Trends of Testicular Cancer Mortality-to-Incidence Ratios in Relation to Health Expenditure: An Ecological Study of 54 Countries
Abstract
1. Introduction
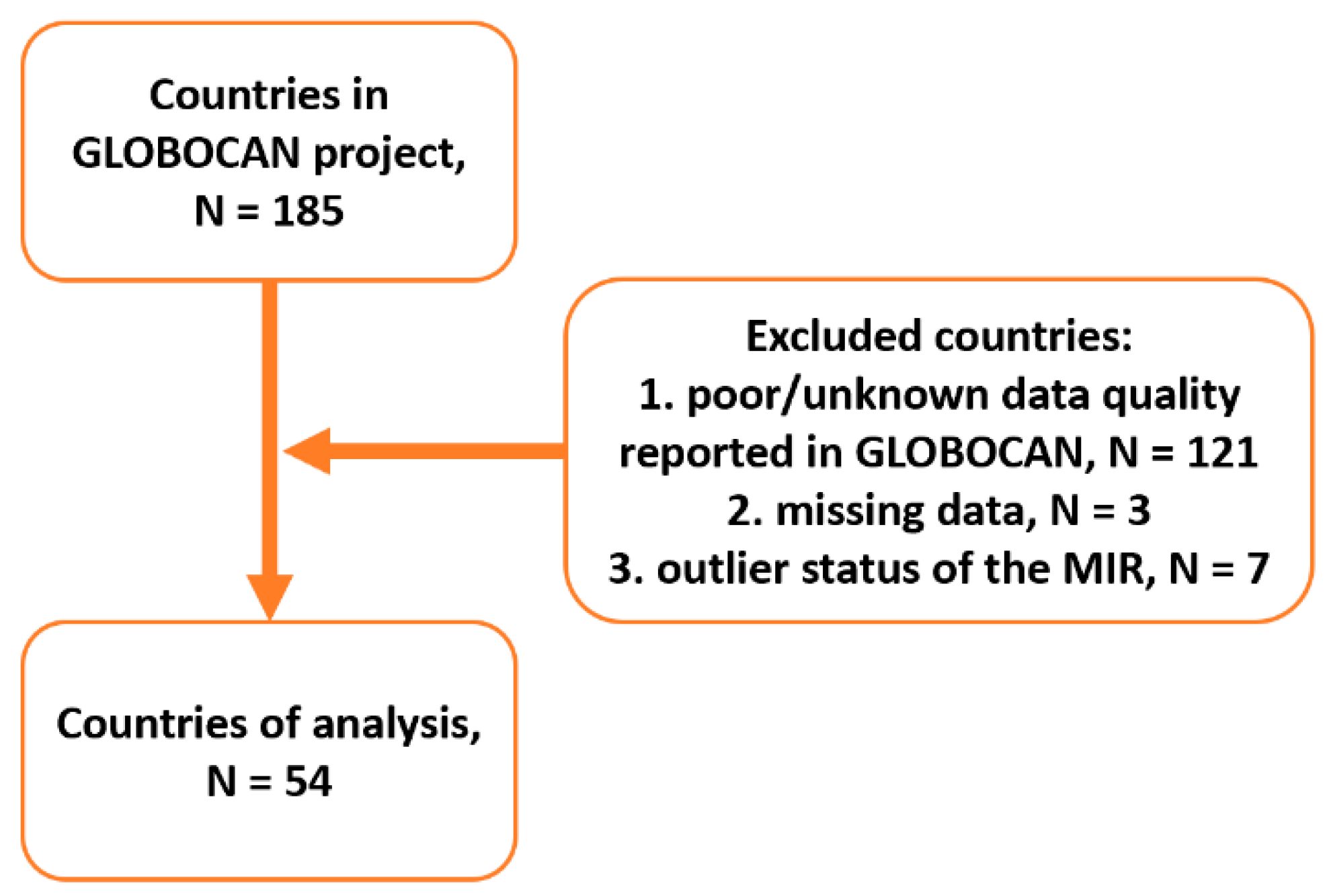
2. Materials and Methods
3. Results
3.1. Incidence, Mortality, and MIR of Testicular Cancer in Five Continents
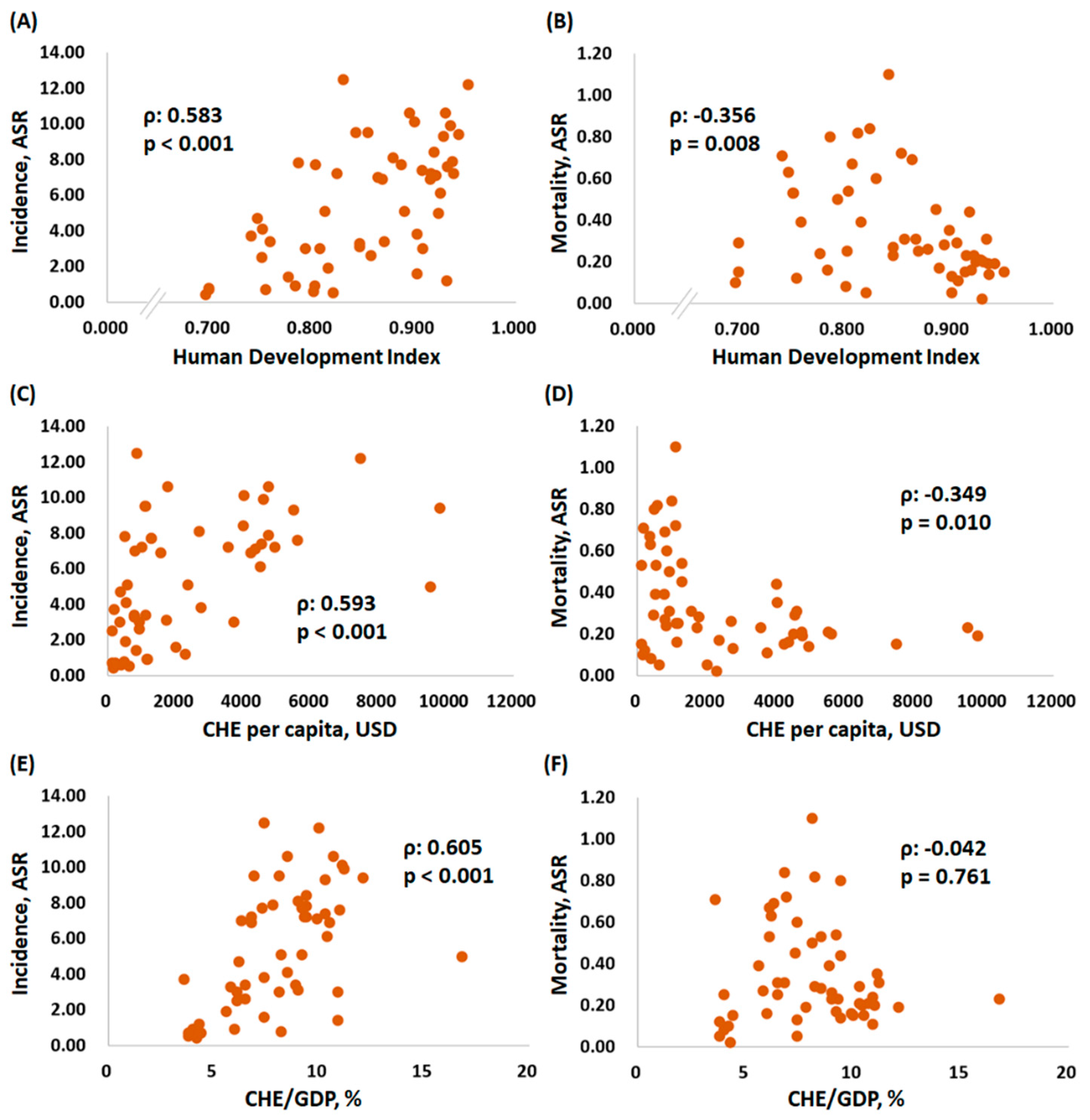
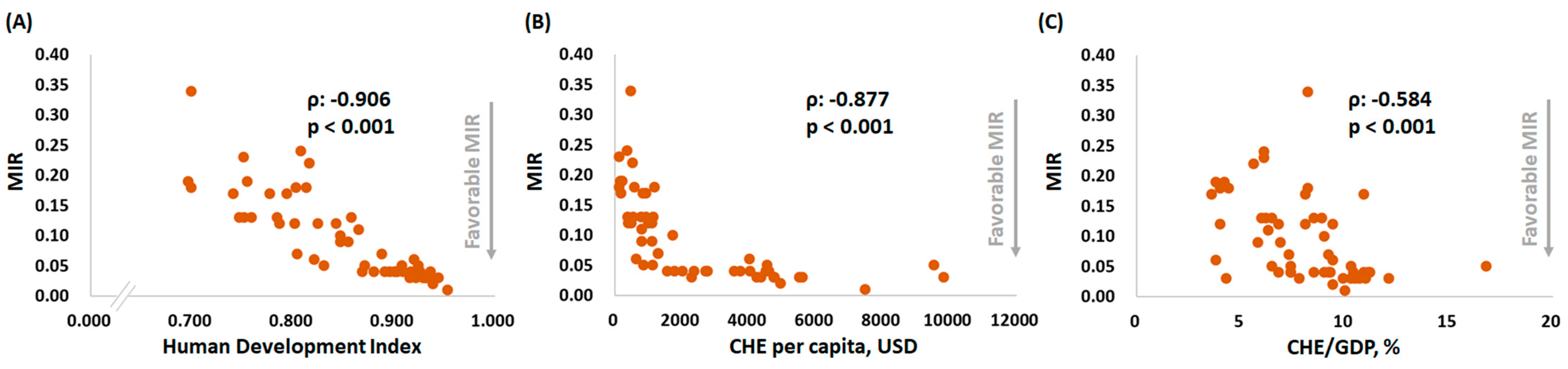
3.2. A Country’s HDI and CHE Are Significantly Associated with a Favorable MIR for Testicular Cancer
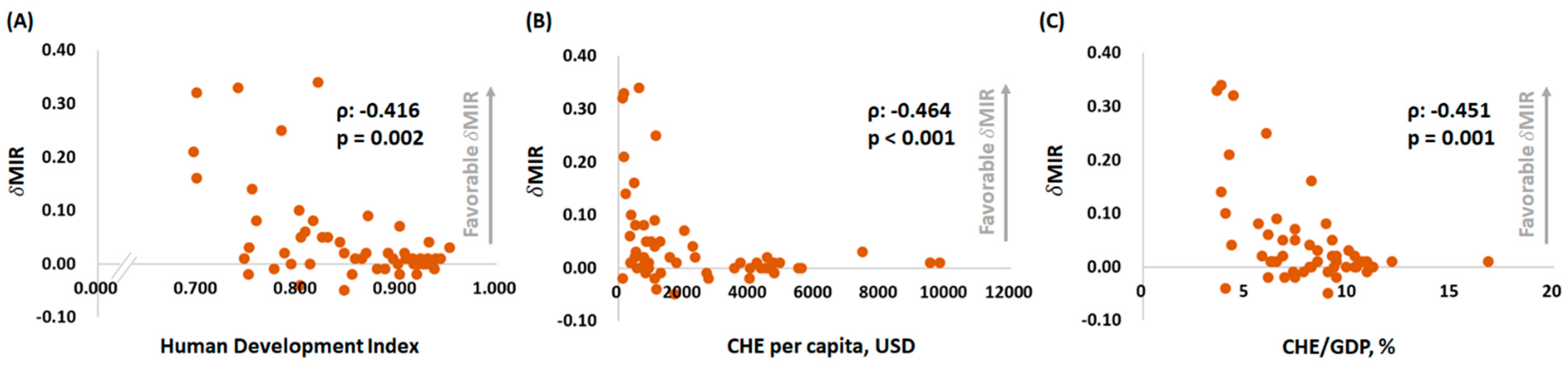
3.3. A Country’s HDI and CHE Are Significantly Associated with an Unfavorable δMIR for Testicular Cancer
4. Discussion.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Znaor, A.; Tieulent, L.J.; Jemal, A.; Bray, F. International variations and trends in testicular cancer incidence and mortality. Eur. Urol. 2014, 65, 1095–1106. [Google Scholar] [CrossRef] [PubMed]
- Pishgar, F.; Mirzaian, H.A.; Ebrahimi, H.; Moghaddam, S.S.; Mohajer, B.; Nowroozi, M.R.; Ayati, M.; Farzadfar, F.; Fitzmaurice, C.; Amini, E. Global, regional and national burden of testicular cancer, 1990–2016: Results from the Global Burden of Disease Study 2016. BJU Int. 2019, 124, 386–394. [Google Scholar] [CrossRef]
- Gurney, J.K.; Florio, A.A.; Znaor, A.; Ferlay, J.; Laversanne, M.; Sarfati, D.; Bray, F.; McGlynn, K.A. International Trends in the Incidence of Testicular Cancer: Lessons from 35 Years and 41 Countries. Eur. Urol. 2019, 76, 615–623. [Google Scholar] [CrossRef]
- Fode, M.; Jensen, C.F.; Azawi, N.; Østergren, P.B. Perspectives on a Global Change in Testicular Cancer Incidence. Eur. Urol. 2019, 76, 624–625. [Google Scholar] [CrossRef]
- Toni, D.L.; Sabovic, I.; Cosci, I.; Ghezzi, M.; Foresta, C.; Garolla, A. Testicular Cancer: Genes, Environment, Hormones. Front. Endocrinol. 2019, 10, 408. [Google Scholar] [CrossRef]
- Skakkebaek, N.E.; Meyts, R.D.E.; Main, K.M. Testicular dysgenesis syndrome: An increasingly common developmental disorder with environmental aspects. Hum. Reprod. 2001, 16, 972–978. [Google Scholar] [CrossRef] [PubMed]
- Richiardi, L.; Vizzini, L.; Pastore, G.; Segnan, N.; Tos, G.A.; Fiano, V.; Grasso, C.; Ciuffreda, L.; Lista, P.; Pearce, N.; et al. Lifetime growth and risk of testicular cancer. Int. J. Cancer 2014, 135, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Kim, J.; Elghiaty, A.; Ham, W.S. Recent global trends in testicular cancer incidence and mortality. Medicine (Baltimore) 2018, 97, 2390. [Google Scholar] [CrossRef]
- Rezaeian, S.; Khazaei, S.; Mansori, K.; Mansori, K.; Sanjari, M.A.; Ayubi, E. Human Development Inequality Index and Cancer Pattern: A Global Distributive Study. Asian Pac. J. Cancer Prev. 2016, 17, 201–204. [Google Scholar] [CrossRef][Green Version]
- Sadeghi, M.; Ghoncheh, M.; Hafshejani, M.A.; Mansori, K.; Sanjari, M.A.; Ayubi, E. Incidence and Mortality of Testicular Cancer and Relationships with Development in Asia. Asian Pac. J. Cancer Prev. 2016, 17, 4251–4257. [Google Scholar]
- Grasgruber, P.; Hrazdira, E.; Sebera, M.; Kalina, T. Cancer Incidence in Europe: An Ecological Analysis of Nutritional and Other Environmental Factors. Front. Oncol. 2018, 8, 151. [Google Scholar] [CrossRef]
- Ellis, L.; Belot, A.; Rachet, B.; Coleman, M.P. The Mortality-to-Incidence Ratio Is Not a Valid Proxy for Cancer Survival. J. Glob. Oncol. 2019, 5, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.L.; Wang, S.C.; Ho, C.J.; Kao, Y.L.; Hsieh, T.Y.; Chen, W.J. Prostate Cancer Mortality-To-Incidence Ratios Are Associated with Cancer Care Disparities in 35 Countries. Sci. Rep. 2017, 7, 3. [Google Scholar] [CrossRef]
- Morales, C.A.; Savitzky, M.J.; Persivale, S.K.; Segura, E.R. Conceptual considerations and methodological recommendations for the use of the mortality-to-incidence ratio in time-lagged, ecological-level analysis for public health systems-oriented cancer research. Cancer 2016, 122, 486–487. [Google Scholar] [CrossRef] [PubMed]
- Hebert, J.R.; Daguise, V.G.; Hurley, D.M.; Wilkerson, R.C.; Mosley, C.M.; Adams, S.A.; Puett, R.; Burch, J.B.; Steck, S.E.; Aldrich, S.W.B.; et al. Mapping cancer mortality-to-incidence ratios to illustrate racial and sex disparities in a high-risk population. Cancer 2009, 115, 2539–2552. [Google Scholar] [CrossRef]
- Sunkara, V.; Hebert, J.R. The colorectal cancer mortality-to-incidence ratio as an indicator of global cancer screening and care. Cancer 2015, 121, 1563–1569. [Google Scholar] [CrossRef] [PubMed]
- Sunkara, V.; Hebert, J.R. The application of the mortality-to-incidence ratio for the evaluation of cancer care disparities globally. Cancer 2016, 122, 487–488. [Google Scholar] [CrossRef]
- Wang, S.C.; Sung, W.W.; Kao, Y.L.; Hsieh, T.Y.; Chen, W.J.; Chen, S.L.; Chang, H.R. The gender difference and mortality-to-incidence ratio relate to health care disparities in bladder cancer: National estimates from 33 countries. Sci. Rep. 2017, 7, 4360. [Google Scholar] [CrossRef]
- Chen, W.J.; Huang, C.Y.; Huang, Y.H.; Wang, S.C.; Hsieh, T.Y.; Chen, S.L.; Sung, W.W.; Lee, T.H. Correlations between Mortality-to-Incidence Ratios and Health Care Disparities in Testicular Cancer. Int. J. Environ. Res. Public Health 2019, 17, 130. [Google Scholar] [CrossRef]
- Sung, W.W.; Wang, S.C.; Hsieh, T.Y.; Ho, C.J.; Huang, C.Y.; Kao, Y.L.; Chen, W.J.; Chen, S.L. Favorable mortality-to-incidence ratios of kidney Cancer are associated with advanced health care systems. BMC Cancer 2018, 18, 792. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Znaor, A.; Skakkebaek, N.E.; Meyts, R.D.E.; Laversanne, M.; Kuliš, T.; Gurney, J.; Sarfati, D.; McGlynn, K.A.; Bray, F. Testicular cancer incidence predictions in Europe 2010-2035: A rising burden despite population ageing. Int. J. Cancer 2020, 147, 820–828. [Google Scholar] [CrossRef]
- Shanmugalingam, T.; Soultati, A.; Chowdhury, S.; Rudman, S.; Hemelrijck, V.M. Global incidence and outcome of testicular cancer. Clin. Epidemiol. 2013, 5, 417–427. [Google Scholar] [CrossRef]
- Saab, M.M.; Davoren, M.; Murphy, A.; Murphy, D.; Cooke, E.; Landers, M.; Fitzgerald, S.; Richardson, N.; Rovito, M.; Wagner, C.V. Promoting men’s awareness, self-examination, and help-seeking for testicular disorders: A systematic review of interventions. HRB Open Res. 2018, 1, 16. [Google Scholar] [CrossRef] [PubMed]
- Bertuccio, P.; Malvezzi, M.; Chatenoud, L.; Bosetti, C.; Negri, E.; Levi, F.; Vecchia, C.L. Testicular cancer mortality in the Americas, 1980–2003. Cancer 2007, 109, 776–779. [Google Scholar] [CrossRef]
- Ugwumba, F.O.; Aghaji, A.E. Testicular cancer: Management challenges in an African developing country. S. Afr. Med. J. 2010, 100, 452–455. [Google Scholar] [CrossRef]
- Chalya, P.L.; Simbila, S.; Rambau, P.F. Ten-year experience with testicular cancer at a tertiary care hospital in a resource-limited setting: A single centre experience in Tanzania. World J. Surg. Oncol. 2014, 12, 356. [Google Scholar] [CrossRef]
- Greiman, A.K.; Rosoff, J.S.; Prasad, S.M. Association of Human Development Index with global bladder, kidney, prostate and testis cancer incidence and mortality. BJU Int. 2017, 120, 799–807. [Google Scholar] [CrossRef] [PubMed]
| Region | Incidence | Mortality | MIR | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Number | CR | ASR | Cum. Risk | Number | CR | ASR | Cum. Risk | ||
| Continent | |||||||||
| Africa | 1784 | 0.28 | 0.34 | 0.03 | 666 | 0.1 | 0.16 | 0.02 | 0.36 |
| Asia | 19,178 | 0.83 | 0.77 | 0.06 | 4520 | 0.2 | 0.18 | 0.02 | 0.24 |
| Europe | 23,864 | 6.7 | 6.3 | 0.48 | 1571 | 0.44 | 0.35 | 0.03 | 0.07 |
| Latin America and the Caribbean | 15,200 | 4.7 | 4.4 | 0.33 | 1917 | 0.6 | 0.54 | 0.04 | 0.13 |
| North America | 9422 | 5.3 | 5.1 | 0.39 | 451 | 0.25 | 0.22 | 0.02 | 0.05 |
| Oceania | 1167 | 5.7 | 5.4 | 0.42 | 39 | 0.19 | 0.17 | 0.01 | 0.03 |
| Country | Human Development Index | Current Health Expenditure | Incidence | Mortality | Mortality-to-Incidence Ratio | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Score | Rank | Per Capita | % of GDP | ASR | CR | Cum. Risk | ASR | CR | Cum. Risk | 2012 | 2018 | δMIR | |
| Argentina | 0.825 | 47 | 998 | 6.8 | 7.20 | 7.80 | 0.55 | 0.84 | 0.93 | 0.07 | 0.17 | 0.12 | 0.05 |
| Australia | 0.939 | 3 | 4934 | 9.4 | 7.20 | 7.60 | 0.55 | 0.14 | 0.17 | 0.01 | 0.03 | 0.02 | 0.01 |
| Austria | 0.908 | 20 | 4536 | 10.3 | 7.40 | 8.10 | 0.58 | 0.29 | 0.40 | 0.03 | 0.07 | 0.05 | 0.02 |
| Belarus | 0.808 | 53 | 352 | 6.1 | 3.00 | 3.40 | 0.23 | 0.67 | 0.82 | 0.06 | 0.30 | 0.24 | 0.06 |
| Belgium | 0.916 | 17 | 4228 | 10.5 | 6.90 | 6.90 | 0.52 | 0.15 | 0.18 | 0.01 | 0.04 | 0.03 | 0.01 |
| Brazil | 0.759 | 79 | 780 | 8.9 | 3.40 | 3.60 | 0.25 | 0.39 | 0.45 | 0.03 | 0.21 | 0.13 | 0.08 |
| Bulgaria | 0.813 | 51 | 572 | 8.2 | 5.10 | 5.50 | 0.40 | 0.82 | 1.00 | 0.07 | 0.18 | 0.18 | 0.00 |
| Canada | 0.926 | 12 | 4508 | 10.4 | 6.10 | 6.30 | 0.46 | 0.20 | 0.25 | 0.02 | 0.04 | 0.04 | 0.00 |
| Chile | 0.843 | 44 | 1102 | 8.1 | 9.50 | 10.70 | 0.72 | 1.10 | 1.30 | 0.09 | 0.16 | 0.12 | 0.04 |
| Colombia | 0.747 | 90 | 374 | 6.2 | 4.70 | 5.30 | 0.36 | 0.63 | 0.71 | 0.05 | 0.14 | 0.13 | 0.01 |
| Costa Rica | 0.794 | 63 | 929 | 8.1 | 3.00 | 3.30 | 0.22 | 0.50 | 0.57 | 0.04 | 0.17 | 0.17 | 0.00 |
| Croatia | 0.831 | 46 | 852 | 7.4 | 12.50 | 13.60 | 0.96 | 0.60 | 0.71 | 0.05 | 0.10 | 0.05 | 0.05 |
| Cuba | 0.777 | 73 | 826 | 10.9 | 1.40 | 1.90 | 0.13 | 0.24 | 0.32 | 0.02 | 0.16 | 0.17 | −0.01 |
| Cyprus | 0.869 | 32 | 1563 | 6.8 | 6.90 | 8.00 | 0.51 | 0.31 | 0.34 | 0.02 | 0.06 | 0.04 | 0.02 |
| Czechia | 0.888 | 27 | 1284 | 7.3 | 7.70 | 8.50 | 0.59 | 0.45 | 0.60 | 0.04 | 0.06 | 0.07 | −0.01 |
| Denmark | 0.929 | 11 | 5497 | 10.3 | 9.30 | 9.50 | 0.72 | 0.21 | 0.25 | 0.02 | 0.03 | 0.03 | 0.00 |
| Ecuador | 0.752 | 86 | 530 | 8.5 | 4.10 | 4.40 | 0.30 | 0.53 | 0.57 | 0.04 | 0.16 | 0.13 | 0.03 |
| Egypt | 0.696 | 115 | 157 | 4.2 | 0.43 | 0.43 | 0.04 | 0.10 | 0.08 | 0.01 | 0.40 | 0.19 | 0.21 |
| Estonia | 0.871 | 30 | 1112 | 6.5 | 3.40 | 3.50 | 0.25 | 0.25 | 0.17 | 0.02 | 0.14 | 0.05 | 0.09 |
| Fiji | 0.741 | 92 | 175 | 3.6 | 3.70 | 3.90 | 0.28 | 0.71 | 0.65 | 0.08 | 0.50 | 0.17 | 0.33 |
| Finland | 0.920 | 15 | 4005 | 9.4 | 8.40 | 8.20 | 0.62 | 0.44 | 0.48 | 0.04 | 0.04 | 0.06 | −0.02 |
| France | 0.901 | 24 | 4026 | 11.1 | 10.10 | 10.20 | 0.78 | 0.35 | 0.40 | 0.03 | 0.04 | 0.04 | 0.00 |
| Germany | 0.936 | 5 | 4592 | 11.2 | 9.90 | 10.90 | 0.79 | 0.31 | 0.42 | 0.03 | 0.04 | 0.04 | 0.00 |
| Ireland | 0.938 | 4 | 4757 | 7.8 | 7.90 | 8.10 | 0.60 | 0.19 | 0.21 | 0.02 | 0.02 | 0.03 | −0.01 |
| Israel | 0.903 | 22 | 2756 | 7.4 | 3.80 | 3.80 | 0.29 | 0.13 | 0.14 | 0.01 | 0.02 | 0.04 | −0.02 |
| Italy | 0.880 | 28 | 2700 | 9.0 | 8.10 | 7.70 | 0.60 | 0.26 | 0.31 | 0.02 | 0.03 | 0.04 | −0.01 |
| Japan | 0.909 | 19 | 3733 | 10.9 | 3.00 | 3.20 | 0.24 | 0.11 | 0.13 | 0.01 | 0.05 | 0.04 | 0.01 |
| Kuwait | 0.803 | 56 | 1169 | 4.0 | 0.90 | 0.95 | 0.06 | 0.25 | 0.17 | 0.01 | 0.14 | 0.18 | −0.04 |
| Latvia | 0.847 | 41 | 784 | 5.8 | 3.30 | 4.00 | 0.28 | 0.27 | 0.34 | 0.02 | 0.11 | 0.09 | 0.02 |
| Lithuania | 0.858 | 35 | 923 | 6.5 | 2.60 | 3.00 | 0.21 | 0.31 | 0.38 | 0.03 | 0.14 | 0.13 | 0.01 |
| Malaysia | 0.802 | 57 | 386 | 4.0 | 0.59 | 0.66 | 0.04 | 0.08 | 0.08 | 0.01 | 0.22 | 0.12 | 0.10 |
| Netherlands | 0.931 | 10 | 4746 | 10.7 | 10.60 | 10.30 | 0.79 | 0.21 | 0.26 | 0.02 | 0.04 | 0.03 | 0.01 |
| New Zealand | 0.917 | 16 | 3554 | 9.3 | 7.20 | 7.40 | 0.56 | 0.23 | 0.26 | 0.02 | 0.04 | 0.04 | 0.00 |
| Norway | 0.953 | 1 | 7464 | 10.0 | 12.20 | 13.00 | 0.94 | 0.15 | 0.19 | 0.01 | 0.04 | 0.01 | 0.03 |
| Oman | 0.821 | 48 | 636 | 3.8 | 0.52 | 1.00 | 0.03 | 0.05 | 0.06 | 0.00 | 0.40 | 0.06 | 0.34 |
| Philippines | 0.699 | 113 | 127 | 4.4 | 0.69 | 0.66 | 0.06 | 0.15 | 0.12 | 0.02 | 0.50 | 0.18 | 0.32 |
| Poland | 0.865 | 33 | 797 | 6.3 | 7.00 | 7.70 | 0.53 | 0.69 | 0.87 | 0.06 | 0.12 | 0.11 | 0.01 |
| Portugal | 0.847 | 41 | 1722 | 9.0 | 3.10 | 3.00 | 0.22 | 0.23 | 0.31 | 0.02 | 0.05 | 0.10 | −0.05 |
| Russian Federation | 0.816 | 49 | 524 | 5.6 | 1.90 | 2.20 | 0.15 | 0.39 | 0.49 | 0.03 | 0.30 | 0.22 | 0.08 |
| Serbia | 0.787 | 67 | 491 | 9.4 | 7.80 | 8.00 | 0.57 | 0.80 | 0.99 | 0.07 | 0.14 | 0.12 | 0.02 |
| Singapore | 0.932 | 9 | 2280 | 4.3 | 1.20 | 1.30 | 0.09 | 0.02 | 0.04 | 0.00 | 0.07 | 0.03 | 0.04 |
| Slovakia | 0.855 | 38 | 1108 | 6.9 | 9.50 | 10.10 | 0.69 | 0.72 | 0.88 | 0.06 | 0.07 | 0.09 | −0.02 |
| Slovenia | 0.896 | 25 | 1772 | 8.5 | 10.60 | 11.00 | 0.79 | 0.28 | 0.49 | 0.03 | 0.05 | 0.04 | 0.01 |
| South Africa | 0.699 | 113 | 471 | 8.2 | 0.76 | 0.77 | 0.07 | 0.29 | 0.26 | 0.03 | 0.50 | 0.34 | 0.16 |
| South Korea | 0.903 | 22 | 2013 | 7.4 | 1.60 | 1.50 | 0.11 | 0.05 | 0.06 | 0.00 | 0.11 | 0.04 | 0.07 |
| Spain | 0.891 | 26 | 2354 | 9.2 | 5.10 | 5.00 | 0.37 | 0.17 | 0.21 | 0.01 | 0.06 | 0.04 | 0.02 |
| Sweden | 0.933 | 7 | 5600 | 11.0 | 7.60 | 7.80 | 0.58 | 0.20 | 0.24 | 0.02 | 0.03 | 0.03 | 0.00 |
| Switzerland | 0.944 | 2 | 9818 | 12.1 | 9.40 | 10.30 | 0.74 | 0.19 | 0.26 | 0.02 | 0.04 | 0.03 | 0.01 |
| Thailand | 0.755 | 83 | 217 | 3.8 | 0.70 | 0.74 | 0.05 | 0.12 | 0.14 | 0.01 | 0.33 | 0.19 | 0.14 |
| Trinidad and Tobago | 0.784 | 69 | 1146 | 6.0 | 0.91 | 1.20 | 0.08 | 0.16 | 0.15 | 0.01 | 0.38 | 0.13 | 0.25 |
| Ukraine | 0.751 | 88 | 125 | 6.1 | 2.50 | 2.90 | 0.20 | 0.53 | 0.67 | 0.05 | 0.21 | 0.23 | −0.02 |
| United Kingdom | 0.922 | 14 | 4356 | 9.9 | 7.10 | 7.60 | 0.57 | 0.16 | 0.20 | 0.01 | 0.03 | 0.03 | 0.00 |
| United States of America | 0.924 | 13 | 9536 | 16.8 | 5.00 | 5.20 | 0.38 | 0.23 | 0.25 | 0.02 | 0.06 | 0.05 | 0.01 |
| Uruguay | 0.804 | 55 | 1281 | 9.2 | 7.70 | 8.20 | 0.58 | 0.54 | 0.60 | 0.05 | 0.12 | 0.07 | 0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, S.-C.; Chang, N.-W.; Chen, W.-J.; Yang, M.-H.; Chen, S.-L.; Sung, W.-W. Trends of Testicular Cancer Mortality-to-Incidence Ratios in Relation to Health Expenditure: An Ecological Study of 54 Countries. Int. J. Environ. Res. Public Health 2021, 18, 1546. https://doi.org/10.3390/ijerph18041546
Wang S-C, Chang N-W, Chen W-J, Yang M-H, Chen S-L, Sung W-W. Trends of Testicular Cancer Mortality-to-Incidence Ratios in Relation to Health Expenditure: An Ecological Study of 54 Countries. International Journal of Environmental Research and Public Health. 2021; 18(4):1546. https://doi.org/10.3390/ijerph18041546
Chicago/Turabian StyleWang, Shao-Chuan, Nai-Wen Chang, Wen-Jung Chen, Min-Hsin Yang, Sung-Lang Chen, and Wen-Wei Sung. 2021. "Trends of Testicular Cancer Mortality-to-Incidence Ratios in Relation to Health Expenditure: An Ecological Study of 54 Countries" International Journal of Environmental Research and Public Health 18, no. 4: 1546. https://doi.org/10.3390/ijerph18041546
APA StyleWang, S.-C., Chang, N.-W., Chen, W.-J., Yang, M.-H., Chen, S.-L., & Sung, W.-W. (2021). Trends of Testicular Cancer Mortality-to-Incidence Ratios in Relation to Health Expenditure: An Ecological Study of 54 Countries. International Journal of Environmental Research and Public Health, 18(4), 1546. https://doi.org/10.3390/ijerph18041546








