Rostila, M.; Fritzell, J. Mortality Differentials by Immigrant Groups in Sweden: The Contribution of Socioeconomic Position. Am. J. Public Health 2014, 104, 686–695. [Google Scholar] [CrossRef] [PubMed]
- Gadd, M.; Johansson, S.-E.; Sundquist, J.; Wändell, P. The Trend of Cardiovascular Disease in Immigrants in Sweden. Eur. J. Epidemiol. 2005, 20, 755–760. [Google Scholar] [CrossRef] [PubMed]
- Hedlund, E.; Lange, A.; Hammar, N. Acute myocardial infarction incidence in immigrants to Sweden. Country of birth, time since immigration, and time trends over 20 years. Eur. J. Epidemiol. 2007, 22, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Chiu, S.; Redelmeier, D.A.; Tolomiczenko, G.; Kiss, A.; Hwang, S.W. The health of homeless immigrants. J. Epidemiol. Community Health 2009, 63, 943–948. [Google Scholar] [CrossRef] [PubMed]
- Domnich, A.; Panatto, D.; Gasparini, R.; Amicizia, D. The “healthy immigrant” effect: Does it exist in Europe today? Ital. J. Public Health 2012, 9, e7532. [Google Scholar]
- Castañeda, E.; Smith, B.; Vetter, E. Hispanic health disparities and housing: Comparing measured and self-reported health metrics among housed and homeless Latin individuals. J. Migr. Health 2020, 1–2, 100008. [Google Scholar] [CrossRef]
- Gee, E.M.T.; Kobayashi, K.M.; Prus, S.G. Examining the Healthy Immigrant Effect in Mid- to Later Life: Findings from the Canadian Community Health Survey. Can. J. Aging 2004, 23, S55–S63. [Google Scholar] [CrossRef]
- Vang, Z.M.; Sigouin, J.; Flenon, A.; Gagnon, A. Are immigrants healthier than native-born Canadians? A systematic review of the healthy immigrant effect in Canada. Ethn. Health 2017, 22, 209–241. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (n = 475) |
|---|---|
| Age, mean (SD) | 39.4 (12.1) |
| Days homeless, median (IQR) | 119 (570) |
| Deceased, n (%) * | 60 (12.8) |
| Country of birth, n (%) | |
| Catalonia | 91 (19.2) |
| Spain ** | 142 (29.9) |
| Morocco | 134 (28.2) |
| Others | 108 (22.7) |
| Infectious diseases, n (%) | |
| AIDS | 31 (6.5) |
| HCVI | 65 (13.7) |
| TBI | 22 (4.6) |
| Chronic diseases, n (%) | |
| HBP | 73 (15.4) |
| DM | 48 (10.1) |
| COPD | 38 (8.0) |
| CVD | 72 (8.4) |
| Mental disorders, n (%) | |
| Depressive disorder | 49 (10.3) |
| Psychotic disorder | 52 (10.9) |
| Personality disorder | 29 (6.1) |
| Substance abuse, n (%) | |
| Alcohol | 148 (31.2) |
| Cocaine | 59 (12.4) |
| Opioids | 62 (13.1) |
| Cannabis | 34 (7.2) |
| Characteristics | Global (n = 475) | Spanish-Born (n = 242) | Foreign-Born (n = 246) |
|---|---|---|---|
| Age, mean (SD) | 39.4 (12.1) | 43.8 (12.5) | 34.9 (9.3) |
| Days homelessness, median (IQR) | 119 (570) | 722.6 (1147.1) | 454.9 (897.5) |
| Deceased *, n (%) | 60 (12.8) | 52 (22.9) | 8 (3.3) |
| Infectious diseases, n (%) | |||
| AIDS | 31 (6.5) | 21 (9.2) | 10 (4.1) |
| HCVI | 65 (13.7) | 51 (22.3) | 14 (5.7) |
| TBI | 22 (4.6) | 12 (5.2) | 10 (4.1) |
| Chronic diseases, n (%) | |||
| HBP | 73 (15.4) | 51 (22.3) | 22 (8.9) |
| DM | 48 (10.1) | 28 (12.2) | 20 (8.1) |
| COPD | 38 (8.0) | 30 (13.1) | 8 (3.3) |
| CVD | 72 (8.4) | 29 (12.7) | 11 (4.5) |
| Mental disorders, n (%) | |||
| Depressive disorder | 49 (10.3) | 32 (14.0) | 17 (6.9) |
| Psychotic disorder | 52 (10.9) | 13 (5.7) | 12 (4.9) |
| Personality disorder | 29 (6.1) | 23 (10.0) | 6 (2.4) |
| Substance abuse, n (%) | |||
| Alcohol | 148 (31.2) | 90 (39.3) | 56 (22.8) |
| Cocaine | 59 (12.4) | 35 (15.3) | 16 (6.5) |
| Opioids | 62 (13.1) | 46 (20.1) | 16 (6.5) |
| Cannabis | 34 (7.2) | 14 (6.1) | 13 (5.3) |
| Characteristics | Living (n = 409) | Deceased (n = 60) |
|---|---|---|
| Age, mean (SD) | 38.0 (11.1) | 49.1 (14.3) |
| Days homeless, median (IQR) | 113 (484) | 225 (795) |
| Origin, n (%) | ||
| Spanish-born | 175 (77.1) | 52 (22.9) |
| Foreign-born | 234 (96.7) | 8 (3.3) |
| Infectious diseases, n (%) | ||
| AIDS | 22 (5.4) | 5 (8.3) |
| HCVI | 47 (11.5) | 14 (23.3) |
| TBI | 13 (3.2) | 5 (8.3) |
| Chronic diseases, n (%) | ||
| HBP | 53 (13.0) | 16 (26.7) |
| DM | 28 (6.8) | 16 (26.7) |
| COPD | 24 (5.9) | 10 (16.7) |
| CVD | 21 (5.1) | 15 (25.0) |
| Mental disorders, n (%) | ||
| Depressive disorder | 39 (9.5) | 10 (16.7) |
| Psychotic disorder | 45 (11.0) | 7 (11.7) |
| Personality disorder | 20 (4.9) | 9 (15.0) |
| Substance abuse, n (%) | ||
| Alcohol | 117 (28.6) | 30 (50.0) |
| Cocaine | 51 (12.5) | 7 (11.7) |
| Opioids | 50 (12.2) | 10 (16.7) |
| Cannabis | 32 (7.8) | 2 (3.3) |
| Model 1 * | Model 2 * | Model 3 * | Model 4 * | ||||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | ||||
| AIDS | 1.16 (0.42–3.17) | HBP | 0.85 (0.43–1.69) | Depressive disorder | 1.40 (0.67–2.93) | Alcohol | 2.18 (1.26–3.77) |
| HCVI | 1.7 (0.87–3.56) | DM | 2.80 (1.50–5.25) | Psychotic disorder | 0.89 (0.39–3.95) | Cocaine | 0.90 (0.36–2.28) |
| TBI | 1.83 (0.70–4.74) | COPD | 1.11 (0.51–2.38) | Personality disorder | 1.83 (0.84–3.91) | Opioids | 1.80 (0.80–4.05) |
| CVD | 1.79 (0.86–3.71) | Cannabis | 0.39 (0.08–1.75) | ||||
| HR (95% CI) | |
|---|---|
| Age | 1.06 (1.03–1.08) |
| Gender | |
| Male | 1 |
| Female | 0.81 (0.37–1.77) |
| Days homeless | 1.0 (0.99–1.01) |
| Country of origin | |
| Foreign-born | 1 |
| Spanish-born | 4.34 (1.89–10.0) |
| Infectious diseases | 1.61 (1.09–2.39) |
| DM2 | 2.93 (1.62–5.30) |
| Mental disorders | 1.16 (0.86–1.56) |
| Alcohol abuse | 1.92 (1.12–3.29) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calvo, F.; Turró-Garriga, O.; Fàbregas, C.; Alfranca, R.; Calvet, A.; Salvans, M.; Giralt, C.; Castillejos, S.; Rived-Ocaña, M.; Calvo, P.; et al. Mortality Risk Factors for Individuals Experiencing Homelessness in Catalonia (Spain): A 10-Year Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 1762. https://doi.org/10.3390/ijerph18041762
Calvo F, Turró-Garriga O, Fàbregas C, Alfranca R, Calvet A, Salvans M, Giralt C, Castillejos S, Rived-Ocaña M, Calvo P, et al. Mortality Risk Factors for Individuals Experiencing Homelessness in Catalonia (Spain): A 10-Year Retrospective Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(4):1762. https://doi.org/10.3390/ijerph18041762
Chicago/Turabian StyleCalvo, Fran, Oriol Turró-Garriga, Carles Fàbregas, Rebeca Alfranca, Anna Calvet, Mercè Salvans, Cristina Giralt, Sandra Castillejos, Mercè Rived-Ocaña, Paula Calvo, and et al. 2021. "Mortality Risk Factors for Individuals Experiencing Homelessness in Catalonia (Spain): A 10-Year Retrospective Cohort Study" International Journal of Environmental Research and Public Health 18, no. 4: 1762. https://doi.org/10.3390/ijerph18041762
APA StyleCalvo, F., Turró-Garriga, O., Fàbregas, C., Alfranca, R., Calvet, A., Salvans, M., Giralt, C., Castillejos, S., Rived-Ocaña, M., Calvo, P., Castillo, P., Garre-Olmo, J., & Carbonell, X. (2021). Mortality Risk Factors for Individuals Experiencing Homelessness in Catalonia (Spain): A 10-Year Retrospective Cohort Study. International Journal of Environmental Research and Public Health, 18(4), 1762. https://doi.org/10.3390/ijerph18041762






