Bite Force in Elderly with Full Natural Dentition and Different Rehabilitation Prosthesis
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Inclusion Criteria
- -
- Subjects without problems, in everyday life, with natural dentition.
- -
- Subjects wearing telescopic overdentures with 4 implants (2 in canine zone and two in premolar zone).
- -
- Subjects wearing complete dentures in one arch (and natural teeth in the opposite arch) or both arches.
- -
- All people were wearing their prosthesis at least for 1 year.
- -
- No dental mobility or alveolar bone retraction ≤4.5 mm as measured by orthopantomography (OPT) [20].
- -
- No implant mobility or pain or alveolar bone retraction around implants <1.5 mm measured by intraoral periapical radiographs.
- -
- Absence of psychiatric diseases or movement problems.
- -
- Lack of articular/muscular, dental or spontaneous pain.
2.3. Exclusion Criteria
- -
- Poor oral hygiene.
- -
- Periodontitis.
- -
- Dental mobility.
- -
- Teeth alveolar bone retraction >4.5 mm on OPT.
- -
- Diabetes.
- -
- Ongoing chemotherapy.
2.4. Prostheses
2.5. Experimental Groups
- Subjects with natural full dentition (FD) (n = 204).
- Subjects wearing four implant-retained overdentures (two in canine zone and two in premolar zone) (IRO) (n = 40).
- Subjects with natural teeth in one arch and wearing traditional complete dentures (CD) in opposite dental arch (CD/T) (n = 44).
- Subjects wearing CD in both arches CD/CD (n = 40).
- Edentulous subjects in both arches (ED) (n = 40; the same patients of group 4 after removal of the CD).
2.6. Body Mass Index
2.7. Measurement of Patients Maximum Bite Force (MBF)
2.8. Statistical Analysis
3. Results
3.1. Bite Force and Gender
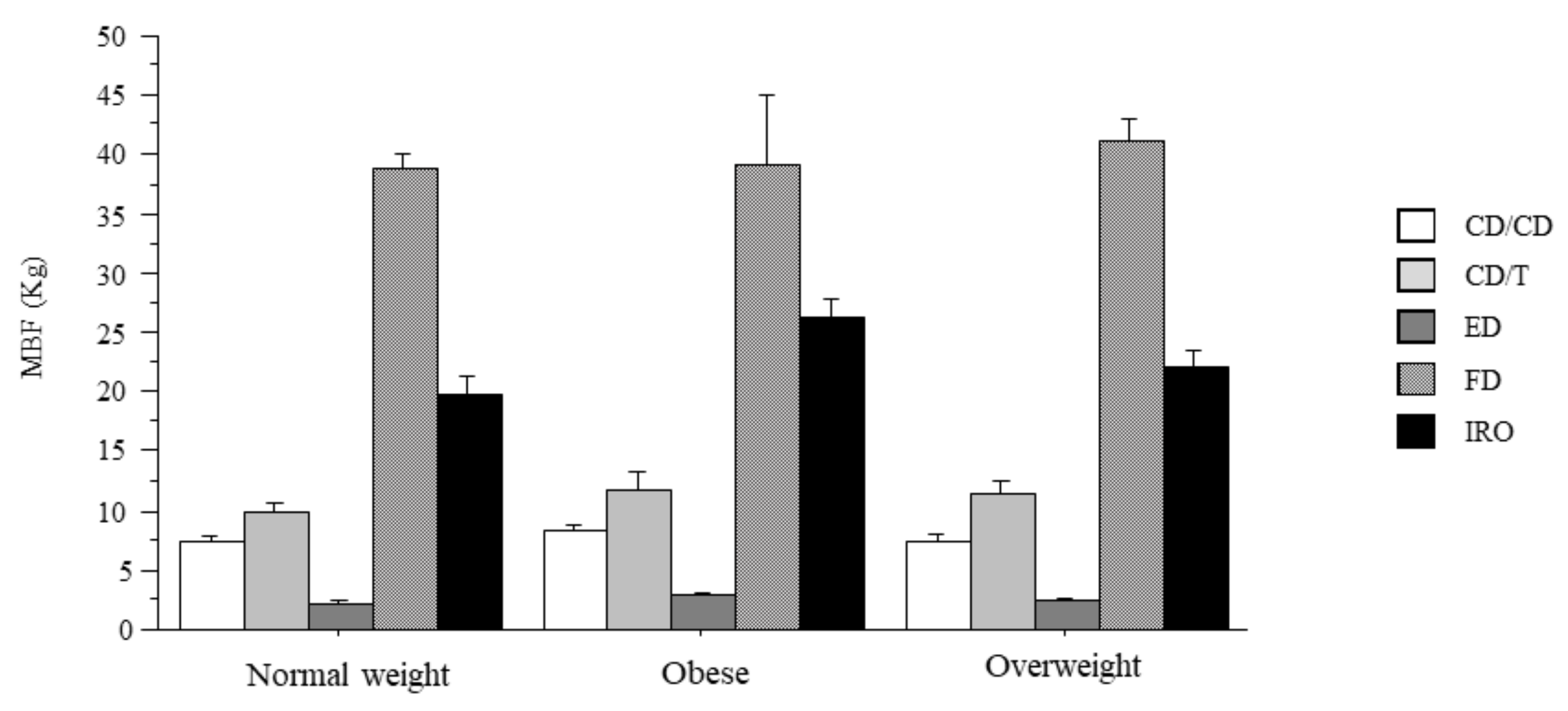
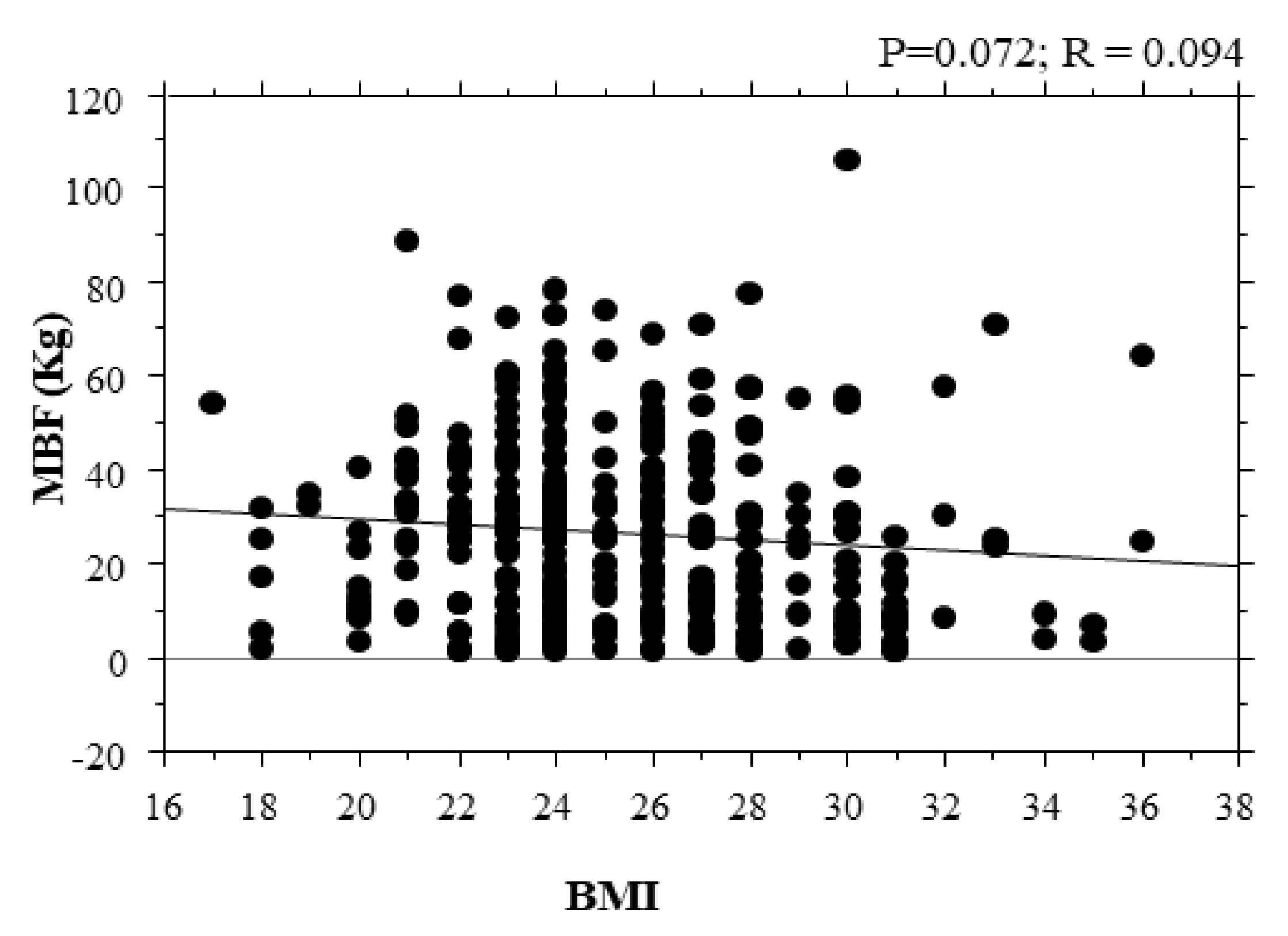
3.2. Bite Force and BMI
3.3. Bite Force and Prothesis
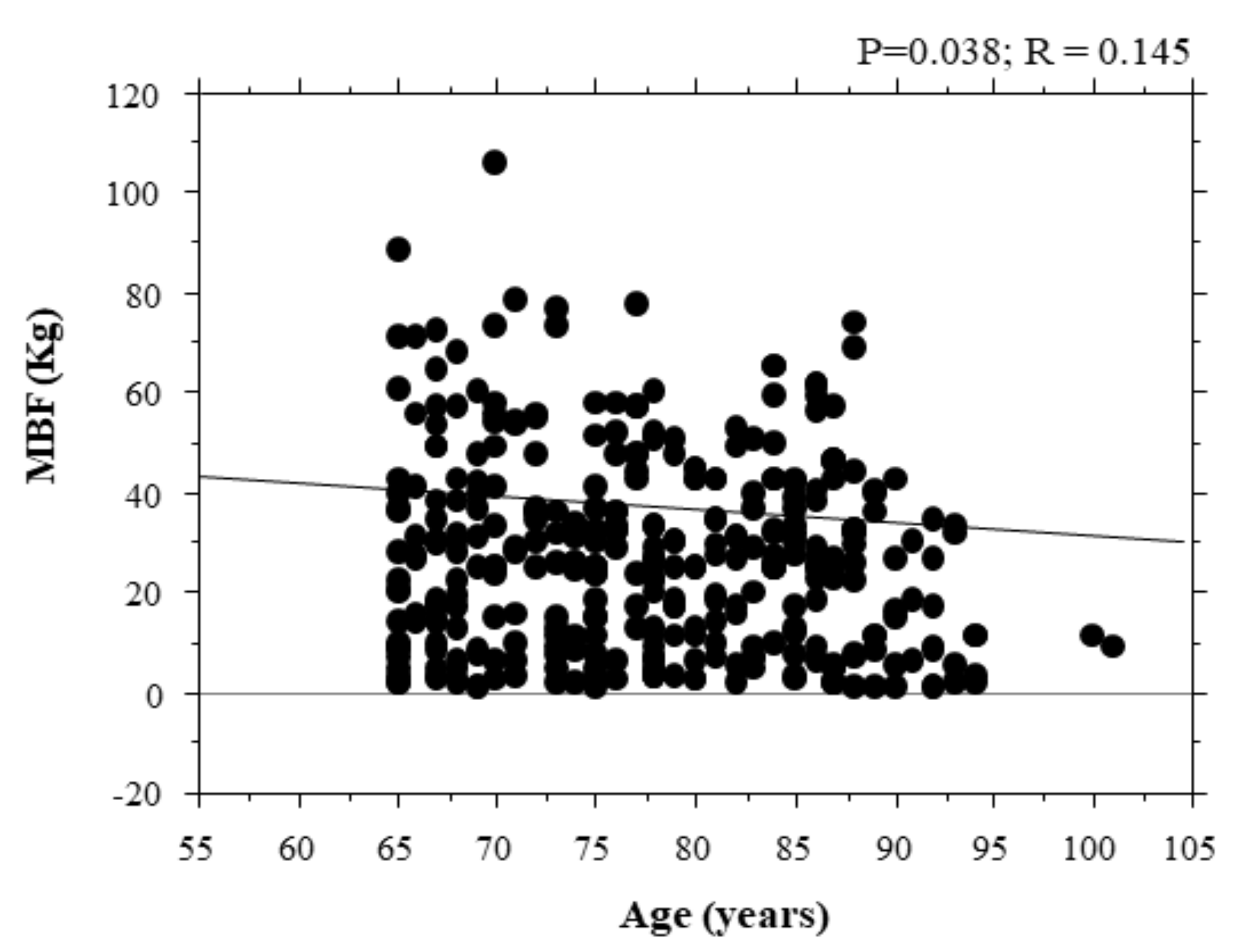
3.4. Correlation of Bite Force with Age
3.5. Correlations of Bite Force with Body Mass Index Values
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Supiyev, A.; Kossumov, A.; Utepova, L.; Kushugulova, A.; Nurgozhin, T.; Zhumadilov, Z. Elderly population. J. Nutr. Health Aging 2013, 17, 869. [Google Scholar]
- Eto, M.; Miyauchi, S. Relationship between occlusal force and falls among community-dwelling elderly in Japan: A cross-sectional correlative study. BMC Geriatr. 2018, 18, 111. [Google Scholar] [CrossRef]
- Weijenberg, R.A.F.; Delwel, S.; Van Ho, B.; Van Der Maarel-Wierink, C.D.; Lobbezoo, F. Mind your teeth—The relationship between mastication and cognition. Gerodontology 2019, 36, 2–7. [Google Scholar] [CrossRef]
- De Angelis, F.; Basili, S.; Giovanni, F.; Dan Trifan, P.; Di Carlo, S.; Manzon, L. Influence of the oral status on cardiovascular diseas-es in an older Italian population. Int. J. Immunopathol. Pharmacol. 2018, 32, 394632017751786. [Google Scholar]
- Su, Y.; Yuki, M.; Hirayama, K.; Sato, M.; Han, T. Denture Wearing and Malnutrition Risk Among Community-Dwelling Older Adults. Nutrients 2020, 12, 151. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.-Y.; Lee, Y.-L.; Lin, S.-Y.; Chou, Y.-C.; Chung, D.; Huang, N.; Chou, Y.-J.; Wu, C.-Y. Association Between Tooth Loss, Body Mass Index, and All-Cause Mortality Among Elderly Patients in Taiwan. Medicine 2015, 94, e1543. [Google Scholar] [CrossRef] [PubMed]
- Van der Bilt, A. Assessment of mastication with implications for oral rehabilitation: A review. J. Oral Rehabil. 2011, 38, 754–780. [Google Scholar] [CrossRef]
- Luke, D.A.; Lucas, P.W. Chewing efficiency in relation to occlusal and other variations in the natural human dentition. Br. Dent. J. 1985, 159, 401–403. [Google Scholar] [CrossRef] [PubMed]
- N’Gom, P.I.; Woda, A. Influence of impaired mastication on nutrition. J. Prosthet. Dent. 2002, 87, 667–673. [Google Scholar] [CrossRef]
- Paphangkorakit, J.; Chaiyapanya, N.; Sriladlao, P.; Pimsupa, S. Determination of chewing efficiency using muscle work. Arch. Oral Biol. 2008, 53, 533–537. [Google Scholar] [CrossRef] [PubMed]
- Macura-Karbownik, A.; Chladek, G.; Żmudzki, J.; Kasperski, J. Chewing efficiency and occlusal forces in PMMA, acetal and polyamide removable partial denture wearers. Acta Bioeng. Biomech. 2016, 18, 137–144. [Google Scholar]
- Okamoto, N.; Amano, N.; Nakamura, T.; Yanagi, M. Relationship between tooth loss, low masticatory ability, and nutritional in-dices in the elderly: A cross-sectional study. BMC Oral Health 2019, 19, 110. [Google Scholar] [CrossRef]
- Newton, J.P.; Yemm, R.; Abel, R.W.; Menhinick, S. Changes in human jaw muscles with age and dental state. Gerodontology 1993, 10, 16–22. [Google Scholar] [CrossRef]
- Motegi, E.; Nomura, M.; Tachiki, C.; Miyazaki, H.; Takeuchi, F.; Takaku, S.; Abe, Y.; Miyatani, M.; Ogai, T.; Fuma, A.; et al. Occlusal force in people in their sixties attending college for elderly. Bull. Tokyo Dent. Coll. 2009, 50, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Elsyad, M.A.; Hegazy, S.A.F.; Hammouda, N.I.; Al-Tonbary, G.Y.; Habib, A.A. Chewing efficiency and electromyographic activity of masseter muscle with three designs of implant-supported mandibular overdentures. A cross-over study. Clin. Oral Implant. Res. 2014, 25, 742–748. [Google Scholar] [CrossRef] [PubMed]
- Slagter, A.P.; Bosman, F.; Van Der Bilt, A. Comminution of two artificial test foods by dentate and edentulous subjects. J. Oral Rehabil. 1993, 20, 159–176. [Google Scholar] [CrossRef] [PubMed]
- Bilhan, H.; Geckili, O.; Mumcu, E.; Cilingir, A.; Bozdag, E. The influence of implant number and attachment type on maximum bite force of mandibular overdentures: A retrospective study. Gerodontology 2012, 29, e116–e120. [Google Scholar] [CrossRef]
- World Health Organization. Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1995; Volume 854, pp. 1–452. [Google Scholar]
- Sieber, C.C. The elderly patient—Who is that? Internist 2007, 48, 1190–1192. [Google Scholar] [CrossRef]
- Geckili, O.; Mumcu, E.; Bilhan, H. The Effect of Maximum Bite Force, Implant Number, and Attachment Type on Marginal Bone Loss around Implants Supporting Mandibular Overdentures: A Retrospective Study. Clin. Implant Dent. Relat. Res. 2012, 14 (Suppl. 1), e91–e97. [Google Scholar] [CrossRef]
- Wagner, F.; Seemann, R.; Marincola, M.; Ewers, R. Fiber-Reinforced Resin Fixed Prostheses on 4 Short Implants in Severely Atrophic Maxillas: 1-Year Results of a Prospective Cohort Study. J. Oral Maxillofac. Surg. 2018, 76, 1194–1199. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, O.; Beaumont, C.; Tatakis, D.N.; Zafiropoulos, G.-G. Telescopic crowns as attachments for implant supported restora-tions: A case series. J. Oral Implantol. 2006, 32, 291–299. [Google Scholar] [CrossRef]
- Heckmann, S.M.; Schrott, A.; Graef, F.; Wichmann, M.G.; Weber, H.-P. Mandibular two-implant telescopic overdentures. Clin. Oral Implant. Res. 2004, 15, 560–569. [Google Scholar] [CrossRef] [PubMed]
- Shinogaya, T.; Sodeyama, A.; Matsumoto, M. Bite force and occlusal load distribution in normal complete dentitions of young adults. Eur. J. Prosthodont. Restor. Dent. 1999, 7, 65–70. [Google Scholar]
- Goiato, M.C.; Garcia, A.R.; Dos Santos, D.M.; Zuim, P.R.J. Analysis of Masticatory Cycle Efficiency in Complete Denture Wearers. J. Prosthodont. 2010, 19, 10–13. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, P.O.; Thornell, L.E. Histochemical and morphological muscle-fibre characteristics of the human masseter, the medial pterygoid and the temporal muscles. Arch. Oral Biol. 1983, 28, 781–795. [Google Scholar] [CrossRef]
- Chong, M.X.; Khoo, C.D.; Goh, K.H.; Rahman, F.; Shoji, Y. Effect of age on bite force. J. Oral Sci. 2016, 58, 361–363. [Google Scholar] [CrossRef]
- Palinkas, M.; Nassar, M.S.; Cecílio, F.A.; Siéssere, S.; Semprini, M.; Machado-de-Sousa, J.P.; Hallak, J.E.C.; Regalo, S.C.H. Age and gender influence on maximal bite force and masticatory muscles thickness. Arch. Oral Biol. 2010, 55, 797–802. [Google Scholar] [CrossRef]
- De Abreu, R.A.M.; Pereira, M.D.; Furtado, F.; Prado, G.P.R.; Mestriner, W.; Ferreira, L.M. Masticatory efficiency and bite force in individuals with normal occlusion. Arch. Oral Biol. 2014, 59, 1065–1074. [Google Scholar] [CrossRef]
- Van der Bilt, A.; Burgers, M.; van Kampen, F.M.C.; Cune, M.S. Mandibular implant-supported overdentures and oral function. Clin. Oral Implant. Res. 2010, 21, 1209–1213. [Google Scholar] [CrossRef]
- Carlsson, G.E.; Lindquist, L.W. Ten-year longitudinal study of masticatory function in edentulous patients treated with fixed complete dentures on osseointegrated implants. Int. J. Prosthodont. 1994, 7, 448–453. [Google Scholar]
- Tripathi, G.A.A.P.; Rajwadha, N.; Chhaparia, N.; Sharma, A.; Anant, M. Comparative evaluation of maximum bite force in den-tulous and edentulous individuals with different facial forms. J. Clin. Diagn. Res. 2014, 8, ZC37. [Google Scholar]
- Schimmel, M.; Katsoulis, J.; Genton, L.; Müller, F. Masticatory function and nutrition in old age. Swiss Dent. J. 2015, 125, 449–454. [Google Scholar] [PubMed]
- Müller, F.; Hernandez, M.; Grütter, L.; Aracil-Kessler, L.; Weingart, D.; Schimmel, M. Masseter muscle thickness, chewing efficiency and bite force in edentulous patients with fixed and removable implant-supported prostheses: A cross-sectional multicenter study. Clin. Oral Implant. Res. 2012, 23, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Amaral, C.F.; Pinheiro, M.A.; Câmara-Souza, M.B.; Carletti, T.M.; Garcia, R.R. Bite Force, Masseter Thickness, and Oral Health–Related Quality of Life of Elderly People with a Single-Implant Mandibular Overdenture. Int. J. Prosthodont. 2019, 32, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, A.K.; Wada, M.; Ikebe, K.; Maeda, Y. To what extent residual alveolar ridge can be preserved by implant? A systematic review. Int. J. Implant. Dent. 2016, 2, 22. [Google Scholar] [CrossRef] [PubMed]
- Luraschi, J.; Schimmel, M.; Bernard, J.-P.; Gallucci, G.O.; Belser, U.; Müller, F. Mechanosensation and maximum bite force in edentulous patients rehabilitated with bimaxillary implant-supported fixed dental prostheses. Clin. Oral Implant. Res. 2012, 23, 577–583. [Google Scholar] [CrossRef]
- Lloyd, P.M. Complete-denture therapy for the geriatric patient. Dent. Clin. N. Am. 1996, 40, 239–254. [Google Scholar] [PubMed]
- Park, J.-H.; Lee, J.-Y.; Shin, S.-W.; Kim, H.J. Effect of conversion to implant-assisted removable partial denture in patients with mandibular Kennedy classification Ⅰ: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2020, 31, 360–373. [Google Scholar] [CrossRef]
- Roccuzzo, M.; Bonino, F.; Gaudioso, L.; Zwahlen, M.; Meijer, H.J.A. What is the optimal number of implants for removable recon-structions? A systematic review on implant-supported overdentures. Clin. Oral Implant. Res. 2012, 23 (Suppl. 6), 229–237. [Google Scholar] [CrossRef]
- Guenin, C.; Martin-Cabezas, R. How many implants are necessary to stabilise an implant-supported maxillary overdenture? Evid. Based Dent. 2020, 21, 28–29. [Google Scholar] [CrossRef]
- Garrett, N.R.; Kapur, K.K.; Hamada, M.O.; Roumanas, E.D.; Freymiller, E.; Han, T.; Diener, R.M.; Levin, S.; Chen, T. A randomized clinical trial comparing the efficacy of mandibular implant-supported overdentures and conventional dentures in diabetic patients. Part II. Comparisons of masticatory performance. J. Prosthet. Dent. 1998, 79, 632–640. [Google Scholar] [CrossRef]
- Sessle, B.J.; Adachi, K.; Avivi-Arber, L.; Lee, J.; Nishiura, H.; Yao, D.; Arber, N.; Yoshino, K. Neuroplasticity of face primary motor cortex control of orofacial movements. Arch. Oral Biol. 2007, 52, 334–337. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, A. Oral processing in elderly: Understanding eating capability to drive future food texture modifications. Proc. Nutr. Soc. 2019, 78, 329–339. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, C.H.; Mahan, P.E.; Lundeen, H.C.; Brehnan, K.; Walsh, E.K.; Holbrook, W.B. Occlusal forces during chewing and swallowing as measured by sound transmission. J. Prosthet. Dent. 1981, 46, 443–449. [Google Scholar] [CrossRef]
- Eerikäinen, E.; Könönen, M. Forces required by complete dentures for penetrating food in simulated function. J. Oral Rehabil. 1987, 14, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Mioche, L.; Bourdiol, P.; Monier, S. Chewing behaviour and bolus formation during mastication of meat with different textures. Arch. Oral Biol. 2003, 48, 193–200. [Google Scholar] [CrossRef]

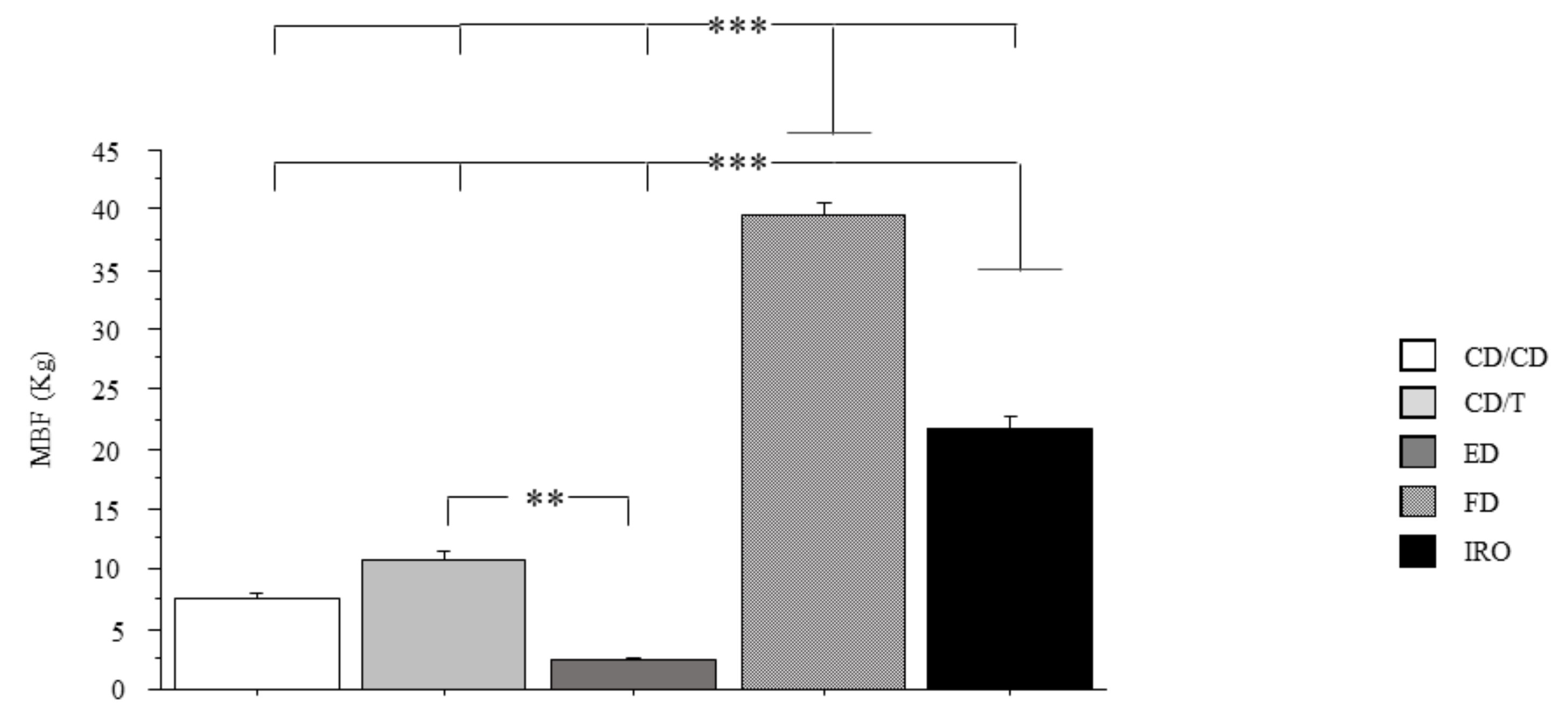
| Experimental Groups | Gender | MBF Max (Right/Left) | MBF Min (Right/Left) | Mean MBF | Total Mean MFB | No. Subject 40% < 8 kg | % | No. Subject 40% > 8 kg | % | Mean % |
|---|---|---|---|---|---|---|---|---|---|---|
| Full dentition (FD) | males | 106 | 15.5 | 44.8 | 39.7 | 7 | 6.6 | 98 | 94.5 | 92.2 |
| females | 65.5 | 11.5 | 34.6 | 10 | 10 | 90 | 90 | |||
| Overdentures/overdentures (IRO) | males | 31 | 8.5 | 22.4 | 21.7 | 7 | 35 | 13 | 65 | 62.5 |
| females | 28 | 12.5 | 21.1 | 8 | 40 | 12 | 60 | |||
| Conventional prosthesis/teeth (CD/T) | males | 20.5 | 6.5 | 11.6 | 10.8 | 21 | 95.4 | 1 | 4.5 | 2.25 |
| females | 14 | 6 | 10 | 0 | ||||||
| Conventional prosthesis in both arches (CD/CD) | males | 11.5 | 4 | 7.7 | 7.4 | 0 | ||||
| females | 11.5 | 3.5 | 7.2 | 0 | ||||||
| Edentulous patients (ED) | males | 4.5 | 1.5 | 2.7 | 2.3 | 0 | ||||
| females | 3 | 1 | 2 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manzon, L.; Vozza, I.; Poli, O. Bite Force in Elderly with Full Natural Dentition and Different Rehabilitation Prosthesis. Int. J. Environ. Res. Public Health 2021, 18, 1424. https://doi.org/10.3390/ijerph18041424
Manzon L, Vozza I, Poli O. Bite Force in Elderly with Full Natural Dentition and Different Rehabilitation Prosthesis. International Journal of Environmental Research and Public Health. 2021; 18(4):1424. https://doi.org/10.3390/ijerph18041424
Chicago/Turabian StyleManzon, Licia, Iole Vozza, and Ottavia Poli. 2021. "Bite Force in Elderly with Full Natural Dentition and Different Rehabilitation Prosthesis" International Journal of Environmental Research and Public Health 18, no. 4: 1424. https://doi.org/10.3390/ijerph18041424
APA StyleManzon, L., Vozza, I., & Poli, O. (2021). Bite Force in Elderly with Full Natural Dentition and Different Rehabilitation Prosthesis. International Journal of Environmental Research and Public Health, 18(4), 1424. https://doi.org/10.3390/ijerph18041424







