Twelve Weeks of a Staged Balance and Strength Training Program Improves Muscle Strength, Proprioception, and Clinical Function in Patients with Isolated Posterior Cruciate Ligament Injuries
Abstract
1. Introduction
2. Materials and Methods
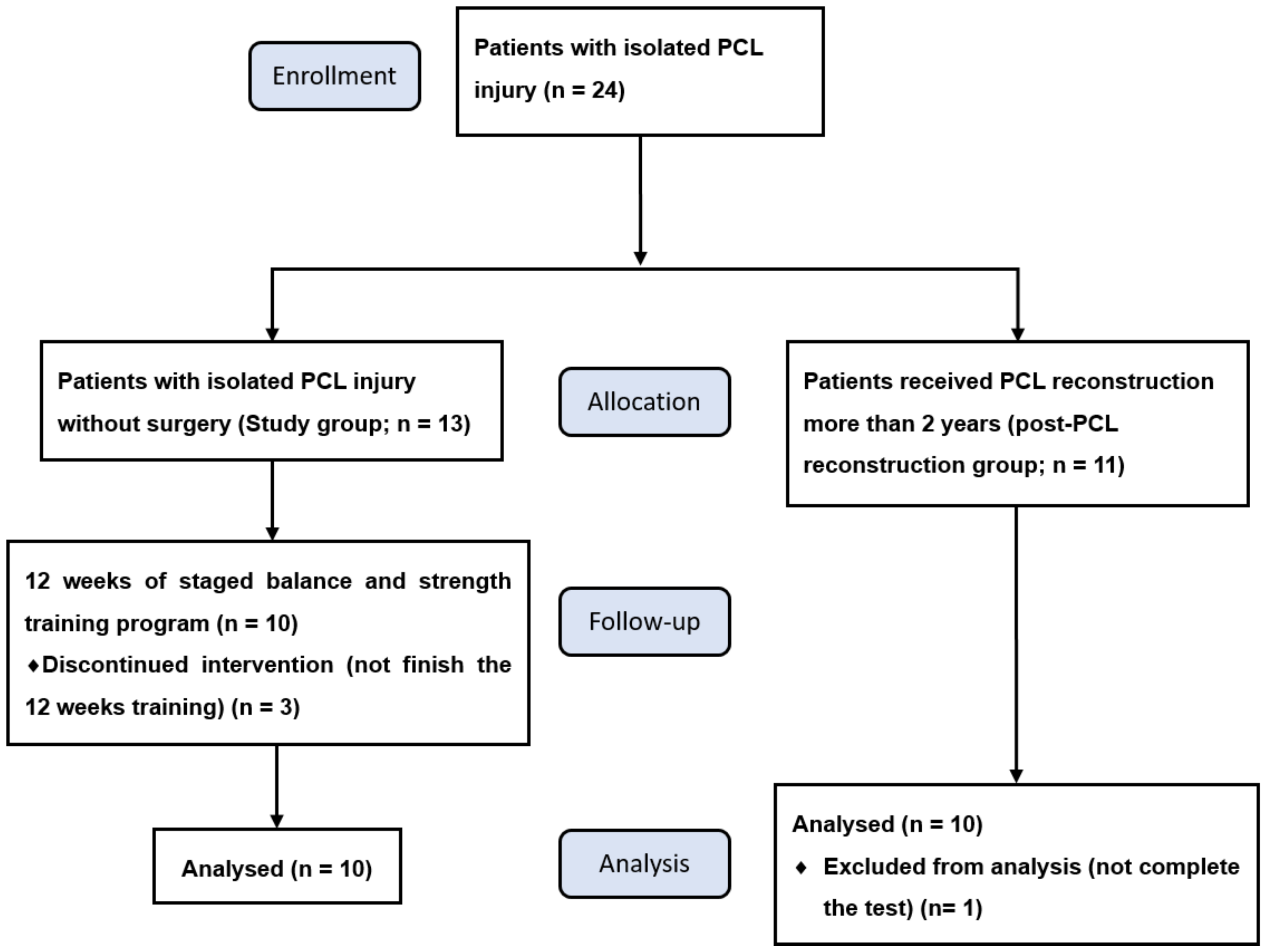
2.1. Subjects
2.2. Balance Combined with Strength Training Program
2.2.1. Warm Up
2.2.2. Muscle Strength Training
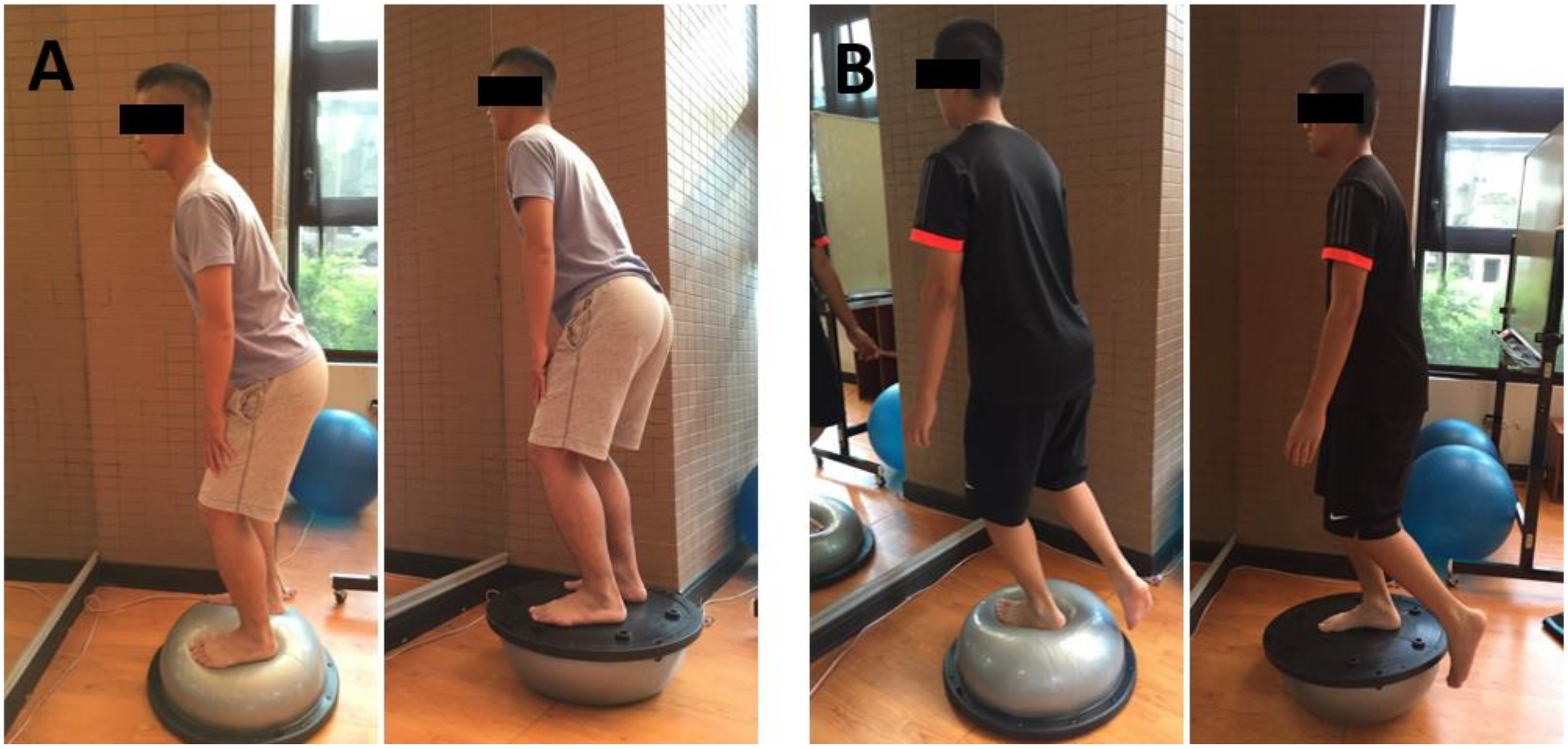
2.2.3. Balance Training
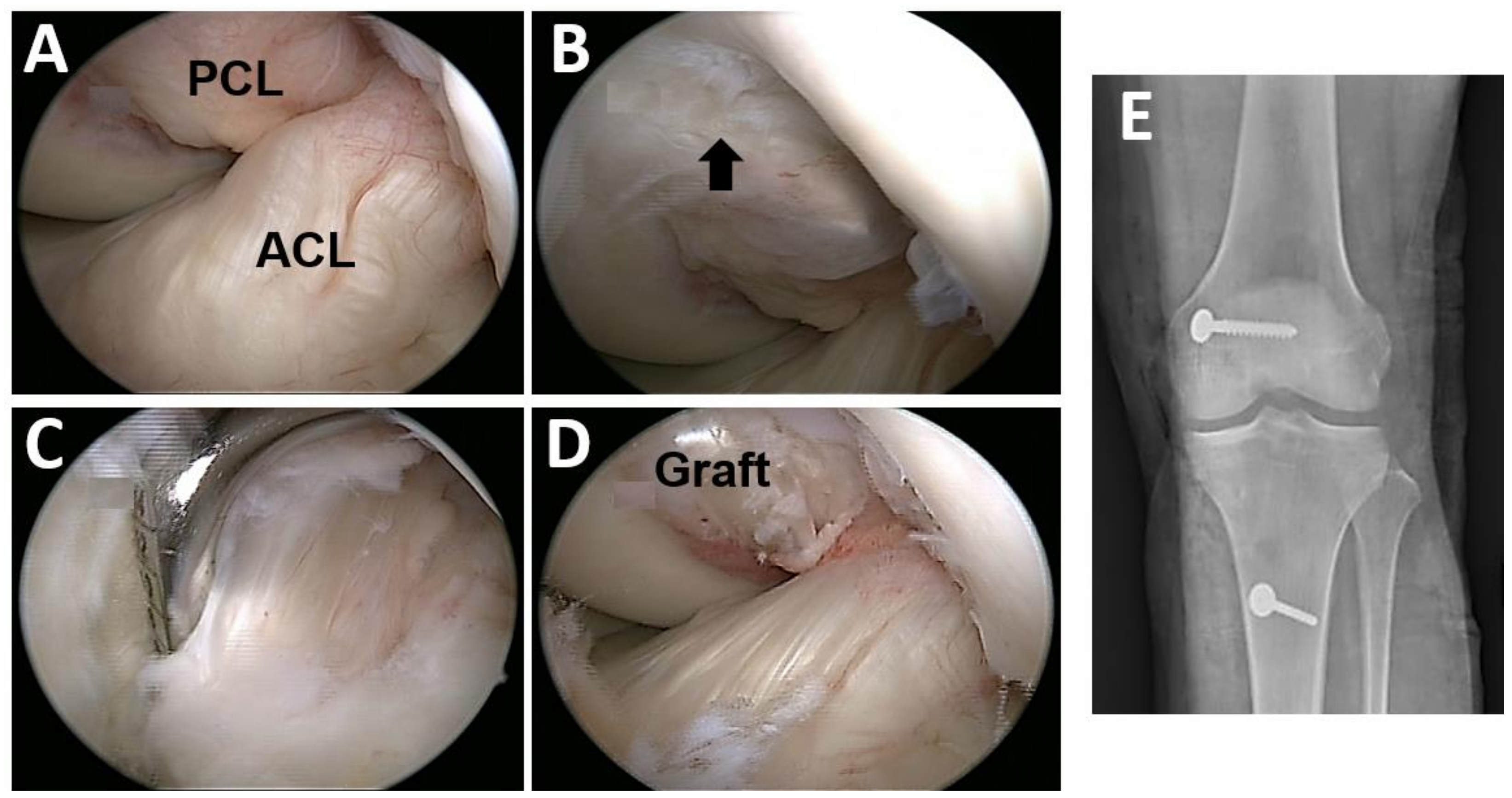
2.3. Posterior Cruciate Ligament Reconstruction Procedure
2.4. Evaluations
2.4.1. Functional Score Analysis
2.4.2. Proprioception Test
2.4.3. Laxity Examination
2.4.4. Strength Test
2.5. Statistical Analysis
3. Results
3.1. Subject Profiles
3.2. Functional Outcome and Proprioception Were Significantly Improved after BOSU Balance and Strength Training in Patients with an Isolated PCL Injury
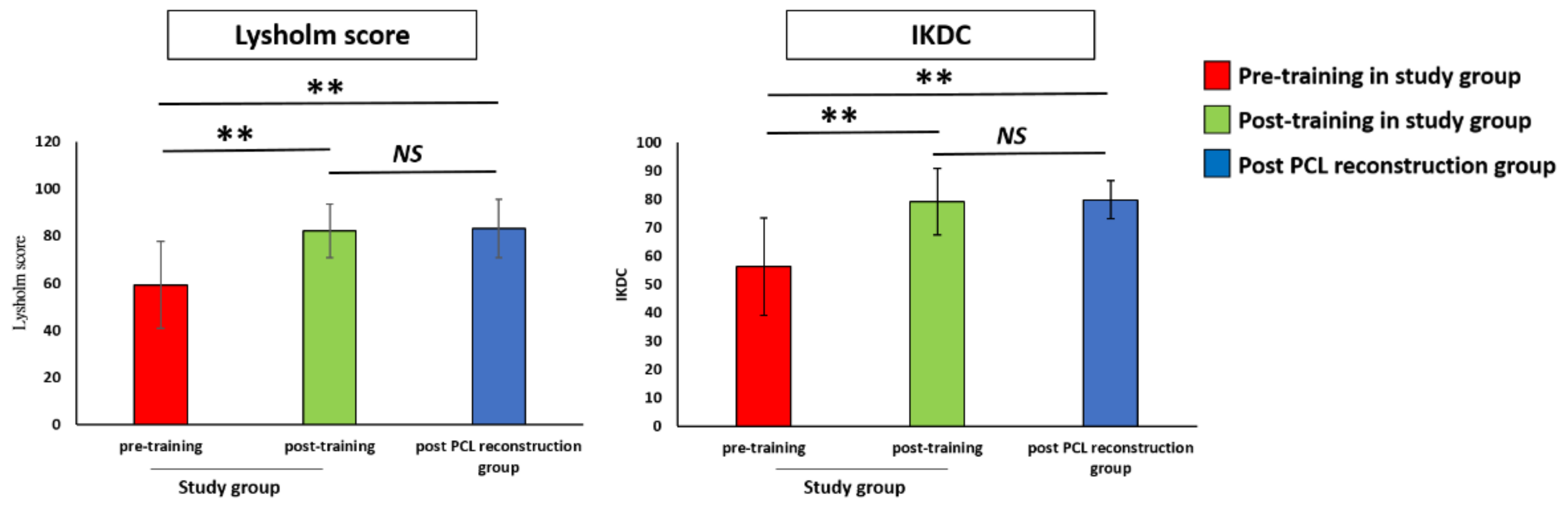
3.2.1. Functional Score
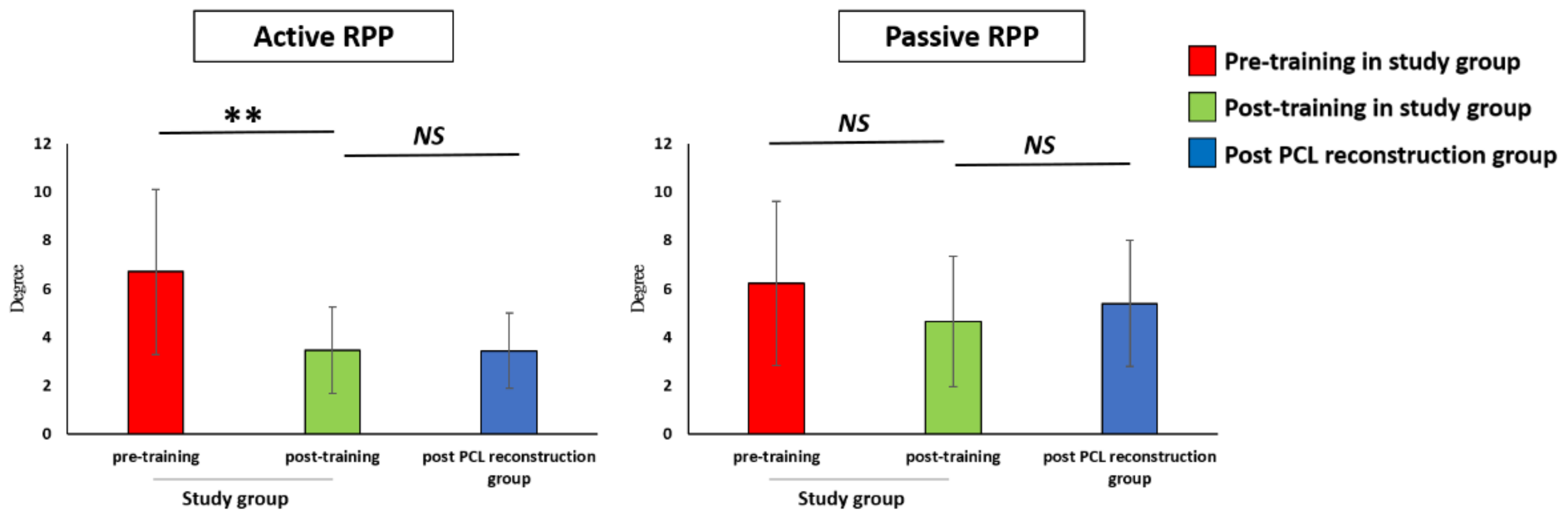
3.2.2. Proprioception
3.3. No Improvement in Knee Joint Laxity after BOSU Balance and Strengthening Training in Patients with an Isolated PCL Injury
Laxity Examination
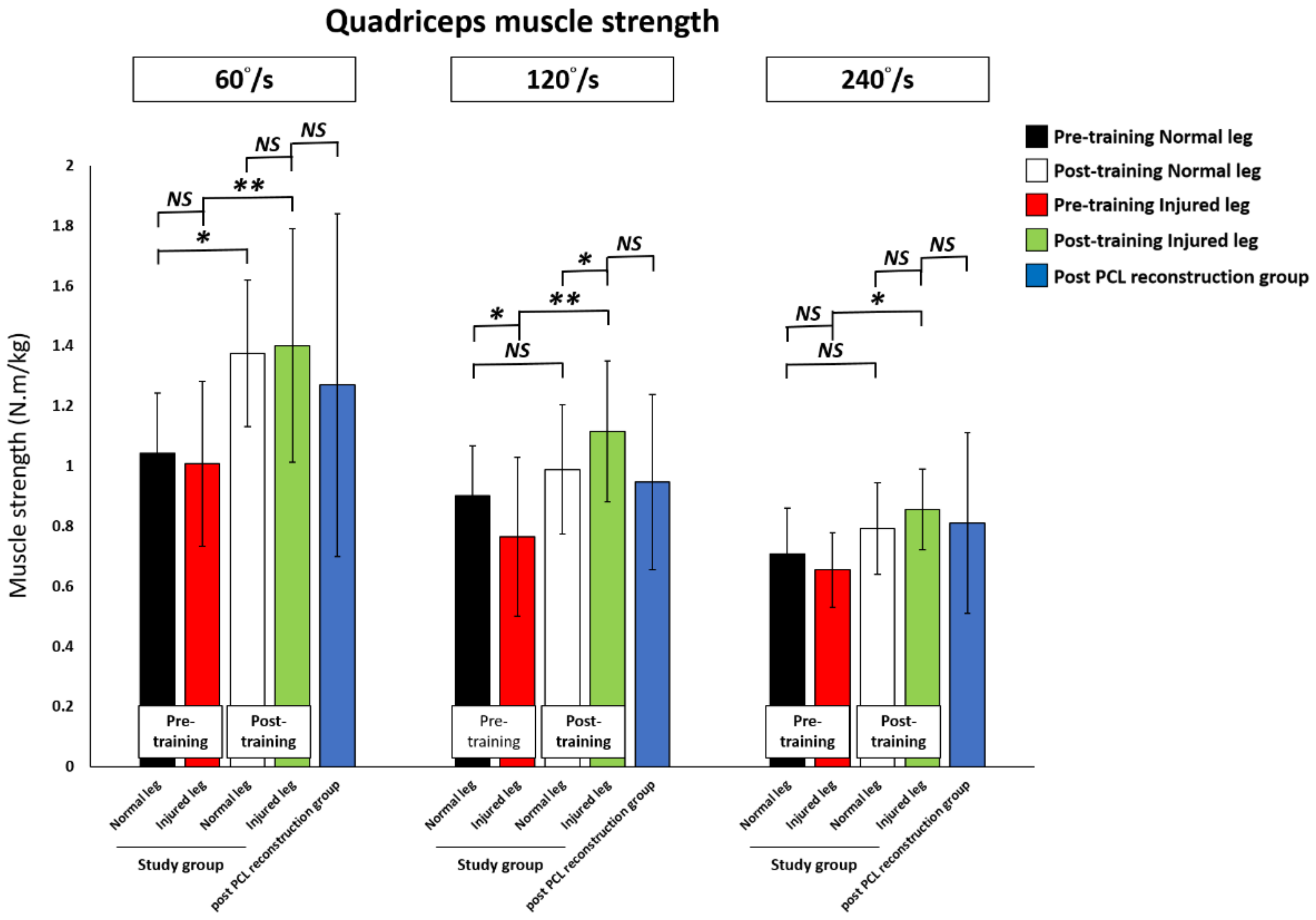
3.4. Quadriceps and Hamstring Muscle Strength after Training Was Significantly Improved in the PCL Injured Knee and Reached the Level of the Post-Training Normal Leg and the Post-PCL Reconstruction Group
3.5. In the Study Group the PCL Injured Leg Presented a Higher Improvement in the Knee Muscle Strength Than the Normal Leg and there was No Difference between the Dominant and Non-Dominant Injured Legs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Wind, W.M., Jr.; Bergfeld, J.A.; Parker, R.D. Evaluation and treatment of posterior cruciate ligament injuries: Revisited. Am. J. Sports Med. 2004, 32, 1765–1775. [Google Scholar] [CrossRef]
- Colvin, A.C.; Meislin, R.J. Posterior cruciate ligament injuries in the athlete: Diagnosis and treatment. Bull. Hosp. Jt. Dis. 2009, 67, 45–51. [Google Scholar]
- Gollehon, D.L.; Torzilli, P.A.; Warren, R.F. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J. Bone Jt. Surg. Am. 1987, 69, 233–242. [Google Scholar] [CrossRef]
- Patel, D.V.; Allen, A.A.; Warren, R.F.; Wickiewicz, T.L.; Simonian, P.T. The nonoperative treatment of acute, isolated (partial or complete) posterior cruciate ligament-deficient knees: An intermediate-term follow-up study. HSS J. 2007, 3, 137–146. [Google Scholar] [CrossRef]
- Clancy, W.G., Jr.; Sutherland, T.B. Combined posterior cruciate ligament injuries. Clin. Sports Med. 1994, 13, 629–647. [Google Scholar] [CrossRef]
- Fanelli, G.C. Posterior cruciate ligament injuries in trauma patients. Arthroscopy 1993, 9, 291–294. [Google Scholar] [CrossRef]
- Harner, C.D.; Hoher, J. Evaluation and treatment of posterior cruciate ligament injuries. Am. J. Sports Med. 1998, 26, 471–482. [Google Scholar] [CrossRef]
- Shelbourne, K.D.; Davis, T.J.; Patel, D.V. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am. J. Sports Med. 1999, 27, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Petrigliano, F.A.; McAllister, D.R. Isolated posterior cruciate ligament injuries of the knee. Sports Med. Arthrosc. Rev. 2006, 14, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Becker, E.H.; Watson, J.D.; Dreese, J.C. Investigation of multiligamentous knee injury patterns with associated injuries presenting at a level I trauma center. J. Orthop. Trauma 2013, 27, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Bedi, A.; Musahl, V.; Cowan, J.B. Management of Posterior Cruciate Ligament Injuries: An Evidence-Based Review. J. Am. Acad Orthop. Surg. 2016, 24, 277–289. [Google Scholar] [CrossRef]
- Wang, D.; Graziano, J.; Williams, R.J., 3rd; Jones, K.J. Nonoperative Treatment of PCL Injuries: Goals of Rehabilitation and the Natural History of Conservative Care. Curr. Rev. Musculoskelet. Med. 2018, 11, 290–297. [Google Scholar] [CrossRef]
- Goyal, K.; Tashman, S.; Wang, J.H.; Li, K.; Zhang, X.; Harner, C. In vivo analysis of the isolated posterior cruciate ligament-deficient knee during functional activities. Am. J. Sports Med. 2012, 40, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Margheritini, F.; Mariani, P.P. Diagnostic evaluation of posterior cruciate ligament injuries. Knee Surg. Sports Traumatol. Arthrosc. 2003, 11, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Shelbourne, K.D.; Clark, M.; Gray, T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am. J. Sports Med. 2013, 41, 1526–1533. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Pareek, A.; Barrett, I.J.; Kremers, H.M.; Bryan, A.J.; Stuart, M.J.; Levy, B.A.; Krych, A.J. Incidence and long-term follow-up of isolated posterior cruciate ligament tears. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3017–3023. [Google Scholar] [CrossRef] [PubMed]
- Van de Velde, S.K.; Gill, T.J.; Li, G. Dual fluoroscopic analysis of the posterior cruciate ligament-deficient patellofemoral joint during lunge. Med. Sci. Sports Exerc. 2009, 41, 1198–1205. [Google Scholar] [CrossRef]
- Kozanek, M.; Fu, E.C.; Van de Velde, S.K.; Gill, T.J.; Li, G. Posterolateral structures of the knee in posterior cruciate ligament deficiency. Am. J. Sports Med. 2009, 37, 534–541. [Google Scholar] [CrossRef]
- Boynton, M.D.; Tietjens, B.R. Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am. J. Sports Med. 1996, 24, 306–310. [Google Scholar] [CrossRef]
- Eitzen, I.; Moksnes, H.; Snyder-Mackler, L.; Risberg, M.A. A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J. Orthop. Sports Phys. Ther. 2010, 40, 705–721. [Google Scholar] [CrossRef] [PubMed]
- Hartigan, E.; Axe, M.J.; Snyder-Mackler, L. Perturbation training prior to ACL reconstruction improves gait asymmetries in non-copers. J. Orthop. Res. 2009, 27, 724–729. [Google Scholar] [CrossRef]
- Myer, G.D.; Ford, K.R.; Brent, J.L.; Hewett, T.E. Differential neuromuscular training effects on ACL injury risk factors in”high-risk” versus “low-risk” athletes. BMC Musculoskelet. Disord. 2007, 8, 39. [Google Scholar] [CrossRef]
- Pierce, C.M.; O’Brien, L.; Griffin, L.W.; Laprade, R.F. Posterior cruciate ligament tears: Functional and postoperative rehabilitation. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1071–1084. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.C.; Shon, O.J.; Kwack, B.H.; Lee, S.J. Proprioception and clinical results of anterolateral single-bundle posterior cruciate ligament reconstruction with remnant preservation. Knee Surg. Relat. Res. 2013, 25, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Yaggie, J.A.; Campbell, B.M. Effects of balance training on selected skills. J. Strength Cond. Res. 2006, 20, 422–428. [Google Scholar]
- Panics, G.; Tallay, A.; Pavlik, A.; Berkes, I. Effect of proprioception training on knee joint position sense in female team handball players. Br. J. Sports Med. 2008, 42, 472–476. [Google Scholar] [CrossRef]
- Paterno, M.V.; Myer, G.D.; Ford, K.R.; Hewett, T.E. Neuromuscular training improves single-limb stability in young female athletes. J. Orthop. Sports Phys. Ther. 2004, 34, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Urabe, Y.; Kawamura, K. Alignment control exercise changes lower extremity movement during stop movements in female basketball players. Knee 2008, 15, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Tegner, Y.; Lysholm, J. Rating systems in the evaluation of knee ligament injuries. Clin. Orthop. Relat. Res. 1985, 198, 43–49. [Google Scholar] [CrossRef]
- Odensten, M.; Lysholm, J.; Gillquist, J. Long-term follow-up study of a distal iliotibial band transfer (DIT) for anterolateral knee instability. Clin. Orthop. Relat. Res. 1983, 176, 129–135. [Google Scholar] [CrossRef]
- Hefti, F.; Muller, W.; Jakob, R.P.; Staubli, H.U. Evaluation of knee ligament injuries with the IKDC form. Knee Surg. Sports Traumatol. Arthrosc. 1993, 1, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Ingersoll, C.D.; Grindstaff, T.L.; Pietrosimone, B.G.; Hart, J.M. Neuromuscular consequences of anterior cruciate ligament injury. Clin. Sports Med. 2008, 27, 383–404. [Google Scholar] [CrossRef] [PubMed]
- Dejour, H.; Walch, G.; Peyrot, J.; Eberhard, P. The natural history of rupture of the posterior cruciate ligament. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1988, 74, 35–43. [Google Scholar] [PubMed]
- Królikowska, A.; Sikorski, Ł.; Czamara, A.; Reichert, P. Effects of Postoperative Physiotherapy Supervision Duration on Clinical Outcome, Speed, and Agility in Males 8 Months After Anterior Cruciate Ligament Reconstruction. Med. Sci. Monit. 2018, 24, 6823–6831. [Google Scholar] [CrossRef] [PubMed]
- Czamara, A.; Tomaszewski, W.; Bober, T.; Lubarski, B. The effect of physiotherapy on knee joint extensor and flexor muscle strength after anterior cruciate ligament reconstruction using hamstring tendon. Med. Sci. Monit. 2011, 17, 35–41. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Czamara, A.; Krzemińska, K.; Widuchowski, W.; Dragan, S.L. The Muscle Strength of the Knee Joint after ACL Reconstruction Depends on the Number and Frequency of Supervised Physiotherapy Visits. Int. J. Environ. Res. Public Health 2021, 18, 10588. [Google Scholar] [CrossRef] [PubMed]
- Safran, M.R.; Allen, A.A.; Lephart, S.M.; Borsa, P.A.; Fu, F.H.; Harner, C.D. Proprioception in the posterior cruciate ligament deficient knee. Knee Surg. Sports Traumatol. Arthrosc. 1999, 7, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Katonis, P.G.; Assimakopoulos, A.P.; Agapitos, M.V.; Exarchou, E.I. Mechanoreceptors in the posterior cruciate ligament. Histologic study on cadaver knees. Acta Orthop. Scand. 1991, 62, 276–278. [Google Scholar] [CrossRef] [PubMed]
- Schutte, M.J.; Dabezies, E.J.; Zimny, M.L.; Happel, L.T. Neural anatomy of the human anterior cruciate ligament. J. Bone Jt. Surg. Am. 1987, 69, 243–247. [Google Scholar] [CrossRef]
- Clark, P.; MacDonald, P.B.; Sutherland, K. Analysis of proprioception in the posterior cruciate ligament-deficient knee. Am. J. Sports Med. 1986, 14, 35–38. [Google Scholar] [CrossRef]
- Grassmayr, M.J.; Parker, D.A.; Coolican, M.R.; Vanwanseele, B. Posterior cruciate ligament deficiency: Biomechanical and biological consequences and the outcomes of conservative treatment. A systematic review. J. Sci. Med. Sport 2008, 11, 433–443. [Google Scholar] [CrossRef]
- Li, G.; Papannagari, R.; Li, M.; Bingham, J.; Nha, K.W.; Allred, D.; Gill, T. Effect of posterior cruciate ligament deficiency on in vivo translation and rotation of the knee during weightbearing flexion. Am. J. Sports Med. 2008, 36, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Parolie, J.M.; Bergfeld, J.A. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am. J. Sports Med. 1986, 14, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Han, S.B.; Lee, J.H.; Lee, S.J.; Suh, D.W.; Jeong, H.J. Quadriceps Strength and Endurance After Posterior Cruciate Ligament Tears Versus Matched Group With Anterior Cruciate Ligament Tears. Arthroscopy 2015, 31, 1097–1101. [Google Scholar] [CrossRef] [PubMed]
- Tibone, J.E.; Antich, T.J.; Perry, J.; Moynes, D. Functional analysis of untreated and reconstructed posterior cruciate ligament injuries. Am. J. Sports Med. 1988, 16, 217–223. [Google Scholar] [CrossRef]
- Czamara, A.; Szuba, Ł.; Krzemińska, A.; Tomaszewski, W.; Wilk-Frańczuk, M. Effect of physiotherapy on the strength of tibial internal rotator muscles in males after anterior cruciate ligament reconstruction (ACLR). Med. Sci. Monit. 2011, 17, 523–531. [Google Scholar] [CrossRef] [PubMed]

| Study Group | Post-PCL Reconstruction Group | p Value | |
|---|---|---|---|
| Number (n) | 10 | 10 | |
| Gender (Male/Female) | 7/3 | 7/3 | |
| Injured site (Right/Left) | 5/5 | 4/6 | |
| Injured site (Dominant/Non-dominant) | 5/5 | ||
| Age (years) | 27.3 ± 9.4 | 30.1 ± 7.3 | 0.49 |
| Body height (cm) | 171.6 ± 6.5 | 169.8 ± 6.7 | 0.57 |
| Body weight (Kg) | 74.2 ± 11.9 | 72.4 ± 12.7 | 0.76 |
| Thigh circumference (cm) | 48.0 ± 3.5 | 46.6 ± 5.2 | 0.48 |
| Total knee range of motion (degree) | 118.7 ± 7.3 | 114.5 ± 7.4 | 0.24 |
| Tegner Activity Scale | 4.6 ± 1.7 | 4.9 ± 1.2 | 0.66 |
| Study Group | Post-PCL Reconstruction Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Training | Post-Training | |||||||||
| Normal Leg | Shapiro -Wilk p | Injured leg | Shapiro -Wilk p | Normal Leg | Shapiro -Wilk p | Injured Leg | Shapiro -Wilk p | Post-PCL Reconstruction | Shapiro -Wilk p | |
| Functional score | ||||||||||
| Lysholm score | 59.30 (19.49) | 0.8377 | 82.20 (11.94) | 0.1312 | 83.20 (13.18) | 0.1378 | ||||
| IKDC | 56.30 (18.07) | 0.3701 | 79.20 (12.40) | 0.7194 | 79.90 (7.20) | 0.9777 | ||||
| Propriception (°) | ||||||||||
| Active RPP | 6.70 (3.61) | 0.0784 | 3.47 (1.89) | 0.9071 | 3.19 (1.46) | 0.5020 | ||||
| Passive RPP | 6.23 (3.56) | 0.4584 | 4.66 (2.83) | 0.1475 | 5.50 (2.85) | 0.8414 | ||||
| Muscle strength (N·m/kg) | ||||||||||
| Ext 60°/s | 1.04 (0.20) | 0.682 | 1.01 (0.27) | 0.6784 | 1.38 (0.24) | 0.5477 | 1.40 (0.39) | 0.6746 | 1.27 (0.57) | 0.4760 |
| Ext 120°/s | 0.90 (0.16) | 0.705 | 0.77 (0.26) | 0.0433 | 0.99 (0.21) | 0.0635 | 1.12 (0.23) | 0.7487 | 0.95 (0.29) | 0.7761 |
| Ext 240°/s | 0.70 (0.15) | 0.687 | 0.65 (0.12) | 0.9340 | 0.79 (0.15) | 0.2230 | 0.86 (0.13) | 0.7566 | 0.81 (0.30) | 0.0664 |
| Flex 60°/s | 0.59 (0.20) | 0.313 | 0.46 (0.19) | 0.9061 | 0.80 (0.25) | 0.0321 | 0.71 (0.33) | 0.6591 | 0.63 (0.28) | 0.0803 |
| Flex 120°/s | 0.58 (0.17) | 0.367 | 0.44 (0.15) | 0.5667 | 0.64 (0.21) | 0.3723 | 0.62 (0.19) | 0.3855 | 0.55 (0.18) | 0.1117 |
| Flex 240°/s | 0.56 (016) | 0.012 | 0.50 (0.15) | 0.4798 | 0.58 (0.14) | 0.4771 | 0.60 (0.17) | 0.6353 | 0.56 (0.14) | 0.5260 |
| Analysis (p) of Quadriceps and Hamstring Muscle Strength Test | ||||||
|---|---|---|---|---|---|---|
| Muscle Strength (N·m/kg) | Pre-Training Normal Leg vs. Pre-Training Injured Leg a | Pre-Training Normal Leg vs. Post-Training Normal Leg a | Pre-Training Injured Leg vs. Post-Training Injured Leg a | Post-Training Injured Leg vs. Post-Training Normal Leg a | Post-Training Injured Leg vs. Post-PCL Reconstruction b | Effect Size (95% CI) |
| Ext 60°/s | 0.6980 | 0.0250 * | 0.0034 ** | 0.7995 | 0.5544 | 1.25 (0.68–1.81) |
| Ext 120°/s | 0.0403 * | 0.3770 | 0.0045 ** | 0.0261 * | 0.1706 | 1.19 (0.65–1.73) |
| Ext 240°/s | 0.0833 | 0.2542 | 0.0103 * | 0.1245 | 0.6662 | 1.02 (0.56–1.49) |
| Flex 60°/s | 0.0410 * | 0.0832 | 0.0134 * | 0.2202 | 0.5719 | 0.97 (0.53–1.41) |
| Flex 120°/s | 0.0074 ** | 0.4477 | 0.0202 * | 0.4965 | 0.4277 | 0.89 (0.49–1.29) |
| Flex 240°/s | 0.0933 | 0.7964 | 0.1583 | 0.5025 | 0.5762 | 0.49 (0.27–0.71) |
| Value Change of Muscle Strength in Study Group | Improvement of Muscle Strength in Study Group | |||||
|---|---|---|---|---|---|---|
| Normal Leg (n = 10) (N·m/kg) | Injured Leg (n = 10) (N·m/kg) | p Value | Normal Leg (n = 10) (%) | Injured Leg (n = 10) (%) | p Value | |
| Ext 60°/s | 33.26 (12.40) | 39.37 (9.99) | 0.5385 | 38.86 (13.93) | 43.16 (10.87) | 0.7362 |
| Ext 120°/s | 8.67 (9.33) | 35.01 (9.31) | 0.0003 ** | 13.80 (12.15) | 58.25 (17.07) | 0.0010 ** |
| Ext 240°/s | 8.41 (6.91) | 20.15 (6.23) | 0.0074 ** | 16.73 (10.82) | 36.22 (12.11) | 0.0029 ** |
| Flex 60°/s | 20.5 (10.53) | 24.73 (8.06) | 0.6381 | 56.49 (26.95) | 65.48 (25.43) | 0.7289 |
| Flex 120°/s | 6.69 (8.43) | 17.94 (6.37) | 0.0457 * | 17.72 (15.38) | 50.79 (16.20) | 0.300 |
| Flex 240°/s | 1.9 (7.15) | 10.48 (6.81) | 0.1732 | 10.79 (13.02) | 28.67 (14.40) | 0.1515 |
| Value Change of Muscle Strength in Injured Leg in Study Group | Improvement of Muscle Strength in Injured Leg in Study Group | |||||
|---|---|---|---|---|---|---|
| Dominant Leg (n = 5) (N·m/kg) | Non-Dominant Leg (n = 5) (N·m/kg) | p Value | Dominant Leg (n = 5) (%) | Non-Dominant Leg (n = 5) (%) | p Value | |
| Ext 60°/s | 40.12 (8.37) | 38.62 (19.47) | 0.9453 | 43.33 (9.33) | 43.00 (21.09) | 0.9891 |
| Ext 120°/s | 34.98 (8.83) | 35.04 (17.65) | 0.9973 | 57.05 (20.36) | 59.45 (29.93) | 0.9488 |
| Ext 240°/s | 23.78 (8.90) | 16.52 (9.43) | 0.4002 | 44.57 (19.18) | 27.87 (16.02) | 0.5233 |
| Flex 60°/s | 22.44 (11.37) | 27.02 (12.68) | 0.7299 | 41.35 (16.36) | 89.61 (48.50) | 0.3899 |
| Flex 120°/s | 18.96 (7.20) | 16.92 (11.42) | 0.7571 | 50.15 (18.30) | 51.43 (29.07) | 0.9714 |
| Flex 240°/s | 9.42 (10.05) | 11.54 (10.35) | 0.8314 | 23.67 (19.31) | 33.67 (23.42) | 0.7508 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, C.-C.; Yao, H.-I.; Fan, T.-Y.; Lin, Y.-C.; Lin, H.-T.; Chou, P.P.-H. Twelve Weeks of a Staged Balance and Strength Training Program Improves Muscle Strength, Proprioception, and Clinical Function in Patients with Isolated Posterior Cruciate Ligament Injuries. Int. J. Environ. Res. Public Health 2021, 18, 12849. https://doi.org/10.3390/ijerph182312849
Lu C-C, Yao H-I, Fan T-Y, Lin Y-C, Lin H-T, Chou PP-H. Twelve Weeks of a Staged Balance and Strength Training Program Improves Muscle Strength, Proprioception, and Clinical Function in Patients with Isolated Posterior Cruciate Ligament Injuries. International Journal of Environmental Research and Public Health. 2021; 18(23):12849. https://doi.org/10.3390/ijerph182312849
Chicago/Turabian StyleLu, Cheng-Chang, Hsin-I Yao, Tsang-Yu Fan, Yu-Chuan Lin, Hwai-Ting Lin, and Paul Pei-Hsi Chou. 2021. "Twelve Weeks of a Staged Balance and Strength Training Program Improves Muscle Strength, Proprioception, and Clinical Function in Patients with Isolated Posterior Cruciate Ligament Injuries" International Journal of Environmental Research and Public Health 18, no. 23: 12849. https://doi.org/10.3390/ijerph182312849
APA StyleLu, C.-C., Yao, H.-I., Fan, T.-Y., Lin, Y.-C., Lin, H.-T., & Chou, P. P.-H. (2021). Twelve Weeks of a Staged Balance and Strength Training Program Improves Muscle Strength, Proprioception, and Clinical Function in Patients with Isolated Posterior Cruciate Ligament Injuries. International Journal of Environmental Research and Public Health, 18(23), 12849. https://doi.org/10.3390/ijerph182312849







