Functional-Belief-Based Alcohol Use Questionnaire (FBAQ) as a Pre-Screening Tool for High-Risk Drinking Behaviors among Young Adults: A Northern Thai Cross-Sectional Survey Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Study Endpoint
2.4. Statistical Analysis
2.4.1. Diagnostic Score Derivation
2.4.2. Diagnostic Performance of the Score
2.4.3. Diagnostic Accuracy of the Score
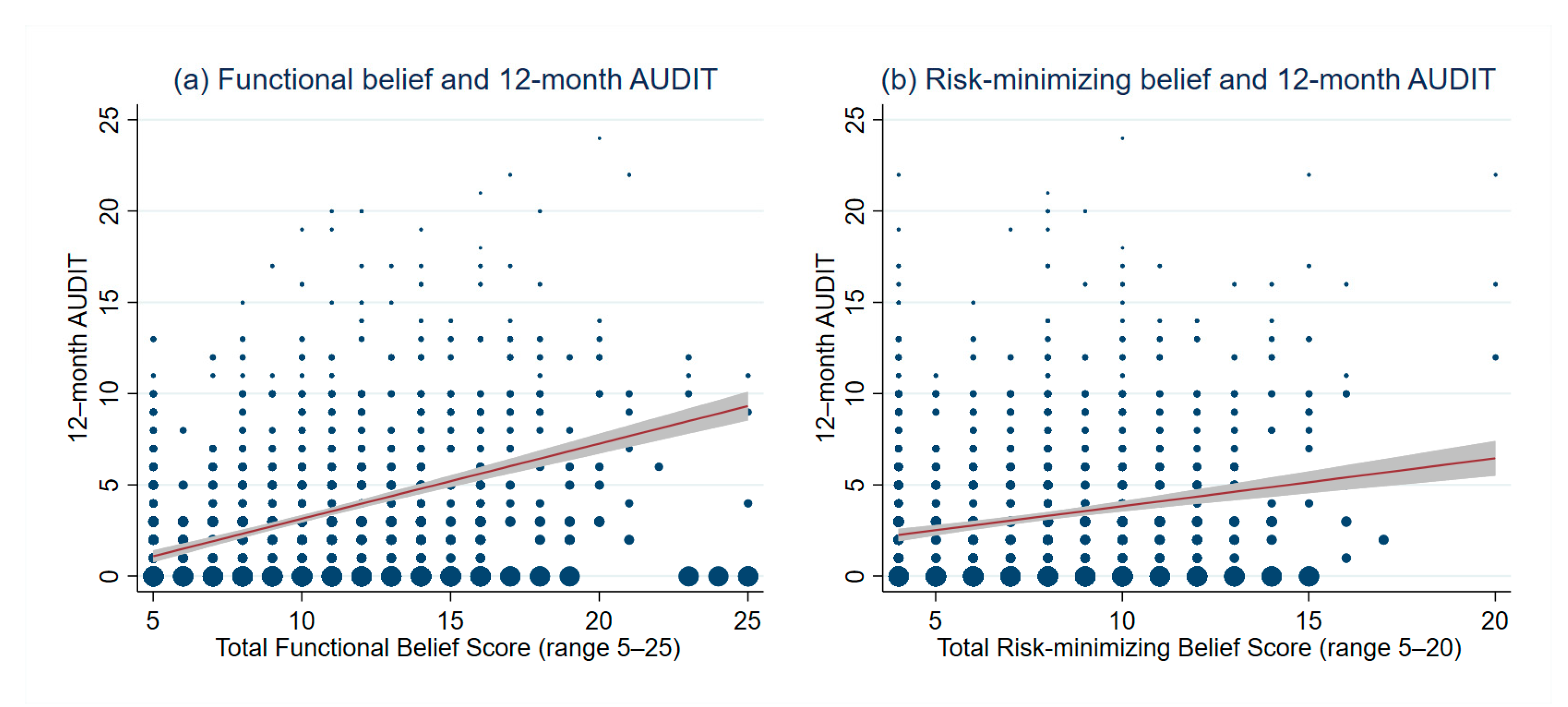
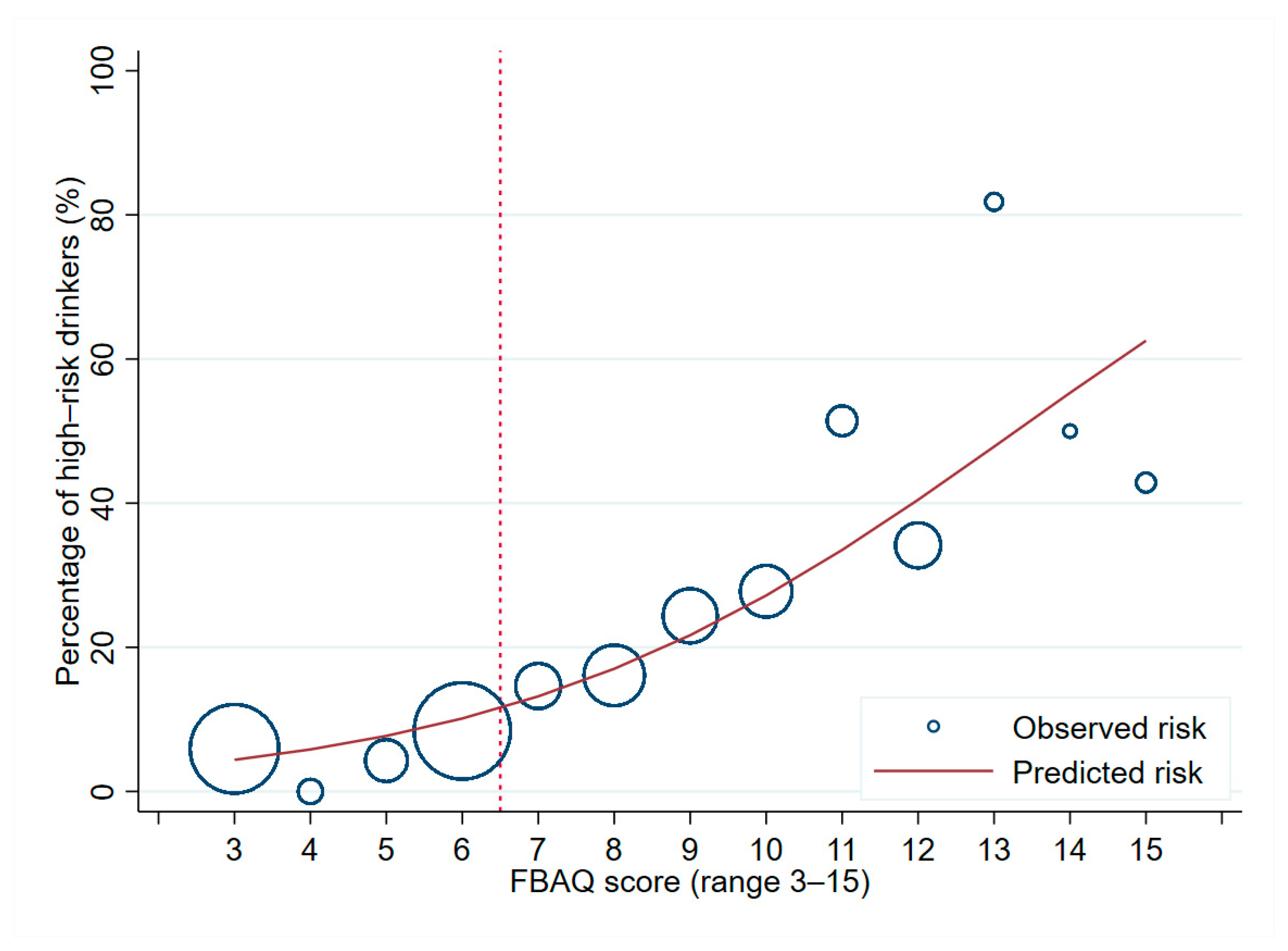
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grucza, R.A.; Sher, K.J.; Kerr, W.C.; Krauss, M.J.; Lui, C.K.; McDowell, Y.E.; Hartz, S.; Virdi, G.; Bierut, L.J. Trends in adult alcohol use and binge drinking in the early 21st-century United States: A meta-analysis of 6 national survey series. Alcohol. Clin. Exp. Res. 2018, 42, 1939–1950. [Google Scholar] [CrossRef] [PubMed]
- Assanangkornchai, S.; Sam-Angsri, N.; Rerngpongpan, S.; Lertnakorn, A. Patterns of alcohol consumption in the Thai population: Results of the national household survey of 2007. Alcohol Alcohol. 2010, 45, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Wakabayashi, M.; Thai Cohort Study Team; McKETIN, R.; Banwell, C.; Yiengprugsawan, V.; Kelly, M.; Seubsman, S.-A.; Iso, H.; Sleigh, A.C. Alcohol consumption patterns in Thailand and their relationship with non-communicable disease. BMC Public Health 2015, 15, 1–9. [Google Scholar] [CrossRef]
- Astudillo, M.; Kuntsche, S.; Graham, K.; Gmel, G. The influence of drinking pattern, at individual and aggregate levels, on alcohol-related negative consequences. Eur. Addict. Res. 2010, 16, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Sritara, P.; Huckle, T.; Mackintosh, A.-M.; Meier, P.; Parry, C.D.H.; Callinan, S.; Cuong, P.V.; Kazantseva, E.; Gray-Phillip, G.; Parker, K.; et al. Drinking patterns vary by gender, age and country-level income: Cross-country analysis of the international alcohol control study. Drug Alcohol Rev. 2018, 37, S53–S62. [Google Scholar] [CrossRef]
- Nair, U.R.; Vidhukumar, K.; Prabhakaran, A. Age at onset of alcohol use and alcohol use disorder: Time-trend study in patients seeking de-addiction services in Kerala. Indian J. Psychol. Med. 2016, 38, 315–319. [Google Scholar] [CrossRef]
- Assanangkornchai, S.; Vichitkunakorn, P. Does drinking initiation of young Thai drinkers vary over time and generation? Results of the national surveys on tobacco and alcohol consumption of the Thai populations 2007 to 2017. Alcohol. Clin. Exp. Res. 2020, 44, 2239–2246. [Google Scholar] [CrossRef]
- Nakhirunkanok, P.; Areesantichai, C. Binge drinking of alcohol consumption among young adults in high socioeconomic nightclubs, Bangkok—Thailand. J. Health Res. 2012, 26, 85–88. [Google Scholar]
- Kim, M.J.; Mason, W.A.; Herrenkohl, T.I.; Catalano, R.F.; Toumbourou, J.W.; Hemphill, S.A. Influence of early onset of alcohol use on the development of adolescent alcohol problems: A longitudinal binational study. Prev. Sci. 2017, 18, 1–11. [Google Scholar] [CrossRef]
- White, A.; Hingson, R. The burden of alcohol use. Alcohol Res. Curr. Rev. 2013, 35, 201–218. [Google Scholar]
- Hodgins, D.C.; Racicot, S. The link between drinking and gambling among undergraduate university students. Psychol. Addict. Behav. 2013, 27, 885–892. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.E.; Oeltmann, J.; Wilson, T.W.; Brener, N.D.; Hill, C.V. Binge drinking among undergraduate college students in the United States: Implications for other substance use. J. Am. Coll. Health 2001, 50, 33–38. [Google Scholar] [CrossRef]
- Jakkaew, N.; Pinyopornpanish, K.; Jiraporncharoen, W.; Wisetborisut, A.; Jiraniramai, S.; Hashmi, A.; Angkurawaranon, C. Risk of harm from alcohol use and heavy alcohol consumption: Its association with other NCD risk factors in Thailand. Sci. Rep. 2019, 9, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Room, R.; Ferris, J.; Laslett, A.-M.; Livingston, M.; Mugavin, J.; Wilkinson, C. The drinker’s effect on the social environment: A conceptual framework for studying alcohol’s harm to others. Int. J. Environ. Res. Public Health 2010, 7, 1855–1871. [Google Scholar] [CrossRef] [PubMed]
- Wattanapisit, A.; Jiraporncharoen, W.; Pinyopornpanish, K.; Jiraniramai, S.; Thaikla, K.; Angkurawaranon, C. Health-risk behaviours and injuries among youth and young adults in Chiang Mai, Thailand: A population-based survey. Int. J. Environ. Res. Public Health 2020, 17, 3696. [Google Scholar] [CrossRef] [PubMed]
- Knox, J.; Hasin, D.S.; Larson, F.R.R.; Kranzler, H.R. Prevention, screening, and treatment for heavy drinking and alcohol use disorder. Lancet Psychiatry 2019, 6, 1054–1067. [Google Scholar] [CrossRef]
- Yuma, P.J.; Lawson, K.A.; Velasquez, M.M.; Von Sternberg, K.; Maxson, T.; Garcia, N. Screening, brief intervention, and referral for alcohol use in adolescents: A systematic review. Pediatrics 2012, 130, 115–122. [Google Scholar] [CrossRef]
- Babor, T.F.; Higgins-Biddle, J.C. Alcohol screening and brief intervention: Dissemination strategies for medical practice and public health. Addiction 2000, 95, 677–686. [Google Scholar] [CrossRef]
- Kuteesa, M.O.; Cook, S.; Weiss, H.A.; Kamali, A.; Weinmann, W.; Seeley, J.; Ssentongo, J.N.; Kiwanuka, T.; Namyalo, F.; Nsubuga, D.; et al. Comparing Alcohol Use Disorders Identification Test (AUDIT) with Timeline Follow Back (TLFB), DSM-5 and Phosphatidylethanol (PEth) for the assessment of alcohol misuse among young people in Ugandan fishing communities. Addict. Behav. Rep. 2019, 10, 100233. [Google Scholar] [CrossRef]
- Johnson, J.A.; Lee, A.; Vinson, D.; Seale, J.P. Use of AUDIT-based measures to identify unhealthy alcohol use and alcohol dependence in primary care: A validation study. Alcohol Clin. Exp. Res. 2012, 37, E253–E259. [Google Scholar] [CrossRef]
- Francis, J.M.; A Weiss, H.; Helander, A.; Kapiga, S.H.; Changalucha, J.; Grosskurth, H. Comparison of self-reported alcohol use with the alcohol biomarker phosphatidylethanol among young people in northern Tanzania. Drug Alcohol Depend. 2015, 156, 289–296. [Google Scholar] [CrossRef]
- Kerr, W.C.; Stockwell, T. Understanding standard drinks and drinking guidelines. Drug Alcohol Rev. 2011, 31, 200–205. [Google Scholar] [CrossRef]
- Gual, A.; Martos, A.R.; Lligoña, A.; Llopis, J.J. Does the concept of a standard drink apply to viticultural societies? Alcohol Alcohol. 1999, 34, 153–160. [Google Scholar] [CrossRef]
- Khadjesari, Z.; White, I.R.; McCambridge, J.; Marston, L.; Wallace, P.; Godfrey, C.; Murray, E. Validation of the AUDIT-C in adults seeking help with their drinking online. Addict. Sci. Clin. Prac. 2017, 12, 1–11. [Google Scholar] [CrossRef]
- Aalto, M.; Alho, H.; Halme, J.T.; Seppä, K. AUDIT and its abbreviated versions in detecting heavy and binge drinking in a general population survey. Drug Alcohol Depend. 2009, 103, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Minugh, P.A.; Rice, C.; Young, L. Gender, health beliefs, health behaviors, and alcohol consumption. Am. J. Drug Alcohol Abus. 1998, 24, 483–497. [Google Scholar] [CrossRef] [PubMed]
- Jiraniramai, S.; Likhitsathian, S.; Jiraporncharoen, W.; Thaikla, K.; Aramrattana, A.; Angkurawaranon, C. Risk-minimizing belief: Its association with smoking and risk of harm from smoking in northern Thailand. J. Ethn. Subst. Abus. 2015, 14, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Blume, A.W.; Lostutter, T.W.; Schmaling, K.B.; Marlatt, G.A. Beliefs about drinking behavior predict drinking consequences. J. Psychoact. Drugs 2003, 35, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Critchlow, B. The powers of John Barleycorn: Beliefs about the effects of alcohol on social behavior. Am. Psychol. 1986, 41, 751–764. [Google Scholar] [CrossRef]
- Brown, S.A.; Carrello, P.D.; Vik, P.W.; Porter, R.J. Change in alcohol effect and self-efficacy expectancies during addiction treatment. Subst. Abus. 1998, 19, 155–167. [Google Scholar] [CrossRef]
- Oei, T.P.; Baldwin, A.R. Expectancy theory: A two-process model of alcohol use and abuse. J. Stud. Alcohol 1994, 55, 525–534. [Google Scholar] [CrossRef]
- Oei, T.P.; Fergusson, S.; Lee, N.K. The differential role of alcohol expectancies and drinking refusal self-efficacy in problem and nonproblem drinkers. J. Stud. Alcohol 1998, 59, 704–711. [Google Scholar] [CrossRef][Green Version]
- Brotchie, J.; Meyer, C.; Copello, A.; Kidney, R.; Waller, G. Cognitive representations in alcohol and opiate abuse: The role of core beliefs. Br. J. Clin. Psychol. 2004, 43, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Jiraniramai, S.; Jiraporncharoen, W.; Pinyopornpanish, K.; Jakkaew, N.; Wongpakaran, T.; Angkurawaranon, C. Functional beliefs and risk minimizing beliefs among Thai healthcare workers in Maharaj Nakorn Chiang Mai hospital: Its association with intention to quit tobacco and alcohol. Subst. Abus. Treat. Prev. Policy 2017, 12, 34. [Google Scholar] [CrossRef]
- Miles, H.; Winstock, A.R.; Strang, J. Identifying young people who drink too much: The clinical utility of the five-item Alcohol Use Disorders Identification Test (AUDIT). Drug Alcohol Rev. 2001, 20, 9–18. [Google Scholar] [CrossRef]
- Mona, A.E.-R.; Mahmoud, A.-K.; Amal, M.; Mahmoud, S. The application of alcohol brief intervention using the health belief model in hospitalised alcohol use disorders patients. Int. J. Caring Sci. 2014, 7, 843–854. [Google Scholar]
- Fotuhi, O.; Fong, G.T.; Zanna, M.P.; Borland, R.; Yong, H.-H.; Cummings, K.M. Patterns of cognitive dissonance-reducing beliefs among smokers: A longitudinal analysis from the International Tobacco Control (ITC) four country survey. Tob. Control. 2012, 22, 52–58. [Google Scholar] [CrossRef]
- Oakes, W.; Chapman, S.; Borland, R.; Balmford, J.; Trotter, L. Bulletproof skeptics in life’s jungle? Which self-exempting beliefs about smoking most predict lack of progression towards quitting? Prev. Med. 2004, 39, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Lapham, S.C.; Brown, P.; Suriyawongpaisal, P.; Skipper, B.J.; Chadbunchachai, W.; Paisarnsilp, S. Measurements, instruments, scales, and tests: Use of AUDIT for alcohol screening among emergency room patients in Thailand. Subst. Use Misuse 1999, 34, 1881–1895. [Google Scholar] [CrossRef]
- Sau, A. AUDIT (Alcohol Use Disorders Identification Test) to estimate the pattern and correlates of alcohol consumption among the adult population of west Bengal, India: A community based cross-sectional study. J. Clin. Diagn. Res. 2017, 11, LC01–LC04. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; De La Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Bravo, A.J.; Prince, M.A.; Pearson, M.R. College-related alcohol beliefs and problematic alcohol consumption: Alcohol protective behavioral strategies as a mediator. Subst. Use Misuse 2017, 52, 1059–1068. [Google Scholar] [CrossRef] [PubMed]
- Osberg, T.M.; Boyer, A. College alcohol beliefs and drinking consequences: A multiple mediation analysis of norms, expectancies, and willingness to experience drinking consequences. J. Am. Coll. Health 2018, 66, 209–218. [Google Scholar] [CrossRef]
- Yoshimoto, K.; McBride, W.; Lumeng, L.; Li, T.-K. Alcohol stimulates the release of dopamine and serotonin in the nucleus accumbens. Alcohol 1992, 9, 17–22. [Google Scholar] [CrossRef]
- Kano, M.; Gyoba, J.; Kamachi, M.; Mochizuki, H.; Hongo, M.; Yanai, K. Low doses of alcohol have a selective effect on the recognition of happy facial expressions. Hum. Psychopharmacol. Clin. Exp. 2003, 18, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Amaral, M.B.D.; Lourenço, L.M.; Ronzani, T.M. Beliefs about alcohol use among university students. J. Subst. Abus. Treat. 2006, 31, 181–185. [Google Scholar] [CrossRef]
- Crawford, L.A.; Novak, K.B. Alcohol abuse as a rite of passage: The effect of beliefs about alcohol and the college experience on undergraduates’ drinking behaviors. J. Drug Educ. 2006, 36, 193–212. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Young, A.; Morales, M.; McCabe, S.E.; Boyd, C.J.; D’Arcy, H. Drinking like a guy: Frequent binge drinking among undergraduate women. Subst. Use Misuse 2005, 40, 241–267. [Google Scholar] [CrossRef]
- Becker, J.B.; McClellan, M.L.; Reed, B.G. Sex differences, gender and addiction. J. Neurosci. Res. 2017, 95, 136–147. [Google Scholar] [CrossRef]
- Andrews, J.A.; Tildesley, E.; Hops, H.; Li, F. The influence of peers on young adult substance use. Health Psychol. 2002, 21, 349–357. [Google Scholar] [CrossRef]
- Schulte, M.T.; Ramo, D.; Brown, S.A. Gender differences in factors influencing alcohol use and drinking progression among adolescents. Clin. Psychol. Rev. 2009, 29, 535–547. [Google Scholar] [CrossRef] [PubMed]
- Borland, R.; Yong, H.-H.; Balmford, J.; Fong, G.T.; Zanna, M.P.; Hastings, G. Do risk-minimizing beliefs about smoking inhibit quitting? Findings from the International Tobacco Control (ITC) Four-Country Survey. Prev. Med. 2009, 49, 219–223. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Missing Data | Male (n = 763) | Female (n = 638) | Overall (n = 1401) | |||
|---|---|---|---|---|---|---|---|
| n (%) | n | (%) | n | (%) | n | (%) | |
| Age (years, mean ± SD) | 0(0) | 29.6 | ±6.4 | 30.2 | ±6.1 | 29.9 | ±6.3 |
| Religion | |||||||
| Buddhism | 1(0.1) | 742 | (97.4) | 612 | (95.9) | 1354 | (96.7) |
| Others | 20 | (2.6) | 26 | (4.1) | 46 | (3.3) | |
| Marital status | |||||||
| Single/divorced | 8(0.6) | 360 | (47.6) | 186 | (29.3) | 546 | (39.2) |
| Married | 397 | (52.4) | 450 | (70.7) | 847 | (60.8) | |
| Occupation | |||||||
| Constant income | 0(0) | 108 | (14.2) | 70 | (11.0) | 178 | (12.7) |
| Non-constant income | 503 | (65.9) | 400 | (62.7) | 903 | (64.5) | |
| No income/vacancy | 47 | (6.2) | 63 | (9.9) | 110 | (7.9) | |
| Others/unspecified | 105 | (13.8) | 105 | (16.5) | 210 | (15.0) | |
| Current smoker (within 12 months) | 0(0) | 298 | (37.9) | 11 | (1.7) | 300 | (21.4) |
| Current drinker (within 12 months) | 0(0) | 602 | (78.9) | 189 | (29.6) | 791 | (56.5) |
| Last drinking | |||||||
| Within 1 week | 0(0) | 326 | (42.7) | 80 | (12.5) | 406 | (29.0) |
| Within 1 month | 178 | (23.3) | 61 | (9.6) | 239 | (17.1) | |
| Over 1 month | 98 | (12.8) | 49 | (7.7) | 147 | (10.5) | |
| Over 12 months or never drink | 161 | (21.1) | 448 | (70.2) | 609 | (43.4) | |
| Drinking frequency within the past 12 months | |||||||
| Never drink | 0(0) | 161 | (21.1) | 450 | (70.5) | 611 | (43.6) |
| 5–7 days per week | 233 | (30.5) | 134 | (21.0) | 367 | (26.2) | |
| 3–4 days per week | 142 | (18.6) | 28 | (4.4) | 170 | (12.1) | |
| 1–2 days per week | 128 | (16.8) | 16 | (2.5) | 144 | (10.3) | |
| <4 times per month | 99 | (13.0) | 10 | (1.6) | 109 | (7.8) | |
| Number of standard drinks per day | |||||||
| Never drink | 0(0) | 315 | (41.3) | 537 | (84.2) | 852 | (60.8) |
| 1–2 | 264 | (34.6) | 66 | (10.3) | 330 | (23.6) | |
| 3–4 | 111 | (14.6) | 26 | (4.1) | 137 | (9.8) | |
| 5–6 | 38 | (5.0) | 4 | (0.6) | 42 | (3.0) | |
| 7–9 | 35 | (4.6) | 5 | (0.8) | 40 | (2.9) | |
| ≥10 | |||||||
| Total AUDIT score (mean ± SD) | 0(0) | 4.8 | ±4.5 | 1.2 | ±2.8 | 3.2 | ±4.2 |
| Median (IQR) | 0(0) | 4 | (1, 7) | 0 | (0, 1) | 1 | (0, 5) |
| 0–7 | 0(0) | 580 | (76.0) | 608 | (95.3) | 1188 | (84.8) |
| 8–15 | 158 | (20.7) | 27 | (4.2) | 185 | (13.2) | |
| 16–19 | 17 | (2.2) | 2 | (0.3) | 19 | (1.4) | |
| 20–40 | 8 | (1.1) | 1 | (0.2) | 9 | (0.6) | |
| High-risk drinking (≥8) | 183 | (24.0) | 30 | (4.7) | 213 | (15.2) | |
| Could not stop drinking | 611(43.6) | 71 | (11.8) | 20 | (10.6) | 91 | (11.5) |
| Impaired function due to drinking | 610(43.5) | 27 | (4.5) | 16 | (8.5) | 43 | (5.4) |
| Drinking for activity of daily living | 610(43.5) | 20 | (3.3) | 6 | (3.2) | 26 | (3.3) |
| Attempt to quit alcohol drinking | |||||||
| Never | 461(32.9) | 538 | (82.6) | 258 | (89.3) | 796 | (84.7) |
| Within the last 3 months | 45 | (6.9) | 17 | (5.9) | 82 | (8.7) | |
| More than 3 months | 68 | (10.5) | 14 | (4.8) | 62 | (6.6) | |
| High-Risk Drinking (AUDIT ≥ 8) (n = 213) | Low-Risk Drinking (AUDIT ≤ 7) (n = 1188) | Multivariable Model | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | ±SD | Mean | ±SD | p-Value | OR | 95%CI | p-Value | |
| Functional beliefs | ||||||||
| 2.49 | ±1.23 | 1.76 | ±0.87 | <0.001 | 1.25 | 1.04, 1.52 | 0.020 |
| 3.08 | ±1.27 | 2.12 | ±1.14 | <0.001 | 1.37 | 1.14, 1.64 | 0.001 |
| 2.13 | ±1.12 | 1.63 | ±0.74 | <0.001 | 0.96 | 0.74, 1.25 | 0.763 |
| 2.11 | ±1.06 | 1.59 | ±0.71 | <0.001 | 1.25 | 0.96, 1.63 | 0.094 |
| 3.28 | ±1.24 | 2.45 | ±1.24 | <0.001 | 1.25 | 1.06, 1.47 | 0.007 |
| Risk-minimizing beliefs | ||||||||
| 2.54 | ±1.29 | 2.26 | ±1.20 | 0.002 | 1.05 | 0.88, 1.24 | 0.599 |
| 2.21 | ±1.19 | 1.86 | ±0.94 | <0.001 | 1.08 | 0.86, 1.36 | 0.507 |
| 1.97 | ±1.05 | 1.61 | ±0.67 | <0.001 | 0.93 | 0.71, 1.21 | 0.574 |
| 1.97 | ±1.01 | 1.60 | ±0.66 | <0.001 | 1.23 | 0.96, 1.58 | 0.104 |
| Total beliefs score | 21.77 | ±6.37 | 16.89 | ±5.47 | <0.001 | |||
| OR | 95% CI | p-Value | Coefficient | Weighted Score | |
|---|---|---|---|---|---|
| You enjoy alcohol drinking too much to give it up | 1.36 | 1.15, 1.62 | <0.001 | 0.3101 | 1 × score |
| Alcohol drinking calms you down when you are stressed or upset | 1.40 | 1.17, 1.66 | <0.001 | 0.3331 | 1 × score |
| Alcohol drinking makes it easier for you to socialize | 1.29 | 1.10, 1.50 | 0.001 | 0.2512 | 1 × score |
| Constant | 0.02 | −3.9496 |
| Reference Standard | Index Test | Sensitivity (95% CI) | Specificity (95% CI) | Positive Likelihood Ratio (95% CI) | Negative Likelihood Ratio (95% CI) |
|---|---|---|---|---|---|
| Overall (n = 1401) | |||||
| 12-month AUDIT ≥ 8 | FBAQ ≥ 5 | 91.1 (86.4, 94.5) | 27.4 (24.8, 30.0) | 1.25 (1.19, 1.32) | 0.33 (0.21, 0.51) |
| FBAQ ≥ 6 | 89.7 (84.8, 93.4) | 33.0 (30.3, 35.8) | 1.34 (1.26, 1.42) | 0.31 (0.21, 0.47) | |
| FBAQ ≥ 7 | 74.6 (68.3, 80.3) | 62.4 (59.5, 65.1) | 1.98 (1.78, 2.21) | 0.41 (0.32, 0.51) | |
| Male (n = 763) | |||||
| 12-month AUDIT ≥ 8 | FBAQ ≥ 5 | 90.2 (84.9, 94.1) | 21.6 (18.3, 25.1) | 1.15 (1.08, 1.23) | 0.46 (0.29, 0.73) |
| FBAQ ≥ 6 | 88.5 (83.0, 92.8) | 27.6 (24.0, 31.4) | 1.22 (1.14, 1.31) | 0.42 (0.27, 0.64) | |
| FBAQ ≥ 7 | 72.7 (65.6, 79.0) | 54.5 (50.3, 58.6) | 1.60 (1.41, 1.81) | 0.50 (0.39, 0.64) | |
| Female (n = 638) | |||||
| 12-month AUDIT ≥ 8 | FBAQ ≥ 5 | 96.7 (82.8, 99.9) | 32.9 (29.2, 36.8) | 1.44 (1.32, 1.57) | 0.10 (0.01, 0.70) |
| FBAQ ≥ 6 | 96.7 (82.8, 99.9) | 38.2 (34.3, 42.2) | 1.56 (1.43, 1.71) | 0.09 (0.01, 0.60) | |
| FBAQ ≥ 7 | 86.7 (69.3, 96.2) | 69.9 (66.1, 73.5) | 2.88 (2.39, 3.47) | 0.19 (0.08, 0.48) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yingchankul, N.; Jiraporncharoen, W.; Pateekhum, C.; Jiraniramai, S.; Thaikla, K.; Angkurawaranon, C.; Phinyo, P. Functional-Belief-Based Alcohol Use Questionnaire (FBAQ) as a Pre-Screening Tool for High-Risk Drinking Behaviors among Young Adults: A Northern Thai Cross-Sectional Survey Analysis. Int. J. Environ. Res. Public Health 2021, 18, 1536. https://doi.org/10.3390/ijerph18041536
Yingchankul N, Jiraporncharoen W, Pateekhum C, Jiraniramai S, Thaikla K, Angkurawaranon C, Phinyo P. Functional-Belief-Based Alcohol Use Questionnaire (FBAQ) as a Pre-Screening Tool for High-Risk Drinking Behaviors among Young Adults: A Northern Thai Cross-Sectional Survey Analysis. International Journal of Environmental Research and Public Health. 2021; 18(4):1536. https://doi.org/10.3390/ijerph18041536
Chicago/Turabian StyleYingchankul, Nalinee, Wichuda Jiraporncharoen, Chanapat Pateekhum, Surin Jiraniramai, Kanittha Thaikla, Chaisiri Angkurawaranon, and Phichayut Phinyo. 2021. "Functional-Belief-Based Alcohol Use Questionnaire (FBAQ) as a Pre-Screening Tool for High-Risk Drinking Behaviors among Young Adults: A Northern Thai Cross-Sectional Survey Analysis" International Journal of Environmental Research and Public Health 18, no. 4: 1536. https://doi.org/10.3390/ijerph18041536
APA StyleYingchankul, N., Jiraporncharoen, W., Pateekhum, C., Jiraniramai, S., Thaikla, K., Angkurawaranon, C., & Phinyo, P. (2021). Functional-Belief-Based Alcohol Use Questionnaire (FBAQ) as a Pre-Screening Tool for High-Risk Drinking Behaviors among Young Adults: A Northern Thai Cross-Sectional Survey Analysis. International Journal of Environmental Research and Public Health, 18(4), 1536. https://doi.org/10.3390/ijerph18041536






