Bleeding Complications in Anticoagulated and/or Antiplatelet-Treated Patients at the Dental Office: A Retrospective Study
Abstract
1. Introduction
2. Material and Methods.
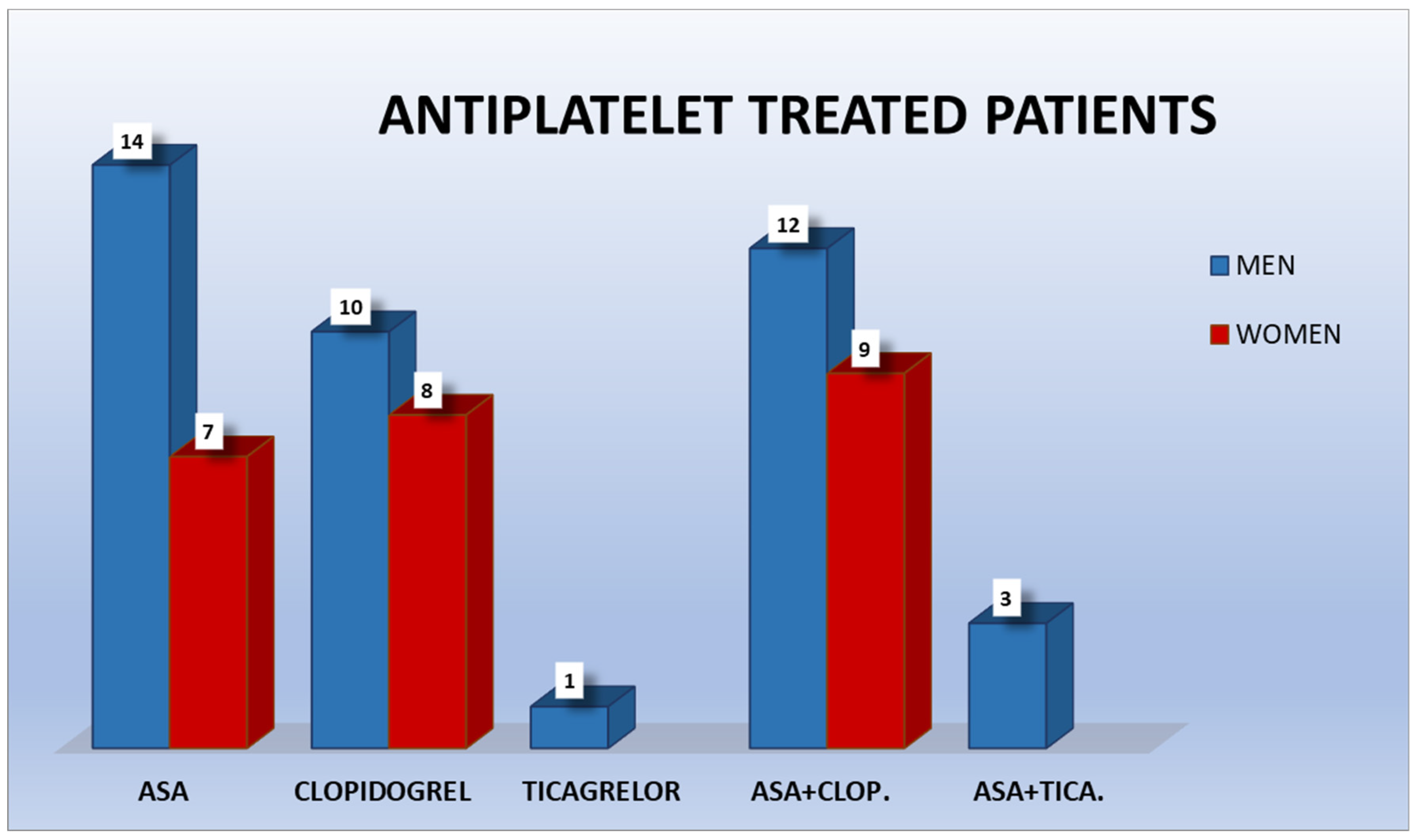
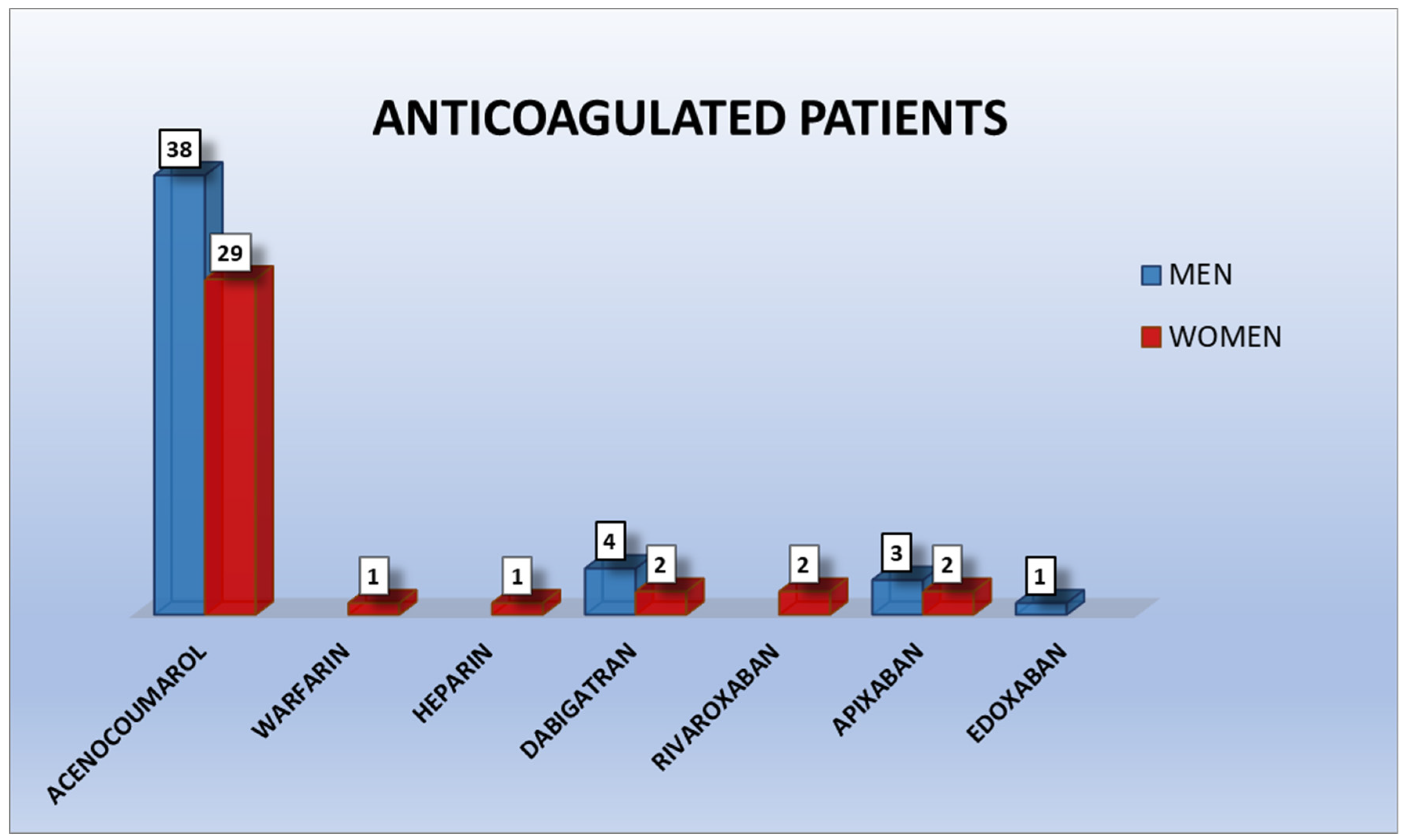
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martínez-López, F.; Oñate-Sánchez, R.; Arrieta-Blanco, J.J.; Oñate-Cabrerizo, D.; Cabrerizo-Merino, M.C. Clinical diseases with thrombotic risk and their pharmacologycal treatment: How they change the therapeutic attitude in dental treatments. Med. Oral Patol. Oral Cir. Bucal 2013, 18, 888–895. [Google Scholar] [CrossRef]
- Precht, C.; Demirel, Y.; Assaf, A.T.; Pinnschmidt, H.O.; Knipfer, C.; Hanken, H.; Friedrich, R.E.; Wikner, J. Perioperative Management in Patients with Undergoing Direct Oral Anticoagulant Therapy in Oral Surgery—A Multicentric Questionnaire Survey. In Vivo 2019, 33, 855–862. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Fiorillo, L.; Monte, I.P.; De Stefano, R.; Laino, L.; Crimi, S.; Bianchi, A.; Herford, A.S.; Biondi, A.; Cicciù, M. Advances in Antiplatelet Therapy for Dentofacial Surgery Patients: Focus on Past and Present Strategies. Materials 2019, 12, 1524. [Google Scholar] [CrossRef]
- Fernández-Tresguerres, F.G.; Sirvent, A.A.; Denche, J.T.; Fernández, I. Nuevos anticoagulantes orales: Repercusión odontológica. Cient. Dent. 2016, 13, 139–148. [Google Scholar]
- Serrano-Sanchez, V.; Ripolles-de Ramon, J.; Collado-Yurrita, L.; Vaello-Checa, I.; Colmenero-Ruiz, C.; Helm, A.; Ciudad-Cabañas, M.J.; Serrano-Cuenca, V. New horizons in anticoagulation: Direct oral anticoagulants and their implications in oral surgery. Med. Oral Patol. Oral Cir. Bucal 2017, 22, e601–e608. [Google Scholar]
- Manfredi, M.; Dave, B.; Percudani, D.; Christoforou, J.; Karasneh, J.; Diz Dios, P.; Glick, M.; Kumar, N.; Lockhart, P.B.; Patton, L.L. World workshop on oral medicine VII: Direct anticoagulant agents management for invasive oral procedures: A systematic review and meta-analysis. Oral Dis. 2019, 25, 157–173. [Google Scholar] [CrossRef]
- Lanau, N.; Mareque, J.; Giner, L.; Zabalza, M. Direct oral anticoagulants and its implications in dentistry. A review of literature. J. Clin. Exp. Dent. 2017, 9, e1346–e1354. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.Y.; Ho, P. Direct Oral Anticoagulants in Dental Patients Including the Frail Elderly Population. Dent. J. 2016, 4, 7. [Google Scholar] [CrossRef] [PubMed]
- Iwabuchi, H.; Imai, Y.; Asanami, S.; Shirakawa, M.; Yamane, G.Y.; Ogiuchi, H.; Kurashina, K.; Miyata, M.; Nakao, H.; Imai, H. Evaluation of postextraction bleeding incidence to compare patients receiving and not receiving warfarin therapy: A cross-sectional, multicentre, observational study. BMJ Open 2014, 4, e005777. [Google Scholar] [CrossRef]
- Schulman, S.; Crowther, M.A. How I treat anticoagulants in 2012: New and old anticoagulants, and when and how to switch. Blood 2012, 119, 3016–3023. [Google Scholar] [CrossRef]
- Singh Gill, A.; Morrissey, H.; Rahman, A. A Systematic Review and Meta-Analysis Evaluating Antibiotic Prophylaxis in Dental Implants and Extraction Procedures. Medicina 2018, 54, 95. [Google Scholar] [CrossRef]
- Cervino, G.; Cicciù, M.; Biondi, A.; Bocchieri, S.; Herford, A.S.; Laino, L.; Fiorillo, L. Antibiotic Prophylaxis on Third Molar Extraction: Systematic Review of Recent Data. Antibiotics 2019, 8, 53. [Google Scholar] [CrossRef]
- Giudice, A.; Esposito, M.; Bennardo, F.; Brancaccio, Y.; Buti, J.; Fortunato, L. Dental extractions for patients on oral antiplatelet: A within-person randomised controlled trial comparing haemostatic plugs, advanced-platelet-rich fibrin (A-PRF+) plugs, leukocyte-and platelet-rich fibrin (L-PRF) plugs and suturing alone. Int. J. Oral Implantol. 2019, 12, 77–87. [Google Scholar]
- Berton, F.; Costantinides, F.; Rizzo, R.; Franco, A.; Contarin, J.; Stacchi, C.; Maglione, M.; Visintini, E.; Di Lenarda, A.; Di Lenarda, R. Should we fear direct oral anticoagulants more than vitamin K antagonists in simple single tooth extraction? A prospective comparative study. Clin. Oral Investig. 2019, 23, 3183–3192. [Google Scholar] [CrossRef]
- Tang, M.; Yu, C.; Hu, P.; Wang, C.; Sheng, J.; Ma, S. Risk factors for bleeding after dental extractions in patients over 60 years of age who are taking antiplatelet drugs. Br. J. Oral Maxillofac. Surg. 2018, 56, 854–858. [Google Scholar] [CrossRef]
- Lu, S.Y.; Lin, L.H.; Hsue, S.S. Management of dental extractions in patients on warfarin and antiplatelet therapy. J. Formos. Med. Assoc. 2018, 117, 979–986. [Google Scholar] [CrossRef] [PubMed]
- Cabbar, F.; Turer Cabbar, A.; Cosansu, K.; Cekirdekci, E.I. Effects of Direct Oral Anticoagulants on Quality of Life during Periprocedural Management for Dental Extractions. J. Oral Maxillofac. Surg. 2019, 77, 904–911. [Google Scholar] [CrossRef] [PubMed]
- Ehrhard, S.; Burkhard, J.P.; Exadaktylos, A.K.; Sauter, T.C. Severe Enoral Bleeding with a Direct Oral Anticoagulant after Tooth Extraction and Heparin Bridging Treatment. Case Rep. Emerg. Med. 2019, 2019, 6208604. [Google Scholar] [CrossRef] [PubMed]
- Ockerman, A.; Vanhaverbeke, M.; Miclotte, I.; Belmans, A.; Vanassche, T.; Politis, C.; Jacobs, R.; Verhamme, P. Tranexamic acid to reduce bleeding after dental extraction in patients treated with non-vitamin K oral anticoagulants: Design and rationale of the EXTRACT-NOAC trial. Br. J. Oral Maxillofac. Surg. 2019, 57, 1107–1112. [Google Scholar] [CrossRef]
- Brennan, Y.; Gu, Y.; Schifter, M.; Crowther, H.; Favaloro, E.J.; Curnow, J. Dental extractions on direct oral anticoagulants vs. warfarin: The DENTST study. Res. Pract. Thromb. Haemost. 2020, 4, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Cocero, N.; Basso, M.; Grosso, S.; Carossa, S. Direct Oral Anticoagulants (DOACs) and Medical Comorbidities in Patients Needing Dental Extractions: Management of the Risk of Bleeding. J. Oral Maxillofac. Surg. 2019, 77, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Andrade, M.V.; Andrade, L.A.; Bispo, A.F.; Freitas, L.D.; Andrade, M.Q.; Feitosa, G.S.; Feitosa-Filho, G.S. Evaluation of the Bleeding Intensity of Patients Anticoagulated with Warfarin or Dabigatran Undergoing Dental Procedures. Arq. Bras. Cardiol. 2018, 111, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Yagyuu, T.; Kawakami, M.; Ueyama, Y.; Imada, M.; Kurihara, M.; Matsusue, Y.; Imai, Y.; Yamamoto, K.; Kirita, T. Risks of postextraction bleeding after receiving direct oral anticoagulants or warfarin: A retrospective cohort study. BMJ Open 2017, 7, e015952. [Google Scholar] [CrossRef]
- Gupta, R.; Dugal, A.; Sane, V.D.; Hiwarkar, S.; Khandelwal, S.; Iyengar, A. Effect of Low-Dose Aspirin on Bleeding Following Exodontia: A Prospective Clinical Study. J. Maxillofac. Oral Surg. 2018, 17, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, I.; Younis, M.; Ahmed Shah, A. Extraction in Patients on Oral Anticoagulant Therapy with and without Stopping the Drug: A Comparative Study. J. Maxillofac. Oral Surg. 2019, 18, 555–558. [Google Scholar] [CrossRef]
- Mauprivez, C.; Khonsari, R.H.; Razouk, O.; Goudot, P.; Lesclous, P.; Descroix, V. Management of dental extraction in patients undergoing anticoagulant oral direct treatment: A pilot study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, 146–155. [Google Scholar] [CrossRef]
- Kwak, E.-J.; Nam, S.; Park, K.; Kim, S.; Huh, J.; Park, W. Bleeding related to dental treatment in patients taking novel oral anticoagulants (NOACs): A retrospective study. Clin. Oral Investig. 2019, 23, 477–484. [Google Scholar] [CrossRef]
- Lababidi, E.; Breik, O.; Savage, J.; Engelbrecht, H.; Kumar, R.; Crossley, C.W. Assessing an oral surgery specific protocol for patients on direct oral anticoagulants: A retrospective controlled cohort study. Int. J. Oral Maxillofac. Surg. 2018, 47, 940–946. [Google Scholar] [CrossRef]
- de Almeida Barros Mourão, C.F.; Calasans-Maia, M.D.; de Mello Machado, R.C.; de Brito Resende, R.F.; Alves, G.G. The use of platelet-rich fibrin as a hemostatic material in oral soft tissues. Oral Maxillofac. Surg. 2018, 22, 329–333. [Google Scholar] [CrossRef]
- Doganay, O.; Atalay, B.; Karadag, E.; Aga, U.; Tugrul, M. Bleeding frequency of patients taking ticagrelor, aspirin, clopidogrel, and dual antiplatelet therapy after tooth extraction and minor oral surgery. J. Am. Dent. Assoc. 2018, 149, 132–138. [Google Scholar] [CrossRef]
- Hamzah, N.A.; Graf, H.L.; Meyer, A.L.; Dieterlen, M.T.; Hemprich, A. Haemostasis in oral surgical procedures involving patients with a ventricular assist device. Int. J. Oral Maxillofac. Surg. 2020, 49, 1355–1359. [Google Scholar] [CrossRef] [PubMed]
- Yamada, S.I.; Hasegawa, T.; Soutome, S.; Yoshimura, H.; Miyakoshi, M.; Ueda, N.; Okamoto, K.; Hishida, S.; Rokutanda, S.; Nakahara, H.; et al. Prevalence of and risk factors for postoperative hemorrhage after lower third molar extraction on warfarin therapy: A multicenter retrospective study in Japan. Odontology 2020, 108, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Sannino, G.; Capparé, P.; Montemezzi, P.; Alfieri, O.; Pantaleo, G.; Gherlone, E. Postoperative bleeding in patients taking oral anticoagulation therapy after ‘All-on-four’ rehabilitation: A case-control study. Int. J. Oral Implantol. 2020, 13, 77–87. [Google Scholar]
- Zirk, M.; Zinser, M.; Buller, J.; Bilinsky, V.; Dreiseidler, T.; Zöller, J.E.; Kreppel, M. Supportive topical tranexamic acid application for hemostasis in oral bleeding events—Retrospective cohort study of 542 patients. J. Craniomaxillofac. Surg. 2018, 46, 932–936. [Google Scholar] [CrossRef]
- Febbo, A.; Cheng, A.; Stein, B.; Goss, A.; Sambrook, P. Postoperative Bleeding Following Dental Extractions in Patients Anticoagulated with Warfarin. J. Oral Maxillofac. Surg. 2016, 74, 1518–1523. [Google Scholar] [CrossRef] [PubMed]

| Treatment of infection or inflammation using antibiotic coverage and/or chlorhexidine mouthwash before the tooth extraction [1]. |
| Atraumatic surgery, bone regularization, and removal of the granulation tissue [1]. |
| Dental suturing [1]. |
| Alveolus irrigation using tranexamic acid [1]. |
| Biting an tranexamic acid-dampened gauze [1] for 30 min [9]. |
| Monitoring International Normalized Ratio (INR) a maximum of 72 h prior to dental extraction in Vitamin K antagonists (VKAs) anticoagulated patients [1]. |
| Grade | Clinical Correlation |
|---|---|
| 0 | No bleeding. |
| 1 | Adequate hemostasis, blood clot is present. |
| 2.1 | Hemostasis was reached after the compression of the wound for more than 30 min. |
| 2.2 | Blood oozing in regions where hemostasis was achieved the next day or the same day of the extraction using compression. |
| 3 | Hemostasis was achieved by procedures that differ from compression. |
| Gender | Antiplatelet Therapy | Anticoagulant Therapy | Both | Total |
|---|---|---|---|---|
| Women | 24 | 37 | 0 | 61 |
| Men | 39 | 46 | 1 | 86 |
| Total | 63 | 83 | 1 | 147 |
| Women (n = 61) | Men (n = 86) | Total (n = 147) | ||||
|---|---|---|---|---|---|---|
| Age | SD | SD | SD | |||
| 41–50 | 0 | 0 | 46 | 0 | 46 | 0 |
| 51–60 | 53.400 | 1.673 | 56.444 | 3.395 | 55.357 | 3.201 |
| 61–70 | 65.846 | 3.648 | 65.115 | 2.930 | 65.359 | 3.158 |
| 71–80 | 74.600 | 2.720 | 74.667 | 2.443 | 74.641 | 2.518 |
| 81–90 | 84.375 | 2.337 | 84.500 | 2.844 | 84.437 | 2.576 |
| 91–100 | 91.500 | 1 | 91.500 | 0.707 | 91.500 | 0.837 |
| Test | Value | Degrees of Freedom | Bilateral Asymtotic Significance |
|---|---|---|---|
| Pearson’s chi-square | 11.944 | 2 | 0.003 |
| Likelihood ratio | 7.323 | 2 | 0.026 |
| Linear-by-linear association | 2.276 | 1 | 0.131 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Moreno, E.; Martínez-López, F.; Rodríguez-Lozano, F.J.; Oñate-Sánchez, R.E. Bleeding Complications in Anticoagulated and/or Antiplatelet-Treated Patients at the Dental Office: A Retrospective Study. Int. J. Environ. Res. Public Health 2021, 18, 1609. https://doi.org/10.3390/ijerph18041609
Martínez-Moreno E, Martínez-López F, Rodríguez-Lozano FJ, Oñate-Sánchez RE. Bleeding Complications in Anticoagulated and/or Antiplatelet-Treated Patients at the Dental Office: A Retrospective Study. International Journal of Environmental Research and Public Health. 2021; 18(4):1609. https://doi.org/10.3390/ijerph18041609
Chicago/Turabian StyleMartínez-Moreno, Esther, Federico Martínez-López, Francisco Javier Rodríguez-Lozano, and Ricardo Elías Oñate-Sánchez. 2021. "Bleeding Complications in Anticoagulated and/or Antiplatelet-Treated Patients at the Dental Office: A Retrospective Study" International Journal of Environmental Research and Public Health 18, no. 4: 1609. https://doi.org/10.3390/ijerph18041609
APA StyleMartínez-Moreno, E., Martínez-López, F., Rodríguez-Lozano, F. J., & Oñate-Sánchez, R. E. (2021). Bleeding Complications in Anticoagulated and/or Antiplatelet-Treated Patients at the Dental Office: A Retrospective Study. International Journal of Environmental Research and Public Health, 18(4), 1609. https://doi.org/10.3390/ijerph18041609







